Abstract
Embryonal Rhabdomyosarcoma ‘Botryoid Type’ is a rare soft tissue tumor that arises within the wall of the bladder or vagina and seen almost exclusively in infants. Treatment is combination of surgery with adjuvants chemotherapy and radiotherapy. We report a case of an 18-month-old Saudi girl presented with history of abdo-pelvic mass, bleeding per vagina and a mass protruding through the introitus. Computed tomography (CT) done reveling large heterogeneous pelvic mass arising from the uterus, biopsy of mass confirmed the diagnosis (sarcomabotryoidal). The patient received multiple cycles of combination chemotherapy as a neoadjuvant treatment then underwent total abdominal hysterectomy with upper vaginectomy. Postoperatively, the patient received more cycles of chemotherapy. CT scan for post-treatment evaluation was done and showed no evidence of local recurrence or distant metastasis. Currently, she is disease-free on remission with no complains.
INTRODUCTION
Gynecologic tumors in children are rare and represent <5% of all pediatrics neoplasms [1]. Rhabdomyosarcoma (RMS) are malignant mesenchymal tumors originating from myogenic progenitor cells. They represent the most common soft tissue tumor in childhood. The head and neck region are the most affected tumor sites, followed by the genitourinary tract [2]. Four major histologic subtypes of RMS are identified, Embryonal, Alveolar, Botryoid, pleomorphic/undifferentiated [2, 3].
Botryoid variant is a type of embryonal RMS arising within the wall of the bladder or vagina, can also occur in the cervix. This tumor is seen almost exclusively in infants, it is characterized by ‘grape-like’ appearance caused by polypoid mass arising in submucosal tissue [2, 4].
Embryonal RMS of the uterus is a variant which represent an extreme rare and aggressive form associated with poor prognosis [2].
The case
An 18-month-old Saudi female, full term, presented with history of vaginal bleeding at the age of 8 months, it was spontaneous, intermittent, fresh blood and painless. A red small mass protrude through the introitus was noticed at the age of 12 months by the mother initially; there was also difficult micturition without change in urine’s color or odor. No history of medication use by mother during pregnancy. Family history was unremarkable.
Physical examination
The baby appeared well, vitally stable.
Abdomen was distended with a suprapubic mass extending to the umbilical level, no skin changes, it was ~8 × 7 cm, firm, non-tender with limited mobility, upper and side border are rounded and lower border was deep in the pelvis, no palpable inguinal lymph node, no hepato-splenomegaly.
Pelvic examination revealed a grape-like appearance red mass 2 × 2 cm, protruding through the vaginal introitus, normal labia minora and majora.
Digital rectal exam: palpable non-fixed mass pushing on the rectum.
Other examinations were within normal.
A Body (computed tomography [CT]) revealed a retroperitoneal, pelvi-abdominal solid mass 10 × 6 cm with heterogeneous enhancement (Fig. 1), compressing on the bladder and both ureters with bilateral hydronephrosis, sparing the rectum, uterus cannot be traced, extending up to the umbilicus with no plain identified between the tumor and the abdominal wall. Bowel loops were displaced but no sign of intestinal obstruction/invasion, liver, spleen, lung and mediastinum were normal.
Figure 1:

Before treatment sagittal view (CT) showing a large mass (white arrow) compressing on bladder (red arrow).
A biopsy from the vaginal lesion was consistent with Embryonal RMS, Botryoid Type. Patient referred to pediatric oncology where she received 10 cycles of neoadjuvant chemotherapy (Vincristine, Actinomycin-D and Cyclophosphamide).
Afterwards, re-assessment through body CT revealed a reduction in mass size. It measures 4.2 × 5 × 3.6 cm compared to 10 × 6 cm (before chemo) (Fig. 2), the previously seen hydronephrosis was completely resolved. Without abdominal or pelvic lymphadenopathy. Afterwards she underwent surgery. A total abdominal hysterectomy, bilateral salpingectomy with upper vaginectomy (Fig. 3), ureterolysis and bilateral ovarian transposition (oopexy) was done.
Figure 2:

Sagittal view (CT) for the mass (white arrow) post-chemotherapy showing reduction in size (red arrow) bladder.
