Abstract
Background
Patients with repeated hospitalizations represent a group with potentially avoidable utilization. Recent publications have begun to highlight the heterogeneity of this group. Latent class analysis provides a novel methodological approach to utilizing administrative data to identify clinically meaningful subgroups of patients to inform tailored intervention efforts.
Objectives
To identify clinically distinct subgroups of adult super-utilizers. Research Design: Retrospective cohort analysis. Subjects: Adult patients who had an admission at an urban safety-net hospital in 2014 and two or more admissions within the preceding 12 months.
Measures
Patient-level medical, mental health and substance use diagnoses, social characteristics, demographics, utilization and charges were obtained from administrative data. Latent class analyses were used to determine the number and characteristics of latent subgroups that best represented these data.
Results
In this cohort (N=1,515), a 5-class model was preferred based on model fit indices, clinical interpretability and class size: Class 1 (16%) characterized by alcohol use disorder and homelessness; Class 2 (14%) characterized by medical conditions, mental health/substance use disorders and homelessness; Class 3 (25%) characterized primarily by medical conditions; Class 4 (13%) characterized by more serious mental health disorders, drug use disorder and homelessness; and Class 5 (32%) characterized by medical conditions with some mental health and substance use. Patient demographics, utilization, charges and mortality also varied by class.
Conclusions
The overall cohort had high rates of multiple chronic medical conditions, mental health, substance use disorders and homelessness. However, the patterns of these conditions were different between subgroups, providing important information for tailoring interventions.
Keywords: Super-Utilizer, Latent Class Analysis, Mental health, Social determinants of health, Urban Safety-net
Introduction
Healthcare spending in the United States is largely concentrated among a small proportion of the population.1–3 While high costs are related to several factors such as multiple chronic conditions, catastrophic illnesses, surgeries or procedures, and prescription drug costs,3–5 it is estimated that approximately half of the costs among these disproportionately costly patients are a result of repeated utilization of acute care services (e.g., hospital and emergency department visits).6 Total cost estimates for patients with repeated hospitalizations, or “super-utilizers,” range from 17.9%7 to 30%8 depending on the population evaluated and charges included. This disproportionate share of costs has generated interest in better understanding the needs of this at-risk population.
Descriptive analyses on high-utilizing Medicaid or uninsured populations consistently find that such populations are likely to have multiple chronic conditions.2,8,9 However, medical complexity alone does not fully explain patterns of repeat hospitalizations. As compared to the Medicare population, Medicaid patients with readmissions are more likely to have comorbid behavioral health or substance abuse conditions.10 Additionally, programs targeting this population report that social risk factors such as language, health literacy, unemployment, substance abuse and housing are important factors driving healthcare utilization.11,12 Healthcare systems are increasingly interested in understanding how social determinants influence health and healthcare utilization as they grapple with at-risk payment models. Hence, a better understanding of these factors and their association with healthcare utilization is needed.
Interventions targeting high-cost patients have invested heavily in care management/coordination with wrap around social and behavioral health support. Despite the proliferation of these programs, the evidence assessing their impact is limited and those with some demonstrated success utilize a strategic approach to targeting patients.13,14 Further underscoring the need for a strategic targeting of patients, a recent analysis described the prevalence and differential charges among several mutually exclusive subgroups of adult super-utilizers based on the presence of a single variable (e.g. trauma, cancer, mental health).8 While this analysis provides information on the heterogeneity of the population it did not take into account the co-occurring nature of many medical, behavioral and social conditions and thus may not provide the sufficient precision needed for targeting clinical interventions.
In this current work, we sought to take a more data driven and inclusive approach that utilized all available data to assess whether distinct patient subgroups might exist within a super-utilizer population. Latent Class Analysis (LCA) was used to determine if individual level, observable, administrative data representing social, medical and behavioral health conditions coalesced to form specific clinically relevant subgroups of patients. This is a novel way to utilize administrative data that accounts for super-utilizer complexity and provides information to inform tailored intervention approaches based on different patient profiles.
Methods
Setting
This study was conducted at Denver Health (DH), an integrated safety-net healthcare system in Denver, Colorado.15 Among other services, DH includes a Level 1 Adult Trauma Center, 500 bed acute care hospital and nine federally qualified community health centers, serving about a quarter of the Denver population and is the largest healthcare provider in Colorado to people with Medicaid or no insurance.
Participants
The literature contains varying definitions for super-utilizer and the definition used for this analysis was adapted from prior work.8 Super-utilizers were defined as adult patients (≥18 years of age) who had a hospital admission during the study period (January 1, 2014 to December 31, 2014) and had two or more admissions within the preceding 12 months of this index admission. Therefore, all included patients had at least 3 admissions within a 12-month time period. The aim of this analysis was to assess the extent to which a broad definition of super-utilization might contain clinically relevant subgroups amenable to unique clinical interventions. Therefore, the only exclusion criteria applied was a small group of patients requiring nearly weekly admissions for emergent dialysis, as this admission is not preventable through existing clinical management options.
Data Sources
Administrative data from DH’s clinical and financial data warehouse were used to obtain the clinical and service utilization variables of interest. DH’s data warehouse integrates comprehensive information from Denver Health’s electronic medical record with administrative data from the financial, clinical encounter, and claims systems. For patients who participated in DH’s healthcare plans, non-DH clinical, service and financial data were also available through health plan billing data. Mortality data were obtained from the Colorado Department of Public Health and Environment. The Colorado Multiple Institutional Review Board reviewed this project and determined that it was not human subjects research.
