Abstract
Immunotherapies include various approaches, ranging from stimulating effector mechanisms to counteracting inhibitory and suppressive mechanisms, and creating a forum for discussing the most effective means of advancing these therapies through imaging is the focus of the newly formed Imaging in Cellular and Immune Therapies (ICIT) interest group within the World Molecular Imaging Society. Efforts are being made in the identification and validation of predictive biomarkers for a number of immunotherapies. Without predictive biomarkers, a considerable number of patients may receive treatments that have no chance of offering a benefit. This will reflect poorly on the field of immunotherapy and will yield false hopes in patients while at the same time contributing to significant cost to the healthcare system. This review summarizes the main strategies in cancer immune and cell-based therapies and discusses recent advances in imaging strategies aimed to improve cancer immunotherapy outcomes.
Key words: Cell-based therapy, Imaging, Immunotherapy
Introduction
Recently, immuno-based therapies have been found to provide lasting and curative benefits to patients who have previously had very few treatment options available to them. These immunotherapeutic approaches thereby have the potential to revolutionize cancer therapy and become an important part of comprehensive therapeutic approaches for treating many diseases including cancer. These therapies build on the primary function of the immune system to rid the body of threats, both “foreign”, such as bacterial and viral pathogens and “domestic”, such as cancer cells. Over the past several decades of cancer immunology research, there has been evidence that tumor cells are recognized by the native or genetically engineered adoptive immunity, but also that tumors can modify these responses and escape immune recognition [1]. Immune modulation in cancer treatment, therefore, refers to a range of approaches aimed at harnessing and enhancing the patient’s immune system and overcoming immune escape, to achieve tumor control, stabilization, and potential eradication of disease. This has led to the development of therapies that permit specific tumor destruction with minimal toxicity to normal tissue [2–6]. Such strategies also have the potential to prevent tumor recurrence because of the immune systems long-term memory. Within the World Molecular Imaging Society, we have constituted an interest group comprised of members of the society who share the common interest of fostering the use of imaging to advance and understand cellular and immune-based therapies. This Interest Group is called Imaging in Cellular and Immune Therapies (ICIT), and we present here a brief summary of the field and our efforts in the society to support developments in this important area of investigation.
Current Advances in Immune and Cell Therapies
The main categories of immunotherapies being developed include monoclonal antibodies, recombinant cytokines, cancer-specific, and other types of vaccines and adoptive immune cell transfer [3, 7, 8]. Several immunotherapies have been approved by the Food and Drug Administration (FDA), and others are being evaluated in pre-clinical and clinical trials. The field of immunotherapy for cancer has received a significant boost by the approval of several immunotherapies. These include immunostimulatory cytokines for the treatment of cancer, viral hepatitis and osteopetrosis (e.g., IL-2 [9], interferons [10, 11]). The autologous cellular vaccine, sipuleucel-T, has also recently been approved for the treatment of prostate cancer [12]. Perhaps the immunotherapies that have received the most attention are the immune checkpoint inhibitors that overcome immune escape. These target the anti-cytotoxic T lymphocyte-associated protein 4 (anti-CTLA-4) and the anti-programmed cell death protein/protein ligand 1 (anti-PD-1/PD-L1) with antibodies and are being used for the treatment of melanoma, lung cancer, renal cell carcinoma and head and neck tumors [13–16]. Other forms of immunotherapy including administration of ex vivo expanded tumor infiltrating lymphocytes (TILs), transgenic endogenous T cell receptor (TCR)- or chimeric antigen receptor (CAR)-grafted T cells have been successfully tested in clinical trials in patients with melanoma, B cell malignancies, mesothelioma, ovarian and prostate cancers and will likely get FDA approval in the near future [17–23]. This emerging collection of immune-based therapeutic approaches hold great promise for the treatment of cancer, but are also be adopted for many non-malignant conditions such as autoimmunity, infectious diseases, and immunodeficiencies [24–26].
At the moment, immunotherapy with checkpoint inhibitors provide a foundation for many of the combinatorial strategies [27] as it allows for enhancing an immune response against multiple cancers including tumors expressing weak antigens [28]. However, one of the main obstacles to the development of a successful immunotherapeutic approach is in identification and in vivo assessment of the most suitable antigen(s) to use. Molecular imaging reagents that target specific cancer antigens can help selecting patients that will likely respond to antigen-directed immunotherapies and will allow for early response assessment and prediction of treatment outcome by visualizing antigen distribution preceding tumor targeting with radioimmunotherapy, drug-immunoconjugates, or antigen-specific T lymphocytes [29–33].
Imaging as an Outcome Measure
A vital component of any cancer treatment is the objective assessment and monitoring of tumor response to anticancer therapy using imaging and specific response evaluation criteria. The response evaluation criteria in solid tumors (RECIST) was proposed in 2000, and this criterion is anatomic in nature and specifies the number of disease sites and their dynamics as the imaging metric for determining response (e.g., complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD)) [34]. However, clinical experience suggests that RECIST may be inadequate to cover the spectrum of imaging responses to immunotherapy since the determinants of increase in tumor size and/or the appearance of new lesions that often suggest treatment failure, might not be entirely applicable here. As observed in multiple studies, immunotherapy often demonstrates initial anatomical imaging changes that would be classified as disease progression, followed by radiological and clinical response suggesting therapeutic response [35, 36].