Figure 3:
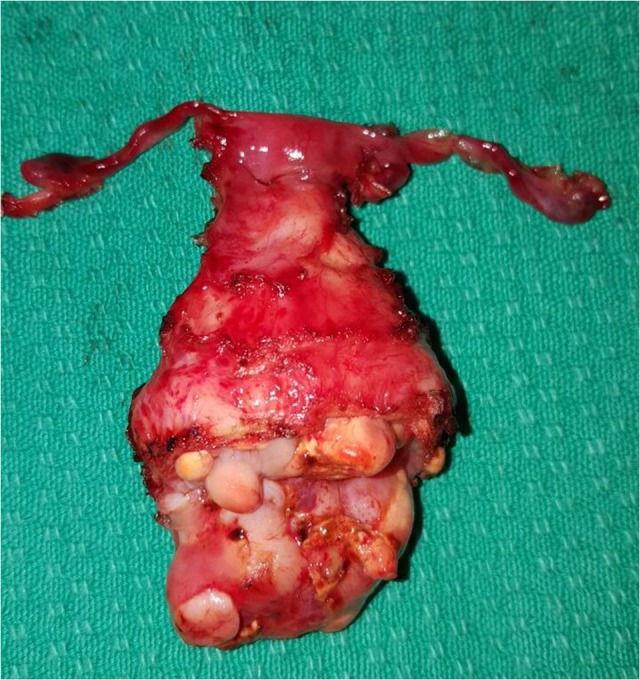
Total abdominal hysterectomy, bilateral salpingectomy with upper vaginectomy.
The Histopathological examination of the specimen revealed residual Embryonal RMS, Botryoid type. Most of the tumor mass show fibrosis, histiocytic inflammation and hemosiderin deposition, consistent with treatment effect.
Postoperatively, she had uneventful recovery and referred back to pediatric oncology where she received five more cycles of VAC chemotherapy. A repeat CT for post-treatment evaluation showed; no evidence of recurrence at the surgical site or distant metastasis (Fig. 4). Follow-up visits were arranged; she is now 12-month post-treatment completion. The assessment shows that she is completely healthy, a symptomatic with normal developmental milestone.
Figure 4:

Post-treatment sagittal view (CT) with no evidence of recurrence arising from the uterus (red arrow) bladder.
DISCUSSION
Embryonal RMS is a rare tumor affecting children, the genitourinary tract variant is a rapidly growing rare malignancy seen in 40% of RMS cases [5], occurring between 0 and 4 years of age. The average age at diagnosis of embryonal RMS of the vagina is ~2 years. The vast majority of cases occur sporadically with no recognized predisposing risk factors, although in a small proportion of the cases there may be a genetic link between cervical RMS and other primary tumors; most notably Sertoli–Leydig tumor [5]. Typically, grape-like structure arises under the mucosal surface of the organs and the vagina is the most common site. Our reported patient is diagnosed with RMS tumor that involved the uterus, cervix and vagina. She presented with vaginal bleeding and vaginal lesion. Some patient experienced additional symptoms included leukorrhea, bleeding and malodorous discharge. The patient we are reporting fulfilled all the three criteria essential for the diagnosis of botryoid variety of RMS; a polypoid appearance of the lesion, an origin below a mucous membrane-covered surface and the presence of a cambium layer [6]. Many authors recommend that any polypoidal mass found in a child be regarded as botryoid RMS unless proven otherwise [4]. However, the patient generally was looking well, in abdo-pelvic examination there was palpable mass at the umbilicus deep into the pelvis with grape-like mass protruded through the introits with no lymph nodes or hepatic involvement. Vaginal biopsy showed Embryonal RMS, botryoid type. The role of histopathology in the diagnosis of RMS cannot be underestimated and it is the gold standard test in the diagnosis. Although three varieties of RMS have been described (Embryonal, Alveolar and Undifferentiated), the embryonal type is the most common and has a favorable prognosis, whereas the alveolar type is rare with a poor prognosis. Embryonal RMS of the cervix must be distinguished pathologically from adenosarcomas, malignant mixed Müllerian tumors and low-grade stromal sarcomas as the optimal management strategies and clinical outcomes differ for each [5].
The optimal number of adjuvant chemotherapy cycles needed varies; it depends upon the clinical and radiological response. There are many reports of neoadjuvant chemotherapy being used to shrink large tumors before the surgery [5]. In this case, a neoadjuvant therapy was used of which 10 cycles of VAC protocol (vincristine, d-actinomycin and cyclophosphamide) were given. The VAC protocol is the most widely used chemotherapy regimen in RMS [4]. After the proven response to neoadjuvant chemotherapy; surgery was uneventful in the form of total abdominal hysterectomy, bilateral salpingectomy, upper vaginectomy (Fig. 3), ureterolysis and bilateral ovarian transposition (oopexy), the oopexy is to preserve the ovarian function knowing that she may receive radiation therapy too. Over the decades, there has been a paradigm shift in management strategies for botryoid RMS. Although ultra-radical surgery i.e. pelvic exenteration was considered the treatment of choice in the late 1960s, outcomes were often unsatisfactory. In the 1970s, limited surgery with adjuvant chemotherapy and/or irradiation showed improved survival [6].