LCA Indicator Variables
For the LCA we were interested in identifying individual level indicator variables that represented medical, mental health/substance use and social conditions influencing overall health. Based on the super-utilizer literature, available administrative data, internal clinical insight, and the Institute of Medicine recommendations,16 multiple variables were reviewed for inclusion. Elixhauser comorbidity software17,18 and the Clinical Classification Software (CCS) system19 were used to create validated summary variables that grouped similar Individual International Classification of Diseases, Ninth Revision (ICD-9) codes. Where greater granularity was desired or validated summary variables were not available we utilized single ICD-9 codes. Based on variable distribution and clinical relevance, 30 variables were selected for inclusion (see Table, Supplemental Digital Content 1, which provides the ICD9s used to identify medical, mental health and substance use disorders).
Medical Conditions
The Elixhauser software generates 29 common comorbidities. However, based on low distributions and lack of clinical relevance and the ability to combine some of the conditions, 14 dichotomous conditions were retained: congestive heart failure, valvular disease, pulmonary circulation disorders, peripheral vascular disease, hypertension, other neurological disorders, chronic pulmonary disease, diabetes (including diabetes with complications and diabetes without complications), renal failure, liver disease, cancer (including lymphoma, metastatic cancer, and solid tumor without metastases), coagulopathy, obesity and anemia (including blood loss and deficiency anemias). Three additional medical variables were created: the CCS definition was used to identify coronary artery disease; ICD-9 338.2x was used to identify chronic pain, and the DH trauma registry was used to identify exposure to a serious physical injury.
Mental Health (MH) and Substance Use Disorders (SUD)
Eight dichotomous variables related to mental health and substance use were included. The CCS definitions were used to identify schizophrenia, depression, bipolar disorder and anxiety disorders as these definitions provided more granular mental health groupings compared to Elixhauser. The ICD-9 309.81 was used to identify post-traumatic stress disorder. The Elixhauser definition was used to identify alcohol and drug use disorders and the ICD-9 305.1 was used to identify tobacco use disorder.
Social Characteristics
The following 5 dichotomous variables were obtained: homelessness and marital status at the index admission and high utilization of emergency department services (≥4 visits) use of non-medical alcohol detoxification services and having had at least one primary care visit in the 12 months prior to index admission.
Additional Data
Demographics
Demographics variables included age, gender, race/ethnicity, primary language and payer source at the time of the 2014 index admission. Dual-eligibility was defined as having a primary payer of Medicare and a secondary payer of Medicaid or participation in DH’s dual-eligible health plan.
Healthcare utilization and charges
Visit level data reflecting admissions, outpatient utilization, and total charges were obtained for the 12 months prior and 6 months after the index admission. Total charges included DH admissions and outpatient services (medical/surgical and behavioral), professional charges, laboratory, radiology, durable medical equipment (dispensed at hospitalization or outpatient visit), dental, pharmacy (inpatient only) and medical supplies. Total charges outside the DH system were also captured for patients with a DH health plan.
To provide additional descriptive detail concerning illness burden, the 3M™ Clinical Risk Groups software was used to calculate clinical risk groups (CRGs).20 CRGs are a predictive modeling tool that calculates risk strata and future healthcare utilization based on age, gender, site of service, timing and duration of treatment, pharmacy claims, diagnoses and procedures21.
Latent Class Analysis
Latent Class analysis (LCA) is a data-driven method that utilizes individual level observable data (indicator variables) to identify underlying latent groups of people (classes). It is conceptually similar to exploratory factor analysis (EFA); however, LCA examines patterns within people across the indicators whereas EFA takes a variable centered approach based on correlations within the whole sample. The iterative procedure attempts to find the best fitting set of classes to describe underlying profiles among the indicator variables. Thus, the identified latent classes explain shared patterns among the multiple observed indicator variables. In this way, the analysis takes a person-centered approach to identifying homogenous subgroups of people and for each class provides information on the probability of each indicator variable allowing for the identification of the most prominent attributes of each class. Additionally, unlike other analyses (e.g., multiple regression), LCA does not benefit from parsimony of variables because it is a person-centered rather than variable-centered analysis. Therefore, all variables believed to be clinically relevant can be included in the analysis.22
A central decision point in LCA is to determine how many classes best fit the data. This is done by comparing the fit of a set of models (e.g., 2 classes to 3 and so on) using fit statistics as well as interpretability of the produced classes. Model fit is often evaluated using the Akaike Information Criterion23 (AIC) and the sample size adjusted Bayesian Information Criterion24 (adj BIC). These indices reflect the extent to which shared patterns across indicator variables are not well explained by the estimated classes. Lower values on these indices from each successive model indicate a better fit. Additionally, the Lo-Mendell-Rubin (L-M-R) statistic25 and bootstrapped Likelihood Ratio Test 26 (BLRT) directly assess whether successive solutions fit the data better than a nested model with one fewer class. These tests provide a statistical test that directly compares two models to determine which number of classes is best. The entropy statistic, an indicator of accurate class differentiation and posterior probabilities, ranges from 0 to 1; values closer to 1 indicate higher classification accuracy. Finally, the estimated probabilities of each of the indicator variables within each class provides information to describe the classes and determine whether the classes are distinct from one another and clinically interpretable.
Statistical Analyses
LCA was run using Mplus 7.1 software27 with the 30 identified dichotomous indicators. Separate LCA models were estimated with 2 through 7 class solutions. To identify which model was the best fit for these data, the model fit indices described above were reviewed as well as the clinical interpretability and size of each class; models with classes smaller than 10% were not retained. SAS Enterprise Guide software version 9.3 was used to examine demographic, burden of illness, charge and utilization differences among the identified classes, using Chi-square and analysis of variance tests where appropriate.