As immunotherapies continue to be developed and undergo testing in clinical trials, consideration needs to be given to the unique appearance of images that predict tumor responses. Such studies have found four distinct response patterns on imaging, all of which were associated with favorable survival: (a) shrinkage of baseline lesions without new lesions, which is consistent with RECIST; (b) durable SD followed by a slow, steady decline in total tumor burden in some patients; (c) response after initial increase in total tumor burden; and (d) response in the presence of new lesions [37–39]. These updated immune-related response criteria (IrRC) are defined as a way to incorporate imaging patterns observed with immunotherapy into the response assessment criteria including metabolic response to treatment assessed by 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) and positron emission tomography (PET) [40]. One of the aims of the ICIT Interest Group is to verify and validate these measures over a range of immune-based therapies, and to continue to develop new measures as new tools and technologies are developed for both treating and imaging cancer.
Imaging Biomarkers
One of the challenges of immunotherapy is that accurate and reproducible biomarkers that would allow treating physicians to select the patients most likely to respond have yet to be identified, vetted, and deployed. The potential of molecular imaging to detect these biomarkers and better stratify the patients for targeted therapies and interpreting their response to this novel treatment option cannot be overestimated. Currently, there is no single robust biomarker to identify the patients who will most likely benefit from these treatments, and as we advance precision medicine, it is likely that panels of biomarkers will be required for guiding therapy and assessing outcome. For example, PD-L1 expression levels have been suggested as a positive prognostic biomarker for patients undergoing immune checkpoint blockade therapy [41]. Following pathology-derived data, a number of PD-L1-specific radiotracers were developed that allowed for non-invasive assessment of tumor PD-L1 status in murine models, with the intent of predicting the efficacy of PD-1 checkpoint blockade [42–45]. However, studies have demonstrated the lack of clinical benefit in some patients treated with anti-PD-1 antibodies despite positive PD-L1 status of their tumors [46, 47]. Therefore, the levels of PD-L1 within the tumor microenvironment cannot, at present, be considered an optimal biomarker for patient selection until we can better reveal and understand the basic biology and mechanisms of action of check-point blockade.
There are certain challenges with [18F]FDG and [18F]FLT PET avidity as biomarkers in assessment of the efficacy of immunotherapy that include the difficulty of discriminating between viable tumor and the infectious or inflammatory processes associated with novel therapies [48, 49]. A number of new radiopharmaceuticals have been proposed and evaluated in pre-clinical and clinical studies aiming to distinguish rapidly proliferating immune cells invading the tumor or involved in any type of immune response. Several 18F–labeled nucleoside analogs, including 1-(2′-Deoxy-2′-[18F]fluoroarabinofuranosylcytosine (aka [18F]FAC) [50, 51], 2-chloro-2′-deoxy-2′-[(18)F]fluoro-9-β-d-arabinofuranosyl-adenine (aka [18F]CFA) [52, 53], and 2′-deoxy-2′-[18F]fluoro-9-β-D-arabinofuranosylguanine (aka [18F]AraG) [54] that are specific for key enzymes involved in T lymphocyte and other immune cell activation and proliferation, have been used for detecting location of activated T cells, monitoring transplant rejection, and graft–versus–host–disease and diagnosis and staging of auto–immune disorders. These new radiotracers can be early predictors of response and adverse reactions to immunotherapy measuring functional status of immune cells involved.
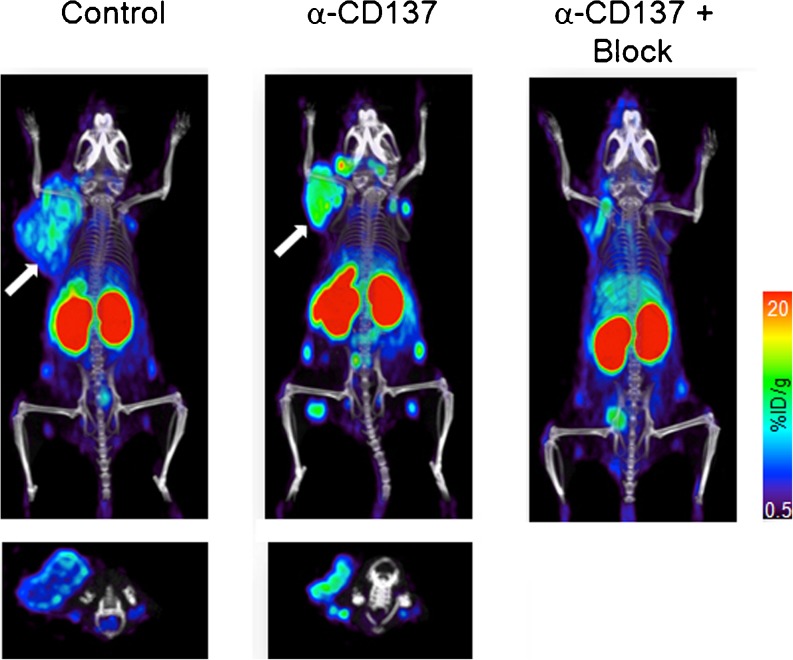
Another imaging approach that can directly visualize immune cells behavior is immuno-PET. In this approach, antibodies or antibody fragments are used to direct PET radionuclides to immune cells for detection, localization and typing. Immuno-PET has the potential to detect T cell subsets within tumors or lymphoid tissues and noninvasively monitor distribution and temporal dynamics of CD8 cytotoxic and CD4 helper T lymphocytes that participate in the inflammation and cytotoxic attack within tumors. Anti-CD8 full size antibodies and mini-bodies labeled with Cu-64, Zr-89, F-18, or I-124 showed excellent PET imaging and target specificity and importantly did not deplete CD8 T cells due to the absence of Fc function (Fig. 1) [55, 56]. Other targets include markers of immunostimulatory dendritic cells (MHC II, IDO1), chemokine ligands, and receptors (CXCR3,-4, CXCL9,-12 CCR5) as well as immunosuppressive neutrophils and macrophages (CD11b, CD47), which may downregulate T cell responses within tumors [57–61]. Examples of immuno-imaging targets and agents are summarized in Table 1.
