Abstract
AIM
To evaluate the clinical outcomes of V4c implantable collamer lens (Hole ICL) implantation with regard to the optical quality assessed according to different degrees of decentering.
METHODS
This included 49 eyes that received conventional ICL and 94 eyes that received Hole ICL. The eyes that received Hole ICL were divided into three groups according to the degree of decentering: group 1, central hole within 1 hole diameter (HD) from the pupil center; group 2, central hole within 1 HD to 2 HD; and group 3, central hole within 2 HD to 3 HD. Visual acuity (VA), intraocular pressure (IOP), and spherical equivalent (SE) values were assessed at 1wk, 1 and 3mo after surgery. The ocular modulation transfer function, Strehl ratio, objective scattering index, and higher order aberrations (HOAs) were measured for 4-mm pupils at 3mo after surgery.
RESULTS
There were no significant differences in VA, IOP, and SE among the conventional and Hole ICL groups. With regard to HOAs, values for coma and spherical aberrations showed no differences. The total HOA and trefoil values were significantly higher in group 2 than in group 1 (P=0.02, 0.03, respectively). There were no significant differences among groups with regard to other optical quality parameter at 3mo after surgery.
CONCLUSION
Our results suggest that Hole ICL implantation provides satisfactory visual quality that is equivalent to that provided by conventional ICL, regardless of the presence of central hole and degree of decentering.
Keywords: implantable collamer lens, optical quality, phakic IOL, refractive surgery
INTRODUCTION
The implantable collamer lens (ICL; STAAR Surgical, Nidau, Switzerland), used as a posterior chamber phakic intraocular lens (pIOL), is made from collamer, a biocompatible hydrophilic copolymer of collagen and hydroxyethyl methacrylate with an ultraviolet light-filtering chromophore. It is effective and safe for the correction of myopia[1]–[3], hyperopia[4]–[5], and astigmatism[6]–[7]. However, some reported postoperative complications include increased intraocular pressure (IOP)[8], pupillary block[9], glaucoma[8]–[10], and anterior subcapsular cataract. Accordingly, ICL models have been modified to prevent these complications. The recently developed KS AquaPORT® (Visian ICL with Centra FLOW® technology, V4c; STAAR surgical company, Monrovia, CA, USA) model is designed with a central hole measuring 0.36 mm (KS-Aquaport) to facilitate more natural flow of the aqueous humor and decrease the risk of secondary cataract formation. It provides good IOP outcomes without the requirement for additional peripheral iridotomy or iridectomy[11].
A previous study demonstrated that the V4c ICL (hereafter referred to as Hole ICL) model for the correction of moderate to high myopia performed well in all measures of safety, efficacy, predictability, and stability, suggesting the viability of this model as an effective surgical option[12].
However, the presence of the central hole in Hole ICL can affect the postoperative optical quality. For instance, it can result in the introduction of a glare or a halo. In a previous study, Shimizu et al[13] evaluated the visual performance of patients after Hole ICL implantation and found that this lens was similar to conventional ICL with regard to the induction of higher order aberrations (HOAs) and contrast sensitivity (CS). Uozato et al[14] measured the modulation transfer function (MTF) of conventional ICL and Hole ICL at various powers and pupil diameters and reported small and clinically negligible differences between the two models.
Meanwhile, the influence of the position of the central hole on HOAs and the visual quality of patients is another concern. In some previous studies, it was demonstrated that decentering of Hole ICL did not affect the visual quality[15]–[16]. However, these studies were experimental laboratory studies, with small sample sizes. Therefore, clinically meaningful studies with statistical evaluations are desirable to clarify these findings.
From the above perspectives, we conducted the present study to evaluate the clinical outcomes of Hole ICL implantation with regard to the optical quality assessed according to the degree of decentering in a large patient population.
