Abstract
AIM
To study the expression of collagen I and transcription factor specificity protein 1 (Sp1), a transforming growth factor-β1 (TGF-β1) downstream target, and reveal the impact of the TGF-β1-Sp1 signaling pathway on collagen remodeling in myopic sclera.
METHODS
Seventy-five 1-week-old guinea pigs were randomly divided into normal control, form deprivation myopia (FDM), and self-control groups. FDM was induced for different times using coverage with translucent latex balloons and FDM recovery was performed for 1wk after 4wk treatment; then, changes in refractive power and axial length were measured. Immunohistochemistry and reverse transcription-polymerase chain reaction were used to evaluate dynamic changes in collagen I and Sp1 expression in the sclera of guinea pigs with emmetropia and experimental myopia, and the relationship between collagen I and Sp1 levels was analyzed.
RESULTS
In the FDM group, the refractive power was gradually changed (from 2.09±0.30 D at week 0 to -1.23±0.69 D, -4.17±0.59 D, -7.07±0.56 D, and -4.30±0.58 D at weeks 2, 4, 6, and 1wk after 4wk, respectively; P<0.05), indicating deepening of myopia. The axial length was increased (from 5.92±0.39 mm at week 0 to 6.62±0.36 mm, 7.30±0.34 mm, 7.99±0.32 mm, and 7.41±0.36 mm at weeks 2, 4, 6, and 1wk after 4wk; P<0.05). The mRNA and protein expression of Sp1 and collagen I in the sclera of the FDM group was lower than that of the control groups (P<0.05), and the reduction was eye-coverage time-dependent. Furthermore, correlation between Sp1 and collagen I down-regulation in the myopic sclera was observed
CONCLUSION
Our data indicate that transcription factor Sp1 may be involved in the regulation of type I collagen synthesis/degradation during myopic sclera remodeling, suggesting that TGF-β1 signaling plays a role in the development and progression of myopia.
Keywords: form-deprivation myopia, sclera remodeling, transforming growth factor-β1, specificity protein 1, collagen I
INTRODUCTION
Myopia is one of the most prevalent visual disorders, and is very common in school-age children and adolescents. In Asian and Southeast Asian cities, mostly young people suffer from myopia; thus, 80% to 90% of college students have myopia, and 20% of them have high myopia. Myopia brings distress to young people, and presents a significant socioeconomic burden worldwide[1]–[2]. In China, the incidence of myopia has been ranked the second in the world only to Japan, accounting for 33% of the total number of myopia cases worldwide and negatively affecting the quality of life[3]. Therefore, the investigation of myopia etiology and pathogenesis, and the development of preventive and treatment measures are urgent for ophthalmologists to be able to solve this fundamental problem of great social significance.
At present, the pathogenesis of myopia is generally considered to be a combination of genetic and environmental factors[4]. Nowadays, an increasing number of biologically active molecules playing an important role in sclera remodeling in myopia have been identified owing to advances in molecular biology. Thus, it has been shown that transforming growth factor-β1 (TGF-β1) is involved in myopic sclera remodeling[5], while transcription factor specificity protein 1 (Sp1) identified as a TGF-β1 downstream target was found to regulate the synthesis and degradation of collagen type I[6]–[7], suggesting that it may play a role in sclera remodeling during myopia progression. However, in ophthalmology, Sp1 expression and its association with myopic sclera remodeling has not been investigated.
In this study, we explored the role of Sp1 in myopic sclera and its relationship with the synthesis and biodegradation of collagen type I using a guinea pig model of form deprivation myopia (FDM). Immunohistochemistry and reverse transcription-polymerase chain reaction (RT-PCR) were used to evaluate dynamic expression of Sp1 and type I collagen in guinea pigs with emmetropia and myopia at different time points after FDM induction. Our results have clarified the relationship between TGF-β1 signaling and collagen I expression in myopia, suggesting a novel mechanism underlying the disease pathogenesis.
MATERIALS AND METHODS
Ethics Statement
All experimental procedures were performed according to the Guidelines for the Care and Use of Laboratory Animals (No. 85-23 National Publication, revised in 1985). The study protocol was approved by the Experimental Animal Ethics Committee of Anhui Medical University.