Fig. 1.
Anti-CD8 immuno-PET in subcutaneous colorectal immunotherapy model. CT26 murine colon cancer-grafted mice were treated with CD137-agonistic Abs: CD137-treated, CD137-treated/CD8-blocked mice, and control mice (no anti-CD137 therapy) were injected with 89Zr-malDFO-169 cDb and immuno-PET images were acquired at 22 h postinjection. Note the presence of increased CD8+ tumor-infiltrating lymphocytes within the tumor in CD137-treated animal (white arrow, adapted from [56]).
Table 1.
Immuno-imaging targets and agents
| Immune cell compartment/function | Molecular target | Imaging agent | Modality | Stage of development |
|---|---|---|---|---|
| Tumor/Tumor immunosuppressive microenvironment | PD-L1 | [89Zr]/[64Cu]Anti-PD-L1-Ab/peptide [43−45] ([89Zr]MPDL3280A) [NCT02453984] | PET | Clinical |
| Immune cell proliferation | Deoxycytidine kinase | L-[18F]FAC, −CFA [51, 53] | PET | Clinical |
| T lymphocyte activation | Deoxyguanosine kinase | [18F]AraG [54] | PET | Clinical |
| Cytotoxic T lymphocytes | CD8 | [89Zr]/[64Cu]Anti-CD8-Ab [55, 56] ([89Zr]IAB22M2C) | PET | Clinical |
| Macrophages | N/A | Ferumoxytol [62] | MRI | Clinical |
| T lymphocyte inhibition | CTLA-4 | [64Cu]Anti-CTLA-4-Ab [63] | PET | Pre-clinical |
| T lymphocyte inhibition | PD-1 | [64Cu]Anti-PD-1-Ab [45] | PET | Pre-clinical |
| Macrophages (TAMs) | CD47 | [89Zr]Anti-CD47-Ab [58] | PET | Pre-clinical |
| Neutrophils | CD11b/MHC-II | [18F]/[64Cu]Anti-CD11b/MHC-II-Ab [57] | PET | Pre-clinical |
| Transgeneic T cells | Transgeneic TCR | [89Zr]/[64Cu]Anti–TCR-Ab [64, 65] | PET | Pre-clinical |
| T lymphocyte trafficking | CXCR4 | [64Cu]AMD3100 [60] | PET | Pre-clinical |
| Macrophages (TAMs) | B7-H3 | MicrobubblesAnti-B7-H3 [66] | Ultrasound | Pre-clinical |
N/A not available
Imaging of Immune Cells
Recent advances in the field of adoptive immunotherapy require the ability to monitor the trafficking, targeting, and activation/proliferation of the administered cells. The application of labeling molecules and genetic reporter systems (gene/probe combinations) together with non-invasive imaging modalities, such as PET, SPECT, and MRI, has shown the potential for monitoring T cells in clinical settings [67–69]. In-111, in particular, found a wide clinical application in oncology as an imaging agent for monitoring immunotherapy with tumor-infiltrating lymphocytes and granulocytes administration [70, 71]. However, imaging approaches that require ex vivo cell labeling encompass a number of limitations such as radiotoxicity and limited period of monitoring as a result of cell division, biological clearance and radiolabel decay [72, 73].
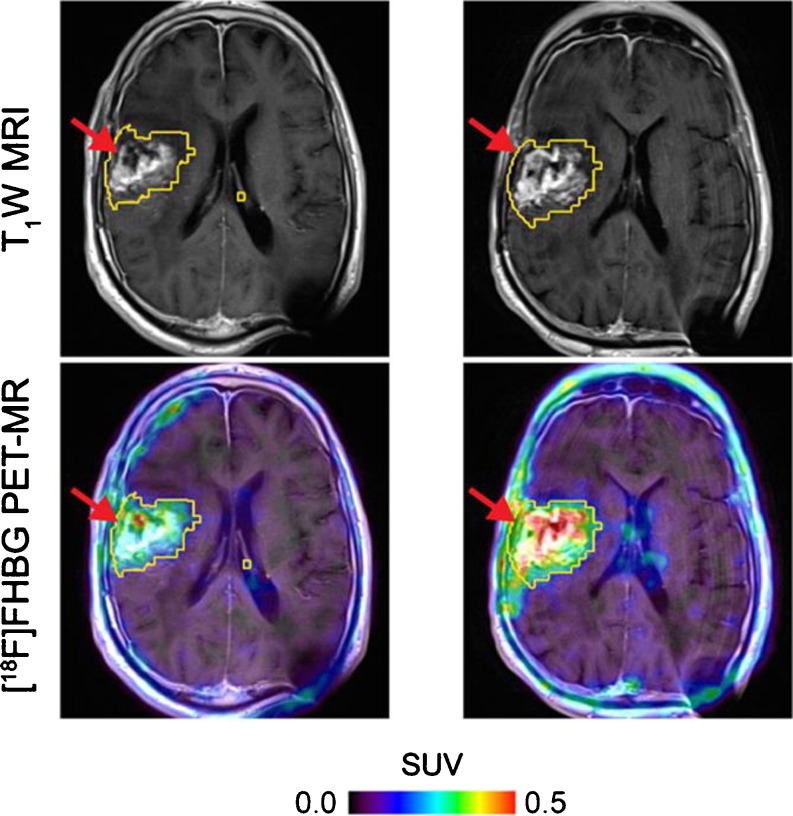
Stable genetic labeling of adoptively transferred cells with reporter genes (genes encoding easily detectable proteins not normally expressed by the cells) has been used to circumvent the temporal limitations of ex vivo radiolabeling. Several reporter gene/reporter probe combinations have been used in the majority of the seminal studies on imaging immune cell trafficking including ex vivo expanded cytotoxic lymphocytes (CTLs) and CAR-grafted Tcells by optical and nuclear techniques (e.g., luciferases, fluorescent proteins, HSV1tk, respectively [67, 68, 74–79]) including imaging in humans (Fig. 2) [80]. In addition, reporter gene imaging allows for visualization of T lymphocyte functional status following T cell receptor engagement by using inducible reporter systems sensitive to T cell activation [81]. This circumstance makes this imaging approach clinically valuable, as it allows for monitoring functional status of adoptively