Highlights
-
•
Splenic tumors are not common, many can have minimal to no symptoms, and they can be found incidentally.
-
•
Splenic tumors can be primary or metastatic. They can be benign or malignant.
-
•
Splenic cysts can be infectious, traumatic or congenital.
-
•
Epidermoid splenic cysts may not always present in a classic fashion on imaging, making diagnosis challenging.
-
•
Many splenic masses and complex cysts would require surgical pathological diagnosis.
Keywords: Epidermoid cyst of spleen, Splenic cyst, Splenic tumor, Imaging of splenic epidermoid cyst, Case report
Abstract
Introduction
Splenic tumors are rare and are either primary or secondary, benign or malignant. Most have none to minimal symptomatology and are found incidentally. Splenic cysts can be infectious, congenital, or traumatic. Epidermoid cysts and parasitic cysts are examples of primary cysts and usually have a classic presentation on imaging. Despite advanced imaging modalities and patient's clinical presentation, it can be difficult to diagnose an epidermoid cyst without histological examination. The purpose of this paper is to discuss typical findings of primary splenic cysts on imaging, but how they may differ in appearance.
Presentation of case
51 year old female who presented with vague abdominal discomfort and was found to have a large splenic mass with cystic components on imaging which did not demonstrate a typical primary splenic cyst appearance. Patient underwent an uneventful hand-assisted laparoscopic total splenectomy and had an uneventful recovery with histopathology revealing an epidermoid splenic cyst.
Conclusion
Primary splenic cysts are difficult to diagnose and differentiate with imaging alone. They have a variable presentation and can present like as a cystic mass. It is important to include them in the differential diagnosis of splenic masses since histopathology is the final determinant of the diagnosis.
1. Introduction
Splenic cysts are rare and are either primary or secondary. Primary cysts have a lined epithelium and secondary cyst could be secondary to trauma. Epidermoid splenic cysts are example of primary congenital cysts that contain an epithelial lining, unlike secondary cysts, which are composed of fibrous tissues [1], [2]. Patients usually do not present with specific symptoms if the cyst is small. When the cyst is large they have nonspecific abdominal symptoms like pain, nausea, or a palpable mass usually in the left upper quadrant [2]. Epidermoid cysts and parasitic cysts are examples of primary cysts and usually have a classic presentation on imaging. Despite imaging modalities and the patient’s history, it can be difficult to diagnose an epidermoid cyst without a histological examination. The purpose of this paper is to discuss variable and atypical radiological presentation of primary splenic cysts including epidermoid cysts.
2. Case presentation
A 51-year-old female presented to the ED using private transportation with complaints of left upper quadrant abdominal pain, nausea and vomiting for a couple days. Patient had been having short episodes of dull generalized abdominal pain for 6 months. Patient denied any precipitating events, trauma or travel. She had significant medical history of hypertension, GERD, and hyperlipidemia with a BMI of 37.5 and no previous surgical history. Patient had quit smoking cigarettes two years prior, does not drink alcohol or use any illicit drugs. Physical exam was significant to being mildly tender to palpation over her left upper quadrant. Vitals, Complete Blood Count, Basic Metabolic Panel, Liver Function Tests, and Urine analysis were all within normal limits.
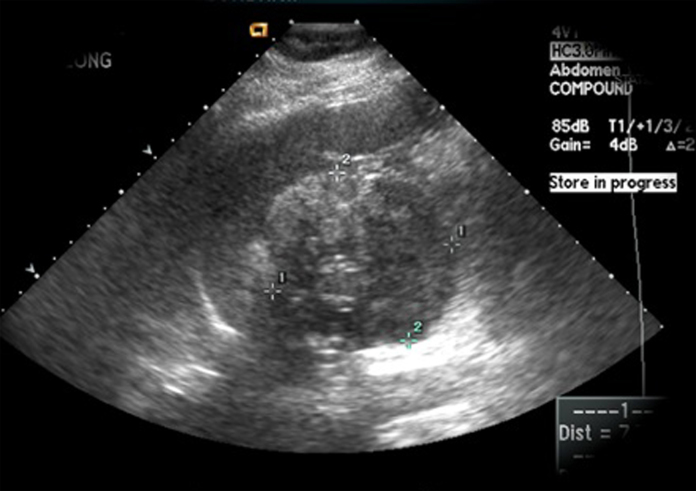
Abdominal ultrasound (Fig. 1) visualized a 7.7 cm complex mass in the medial aspect of the spleen. Enhanced-contrast abdominal computed tomography (CT) (Fig. 2) revealed a hypodense cystic mass in the medial aspect of the spleen measuring 10.4 cm × 8.2 cm with a Hounsfield attenuation of 15; containing multiple foci of fat with Hounsfield attenuation of −102. Patient was assumed to have a confined cystic tumor of unknown etiology without any acute complications at this point.
Fig. 1.
Ultrasound Appearance of Splenic Mass.
Fig. 2.
Enhanced CT scan appearance of Splenic Mass.
Patient felt better in the emergency department and wished to have outpatient follow. She followed up in the surgery clinic. After long discussion with the patient with this large cystic mass of the spleen of unknown pathology, Splenectomy was offered to the patient. She gave informed consent. She received standard splenectomy vaccinations prior to surgery. She underwent uneventful laparoscopic hand-assisted splenectomy 6 weeks after presentation to the ED. Surgery and hospital stay were uneventful and was discharged Post-operative day 3. She continued to have an uneventful recovery on follow-up with no recurrence of painful symptoms.