Establishment of the Form Deprivation Myopia Model and Experimental Design
Seventy-five healthy 1-week-old guinea pigs weighing 100-140 g were maintained in the 12h-light/ 12h-dark environment at the temperature of 22°C in the Experimental Animal Center of Anhui Provincial Hospital affiliated with Anhui Medical University; the animals were given water, vitamin-rich guinea pig feed, and fresh vegetables[8]. Guinea pigs were randomly divided into the normal (untreated) control group (n=25) and FDM group (n=50). FDM was achieved using translucent latex balloons, which covered the animal head and the left eye, while the right eye, nose, mouth, and ears were exposed. The balloon was attached with a stapler to the neck fold to prevent their falling and rotation. Guinea pigs were treated for 2, 4, and 6wk; in addition, FDM recovery was performed for 1wk after 4wk treatment. The uncovered right eyes were used as self-control.
Refractive State and Axial Length
Guinea pigs were marked and numbered. Retinoscopy was performed in a dark room using a streak retinoscope (Liuliu, China) after the eye pupils had been fully dilated by tropicamide. The axial length of the eye was measured using an A-scan ultrasonograph (TOMEY AL-100, Japan) after anesthesia. The data were collected by the same person at every time point of the experiment (0, 2, 4, and 6wk, and 1wk after 4wk treatment) and the values were rounded to two digits after the decimal point[9].
Immunofluorescence
Guinea pigs were sacrificed after anesthesia with 1% sodium pentobarbital; the eyes were removed, the anterior segment discarded, and the samples were put on ice. The posterior sclera was excised around the head of the optic nerve using a 6-mm-diameter trephine, and the head of the optic nerve was discarded. Then, scleral tissues were fixed in 40% formaldehyde solution at 4°C. Samples were cut into sections, which were blocked, incubated with primary antibodies against Sp1 and collagen I, and analyzed under a fluorescent microscope.
Reverse Transcription and Polymerase Chain Reaction
Scleral tissues isolated as described were stored at -80°C until analysis. The required amount of scleral tissue was ground in liquid nitrogen and used to extract total RNA according to the manufacturer's instructions (5 samples from each group were used). Total RNA (2 µg) and 10 µmol/L Oligo (dT) were added to 0.2 mL of RNase-free water and heated for 5min at 65°C; after the reaction, the tubes were immediately put on ice for 3min. Reverse transcription was performed in a tube containing 4.0 µL of 5× reaction buffer, 2 µL of 10 mmol/L dNTP mix, 1 µL of RibolockTM RNase inhibitor, and 1 µL of Revert Aid TM M-MuLV reverse transcriptase at 42°C for 60min and 70°C for 5min. cDNA was extracted and stored at -80°C until PCR analysis. PCR amplification was performed under the following cycling conditions: 95°C for 5min; 35 cycles at 95°C for 30s, 55°C for 30s, and 72°C for 40s; the final extension step at 72°C for 10min and 4°C indefinitely. The amplified products were separated by agarose gel electrophoresis, and the results were analyzed using a gel imaging system. Primer sequences are listed in Table 1; β-actin was used as an internal control. Because guinea pig nucleotide sequences have not been reported, we used the corresponding rat sequences. All experiments were performed at least three times.
Table 1. Primer sequences, annealing temperatures, and predicted product sizes.
| Gene | Forward primer | Reverse primer | Tm (°C) | Size (bp) |
| β-actin | GCTCTATCCTGGCCTCACTC | GGGTGAGGGACTTCCTGTAA | 55 | 400 |
| Collagen I | ACAAGCGATTACACACCCAA | TTAGTTTCCTGCCTCTGCCT | 55 | 239 |
| Sp1 | CTCAAAGGAACAGAGTGGCA | GAGCTGGGAGTCAAGGTAGC | 55 | 486 |
Tm: Temperature.
Statistical Analysis
Statistical analysis was performed using the SPSS 22.0 statistical software. The results of refractive power and axial length measurements were expressed as the mean±SD. Differences were analyzed by paired t-test and ANOVA and considered statistically significant at P<0.05.
RESULTS
Refractive Power and Axial Length
When guinea pigs were born, their eyes went into a state of hyperopia; the axial length was relatively short, and there was no significant difference between the groups in refractive power and axial length (P>0.05, t-test). With the time of FDM induction, the refractive status in the FDM group gradually changed from hyperopia to myopia (P<0.05, t-test). The degree of hyperopia in the normal and self-control groups slightly decreased, while the axial length slightly increased. The differences in refractive power and axial length between the FDM and self-control or the normal control groups were significant at 2, 4, and 6wk and at 1wk after 4wk treatment (P<0.05, ANOVA). The results are presented in Table 2.