transferred immune cells in cancer patients as well as in bone marrow and stem cell recipients. The major impediment to the translation of viral- and bacterial-derived reporter gene imaging approaches into clinical practice is the immunogenicity of these non-human derived reporter proteins. However, there has been a recent focus on human reporter systems to avoid the potential risk of generating an immunological reaction to xenogeneic (non-human) reporter proteins thus allowing for long-term repetitive visualization of adoptively transferred immune cells. These include human-derived sodium iodide symporter (hNIS), norepinephrine transporter (hNET), somatostatin receptor 2 (hSSTR2), truncated, and mutated mitochondrial thymidine kinase type 2 (h∆TK2, h∆TK2DM) and deoxycytidine kinase (hdCKDM, hdCK3M), ferritin reporter, and transferrin receptor [82–89]. Some reporter genes may have the added benefit of suicide gene potential. This provides a mechanism for elimination of rogue reporter gene-expressing immune cells with clinically approved chemo- and radiotherapeutics (e.g., HSV1tk/ganciclovir, hdCKDM/gemcitabine, hNIS/I-131, hNET/[131I]MIBG [90–93]).
Fig. 2.
Tumor-directed CAR-T cell PET imaging with [18F]FHBG. [18F]FHBG PET imaging was performed in a patient with a recurrent right frontoparietal glioblastoma a before and b 1 week after tumor-specific CAR-T cell infusions. Allogeneic CAR-T cells and IL-2 were injected intratumorally (red arrows). Tumor recurrence was monitored by T1-weighted (T1W) MRI (top panels). [18F]FHBG PET images were fused with MR images (bottom panels), and three-dimensional (3D) volumes of interest were drawn using a 50 % [18F]FHBG SUVmaxthreshold, outlined in yellow (adapted from [80]).
Principles of immuno-PET can be applied to imaging adoptively transferred cells by administrating anti-antigen-specific transgenic TCR radiolabeled antibodies. Antigen-specific TCR transgenic T cells were successfully visualized with PET using 89Zr-89 labeled anti–TCRmu-F(ab')2 fragment [64] and [64Cu]DOTA–modified cOVA-TCR–specific mAbs [65].
The potential of imaging for quantifying cell signals in a region of anatomical interest (ROI) provides a unique opportunity to estimate the absolute number of injected labeled cells at the target site. Several studies determined the correlation of PET signal to cell number and characterized the cellular limit of detection for PET imaging using human and mouse T cells transduced with different human and non-human reporters with a limit of detection below 105 cells in a region of interest of 0.1 ml volume [85, 87, 94]. This level of sensitivity enables effective assessment of cell localization at target sites and assessment of off target homing in vivo and will be useful in guiding development of novel immune therapies.
Conclusion
As immunotherapies continue to be developed and undergo testing in clinical trials, consideration needs to be given to the differences observed in response following immunotherapy, and as a community, we need to standardize these measures and ensure uniformity among studies. While optimal combinations of treatment schemas still need to be determined, significant efforts have to be made in the identification and validation of predictive biomarkers that can be used alone or in combination in imaging, but also in conjunction with blood and tissue markers ex vivo. It is imperative that we as a community of imaging scientists interested in immunotherapy be proactive in advancing this field.
Compliance with Ethical Standards
Conflict of Interest
The author declares that he has no conflict of interest.