3. Pathology
On gross examination of the spleen (Fig. 3, Fig. 4), it weighed 404 g, and was 17 × 11 × 5 cm in dimensions and was partially cystic. 11 × 10 × 7 cm smooth walled yellow tan cyst was present.
Fig. 3.
Gross Surgical Pathology of Splenectomy with Tumor.
Fig. 4.

Pathological Specimen.
On microscopic examination, sections demonstrated unremarkable splenic parenchyma and cyst walls lined by stratified squamous epithelium. Immunohistochemical stains demonstrated an adequate distribution of CD20+ B-lymphocytes and CD3+ T-lymphocytes. Pathological diagnosis indicated a splenic epidermoid cyst.
4. Discussion
Splenic masses can be primary or secondary neoplasms. They could be Benign or malignant. Examples of primary malignant neoplasms involving the spleen are lymphomas and angiosarcomas. Examples of primary benign neoplasms involving the spleen include haemangiomas, lymphangiomas, angiomas and splenic mesenchymal tumors such as lipomas, angiomyolipomas, fibromas, fibrosarcomas, and leiomyosarcomas. Splenic cysts are also rare. They could be a pseudocyst secondary to trauma or a true cyst, which might be infectious or congenital such as an epidermoid cyst.
Epidermoid splenic cysts are primary congenital cysts that contain an epithelial lining, unlike secondary cysts which are composed of fibrous tissues [1], [2]. Patients usually do not present with specific symptoms if the cyst is small, and when the cyst is large, they have nonspecific abdominal symptoms like pain, nausea, or a palpable mass usually in the left upper quadrant [2].
On imaging, epidermoid and parasitic cysts, which are also primary cysts, can be similar in appearance showing up as well-defined solitary lesions with septations [2]. On computed tomography, septations, calcifications and internal debris can be visualized with no enhancement [2]. When findings are consistent with multiple neighboring cysts or daughter cysts, parasitic cysts are in favor as a diagnosis. Epidermoid cysts of the spleen usually have a thin-walled anechoic appearance on ultrasound with no evidence of calcification on computed tomography [3]. On T2-weighted magnetic resonance imaging, the cyst is hyper-intense, and on T1-weighted imaging, it is hypo-intense but can be increased depending on cyst contents [1]. We used computed tomography to accurately identify the location, size, and adjacent structures of the cyst with an understanding that a definitive diagnosis would only be made by histopathological examination. We identified a complex mass on ultrasound and a hypodense lesion on computed tomography with multiple foci of fat, which were very different demonstrations from what is expected of a classic epidermoid or parasitic cyst on imaging.
When examined, an epidermoid cyst usually has a white or grey smooth internal wall with fibrous trabeculations [2]. Under microscopic examination, an epithelium is visualized that is stratified squamous, which was consistent with our findings, and the contents can be serous, turbid, or thick and vary in color.
Radiological needle biopsies are not recommended due to the risk of complications. Surgical treatment is recommended for a symptomatic splenic cyst and for cysts larger than 5 cm [1], [2], [3]. Marsupialization or fenestration as treatments are indicated for superficial cysts, but they have a high recurrence rate [2], [4]. In our case a large cyst, greater than 5 cm was identified and extended behind the stomach and into the medial aspect of the spleen. A total splenectomy was our indicated diagnostic and treatment of choice due to size of the cyst, presentation with symptoms, and also as a preventative intervention against future rupture, hemorrhage, infection, or recurrence.
Our case has been reported in line with the SCARE criteria [5].
5. Conclusion
It is important to recognize that epidermoid splenic cysts may not always present in a classic fashion on imaging so it is trivial to include them as a differential diagnosis when warranted. The exact nature of a cyst will not be known prior to histological examination as in our case when imaging is not accurate or definitive in differentiation. Therefore, the cyst was treated based on symptomology, size, and location and a total splenectomy which was indicated, was performed.
Funding
No source of Funding.
Ethical approval
Case report, does not apply.
Consent
Consent for publication has been obtained.
Author contribution
Bilal Kharbutli, MD and Sharmilee Vuyyuru, DO have contributed in the study concept and writing.
Guarantor
Bilal Kharbutli, MD and Sharmilee Vuyyuru, DO
References
- 1.Cianci P., Tartaglia N., Altamura A. A recurrent epidermoid cyst of the spleen: report of a case and literature review. World J. Surg. Oncol. 2016;14:98. doi: 10.1186/s12957-016-0857-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vo Q.D., Monnard E., Hoogewoud H.M. Epidermoid cyst of the spleen. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-009707. pii: bcr2013009707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rana A.P., Kaur M., Singh P. Splenic epidermoid cyst – a rare entity. J. Clin. Diagn. Res. 2014;8:175–176. doi: 10.7860/JCDR/2014/6901.4050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y.Y., Shyr Y.M., Wang S.E. Epidermoid cyst of the spleen. J. Gastrointest. Surg. 2013;17:555–561. doi: 10.1007/s11605-012-2088-y. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE Statement: Consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]