Results
There were 17,524 unique adult admissions in 2014, with 1,515 identified as super-utilizing patients. The demographics, clinical risk status and average charges are presented in Table 1. Compared to the entire sample of admissions, super-utilizers were older, more likely to be homeless, from a minority population, male, more likely to have a significant medical burden (CRG of 6 or higher) and less likely to have private insurance. On average super-utilizer charges were 8 times that of the overall population of any admitted patient.
TABLE 1.
Demographic Characteristics of Denver Health 2014 Adult Admissions and the Subset of Super-Utilizers
| DH Admission (N=17,524) | Super-Utilizers (N=1,515) | |
|---|---|---|
| Age [Mean (SD)] | 33.1 (24.5) | 53.8 (15.4) |
| N(%) | N (%) | |
| Homeless | 1,788 (10.2) | 670 (44.2) |
| Primary Language is English | 13,833 (79.3) | 1,261 (83.0) |
| Race/Ethnicity | ||
| Hispanic/Latino | 5991(34.2) | 612 (40.4) |
| White | 8206(46.8) | 569 (37.6) |
| Black | 2350(13.4) | 262 (17.3) |
| Asian | 518(3.0) | 23 (1.5) |
| Other | 459(2.6) | 49 (3.2) |
| Gender | ||
| Male | 7,917(45.2) | 832 (54.9) |
| Female | 9,607(54.8) | 683 (45.1) |
| Payer Source at Index Admission | ||
| Commercial | 2320(13.2) | 35 (2.3) |
| Medicaid | 10406(59.4) | 857 (56.6) |
| Medicare | 2468(14.1) | 319 (21.0) |
| Over 65 and dual eligible | 160(0.9) | 120 (7.9) |
| Under 65 and dual eligible | 74(0.4) | 114 (7.5) |
| Uninsured | 1938(11.0) | 69 (4.6) |
| Unknown* | 2(0.0) | 1 (0.0) |
| Clinical Risk Group Status | ||
| 1: Healthy | 4,551 (26.9) | 3 (0.2) |
| 2: History of Significant Acute Disease | 1,674 (9.9) | 11 (0.7) |
| 3: Single Minor Chronic Condition | 711 (4.2) | 10 (0.7) |
| 4: Minor Chronic Disease in Multiple Organ Systems | 139 (0.8) | 2 (0.1) |
| 5: Single Dominant or Moderate Chronic Condition | 3,190 (18.9) | 49 (3.2) |
| 6: Significant Chronic Conditions in Multiple Organ Systems | 4,685 (27.7) | 649 (42.8) |
| 7: Dominant Chronic Disease in 3 or More Organ Systems | 1,051 (6.2) | 433 (28.6) |
| 8: Dominant, Metastatic and Complicated Malignancies | 319 (1.9) | 111 (7.3) |
| 9: Catastrophic Conditions | 601 (3.6) | 247 (16.3) |
| Total Charges in Previous 12 months [Mean (SD)] | $20,724 ($178,331) | $166,735 ($165,707) |
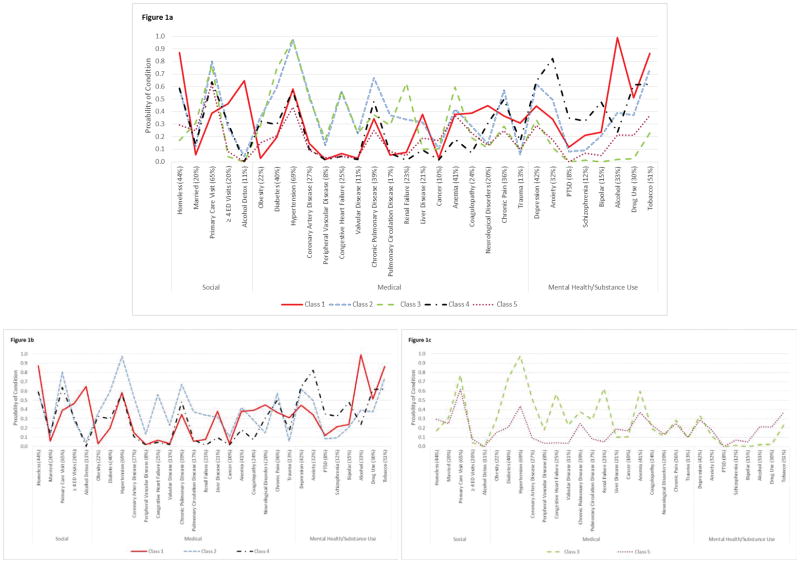
A final LCA model was identified that consisted of 5 classes. Entropy of the 5 class model was .785 and classes ranged in size from 13% to 32% of the sample. Figure 1 summarizes the overall prevalence of each indicator variable (x axis) and probability of individuals in each class having each of the 30 specific social, medical, mental health and substance use disorder indicators (y axis).
Figure 1. Probability of Social, Medical and Mental Health/Substance Use Indicators by 5 Latent Classes.
1a. The estimated probability (Y axis) for each indicator variable (X axis) in the latent class analysis is shown for each of the 5 classes. On the horizontal axis, the overall sample prevalence for each indicator is given (%) and the indicators are grouped by social, medical, and mental health/substance use. The separate lines demonstrate how the classes differ across the indicators and provide information on which indicators are more prevalent for each of the 5 classes. 1b and 1c presents the same data but separates it by the high homelessness classes (1b) and the primarily medical classes (1c).