SUBJECTS AND METHODS
Design and Participants
This retrospective, observational study included the medical records of patients who had received V4 or V4cICL for the correction of myopia at Busan Sungmo Eye Hospital, Busan, Korea. At the time of surgery, all patients were fully informed of the details and possible risks related to the surgical procedure, following which written informed consent was obtained in accordance with the Declaration of Helsinki. The study protocols were approved by the institutional review board.
The inclusion criteria were as follows: myopia in a range that was correctable by V4c ICL implantation [-0.50 diopter (D) to -18.00 D], a corrected distance visual acuity (CDVA) of 20/25 or better, stable refraction, and a clear central cornea. The exclusion criteria were as follows: previous corneal refractive surgery; an anterior chamber depth (ACD) of less than 2.8 mm; an endothelial cell density (ECD) of less than 2000 cells/mm2; cataract; and a history of glaucoma, retinal detachment, macular degeneration, retinopathy, neuro-ophthalmic disease, and/or a history of ocular inflammation. Patients with a shift in the pupil center that was greater than 0.2 mm, as assessed by the KR-1W viewer (Topcon Co., Tokyo, Japan) and Pentacam (Oculus, Wetzlar, Germany) were also excluded.
Preoperative Evaluations
Before surgery, all patients underwent complete ophthalmological examinations, including uncorrected distance visual acuity (UDVA) and CDVA measurements, manifest and cycloplegic refraction assessments, tonometry (TonopachyNT-530P, Nidek Co., LTD, Tokyo, Japan), gonioscopy, keratometry, corneal pachymetry, corneal topography (Orbscan IIZ® Corneal Topography System; Bausch and Lomb, Bridgewater, NJ, USA), central endothelial cell count (ECC) assessments (SP-3000P: Topcon Corporation, Tokyo, Japan), slit lamp biomicroscopy, and binocular indirect ophthalmoscopy through dilated pupils.
Postoperative Evaluations
All patients were followed-up for 3mo. Patients underwent slit lamp biomicroscopy and measurement of UDVA, CDVA, manifest refraction, and IOP at 1wk, 1 and 3mo postoperatively.
Implantable Collamer Lens Decentering
Decentering was measured using slit lamp examinations at 3mo after surgery. Digital slit lamp photographs were obtained without mydriatic agents to allow identification of the pupil center under low lighting condition. Using image editing software (Adobe Photoshop 7.0 software), we classified the eyes into three groups as follows: group 1, central hole within 1 hole diameter (HD) from the pupil center; group 2, central hole within 1 HD to 2 HD; and group 3, central hole within 2 HD to 3 HD (Figure 1).
Figure 1. Degrees of decentering of the V4c implantable collamer lens (Hole ICL) implanted in the present study.

Group 1: Central hole within 1 HD from the pupil center; Group 2: Central hole within 1 HD to 2 HD; Group 3: Central hole within 2 HD to 3 HD. Adobe Photoshop 7.0 software has been used for classification.
Optical Quality Parameters
The optical quality was analyzed using the Optical Quality Analysis System (Visiometrics SL, Tarrasa, Spain) at 3mo after surgery. Through an analysis of the double-pass image, the system estimates the ocular MTF and the corresponding Strehl ratio. It also assesses the objective scatter index (OSI) as a measure of the amount of light scattered during passage through the ocular structures. We calculated OSI, MTF cutoff frequency (cpd), and Strehl ratio values for 4-mm pupils.
Higher Order Aberrations
The KR-1W viewer was used to analyze and measure wavefront aberrations at 3mo after surgery. The KR-1W viewer provided a measured value for spherical aberrations in 4-mm and 6-mm optical zones. We obtained the root mean square values of the total HOAs, trefoil, coma, and spherical aberrations for 4-mm pupils.
Statistical Analysis
All statistical analyses were performed using SPSS statistical package version 18.0 (SPSS Inc., Chicago, Illinois, USA). One-way analysis of variance (ANOVA) was used to detect differences between the conventional ICL and Hole ICL groups divided according to the degree of decentering. A P-value of <0.05 was considered statistically significant.