Table 2. Refractive state and axial length between the eyes of the three groups.
| Time (wk) | Refractive power (D) |
Axial length (mm) |
||||
| Normal control | Self-control | FDM | Normal control | Self-control | FDM | |
| 0 | 2.19±0.29 | 2.11±0.32 | 2.09±0.30 | 5.93±0.34 | 5.87±0.36 | 5.92±0.39 |
| 2 | 1.39±0.26a | 1.28±0.29a | -1.23±0.69 | 6.22±0.32a | 6.24±0.34a | 6.62±0.36 |
| 4 | 0.62±0.24a | 0.48±0.27a | -4.17±0.59 | 6.50±0.31a | 6.58±0.31a | 7.30±0.34 |
| 1 after 4 | 0.56±0.40a | 0.39±0.29a | -4.30±0.58 | 6.59±0.31a | 6.60±0.34a | 7.41±0.36 |
| 6 | -0.14±0.25a | -0.33±0.26a | -7.07±0.56 | 6.80±0.28a | 6.97±0.35a | 7.99±0.32 |
aP<0.05, compared with FDM group.
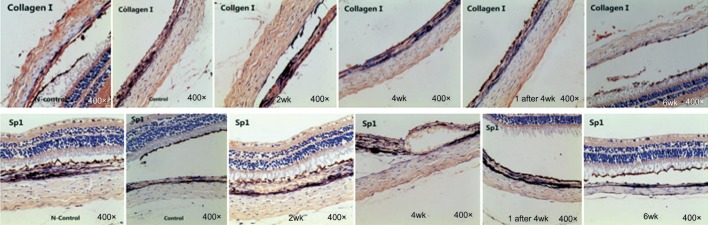
Changes in Protein Expression of Sp1 and Collagen I
Weak expression of collagen I and Sp1 protein in guinea pig scleral tissue was observed at 2, 4, and 6wk (Figure 1). At 1wk after 4wk treatment, the levels of collagen I and Sp1 were higher compared with those at 6wk, but lower compared with those at 4wk. There was no significant difference in collagen I and Sp1 expression between the normal control and self-control groups, but there were significant differences between the other groups (P<0.05, respectively) (Table 3).
Figure 1. Distribution of Sp1 and type I collagen in guinea pig sclera analyzed by immunofluorescence.
Table 3. Relative protein expression of Sp1 and collagen I.
| Time (wk) | n | Sp1 | Collagen I |
| 0 | 15 | 0.797±0.038 | 0.928±0.016 |
| 2 | 15 | 0.543±0.010a | 0.743±0.012c |
| 4 | 15 | 0.378±0.010a | 0.552±0.014c |
| 1 after 4 | 15 | 0.369±0.014a | 0.533±0.011c |
| 6 | 15 | 0.350±0.018a | 0.402±0.019c |
aP<0.05, cP<0.05, compared with 0wk.
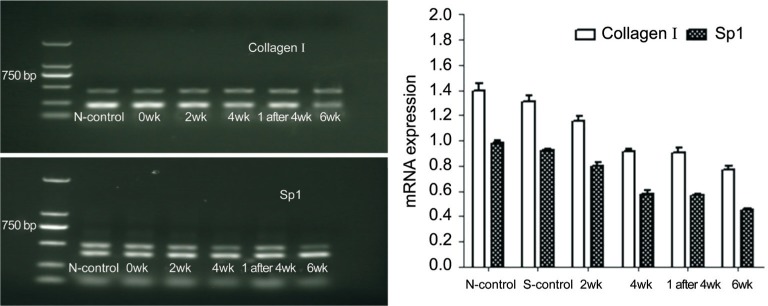
Changes in Sp1 and Collagen I mRNA Expression
The expression of collagen I and Sp1 mRNA in guinea pig scleral tissue gradually decreased with the time of FDM induction; however, at 1wk after 4wk treatment, collagen I and Sp1 transcription was higher compared with that at 6wk, but lower compared with that at 4wk. There was no significant difference in the expression of collagen I and Sp1 mRNA between the normal control and self-control groups, but significant differences were observed between the other groups (P<0.05) (Figure 2).
Figure 2. Influence of myopia induction on Sp1 and collagen I mRNA expression in guinea pig sclera.
Correlation Analysis of Sp1 and Collagen I Expression
In the scleral tissue, collagen I and Sp1 expression showed significant correlation both at the protein and mRNA levels (r=1; P=0.0 and P<0.05, respectively).