References
- 1.Whiteside TL, Demaria S, Rodriguez-Ruiz ME, et al. Emerging opportunities and challenges in cancer immunotherapy. Clin Cancer Res. 2016;22:1845–1855. doi: 10.1158/1078-0432.CCR-16-0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menon S, Shin S, Dy G (2016) Advances in cancer immunotherapy in solid tumors. Cancers (Basel) 8: doi:10.3390/cancers8120106. [DOI] [PMC free article] [PubMed]
- 4.Geyer MB, Brentjens RJ. Review: Current clinical applications of chimeric antigen receptor (CAR) modified T cells. Cytotherapy. 2016;18:1393–1409. doi: 10.1016/j.jcyt.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D'Souza NM, Fang P, Logan J, et al. Combining radiation therapy with immune checkpoint blockade for central nervous system malignancies. Front Oncol. 2016;6:212. doi: 10.3389/fonc.2016.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes PE, Caenepeel S, Wu LC. Targeted therapy and checkpoint immunotherapy combinations for the treatment of cancer. Trends Immunol. 2016;37:462–476. doi: 10.1016/j.it.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Kandalaft LE, Powell DJ, Singh N, Coukos G. Immunotherapy for ovarian cancer: what’s next? J Clin Oncol. 2011;29:925–933. doi: 10.1200/JCO.2009.27.2369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabado RL, Balan S, Bhardwaj N. Dendritic cell-based immunotherapy. Cell Res. 2017;27:74–95. doi: 10.1038/cr.2016.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millet A, Martin AR, Ronco C, et al. Metastatic melanoma: insights into the evolution of the treatments and future challenges. Med Res Rev. 2017;37:98–148. doi: 10.1002/med.21404. [DOI] [PubMed] [Google Scholar]
- 10.Hayes CN, Chayama K. Interferon stimulated genes and innate immune activation following infection with hepatitis B and C viruses. J Med Virol. 2017;89:388–396. doi: 10.1002/jmv.24659. [DOI] [PubMed] [Google Scholar]
- 11.Razaghi A, Owens L, Heimann K. Review of the recombinant human interferon gamma as an immunotherapeutic: Impacts of production platforms and glycosylation. J Biotechnol. 2016;240:48–60. doi: 10.1016/j.jbiotec.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Hu R, George DJ, Zhang T. What is the role of sipuleucel-T in the treatment of patients with advanced prostate cancer? An update on the evidence. Ther Adv Urol. 2016;8:272–278. doi: 10.1177/1756287216645314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodi FS, Chesney J, Pavlick AC, et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016;17:1558–1568. doi: 10.1016/S1470-2045(16)30366-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du L, Herbst RS, Morgensztern D Immunotherapy in lung cancer. Hematol Oncol Clin North Am 31:131–141 [DOI] [PubMed]
- 15.Donin NM, Lenis AT, Holden A, et al. Immunotherapy for the treatment of Urothelial carcinoma. J Urol. 2017;197:14–22. doi: 10.1016/j.juro.2016.02.3005. [DOI] [PubMed] [Google Scholar]
- 16.Msaouel P, Massarelli E. Immune checkpoint therapy in head and neck cancers. Cancer J. 2016;22:108–116. doi: 10.1097/PPO.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 17.Sadelain M. Chimeric antigen receptors: driving immunology towards synthetic biology. Curr Opin Immunol. 2016;41:68–76. doi: 10.1016/j.coi.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson LA, June CH. Driving gene-engineered T cell immunotherapy of cancer. Cell Res. 2017;27:38–58. doi: 10.1038/cr.2016.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang JC, Rosenberg SA. Adoptive T-cell therapy for cancer. Adv Immunol. 2016;130:279–294. doi: 10.1016/bs.ai.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anurathapan U, Leen AM, Brenner MK, Vera JF. Engineered T cells for cancer treatment. Cytotherapy. 2014;16:713–733. doi: 10.1016/j.jcyt.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JH, Geyer MB, Brentjens RJ. CD19-targeted CAR T-cell therapeutics for hematologic malignancies: interpreting clinical outcomes to date. Blood. 2016;127:3312–3320. doi: 10.1182/blood-2016-02-629063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koneru M, O’Cearbhaill R, Pendharkar S, et al. A phase I clinical trial of adoptive T cell therapy using IL-12 secreting MUC-16(ecto) directed chimeric antigen receptors for recurrent ovarian cancer. J Transl Med. 2015;13:102. doi: 10.1186/s12967-015-0460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morello A, Sadelain M, Adusumilli PS. Mesothelin-targeted CARs: driving T cells to solid tumors. Cancer Discov. 2016;6:133–146. doi: 10.1158/2159-8290.CD-15-0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Northrup L, Christopher MA, Sullivan BP, Berkland C. Combining antigen and immunomodulators: Emerging trends in antigen-specific immunotherapy for autoimmunity. Adv Drug Deliv Rev. 2016;98:86–98. doi: 10.1016/j.addr.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 25.Tashiro H, Brenner MK. Immunotherapy against cancer-related viruses. Cell Res. 2017;27:59–73. doi: 10.1038/cr.2016.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLaughlin LP, Bollard CM, Keller M. Adoptive T cell immunotherapy for patients with primary immunodeficiency disorders. Curr Allergy Asthma Rep. 2017;17:3. doi: 10.1007/s11882-017-0669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vilgelm AE, Johnson DB, Richmond A. Combinatorial approach to cancer immunotherapy: strength in numbers. J Leukoc Biol. 2016;100:275–290. doi: 10.1189/jlb.5RI0116-013RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Desrichard A, Snyder A, Chan TA. Cancer neoantigens and applications for immunotherapy. Clin Cancer Res. 2016;22:807–812. doi: 10.1158/1078-0432.CCR-14-3175. [DOI] [PubMed] [Google Scholar]