Class 1 (N=243, 16.0%) was characterized by significant alcohol use and homelessness. Individuals in this group had a 99% probability of alcohol use disorder and a high probability of being homeless (87%). Compared to the other classes, this class had the highest probability of high ED utilization (47%) and alcohol detoxification admissions (65%) and had the lowest probability of utilizing primary care services (39%). This class also had the highest probability of physical trauma (31%), liver disease (38%), neurological conditions (45%) and tobacco use (86%) and the lowest probability of being married (6%). While not as high as Class 4, this class had high probabilities of PTSD (12%), schizophrenia/other psychotic disorders (21%), bipolar disorder (24%) and drug use disorder (51%).
Classes 2 (N=218, 14.4%) and 3 (N=374, 24.7%) both represented medically complex patients with similar probabilities for primary care utilization (80% vs. 77%) and similar probabilities across many of the medical conditions; however, Class 2 was characterized by medical conditions, mental health and substance use disorders and homelessness and Class 3 was primarily characterized by medical conditions. In contrast to Class 3, Class 2 had a higher probability of being homeless (58% vs. 17%) and a lower probability of being married (12% vs. 31%), a higher probability of high ED utilization (27% vs. 4%) and much higher probabilities for all the mental health and substance use disorders. Class 3 had the lowest probability out of all the classes for any of the mental health and substance use disorders, except depression.
Class 4 (N=189, 12.5%) was the smallest class and was characterized by more serious mental health disorders, drug use disorders and homelessness. Compared to all other classes, this class had the highest probability of anxiety (82%), depression (65%), bipolar (48%), PTSD (35%), and schizophrenia/other psychotic disorders (32%). This class also had the second highest probability of chronic pain (50%) and a fairly high probability of high ED utilization (31%).
Class 5 (N=491, 32.4%) was the largest class and was characterized mostly by medical conditions but in comparison to Class 3, the primarily medical group, this class had lower probabilities for most of the medical conditions but higher probabilities for all substance use disorders, anxiety (18%), schizophrenia (7%) and bipolar (5%) as well as homelessness (30%).
Tables 2 presents demographic and more detailed pre-index admission utilization and charge data for the classes. Class 1 characterized by alcohol use and homelessness was more likely to be male, white, and had the highest average ED visits and the lowest primary care visits of all classes. Classes 2, 3 and 5 all were characterized by medical conditions but were differentiated by MH/SUDs and social challenges. Class 2, medically complex with MH/SUDs and homelessness, also were more likely to be male and were more likely to be Black. This class had the highest charges and average primary care visits and second highest average admissions. Class 3, primarily medically complex, were more likely to be older, Hispanic/Latino and primarily speak Spanish than the other classes. They had the highest average admissions and the second highest average charges. Class 5, the third medical class, had the second highest proportion of patients who primarily speak Spanish. Class 4, the class characterized by MH/drug use disorders and homelessness had the highest proportion of females, were the youngest and had the lowest total charges as compared to the other classes.
TABLE 2.
Additional Adult Super-Utilizer Characteristics by Class (N=1,515)
| Class 1: Alcohol/Homeless N= 243 (16%) | Class 2: Medical, MH/SUDs, Homeless N=218 (14%) | Class 3: Medical N=374 (25%) | Class 4: MH/Drug Use, Homeless N=189 (13%) | Class 5:Medical (lower with some MH/SUDs) N=491 (32%) | p-value | |
|---|---|---|---|---|---|---|
| Age1 | ||||||
| Mean (SD) | 50.5 (10.5) | 55.6 (9.7) | 64.6 (13.8) | 46.2 (13.0) | 50.1 (17.0) | <.0001 |
| Gender1 | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Female | 52 (21.4) | 82 (37.6) | 191 (51.1) | 108 (57.1) | 251 (51.1) | <.0001 |
| Male | 191 (78.6) | 136 (62.4) | 183 (48.9) | 81 (42.9) | 240 (48.9) | |
| Language1 | ||||||
| English | 238 (97.9) | 209 (95.9) | 244 (65.2) | 182 (96.3) | 388 (79.0) | <.0001 |
| Spanish | 5 (2.1) | 9 (4.1) | 111 (29.7) | 5 (2.7) | 90 (18.3) | |
| Other | 0 (0.0) | 0 (0.0) | 19 (0.1) | 2 (1.0) | 13 (2.7) | |
| Race1 | ||||||
| Black | 35 (14.4) | 59 (27.1) | 59 (15.8) | 33 (17.5) | 76 (15.5) | <.0001 |
| Latino | 54 (22.2) | 66 (30.3) | 204 (54.6) | 56 (29.6) | 232 (47.3) | |