RESULTS
In total, the data for 143 eyes of 85 patients (mean age at the time of surgery, 26.2±6.6y; range, 18 to 45y), including 49 and 94 eyes that received V4 and Hole ICL, respectively, were evaluated in this study. There were no significant differences in the conventional ICL and groups 1, 2, and 3 with regard to age and the anterior chamber depth, corneal white-to-white distance, spherical equivalent (SE), and IOP before surgery (Table 1).
Table 1. Preoperative patient demographics.
| Parameters | Conventional ICL group | Group 1 | Group 2 | Group 3 | Pa |
| Eyes (n) | 49 | 46 | 42 | 6 | |
| Patients (n) | 27 | 28 | 24 | 6 | |
| Age (a) | 28.5±6.0 | 25.6±6.7 | 26.2±6.5 | 25.8±6.3 | 0.15 |
| ACD (mm) | 3.24±0.20 | 3.19±0.20 | 3.18±0.16 | 3.21±0.22 | 0.06 |
| WTW (mm) | 11.47±0.37 | 11.54±0.37 | 11.50±0.42 | 11.48±0.35 | 0.47 |
| Spherical equivalent (D) | -8.52±2.77 | -8.58±2.08 | -8.50±2.23 | -8.56±1.88 | 0.58 |
| Baseline IOP (mm Hg) | 14.05±2.91 | 14.39±2.92 | 14.57±2.71 | 13.50±1.87 | 0.71 |
ACD: Anterior chamber depth; WTW: White to white; IOP: Intraocular pressure. aStudent's t-test.
Degree of Decentering
With regard to the degree of decentering of the Hole ICL, 46 eyes (48.9%) were classified into group 1, 42 (44.7%) into group 2, and six (6.4%) into group 3. The central hole was positioned within 1 HD in 48.9% eyes and within 2 HD in 93.6% eyes.
Postoperative Visual Acuity and Spherical Equivalent Values
The mean UCVA at 3mo after surgery was -0.05±0.08 logMAR, -0.01±0.06 logMAR, -0.04±0.07 logMAR, and -0.03±0.08 logMAR in the conventional ICL groups and groups 1, 2, and 3, respectively. There were no statistically significant differences among groups throughout the postoperative period (P>0.05; Table 2). SE at 3mo after surgery was 0.31±0.29 D, 0.21±0.27 D, 0.32±0.19 D, and 0.38±0.29 D in the conventional ICL group and groups 1, 2, and 3 respectively, with no significant differences among groups (P>0.05; Table 3).
Table 2. Postoperative UDVA (logMAR) values.
| Variables | Conventional ICL group | Group 1 | Group 2 | Group 3 | Pa |
| 1wk | -0.01±0.05 | -0.01±0.07 | -0.02±0.05 | 0.00±0.00 | 0.83 |
| 1mo | -0.05±0.08 | -0.01±0.06 | -0.05±0.08 | -0.03±0.08 | 0.06 |
| 3mo | -0.05±0.08 | -0.01±0.06 | -0.04±0.07 | -0.03±0.08 | 0.09 |
aOne-way ANOVA.
Table 3. Postoperative SE values.
| Variables | Conventional ICL group | Group 1 | Group 2 | Group 3 | Pa |
| 1wk (D) | 0.31±0.31 | 0.28±0.24 | 0.38±0.21 | 0.50±0.40 | 0.12 |
| 1mo (D) | 0.31±0.29 | 0.24±0.27 | 0.35±0.16 | 0.38±0.29 | 0.08 |
| 3mo (D) | 0.31±0.29 | 0.21±0.27 | 0.32±0.19 | 0.38±0.29 | 0.06 |
aOne-way ANOVA.