Hays et al. reported 22 cases of non-metastatic vaginal RMS treated on the IRS I and II protocols, six patients who underwent biopsy only without extensive surgical resection. The response rate to chemotherapy in general was greater than 90%. The combined neoadjuvant chemotherapy with subsequent excision resulted in 79% disease-free survival rate [7]. Mousavi et al. concluded in a retrospective cohort study in Taxes; that this tumor has good prognosis due to early presentation, slow progression and the prognosis of patients treated with multimodal therapy is very good [4].
Albores et al. did review in his study 19 cases of RMS; 12 died from the effects of the tumor, while 2 are living with evidence of recurrence/metastases. Five are apparently free of tumor one and one-half to 6 years following treatment [8]. In Sweden, pediatric RMS showed a higher rate of metastatic disease, this may explain the decreased trend in overall survival in the last decade. However, the reason for the higher frequency of metastasis remains unclear and it would be of great interest to find out more about underlying causes [9].
In our case, we decided to treat the patient with neoadjuvant chemotherapy to down stage the tumor which played a role in ease the surgical procedure and minimize the surgical morbidity and complications. Bokhmanet al. did a review of the literature and analysis of 40 cases of genital malignancies in Russian girls and he found that; most embryonal RMS of the vagina or the vulva occurred in patients under the age of 4 whereas ovarian neoplasms (mostly germ and sex cord tumors) were observed at prepubertal and pubertal age [10].
It is important to know that the exact pathology of such an uncommon lesion in that site and its clinical implications are important to avoid unaccurate and subsequently and mismanagement.
Due to the rarity of these tumors, it may not be feasible to conduct randomized controlled trials to demonstrate the most appropriate treatment approach; however, interval debulking after neoadjuvant chemotherapy might be an acceptable and effective option in the treatment of Embryonal RMS.
ACKNOWLEDGEMENT
Dr Hasan Tarabulsi, Consultant Pediatric Oncology—KFSH RC Jeddah. Dr Samira ALTurkistany, Consultant Chest and Body Imaging—KFSH RC Jeddah.
CONFLICT OF INTEREST STATEMENT
No potential conflict of interest relevant to this article was reported. Consent was taken from family prior to writing this report.
REFERENCES
- 1. Fernandez-Pineda I, Spunt SL, Parida L, Krasin MJ, Davidoff AM, Rao BN. Vaginal tumors in childhood: the experience of St. Jude Children’s Research Hospital. J Pediatr Surg 2011;46:2071–5. [PubMed: PMC3476720]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Strahl O, Hartmann A, Thiel FC, Beckmann MW, Lux MP. 18-year-old woman with an embryonal rhabdomyosarcoma of the uterus in statu nascendi. Geburtshilfe Frauenheilkd 2012;72:1132–6. [PubMed: PMC4168320]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Agarwala S. Pediatric rhabdomyosarcomas and nonrhabdomyosarcoma soft tissue sarcoma. J Indian Assoc Pediatr Surg 2006;11:15–23. http://www.jiaps.com/text.asp?2006/11/1/15/24632. [Google Scholar]
- 4. Mousavi A, Akhavan S. Sarcoma botryoides (embryonalrhabdomyosarcoma)of the uterine cervix in sisters. J Gynecol Oncol 2010;21:273–5. [PubMed: PMC3026308]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dehner LP, Jarzembowski JA, Hill DA. Embryonal rhabdomyosarcoma of the uterine cervix: a report of 14 cases and a discussion of its unusual clinicopathological associations. Mod Pathol 2012;25:602–14. [PubMed: PMC5031244]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Neha B, Manjunath AP, Girija S, Pratap K. Botryoid Rhabdomyosarcoma of the cervix: case report with review of the literature. Sultan Qaboos Univ Med J 2015;15:e433–7. [PubMed PMID: 26357564]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hays DM, Shimada H, Raney RB Jr, Tefft M, Newton W, Crist WM, et al. Sarcomas of the vagina and uterus: the Intergroup Rhabdomyosarcoma Study. J Pediatr Surg 1985;20:718–24. [PubMed: 3910785]. [DOI] [PubMed] [Google Scholar]
- 8. Albores-Saavedra J, Martin RG, Smith JL. Rhabdomyosarcoma: a study of 35 cases. Ann Surg 1963;157:186–97. [PubMed: PMC1466425]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lychou SE, Gustafsson GG, Ljungman GE. Higher rates of metastatic disease may explain the declining trend in Swedish paediatric rhabdomyosarcoma survival rates. Acta Paediatr (Oslo, Norway: 1992) 2016;105:74–81. [PubMed: PMC4738396]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bokhman IaV, Nechaeva ID, Maksimov SIa, Kutusheva GF, Kolygin BA. Malignant tumors of the genitalia in girls. Vopr Onkol 1986;32:74–80. Review. Russian. [PubMed PMID: 3511609]. [PubMed] [Google Scholar]