| Non-Hispanic White | 134 (55.1) | 87 (39.9) | 94 (25.1) | 92 (48.7) | 162 (33.0) | |
| Other | 20 (8.2) | 6 (2.7) | 17 (4.5) | 8 (4.2) | 21 (4.3) | |
| Payer1 | ||||||
| Private | 3 (1.2) | 3 (1.4) | 10 (2.7) | 5 (2.6) | 14 (2.8) | < .0001 |
| Uninsured | 9 (3.7) | 4 (1.8) | 22 (5.9) | 6 (3.2) | 28 (5.7) | |
| Medicaid | 181 (74.5) | 112 (51.6) | 130 (34.8) | 120 (63.5) | 314 (64.0) | |
| Medicare | 21 (8.6) | 48 (22.1) | 85 (22.7) | 22 (11.6) | 67 (13.6) | |
| Dual Eligible Under 65 | 18 (7.4) | 36 (16.6) | 29 (7.8) | 28 (14.8) | 27 (5.5) | |
| Dual Eligible 65+ | 11 (4.5) | 14 (6.5) | 98 (26.2) | 8 (4.2) | 41 (8.4) | |
| Homelessness1 | ||||||
| Homeless | 215(88.5) | 127(58.3) | 63(16.8) | 115(60.9) | 150(30.6) | <.0001 |
| Utilization2 | ||||||
| DH Primary Care Visits [Mean (SD)] | 1.8 (3.1) | 6.5 (6.5) | 5.3 (4.9) | 4.2 (5.0) | 4.2 (5.3) | < .0001 |
| DH Admissions [Mean (SD)] | 2.9 (1.4) | 4.0 (6.1) | 5.7 (11.6) | 2.8 (1.7) | 3.1 (4.9) | < .0001 |
| DH Emergency Department Admissions [Mean (SD)] | 6.0 (9.6) | 3.1 (4.5) | 0.9 (1.2) | 3.5 (4.7) | 1.2 (1.9) | < .0001 |
| Patients with a non-DH admission [# (%)] | 31 (12.8) | 31 (14.2) | 48 (13.8) | 18 (9.5) | 45 (9.2) | 0.0558 |
| Of Patients with non-DH admission, Admissions [Mean (SD)] | 1.5 (0.9) | 2.2 (1.6) | 1.5 (0.9) | 1.7 (1.1) | 1.4 (0.7) | 0.0708 |
| Total Charges (DH and non-DH)2 | ||||||
| Total Charges [Mean (SD)] | 155,546 (136,885) | 203,363 (195,882) | 188,623 (195,857) | 137,977 (150,299) | 150,408 (138,267) | < .0001 |
Index Admission
for the 12 months prior to Index Admission
Table 3 provides information for the 6 month period after the index admission. Class 1 continues to have the highest average ED visits and the lowest primary care visits, Class 2 continues to have the highest average charges and highest primary care visits, Class 3 continues to have the highest admissions and Classes 4 and 5 continue to have the lowest average charges. There is no difference between the classes in the number of months patients continued to meet super-utilizer criteria and overall 70% met criteria 6 months after the index admission. Eight percent of the sample died within 6 months with the highest proportions from the medically complicated classes.
TABLE 3.
Six Months Post Identification: Utilization, Charges, Super-Utilizer Group Stability and Mortality by Latent Class
| Overall | Class 1: Alcohol/Homeless (N=243) | Class 2: MH/SUD, Homeless (N=218) | Medical, Class 3: Medical (N=374) | Class 4: MH/Drug Use, Homeless (N=189) | Class 5: Medical (lower with some MH/SUD) (N=491) | p-value | |
|---|---|---|---|---|---|---|---|
| Utilization and Charges | |||||||
| Utilization | |||||||
| DH Primary Care Visits [Mean (SD)] | 2.5 (2.9) | 1.3 (2.4) | 3.6 (3.3) | 3.1 (2.9) | 2.4 (3.2) | 2.2 (2.5) | < .0001 |
| DH Admissions [Mean (SD)] | 1.8 (4.3) | 1.5 (1.7) | 1.9 (3.4) | 3.1 (6.8) | 0.9 (1.4) | 1.4 (3.7) | < .0001 |
| DH Emergency Department Admissions [Mean (SD)] | 1.8 (3.9) | 4.0 (6.6) | 2.3 (3.9) | 0.6 (1.0) | 2.5 (4.1) | 1.0 (2.7) | < .0001 |
| Patients with an external non-DH admission [# (%)] | 89 (5.9) | 22 (9.1%) | 20 (9.2%) | 20 (5.3%) | 9 (4.8%) | 18 (3.7%) | 0.0084 |
| Of Patients with non-DH admission, Admissions [Mean (SD)] | 1.6 (1.1) | 1.6 (1.1) | 1.9 (1.6) | 1.3 (0.6) | 2.0 (1.7) | 1.2 (0.6) | 0.2147 |
| Charges | |||||||
| Total Charges [Mean (SD)] | $67,319 ($97,395) | 75,115 (99,757) | 80,669 (89,226) | 79,317 (117,569) | 49,809 (84,446) | 54,161 (83,253) | < .0001 |
| Super-Utilizer Group Stability | |||||||
| # (%) Continuous | 1,074(70.1) | 169 (69.6) | 160 (73.4) | 256 (68.5) | 131 (69.3) | 358 (72.9) | 0.533 |
| # (%) Out and in | 72(4.8) | 17 (7.0) | 11 (5.1) | 21 (5.6) | 9 (4.8) | 14 (2.9) | 0.122 |
| # (%) Out | 369(24.4) | 57 (23.5) | 47 (21.6) | 97 (25.9) | 49 (25.9) | 119 (24.2) | 0.774 |
| # Months met SU criteria (Mean, SD) | 5.2(1.6) | 5.2 (1.5) | 5.3 (1.5) | 5.0 (1.7) | 5.3 (1.3) | 5.2 (1.6) | 0.108 |
| Mortality | |||||||
| Mortality 6 months post-index admission (#,%) | 121(8.0) | 7 (2.9) | 23 (10.6) | 35 (9.4) | 9 (4.8) | 47 (9.6) | 0.003 |
Table 4, compares the results of the LCA to a prior single variable subgroups analysis.8 It demonstrates the need to utilize multivariate analyses such as LCA as patients are complex and conditions co-occur and overlap in a one variable grouping. It also highlights the differential distribution across classes on a single variable grouping. For example, while 29% of the cohort had a serious mental health diagnosis, the probability of a mental health condition varies greatly using a multivariate approach as 76% had a mental health diagnosis in Class 4 compared to 8% in Class 3.