Postoperative Intraocular Pressure Values
Figure 2 shows the changes in IOP values over time. There were no significant differences in IOP values among the different groups throughout the follow-up period (Table 4). Moreover, a significant increase in IOP (over 20 mm Hg) was not recorded for any case during the follow-up period.
Figure 2. Comparisons of preoperative and postoperative intraocular pressure among the conventional ICL and three Hole ICL groups.
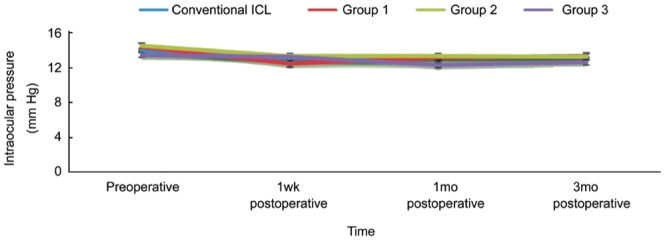
No statically significant differences can be observed among groups. ICL: Implantable collamer lens; Hole ICL: V4c implantable collamer lens.
Table 4. Changes in IOP values.
| Variables | Conventional ICL | Group 1 | Group 2 | Group 3 |
| preoperative | 14.05±2.91 | 14.39±2.92 | 14.57±2.71 | 13.50±1.87 |
| 1wk postoperative | 13.18±2.70 | 12.52±2.34 | 13.40±2.58 | 13.33±2.66 |
| 1mo postoperative | 13.24±2.72 | 13.26±2.80 | 13.38±2.36 | 12.33±1.97 |
| 3mo postoperative | 13.42±2.74 | 13.37±2.80 | 13.33±2.63 | 12.67±1.86 |
Postoperative Optical Quality Parameters
There were no significant differences among the different groups with regard to OSI, MTF cutoff, and Strehl ratio values (P>0.05) at 3mo after surgery (Table 5).
Table 5. Optical quality parameters at 3mo after lens implantation.
| Parameters | Conventional ICL group | Group 1 | Group 2 | Group 3 | Pa |
| OSI | 0.98±0.94 | 0.82±0.56 | 0.94±0.76 | 1.07±1.17 | 0.57 |
| MTF cutoff frequency (cpd) | 31.08±11.45 | 33.42±9.20 | 34.13±9.51 | 32.74±11.94 | 0.91 |
| Strehl ratio | 0.17±0.06 | 0.19±0.06 | 0.18±0.05 | 0.19±0.07 | 0.61 |
OSI: Ocular scatter index; MTF: Modulation transfer function. aOne-way ANOVA.
Postoperative Higher Order Aberration Values
There were no significant differences among groups with regard to coma and spherical aberration values. However, the total HOA (0.179±0.103 µm vs 0.131±0.054 µm; P=0.02) and trefoil values (0.128±0.102 µm vs 0.083±0.045 µm; P=0.03) were significantly higher in group 2 than in group 1 (Table 6).
Table 6. Postoperative HOAs at 3mo after lens implantation.
| RMS | Conventional ICL group | Group 1 | Group 2 | Group 3 | Pa |
| Total HOA (µm) | 0.182±0.080 | 0.131±0.054 | 0.179±0.103 | 0.158±0.050 | 0.02 |
| Coma (µm) | 0.095±0.065 | 0.065±0.046 | 0.090±0.072 | 0.091±0.047 | 0.13 |
| Trefoil (µm) | 0.123±0.078 | 0.083±0.045 | 0.128±0.102 | 0.096±0.031 | 0.03 |
| Spherical aberrations (µm) | 0.009±0.030 | 0.015±0.028 | 0.016±0.036 | 0.017±0.030 | 0.98 |
RMS: Root mean square; HOA: Higher order aberration. aOne-way ANOVA.
DISCUSSION
In the present study, we assessed the optical quality provided by Hole ICL according to the degree of decentering and compared the findings with those for conventional ICL. Hole ICL is widely used because of its advantages over conventional ICL; however, visual disturbances such as a halo or a glare remain a cause for concern. Furthermore, the position of the central hole after implantation is not always in the center, and the influence of this decentering remains another cause for concern.