- 29.Haberkorn U, Eder M, Kopka K, et al. New strategies in prostate cancer: prostate-specific membrane antigen (PSMA) ligands for diagnosis and therapy. Clin Cancer Res. 2016;22:9–15. doi: 10.1158/1078-0432.CCR-15-0820. [DOI] [PubMed] [Google Scholar]
- 30.Sharma SK, Sevak KK, Monette S, et al. Preclinical 89Zr immuno-PET of high-grade serous ovarian cancer and lymph node metastasis. J Nucl Med. 2016;57:771–776. doi: 10.2967/jnumed.115.167072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pandit-Taskar N, O'Donoghue JA, Durack JC, et al. A phase I/II study for analytic validation of 89Zr-J591 ImmunoPET as a molecular imaging agent for metastatic prostate cancer. Clin Cancer Res. 2015;21:5277–5285. doi: 10.1158/1078-0432.CCR-15-0552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rylova SN, Del Pozzo L, Klingeberg C, et al. Immuno-PET imaging of CD30-positive lymphoma using 89Zr-Desferrioxamine-labeled CD30-specific AC-10 antibody. J Nucl Med. 2016;57:96–102. doi: 10.2967/jnumed.115.162735. [DOI] [PubMed] [Google Scholar]
- 33.Kramer K, Kushner BH, Modak S, et al. Compartmental intrathecal radioimmunotherapy: results for treatment for metastatic CNS neuroblastoma. J Neuro-Oncol. 2010;97:409–418. doi: 10.1007/s11060-009-0038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Therasse P, Arbuck SG, Eisenhauer EA, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of cancer, National Cancer Institute of the United States, National Cancer Institute of Canada J Natl Cancer Inst 92: 205–216. [DOI] [PubMed]
- 35.Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li XD, Ji M, Zheng X, et al. Evaluation of tumor response to cytokine-induced killer cells therapy in malignant solid tumors. J Transl Med. 2014;12:215. doi: 10.1186/s12967-014-0215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolchok JD, Hoos A, O'Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–7420. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 38.Khoja L, Kibiro M, Metser U, et al. Patterns of response to anti-PD-1 treatment: an exploratory comparison of four radiological response criteria and associations with overall survival in metastatic melanoma patients. Br J Cancer. 2016;115:1186–1192. doi: 10.1038/bjc.2016.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishino M. Immune-related response evaluations during immune-checkpoint inhibitor therapy: establishing a “common language” for the new arena of cancer treatment. J Immunother Cancer. 2016;4:30. doi: 10.1186/s40425-016-0134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Braschi-Amirfarzan M, Tirumani SH, Hodi FS, Jr, Nishino M. Immune-checkpoint inhibitors in the era of precision medicine: what radiologists should know. Korean J Radiol. 2017;18:42–53. doi: 10.3348/kjr.2017.18.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patel SP, Kurzrock R. PD-L1 expression as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther. 2015;14:847–856. doi: 10.1158/1535-7163.MCT-14-0983. [DOI] [PubMed] [Google Scholar]
- 42.Mayer AT, Natarajan A, Gordon S, et al. Practical ImmunoPET radiotracer design considerations for human immune checkpoint imaging. J Nucl Med. 2016 doi: 10.2967/jnumed.116.177659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chatterjee S, Lesniak WG, Miller MS, et al. Rapid PD-L1 detection in tumors with PET using a highly specific peptide. Biochem Biophys Res Commun. 2017;483:258–263. doi: 10.1016/j.bbrc.2016.12.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lesniak WG, Chatterjee S, Gabrielson M, et al. PD-L1 detection in tumors using [(64)Cu]Atezolizumab with PET. Bioconjug Chem. 2016;27:2103–2110. doi: 10.1021/acs.bioconjchem.6b00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hettich M, Braun F, Bartholomä MA, et al. High-resolution PET imaging with therapeutic antibody-based PD-1/PD-L1 checkpoint tracers. Theranostics. 2016;6:1629–1640. doi: 10.7150/thno.15253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gibney GT, Weiner LM, Atkins MB. Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 2016;17:e542–e551. doi: 10.1016/S1470-2045(16)30406-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang X, Teng F, Kong K, Jinming Y. PD-L1 expression in human cancers and its association with clinical outcomes. Onco Targets Ther. 2016;9:5023–5039. doi: 10.2147/OTT.S105862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Waarde A, Elsinga PH. Proliferation markers for the differential diagnosis of tumor and inflammation. Curr Pharm Des. 2008;14:3326–3339. doi: 10.2174/138161208786549399. [DOI] [PubMed] [Google Scholar]
- 49.Basu S, Kumar R, Alavi A. PET and PET-CT imaging in infection and inflammation: its critical role in assessing complications related to therapeutic interventions in patients with cancer. Indian J Cancer. 2010;47:371–379. doi: 10.4103/0019-509X.73562. [DOI] [PubMed] [Google Scholar]