TABLE 4.
Single Variable Sub-Group Identification by Class
| Overall | Class 1: Alcohol/Homeless | Class 2: Medical, MH/SUD, Homeless | Class 3: Medical | Class 4: MH/Drug Use, Homeless | Class 5: Medical (lower with some MH/SUD) | p-value | |
|---|---|---|---|---|---|---|---|
| Terminal cancer patients | 19 (1.25) | 0 (0.0) | 2 (0.9) | 1 (0.3) | 0 (0.0) | 16 (3.3) | 0.0001 |
| Orthopedic surgical complications | 118 (7.8) | 19 (7.8) | 18 (8.3) | 39 (10.4) | 15 (7.9) | 27 (5.5) | 0.1217 |
| Trauma | 200 (13.2) | 78 (32.1) | 12 (5.5) | 30 (8.0) | 32 (16.9) | 48 (9.8) | 0.0001 |
| Mental health | 440 (29.0) | 97 (39.9) | 81 (37.2) | 29 (7.8) | 143 (75.7) | 90 (18.3) | <.0001 |
| Multiple chronic conditions (including CRG 6–7)* | 1082 (71.4) | 191 (78.6) | 161 (73.8) | 252 (67.4) | 162 (85.7) | 316 (64.4) | <.0001 |
higher CRGs excluded
Conclusions
This study contributes to the growing field of descriptive analyses on adult super-utilizers and is unique in its utilization of latent class analysis to identify and describe subgroups in this population. As opposed to hypothesis driven analyses, the results of an LCA are not limited to a specific test that is defined by a researcher. Rather, it employs a data driven approach that includes multiple clinical variables. This analysis identified five subgroups of super-utilizing patients with distinct clinical, social and demographic patterns and demonstrates the important role that social determinants of health play in providing services to this population and ultimately healthcare utilization and costs.
Among the five subgroups identified, three classes (1, 2 and 4) had a high probability (60% – 87%) of homelessness with very different patient profiles. Class 1 represents a group of patients with significant alcohol use combined with a lack of stability and support, as characterized by high rates of homelessness, low marriage rates, and over utilization of emergency services. The most pervasive medical conditions were neurological disorders, physical trauma and liver disease, conditions associated with adverse social conditions and alcohol abuse. Mental health disorders, drug and tobacco use were also prevalent in this subgroup and over three-fourths of this class were male. Given the lack of primary care utilization and high ED and detoxification utilization, this group may benefit from community based, outreach services or services embedded into an ED setting. Services should include multidisciplinary staff with a strong focus on housing, social support and SUD services.
Individuals in Class 2 have significant housing instability as well, but a much more complex medical profile (similar to Class 3 the primarily medical class) as well as co-occurring MH/SUDs. However, they are more engaged in primary care and have high ED utilization. Their high rates of ambulatory care sensitive conditions (e.g., diabetes, CHF, COPD) and frequent primary care visits suggest that more optimized medical management with alternative primary care models could greatly impact avoidable hospitalizations.28 The ambulatory ICU29 where there are ancillary staff to support medical, behavioral health and social needs might serve as a good model.
Class 4, the smallest group, also represents patients with housing instability but with more serious mental health disorders and drug use disorders as compared to the other two homeless groups. Given the level of mental illness, this group would most likely benefit from services either strongly aligned or embedded within a formal mental health treatment agency that also has co-occurring addiction expertise. Additionally, this group had the highest proportion of females as well as the highest probability of PTSD, indicating that trauma informed and gender-specific services may be important.
Class 3 represents patients with mostly complex medical conditions and an absence of social and behavioral health conditions. It is the second largest group consisting of almost a quarter of the cohort and has the highest average admissions. This group most likely does not need the ancillary behavioral health and social supports that the other groups may need and is unique in that over half identify as Latino and nearly 30% primarily speak Spanish. High-utilizers with multiple chronic conditions often experience significant care fragmentation, which can be exacerbated with each condition30 and with language barriers. Over three-fourths of this group utilized primary care suggesting that they may be responsive to care coordination or patient navigation services embedded within this setting. Community health workers (CHWs) may also be an effective intervention for this group as they often act as community liaisons, helping patients access the right services in the health system and providing critical support, such as educating patients on their medications. By acting as patient navigators and health educators, CHWs may help to decrease admissions through the reduction of recurrent 30-day readmissions and increasing patient activation.31 However, given the medical complexity of this group, additional analyses are needed to truly understand what admissions might be avoidable.
Class 5, the largest group, is ambiguous in that it appears to have a similar medical trajectory, although lower, as class 3 but is complicated with MH and SUDs. Given their lower medical conditions, it may be that these behavioral health conditions are greatly contributing to admissions and would likely benefit from screening in primary care and providing a strong linkage to MH and addiction services. However, this more heterogeneous group likely needs more analysis to truly understand it.
The work presented here has important implications, as it demonstrates how the combination of social, behavioral, and medical information can provide a granular understanding of high risk groups. By identifying patterns of interconnectedness among a costly and vulnerable patient population, it provides the opportunity to transform care in a way that addresses both medical needs and the social determinants of health. This builds on conceptual models that inform our current understanding of complex, multimorbid patients.32 In order for such analytic approaches to be scalable and actionable, health systems will need to routinely capture social and behavioral information33 which will be especially important as payers continue to reward population health approaches such as the CMS Accountable Health Communities payment model.34 For health systems to succeed, they will need to collect standardized data, employ new analytic approaches, and translate these insights into effective interventions to improve the overall health and outcomes of complex patients similar to this super-utilizer population.