DISCUSSION
Previous studies indicate that sclera remodeling plays a crucial role in the occurrence and progress of myopia. The main morphological change in myopia is manifested by excessive extension of the ocular axial length[10]–[11]. Collagen fibers are the most abundant constituents of the sclera, accounting for 90% of the sclera net weight; they are primarily formed by collagens Ι, III, and IV, and collagen Ι fibers occupy the largest area of the sclera. In myopic sclera remodeling, the expression of collagen, especially that of collagen Ι, is declining[12]. It was shown that TGF-β plays an important role in maintaining the normal morphology and function of the sclera and that the expression of TGF-β isoforms 1, 2, 3 is downregulated during myopia progression[13]–[14]. It particularly concerns TGF-β1, which is declining in the process of myopic sclera remodeling, and it is suggested that the TGF-β1-Smad3-connective tissue growth factor pathway may be one of the most important mechanisms underlying scleral changes in myopia[15]–[16]. A previous study indicated that Wnt/β-catenin signaling regulates TGF-β1 and type I collagen expression in fibroblasts of the myopic sclera[17]. Sp1 is proved to be a downstream target of TGF-β1 signaling in many physiological processes. Thus, in gingival wounds healing, TGF-β1 regulates the expression of connexin 43 in fibroblasts through Sp1 and other transcription factors[6]. However, there have been no studies on the expression and function of Sp1 in myopic sclera remodeling. In this study, we examined Sp1 expression and its relationship with collagen I synthesis and degradation in the myopic sclera of guinea pigs.
Previous studies have shown that as the degree of myopia increases, the expression of TGF-β1 and collagen I gradually declines during the process of myopic sclera remodeling, suggesting positive correlation between TGF-β1 and collagen I levels. The results of immunohistochemistry and RT-PCR analyses performed in our study show that the expression of collagen I protein and mRNA gradually declines with the time of FDM induction. However, in the recovery group (1wk after 4wk treatment), collagen I expression was increased both at the mRNA and protein levels compared with 6wk FDM, although it was lower compared with 4wk FDM. These data indicate that as the eye coverage time prolongs and myopia deepens, the expression of collagen I gradually declines, suggesting its association with myopia development, which is consistent with a previous study[18].
Sp1 belongs to the specificity protein/Kruppel-like factor (Sp/XKLF) family of transcription factors, which contain three conservative Cys2/His2 zinc finger DNA-binding sites; the damage of zinc finger structure not only affects Sp1 binding to DNA, but also its nuclear transfer. In mammalian cells, Sp1 regulates multiple cellular progression, including cell cycle, growth, proliferation, metabolism, and apoptosis[19]–[20]. The results of this study show that Sp1 expression in scleral tissues decreases with the time of FDM both at the mRNA and protein levels, but 1wk recovery after 4wk exposure increases Sp1 levels compared to the 6wk FDA group. These results indicate that Sp1 expression is downregulated in myopia, suggesting that Sp1 decrease is involved in myopia development and confirming the role of the TGF-β1 pathway in the process. Moreover, the correlation between Sp1 and collagen I expression in scleral tissues indicates a link between TGF-β1-Sp1 signaling and collagen I production during myopic sclera remodeling, suggesting a molecular mechanism underlying myopia progression.
In conclusion, our study confirms that Sp1 is expressed in the sclera of guinea pigs with experimental myopia, while the correlation between Sp1 and collagen I expression suggests that the TGF-β1 pathway regulates type I collagen synthesis in myopic sclera remodeling. Based on these and previous findings, it can be speculated that TGF-β1-Smad3 signaling is involved in scleral remodeling and myopia pathogenesis, providing a new direction in myopia research and development of preventive measures. We recommend that future studies use a larger sample sample size in order to further validate these results.
Acknowledgments
The authors thank Jing-Jing Zhang for her technical assistance in the measurement of diopter and axial length.
Foundations: Supported by the Natural Science Foundation of Anhui Province (No.1508085MH188); Science Foundation of Anhui Provincial Health Bureau (No.13zc040; No.13zc046).
Conflicts of Interest: Jiang B, None; Wu ZY, None; Zhu ZC, None; Ke GJ, None; Wen YC, None; Sun SQ, None.