Several previous studies have revealed that the outcomes achieved with Hole ICL implantation are equivalent to those achieved with conventional ICL implantation. Shimizu et al[12] reported that the uncorrected visual acuity was -0.20±0.12 logMAR at 6mo after Hole ICL implantation, with 100% eyes presenting values within ±1.00 D of the targeted correction. Moreover, they did not record an increase in IOP for any case. In a more recent study, they reported the 5-year outcomes of Hole ICL implantation[17]. The uncorrected visual acuity was -0.17± 0.14 logMAR, and 96% eyes presented values within ±1.00 D of the targeted correction. The manifest refraction value changed by -0.17±0.41 D between 1mo and 5y. In the present study, satisfactory visual acuity (VA) was achieved for all cases; the UDVA values were under +0.1 logMAR at 3mo after surgery, with a safety index of 1.08±0.15. Moreover, all eyes showed SE values within ±1.00 D, with no significant increase in IOP. With regard to the postoperative UDVA, IOP, and SE values, there were no significant differences between the conventional ICL and Hole ICL groups, as well as among the three Hole ICL groups stratified according to the degree of decentering. These findings were similar to those obtained in a previous study conducted by Perez-Vives et al[16], where VA values achieved with conventional ICL and Hole ICL at different degrees of decentering showed no significant differences for all ICL powers (-3 D, -6 D, -12 D) and pupil diameters (3 mm and 4.5 mm).
Several studies have compared the optical quality achieved with Hole ICL and conventional ICL. In an experimental laboratory study by Perez-Vives et al[15], no statistically significant differences were observed in any Zernike coefficients between the conventional and Hole ICL groups. Kamiya et al[18] showed that there were no significant differences in optical quality parameters between Hole ICL and conventional ICL groups, implying that the optical quality, including intraocular scattering, in eyes with Hole ICL implantation was essentially equivalent to that in eyes with conventional ICL implantation. Other studies demonstrated that Hole ICL implantation was almost equivalent to conventional ICL implantation with regard to the induction of HOAs, CS, and subjective symptoms such as a glare or a halo, and that the optical quality and intraocular scattering in eyes with ICL implantation were essentially equivalent to those in healthy eyes[13],[19]. In the present study, optical quality parameters, specifically the MTF cutoff frequency, Strehl ratio, and OSI were not significantly different between the conventional ICL and Hole ICL groups and among the Hole ICL groups classified according to the degree of decentering.
With regard to HOAs, coma and spherical aberration values were not significantly different among groups in the present study. However, total HOA and trefoil values were significantly different between eyes where the central hole was within 1 HD from the pupil center (group 1) and eyes where the central hole was within 1 HD to 2 HD from the pupil center (Table 5). The precise mechanism by which HOAs affect the visual quality remains unclear. Rocha et al[20] measured the changes in VA induced by individual Zernike ocular aberrations (defocus, astigmatism, coma, trefoil, and spherical aberrations) of various root mean square magnitudes (0.1, 0.3, and 0.9 mm) for 5-mm pupils. Single Zernike aberrations applied with a coefficient of 0.1 µm, with the exception of spherical aberrations, resulted in small changes in VA that ranged between mean values of 0.03 and 0.05 logMAR. Therefore, differences in trefoil and total HOA values between conventional ICL and Hole ICL are not expected to clinically affect the visual quality of patients. Considering the lack of differences in visual parameters in the present study, we consider that the influence of HOA changes on the visual quality to be low. In other study, Perez-Vives et al[15] found statistically significant differences in coma values between conventional centered ICL and Hole ICL with two different degrees of decentering, although they found that an increase in coma aberrations showed a small influence on point spread functions (PSFs) and simulated retinal images. Thus, although HOA changes according to the degree of ICL decentering varied among studies, the effects of HOA changes on the actual visual quality are likely to be small. Further studies on this topic are necessary.