Administrative health data provides a valuable opportunity to describe populations and to inform novel intervention approaches, but there are limitations that should be considered. Complete data capture in our study population was only possible for patients who received all their care in the DH system and/or were in our health plan. Most of the patients had government insurance (93%) at their index admission and therefore most likely utilized the DH system, however, we do not know the extent to which these patients remain in this system and/or exclusively use this system. Additionally, these data most likely underrepresent the presence of MH/SUDs as these conditions are not always validly and reliably coded in medical claims data and do not fully capture social determinants of health information. Similarly, we defined homelessness based on the index admission. This does not fully capture the fluidity of housing and may obscure cases of transient homelessness throughout the year. The results of the LCA are dependent upon how the sample was defined (e.g., by hospital admissions) and the prevalence and selection of indicator variables. Additional analyses are needed to understand the generalizability of these subgroups when selecting samples based on different criteria (e.g., high utilization of other services such as emergency or primary care) and within different healthcare and geographic settings. Lastly, this analysis was conducted by DH and findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor.
In summary, this analysis presents a novel methodological approach to utilizing administrative data to inform service delivery. It demonstrates the heterogeneity among super-utilizers and the need to utilize multivariate analyses such as these, especially with complex patients. This analysis also highlights the importance of ensuring the accurate collection of psychosocial variables in the healthcare setting and including these variables in analyses. We demonstrate the application of LCA in identifying and describing subgroups of super-utilizers unique to a local health system, which can be replicated by other systems in their efforts to provide appropriate and patient-centered services with the goal of improved health and reduced acute healthcare utilization.
Supplementary Material
Acknowledgments
Disclosure of funding: The project described was supported by Grant Number 1C1CMS331064 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented here was conducted by the awardee. Findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor.
Footnotes
Other Disclosure: Mortality data were supplied by the Health Statistics and Evaluation Branch of the Colorado Department of Public Health and Environment, which specifically disclaims responsibility for any analyses, interpretations, or conclusions it has not provided.
Presented in part at Academy Health’s annual conferences: San Diego, CA, June 2014 and Boston, MA, June 2016
Conflict of Interest: Authors declare no conflict of interest.
Contributor Information
Deborah J Rinehart, Associate Research Scientist, Denver Health and Hospital Authority, Assistant Professor, University of Colorado School of Medicine, Denver Health and Hospital Authority, 777 Bannock St., MC 6551, Denver, CO 80204, Phone: 303-602-2743, Fax: 303-602-2741.
Carlos Oronce, Resident Physician, University of Rochester Medical Center, Strong Memorial Hospital, Department of Medicine, Rochester, NY 14642, Phone: 703-577-2627, Fax: 303-602-2741.
M Joshua Durfee, Statistical Research Specialist, Denver Health and Hospital Authority, 777 Bannock St., MC 6551, Denver, CO 80204, Phone: 303-602-2742, Fax: 303-602-2741.
Krista W Ranby, Assistant Professor, Department of Psychology, University of Colorado Denver, 1200 Larimer, Denver, CO 80201, Phone: 303-556-8565, Fax: 303-556-3520.
Holly Batal, Medical Director, Denver Health Medical Plan, Associate Professor, University of Colorado School of Medicine, Ambulatory Care Services, Denver Health and Hospital Authority, 777 Bannock St, MC 1914, Denver, CO 80204, Phone: 303-602-5118, Fax: 303-602-8277.
Rebecca Hanratty, Director of General Internal Medicine, Denver Health and Hospital Authority, Associate Professor, University of Colorado School of Medicine, Denver Health and Hospital Authority, 777 Bannock St., MC 1914, Denver, CO 80204, Phone: 303-602-6397, Fax: 303-602-5132.
Jody Vogel, Attending Emergency Physician, Denver Health and Hospital Authority, Assistant Professor, University of Colorado School of Medicine, Denver Health and Hospital Authority, 777 Bannock St., MC 0108, Denver, CO 80204, Phone: 303-602-5165, Fax: 303-602-5184.
Tracy Johnson, Director, Health Care Reform Initiatives, Denver Health and Hospital Authority, Assistant Professor, University of Colorado School of Public Health, Denver Health and Hospital Authority, Department of Ambulatory Care Services, 21st Century Care Evaluation, 777 Bannock St., MC 6551, Denver, CO 80204, Phone: 303-602-2733, Fax: 303-602-2741.