- 50.Nair-Gill E, Wiltzius SM, Wei XX, et al. PET probes for distinct metabolic pathways have different cell specificities during immune responses in mice. J Clin Invest. 2010;120:2005–2015. doi: 10.1172/JCI41250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schwarzenberg J, Radu CG, Benz M, et al. Human biodistribution and radiation dosimetry of novel PET probes targeting the deoxyribonucleoside salvage pathway. Eur J Nucl Med Mol Imaging. 2011;38:711–721. doi: 10.1007/s00259-010-1666-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim W, Le TM, Wei L, et al. [18F]CFA as a clinically translatable probe for PET imaging of deoxycytidine kinase activity. Proc Natl Acad Sci U S A. 2016;113:4027–4032. doi: 10.1073/pnas.1524212113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barrio M, Spick C, Radu CG, et al. Human biodistribution and radiation dosimetry of 18F-CFA, a PET probe targeting the deoxyribonucleoside salvage pathway. J Nucl Med. 2016 doi: 10.2967/jnumed.116.182394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Namavari M, Chang YF, Kusler B, et al. Synthesis of 2′-deoxy-2′-[18F]fluoro-9-beta-D-arabinofuranosylguanine: a novel agent for imaging T-cell activation with PET. Mol Imaging Biol. 2011;13:812–818. doi: 10.1007/s11307-010-0414-x. [DOI] [PubMed] [Google Scholar]
- 55.Tavare R, McCracken MN, Zettlitz KA, et al. Engineered antibody fragments for immuno-PET imaging of endogenous CD8+ T cells in vivo. Proc Natl Acad Sci U S A. 2014;111:1108–1113. doi: 10.1073/pnas.1316922111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tavare R, Escuin-Ordinas H, Mok S, et al. An effective immuno-PET imaging method to monitor CD8-dependent responses to immunotherapy. Cancer Res. 2016;76:73–82. doi: 10.1158/0008-5472.CAN-15-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rashidian M, Keliher EJ, Bilate AM, et al. Noninvasive imaging of immune responses. Proc Natl Acad Sci U S A. 2015;112:6146–6151. doi: 10.1073/pnas.1502609112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zheleznyak A, Ikotun OF, Dimitry J, et al. Imaging of CD47 expression in xenograft and allograft tumor models. Mol Imaging. 2013;12:1–10. doi: 10.2310/7290.2013.00069. [DOI] [PubMed] [Google Scholar]
- 59.Xie L, Maeda J, Kumata K, et al. (2015) Development of 1-N-(11)C-Methyl-L- and -D-Tryptophan for pharmacokinetic imaging of the immune checkpoint inhibitor 1-Methyl-Tryptophan. Sci Rep 5: doi:10.1038/srep16417 [DOI] [PMC free article] [PubMed]
- 60.Nimmagadda S, Pullambhatla M, Stone K, et al. Molecular imaging of CXCR4 receptor expression in human cancer xenografts with [64Cu]AMD3100 positron emission tomography. Cancer Res. 2010;70:3935–3944. doi: 10.1158/0008-5472.CAN-09-4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Luehmann HP, Pressly ED, Detering L, et al. PET/CT imaging of chemokine receptor CCR5 in vascular injury model using targeted nanoparticle. J Nucl Med. 2014;55:629–634. doi: 10.2967/jnumed.113.132001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schmitz SA, Taupitz M, Wagner S et al (2001) Magnetic resonance imaging of atherosclerotic plaques using superparamagnetic iron oxide particles. J Magn Reson Imaging 14:355–61 [DOI] [PubMed]
- 63.Higashikawa K, Yagi K, Watanabe K et al (2014) 64Cu-DOTA-anti-CTLA-4 mAb enabled PET visualization of CTLA-4 on the T-cell infiltrating tumor tissues. PLoS One 9:109866 [DOI] [PMC free article] [PubMed]
- 64.Mall S, Yusufi N, Wagner R, et al. Immuno-PET imaging of engineered human T cells in tumors. Cancer Res. 2016;76:4113–4123. doi: 10.1158/0008-5472.CAN-15-2784. [DOI] [PubMed] [Google Scholar]
- 65.Griessinger CM, Mauer A, Kesenheimer C, et al. 64Cu antibody-targeting of the T-cell receptor and subsequent internalization enables in vivo tracking of lymphocytes by PET. Proc Natl Acad Sci U S A. 2015;112:1161–1166. doi: 10.1073/pnas.1418391112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bachawal SV, Jensen KC, Wilson KE et al (2015) Breast cancer detection by B7-H3-targeted ultrasound molecular imaging. Cancer Res 75:2501-9 [DOI] [PMC free article] [PubMed]
- 67.Koehne G, Doubrovin M, Doubrovina E, et al. Serial in vivo imaging of the targeted migration of human HSV-TK-transduced antigen-specific lymphocytes. Nat Biotechnol. 2003;21:405–413. doi: 10.1038/nbt805. [DOI] [PubMed] [Google Scholar]
- 68.Dubey P, Su H, Adonai N, et al. Quantitative imaging of the T cell antitumor response by positron-emission tomography. Proc Natl Acad Sci U S A. 2003;100:1232–1237. doi: 10.1073/pnas.0337418100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kircher MF, Allport JR, Graves EE, et al. In vivo high resolution three-dimensional imaging of antigen-specific cytotoxic T-lymphocyte trafficking to tumors. Cancer Res. 2003;63(20):6838–6846. [PubMed] [Google Scholar]
- 70.Thakur ML, Seifert CL, Madsen MT, et al. Neutrophil labeling: problems and pitfalls. Semin Nucl Med. 1984;14:107–117. doi: 10.1016/S0001-2998(84)80024-0. [DOI] [PubMed] [Google Scholar]
- 71.Fisher B, Packard BS, Read EJ, et al. Tumor localization of adoptively transferred indium-111 labeled tumor infiltrating lymphocytes in patients with metastatic melanoma. J Clin Oncol. 1989;7:250–261. doi: 10.1200/JCO.1989.7.2.250. [DOI] [PubMed] [Google Scholar]
- 72.Kircher MF, Gambhir SS, Grimm J. Noninvasive cell-tracking methods. Nat Rev Clin Oncol. 2011;8:677–688. doi: 10.1038/nrclinonc.2011.141. [DOI] [PubMed] [Google Scholar]