There is no accurate method to measure of line of sight yet. There have been attempts to measure the line of sight using the pupil center and the lens center. But the pupil center and the lens center are not always line of sight. Therefore in this paper, to reduce the bias that may occur by considering the pupil center as the line of sight, all of patients underwent KR-1W and Pentacam. Then, patients with a shift in the pupil center that was greater than 0.2 mm were excluded. And all patients underwent digital slit lamp photographs under the same low lighting condition.
This paper has limitations. We do not have preoperative data of the HOAs. Because of that, we can not prove exactly about why a decentered ICL does not induce coma-like aberration. And OQAS device and OSI index are good parameters to define the optical quality, but not gold standard parameters.
In conclusion, the results of our study suggest that Hole ICL implantation provides satisfactory optical quality that is equivalent to that provided by conventional ICL implantation, regardless of the presence of the central hole and the degree of decentering. Hence, surgeons can select Hole ICL implantation without concerns regarding the effects of decentering.
Acknowledgments
Conflicts of Interest: Park MJ, None; Jeon HM, None; Lee KH, None; Han SY, None.
REFERENCES
- 1.Sanders DR, Doney K, Poco M, ICL in Treatment of Myopia Study Group United States food and drug administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111:1683–1692. doi: 10.1016/j.ophtha.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 2.Sanders DR, Vukich JA, Doney K, Gaston M, U.S; Implantable Contact Lens in Treatment of Myopia Study Group Food and drug administration clinical trial of the implantable contact lens for moderate to high myopia. Ophthalmology. 2003;110:255–266. doi: 10.1016/s0161-6420(02)01771-2. [DOI] [PubMed] [Google Scholar]
- 3.Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009;127:845–850. doi: 10.1001/archophthalmol.2009.67. [DOI] [PubMed] [Google Scholar]
- 4.Davidorf JM, Zaldivar R, Oscherow S. Posterior chamber phakic intraocular lens for hyperopia of +4 to +11 diopters. J Refract Surg. 1998;14(3):306–311. doi: 10.3928/1081-597X-19980501-14. [DOI] [PubMed] [Google Scholar]
- 5.Pesando PM, Ghiringhello MP, Di Meglio G, Fanton G. Posterior chamber phakic intraocular lens (ICL) for hyperopia: ten-year follow-up. J Cataract Refract Surg. 2007;33:1579–1584. doi: 10.1016/j.jcrs.2007.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Sanders DR, Schneider D, Martin R, Brown D, Dulaney D, Vukich J, Slade S, Schallhorn S. Toric Implantable Collamer Lens for moderate to high myopic astigmatism. Ophthalmology. 2007;114(1):54–61. doi: 10.1016/j.ophtha.2006.08.049. [DOI] [PubMed] [Google Scholar]
- 7.Schallhorn S, Tanzer D, Sanders DR, Sanders ML. Randomized prospective comparison of visian toric implantable collamer lens and conventional photorefractive keratectomy for moderate to high myopic astigmatism. J Refract Surg. 2007;23(9):853–867. doi: 10.3928/1081-597X-20071101-01. [DOI] [PubMed] [Google Scholar]
- 8.Sanchez-Galeana CA, Zadok D, Montes M, Cortes MA, Chayet AS. Refractory intraocular pressure increase after phakic posterior chamber intraocular lens implantation. Am J Ophthalmol. 2002;134(1):121–123. doi: 10.1016/s0002-9394(02)01414-9. [DOI] [PubMed] [Google Scholar]
- 9.Bylsma SS, Zalta AH, Foley E, Osher RH. Phakic posterior chamber intraocular lens pupillary block. J Cataract Refract Surg. 2002;28(12):2222–2228. doi: 10.1016/s0886-3350(02)01303-2. [DOI] [PubMed] [Google Scholar]