REFERENCES
- 1.He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, Smith W, Rose K, Morgan IG. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 2.Wei X, Zhang JS. Effects and mechanism of prienzeine on lens-induced myopia in the guinea pigs. Rec Adv Ophthalmol. 2010;30(1):20–23. [Google Scholar]
- 3.Song SF, Li H. Progress of epidemiologic study of myopia. Guoji Yanke Zazhi (Int Eye Sci) 2011;11(3):453–454. [Google Scholar]
- 4.Guo L, Yang J, Mai J, Du X, Guo Y, Li P, Yue Y, Tang D, Lu C, Zhang WH. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye (Lond) 2016;30(6):796–804. doi: 10.1038/eye.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meng B, Li SM, Yang Y, Yang ZR, Sun F, Kang MT, Sun YY, Ran AR, Wang JN, Yan R, Bal YW, Wang NL, Zhan SY. The association of TGFB1 genetic polymorphisms with high myopia: a systematic review and meta-analysis. Int J Clini Exp Med. 2015;8(11):20355–20367. [PMC free article] [PubMed] [Google Scholar]
- 6.Tarzemany R, Jiang G, Larjava H, Hakkinen L. Expression and function of connexin 43 in human gingival wound healing and fibroblasts. PLoS One. 2015;10(1):e0115524. doi: 10.1371/journal.pone.0115524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Wang DW, Song LW, Peng RY, Gao YB, Ma JJ. Effects of TGFbeta1 on the transcr iptionalactivity of Sp1, AP1 and Smad3-Smad4 in lung fibroblasts. Xi Bao Yu Fen Zi Mian Yi Xue Za Zi. 2005;21(6):679–682. [PubMed] [Google Scholar]
- 8.Wang Q, Xue ML, Zhao GQ, Liu MG, Ma YN, Ma Y. Form-deprivation myopia induces decreased expression of bone morphogenetic protein-2, 5 in guinea pig sclera. Int J Ophthalmol. 2015;8(1):39–45. doi: 10.3980/j.issn.2222-3959.2015.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu ZC, Zhang JS. Effects of form-deprivation on expression of P-Stat3 in the retina of guinea pigs. Anhui Med J. 2009;30(8):860–862. [Google Scholar]
- 10.Fan L, Zhou X, Jiang L, Fu Y, Lai X, Xie R, Qu J. Axial myopia induced by hyperopic defocus in guinea pigs: a detailed assessment on susceptibility and recovery. Exp Eye Res. 2009;89(1):101–108. doi: 10.1016/j.exer.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 11.Zou L, Liu R, Zhang X, Chu R, Dai J, Zhou H, Liu H. Upregulation of regulator of G-protein signaling 2 in the sclera of a form deprivation myopic animal model. Mol Vis. 2014;20:977–987. [PMC free article] [PubMed] [Google Scholar]
- 12.Gentle A, Liu Y, Martin JE, Conti GL, McBrien NA. Collagen gene expression and the altered accumulation of scleral collagen during the development of high myopia. J Bio Chem. 2003;278(19):16587–16594. doi: 10.1074/jbc.M300970200. [DOI] [PubMed] [Google Scholar]
- 13.Jobling AI, Nguyen M, Gentle A, McBrien NA. Isoform-specific changes in scleral transforming growth factor-beta expression and the regulation of collagen synthesis during myopia progression. J Biol Chem. 2004;279(18):18121–18126. doi: 10.1074/jbc.M400381200. [DOI] [PubMed] [Google Scholar]
- 14.Jobling AI, Wan R, Gentle A, Bui BV, McBrien NA. Retinal and choroidal TGF-beta in the tree shrew model of myopia: isoform expression, activation and effects on function. Exp Eye Res. 2009;88(3):458–466. doi: 10.1016/j.exer.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 15.Ji XY, Zhang JS, Zhu ZC, Sun HL. Expression of Smad3 signal way and CTGF in scleral fibroblasts of guinea pigs. Yixue Zheng Ming. 2009;30(10):920–922. [Google Scholar]
- 16.Ji X, Zhang J, Wang Y, Sun H, Jia P. Mechanism of Smad 3 signaling pathway and connective tissue growth factor in the inhibition of form deprivation myopia by pirenzepine. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2009;34(4):349–355. [PubMed] [Google Scholar]
- 17.Li M, Yuan Y, Chen Q, Me R, Gu Q, Yu Y, Sheng M, Ke B. Expression of Wnt/β-catenin signaling pathway and its regulatory role in type I collagen with TGF-β1 in scleral fibroblasts from an experimentally induced myopia guinea pig model. J Ophthalmol. 2016;2016:5126560. doi: 10.1155/2016/5126560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu H, Xiang N, Zhang H. Influence of high level TGF-beta1 on scleral thickness. J Huazhong Univ Sci Technolog Med Sci. 2007;27(5):601–604. doi: 10.1007/s11596-007-0532-0. [DOI] [PubMed] [Google Scholar]
- 19.Hellweg CE, Spitta LF, Henschenmacher B, Diegeler S, Baumstark-Khan C. Transcription factors in the cellular response to charged particle exposure. Front Oncol. 2016;6:61. doi: 10.3389/fonc.2016.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beishline K, Azizkhan-Clifford J. Sp1 and the “Hallmarks of Cancer”. FEBS J. 2015;282(2):224–258. doi: 10.1111/febs.13148. [DOI] [PubMed] [Google Scholar]