- 73.Zanzonico P, Koehne G, Gallardo HF, et al. [131I]FIAU labeling of genetically transduced, tumor-reactive lymphocytes: cell-level dosimetry and dose-dependent toxicity. Eur J Nucl Med Mol Imaging. 2006;33:988–997. doi: 10.1007/s00259-005-0057-3. [DOI] [PubMed] [Google Scholar]
- 74.Hardy J, Edinger M, Bachmann MH, et al. Bioluminescence imaging of lymphocyte trafficking in vivo. Exp Hematol. 2001;29:1353–1360. doi: 10.1016/S0301-472X(01)00756-1. [DOI] [PubMed] [Google Scholar]
- 75.Stephan MT, Ponomarev V, Brentjens RJ, et al. T cell-encoded CD80 and 4-1BBL induce auto- and transcostimulation, resulting in potent tumor rejection. Nat Med. 2007;13:1440–1449. doi: 10.1038/nm1676. [DOI] [PubMed] [Google Scholar]
- 76.Dobrenkov K, Olszewska M, Likar Y, et al. Monitoring the efficacy of adoptively transferred prostate cancer-targeted human T lymphocytes with PET and bioluminescence imaging. J Nucl Med. 2008;49:1162–1170. doi: 10.2967/jnumed.107.047324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim Y, Dubey P, Ray P, et al. Multimodality imaging of lymphocytic migration using lentiviral-based transduction of a tri-fusion reporter gene. Mol Imaging Biol. 2004;6:331–340. doi: 10.1016/j.mibio.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 78.Dotti G, Tian M, Savoldo B, et al. Repetitive noninvasive monitoring of HSV1-tk-expressing T cells intravenously infused into nonhuman primates using positron emission tomography and computed tomography with 18F-FEAU. Mol Imaging. 2009;8:230–237. [PMC free article] [PubMed] [Google Scholar]
- 79.Singh H, Najjar AM, Olivares S, et al. PET imaging of T cells derived from umbilical cord blood. Leukemia. 2009;23:620–622. doi: 10.1038/leu.2008.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Keu KV, Witney TH, Yaghoubi S, et al. (2017) Reporter gene imaging of targeted T cell immunotherapy in recurrent glioma. Sci Transl Med 9. DOI: 10.1126/scitranslmed.aag2196 [DOI] [PMC free article] [PubMed]
- 81.Ponomarev V, Doubrovin M, Lyddane C, et al. Imaging TCR-dependent NFAT-mediated T-cell activation with positron emission tomography in vivo. Neoplasia. 2001;3:480–488. doi: 10.1038/sj.neo.7900204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Likar Y, Zurita J, Dobrenkov K, et al. A new pyrimidine-specific reporter gene: a mutated human deoxycytidine kinase suitable for PET during treatment with acycloguanosine-based cytotoxic drugs. J Nucl Med. 2010;51:1395–1403. doi: 10.2967/jnumed.109.074344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vedvyas Y, Shevlin E, Zaman M, et al. Longitudinal PET imaging demonstrates biphasic CAR T cell responses in survivors. JCI Insight. 2016;1:e90064. doi: 10.1172/jci.insight.90064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McCracken MN, Vatakis DN, Dixit D, et al. Noninvasive detection of tumor-infiltrating T cells by PET reporter imaging. J Clin Invest. 2015;125:1815–1826. doi: 10.1172/JCI77326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Moroz MA, Zhang H, Lee J, et al. Comparative analysis of T cell imaging with human nuclear reporter genes. J Nucl Med. 2015;56:1055–1060. doi: 10.2967/jnumed.115.159855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Campbell DO, Yaghoubi SS, Su Y, et al. Structure-guided engineering of human thymidine kinase 2 as a positron emission tomography reporter gene for enhanced phosphorylation of non-natural thymidine analog reporter probe. J Biol Chem. 2012;287:446–454. doi: 10.1074/jbc.M111.314666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Doubrovin MM, Doubrovina ES, Zanzonico P, et al. In vivo imaging and quantitation of adoptively transferred human antigen-specific T cells transduced to express a human norepinephrine transporter gene. Cancer Res. 2007;67:11959–11969. doi: 10.1158/0008-5472.CAN-07-1250. [DOI] [PubMed] [Google Scholar]
- 88.Gilad AA, Winnard PT, van Zijl P, Bulte JWF. Developing MR reporter genes: promises and pitfalls. NMR Biomed. 2007;20:275–290. doi: 10.1002/nbm.1134. [DOI] [PubMed] [Google Scholar]
- 89.Vandsburger MH, Radoul M, Cohen B, Neeman M. MRI reporter genes: applications for imaging of cell survival, proliferation, migration and differentiation. NMR Biomed. 2013;26:872–884. doi: 10.1002/nbm.2869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Greco R, Oliveira G, Stanghellini MTL, et al. (2015) Improving the safety of cell therapy with the TK-suicide gene. Front Pharmacol 6: doi:10.3389/fphar.2015.00095 [DOI] [PMC free article] [PubMed]
- 91.Lee JT, Zhang H, Moroz MA, et al. Comparative analysis of human nucleoside kinase-based reporter systems for PET imaging. Mol Imaging Biol. 2017;19:100–108. doi: 10.1007/s11307-016-0981-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kim YH, Youn H, Na J, et al. Codon-optimized human sodium iodide symporter (opt-hNIS) as a sensitive reporter and efficient therapeutic gene. Theranostics. 2015;5:86–96. doi: 10.7150/thno.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Streby KA, Shah N, Ranalli MA, et al. Nothing but NET: a review of norepinephrine transporter expression and efficacy of 131I-mIBG therapy. Pediatr Blood Cancer. 2015;62:5–11. doi: 10.1002/pbc.25200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Su H, Forbes A, Gambhir SS, Braun J. Quantitation of cell number by a positron emission tomography reporter gene strategy. Mol Imaging Biol. 2004;6:139–148. doi: 10.1016/j.mibio.2004.02.001. [DOI] [PubMed] [Google Scholar]