- 10.Brandt JD, Mockovak ME, Chayet A. Pigmentary dispersion syndrome induced by a posterior chamber phakic refractive lens. Am J Ophthalmol. 2001;131(2):260–263. doi: 10.1016/s0002-9394(00)00606-1. [DOI] [PubMed] [Google Scholar]
- 11.Alfonso JF, Lisa C, Fernandez-Vega Cueto L, Belda-Salmeron L, Madrid-Costa D, Montes-Mico R. Clinical outcomes after implantation of a posterior chamber collagen copolymer phakic intraocular lens with a central hole for myopic correction. J Cataract Refract Surg. 2013;39(6):915–921. doi: 10.1016/j.jcrs.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 12.Shimizu K, Kamiya K, Igarashi A, Shiratani T. Early clinical outcomes of implantation of posterior chamber phakic intraocular lens with a central hole (Hole ICL) for moderate to high myopia. Br J Ophthalmol. 2012;96(3):409–412. doi: 10.1136/bjophthalmol-2011-300148. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu K, Kamiya K, Igarashi A, Shiratani T. Intraindividual comparison of visual performance after posterior chamber phakic intraocular lens with and without a central hole implantation for moderate to high myopia. Am J Ophthalmol. 2012;154(3):486–494.e481. doi: 10.1016/j.ajo.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Uozato H, Shimizu K, Kawamorita T, Ohmoto F. Modulation transfer function of intraocular collamer lens with a central artificial hole. Graefes Arch Clin Exp Ophthalmol. 2011;249(7):1081–1085. doi: 10.1007/s00417-010-1602-8. [DOI] [PubMed] [Google Scholar]
- 15.Perez-Vives C, Ferrer-Blasco T, Madrid-Costa D, Garcia-Lazaro S, Montes-Mico R. Optical quality comparison of conventional and hole-visian implantable collamer lens at different degrees of decentering. Am J Ophthalmol. 2013;156:69–76.e61. doi: 10.1016/j.ajo.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Perez-Vives C, Ferrer-Blasco T, Madrid-Costa D, Garcia-Lazaro S, Montes-Mico R. Visual quality comparison of conventional and Hole-Visian implantable collamer lens at different degrees of decentering. Br J Ophthalmol. 2014;98(1):59–64. doi: 10.1136/bjophthalmol-2013-303787. [DOI] [PubMed] [Google Scholar]
- 17.Shimizu K, Kamiya K, Igarashi A, Kobashi H. Long-term comparison of posterior chamber phakic intraocular lens with and without a central hole (hole ICL and conventional ICL) implantation for moderate to high myopia and myopic astigmatism: consort-compliant article. Medicine (Baltimore) 2016;95(14):e3270. doi: 10.1097/MD.0000000000003270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamiya K, Shimizu K, Saito A, Igarashi A, Kobashi H. Comparison of optical quality and intraocular scattering after posterior chamber phakic intraocular lens with and without a central hole (hole ICL and conventional ICL) implantation using the double-pass instrument. PLoS One. 2013;8(6):e66846. doi: 10.1371/journal.pone.0066846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamiya K, Shimizu K, Igarashi A, Kobashi H, Ishii R, Sato N. Clinical evaluation of optical quality and intraocular scattering after posterior chamber phakic intraocular lens implantation. Invest Ophthalmol Vis Sci. 2012;53(6):3161–3166. doi: 10.1167/iovs.12-9650. [DOI] [PubMed] [Google Scholar]
- 20.Rocha KM, Vabre L, Harms F, Chateau N, Krueger RR. Effects of Zernike wavefront aberrations on visual acuity measured using electromagnetic adaptive optics technology. J Refract Surg. 2007;23(9):953–959. doi: 10.3928/1081-597X-20071101-17. [DOI] [PubMed] [Google Scholar]