References
- 1.Allen S, Croke A. The faces of Medicaid: the complexities of caring for people with chronic illnesses and disabilities. Princeton, NJ: Center for Health Care Strategies; 2000. [Google Scholar]
- 2.Kronick R, Bella M, Gilmer T. The faces of Medicaid III: refining the portrait of people with multiple chronic conditions. Princeton, NJ: Center for Health Care Strategies; 2009. [Google Scholar]
- 3.Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood) 2007;26(3):808–816. doi: 10.1377/hlthaff.26.3.808. [DOI] [PubMed] [Google Scholar]
- 4.Szekendi MK, Williams MV, Carrier D, Hensley L, Thomas S, Cerese J. The characteristics of patients frequently admitted to academic medical centers in the United States. J Hosp Med. 2015;10(9):563–568. doi: 10.1002/jhm.2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs associated with multimorbidity among VA patients. Med Care. 2014;52(Suppl 3):S31–36. doi: 10.1097/MLR.0000000000000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen OK, Tang N, Hillman JM, Gonzales R. What's cost got to do with it? Association between hospital costs and frequency of admissions among “high users” of hospital care. J Hosp Med. 2013;8(12):665–671. doi: 10.1002/jhm.2096. [DOI] [PubMed] [Google Scholar]
- 7.Jiang H, Weiss A, Barrett M, Sheng M. HCUP Statistical Brief #190. Agency for Healthcare Research and Quality; Rockville, MD: 2015. Characteristics of Hospital Stays for Super-Utilizers by Payer, 2012. [PubMed] [Google Scholar]
- 8.Johnson TL, Rinehart DJ, Durfee J, et al. For Many Patients Who Use Large Amounts Of Health Care Services, The Need Is Intense Yet Temporary. Health Aff (Millwood) 2015;34(8):1312–1319. doi: 10.1377/hlthaff.2014.1186. [DOI] [PubMed] [Google Scholar]
- 9.Boyd C, Leff B, Weeiss C, Wolff J, Clark R, Richards T. Clarifying multimorbidity to improve targeting and delivry of clinical services for Medicaid populations. Center for Health Care Strategies, Inc; 2010. [Google Scholar]
- 10.Regenstein M, Andres E. Reducing hospital readmissions among medicaid patients: a review of the literature. Qual Manag Health Care. 2014;23(1):20–42. doi: 10.1097/QMH.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 11.Bodenheimer T. [Accessed 2015];Strategies to reduce costs and improve care for high-utilizing Medicaid patients: relections on pioneering programs. 2013 Oct; http://www.chcs.org/resource/strategies-to-reduce-costs-and-improve-care-for-high-utilizing-medicaid-patients-reflections-on-pioneering-programs/
- 12.Hong C, Siegel A, Ferris T. Caring for high-need, high-cost patients: what makes for a successful care management program? New York (NY): Common-wealth Fund; 2014. http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2014/aug/1764_hong_caring_for_high_need_high_cost_patients_ccm_ib.pdf. [PubMed] [Google Scholar]
- 13.Congressional Budget Office. Lessons from Medicare’s Demonstration Projects on Disease Management, Care Coordination, and Value-Based Payment. Washington, DC: Congressional Budget Office; 2012. [Google Scholar]
- 14.Brown RS, Peikes D, Peterson G, Schore J, Razafindrakoto CM. Six features of Medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Aff (Millwood) 2012;31(6):1156–1166. doi: 10.1377/hlthaff.2012.0393. [DOI] [PubMed] [Google Scholar]
- 15.Gabow P, Eisert S, Wright R. Denver Health: a model for the integration of a public hospital and community health centers. Ann Intern Med. 2003;138(2):143–149. doi: 10.7326/0003-4819-138-2-200301210-00016. [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 17.Healthcare Cost and Utilization Project (HCUP) Comorbidity Software, version 3.7 [computer program] Rockville, MD: Agency for Healthcare Research and Quality; [Accessed March 2015]. [Google Scholar]
- 18.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Healthcare Cost and Utilization Project (HCUP) Clinical Classification Software for ICD9-CM [computer program] Rockville, MD: Agency for Healthcare Research and Quality; [Accessed March 2015]. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 20.3M Health Information Systems - US. 3M Clinical Risk Grouping Software Definitions Manual: Updated for v1.9. 2011 http://solutions.3m.com/wps/portal/3M/en_US/Health-Information-Systems/HIS/Products-and-Services/Products-List-A-Z/Clinical-Risk-Grouping-Software/
- 21.Hughes JS, Averill RF, Eisenhandler J, et al. Clinical Risk Groups (CRGs): a classification system for risk-adjusted capitation-based payment and health care management. Med Care. 2004;42(1):81–90. doi: 10.1097/01.mlr.0000102367.93252.70. [DOI] [PubMed] [Google Scholar]
- 22.Hagenaars JA, McCutcheon AL. Applied latent class analysis. Cambridge University Press; 2009. [Google Scholar]
- 23.Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov B, Csaki F, editors. Second international symposium on information theory. Verlag: Springer; 1973. pp. 267–281. [Google Scholar]
- 24.Sclove S. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 25.Yungtai L, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. [Google Scholar]
- 26.Nylund K, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 27.Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 28.AHRQ Quality Indicators. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Rockville, MD: Agency for Healthcare Research and Quality; 2001. Vol AHRQ Pub. No. 02-R0203. [Google Scholar]
- 29.California Healthcare Foundation. How ambulatory intensive care units can reduce costs and improve outcomes. http://www.chcf.org/publications/2011/05/ambulatory-intensive-caring-units.
- 30.Hempstead K, Delia D, Cantor JC, Nguyen T, Brenner J. The fragmentation of hospital use among a cohort of high utilizers: implications for emerging care coordination strategies for patients with multiple chronic conditions. Med Care. 2014;52(Suppl 3):S67–74. doi: 10.1097/MLR.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 31.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. 2014;174(4):535–543. doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 32.Zulman DM, Grant RW. Transforming Care for Complex Patients: Addressing Interconnected Medical, Social, and Behavioral Challenges. J Gen Intern Med. 2016;31(3):263–264. doi: 10.1007/s11606-015-3554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roux A, Katz M, Crews D, Ross D, NA Social and Behavioral Information in Electronic Health Records. American Journal of Preventive Medicine. 2015;49(6):980–983. doi: 10.1016/j.amepre.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 34.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities — Addressing Social Needs through Medicare and Medicaid. New England Journal of Medicine. 2016;374(1):8–11. doi: 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.