Abstract
Childhood stunting, being short for one’s age, has life-long consequences for health, human capital and economic growth. Being stunted in early childhood is associated with slower cognitive development, reduced schooling attainment and adult incomes decreased by 5–53%. The World Health Assembly has endorsed global nutrition targets including one to reduce the number of stunted children under five by 40% by 2025. The target has been included in the Sustainable Development Goals (SDG target 2.2). This paper estimates the cost of achieving this target and develops scenarios for generating the necessary financing. We focus on a key intervention package for stunting (KIPS) with strong evidence of effectiveness. Annual scale-up costs for the period of 2016–25 were estimated for a sample of 37 high burden countries and extrapolated to all low and middle income countries. The Lives Saved Tool was used to model the impact of the scale-up on stunting prevalence. We analysed data on KIPS budget allocations and expenditure by governments, donors and households to derive a global baseline financing estimate. We modelled two financing scenarios, a ‘business as usual’, which extends the current trends in domestic and international financing for nutrition through 2025, and another that proposes increases in financing from all sources under a set of burden-sharing rules. The 10-year financial need to scale up KIPS is US$49.5 billion. Under ‘business as usual’, this financial need is not met and the global stunting target is not reached. To reach the target, current financing will have to increase from US$2.6 billion to US$7.4 billion a year on average. Reaching the stunting target is feasible but will require large coordinated investments in KIPS and a supportive enabling environment. The example of HIV scale-up over 2001–11 is instructive in identifying the factors that could drive such a global response to childhood stunting.
Keywords: Child health, cost, health financing, malnutrition
Key Messages
Scaling up the key intervention package for stunting to reach the SDG stunting target will cost US$49.5 billion over 10 years.
Reaching the global stunting target will require rapid expansion and strong coordination of investments in nutrition from national governments, donors and innovative sources of financing.
To reach the global target, current financing will have to increase from US$2.6 billion to US$7.4 billion a year on average.
With global poverty rates having declined to less than 10% for the first time in history, we have an unprecedented opportunity to save children’s lives, build human capital and drive faster economic growth by tackling stunting.
Introduction
Childhood stunting, being short for one’s age, has life-long consequences not just for health, but also for human capital and economic growth at the individual, household and national levels. Being stunted in early childhood is associated with slower cognitive development and lower IQ scores, reduces schooling attainment by 1 year (Martorell et al. 2010), and decreases adult incomes by 5–53% (Hoddinott et al. 2008, 2011). Consequently, reductions in stunting prevalence can increase economic productivity by 4–11% in Africa and Asia (Horton and Steckel 2013). Because of that, nutrition interventions are consistently identified as one of the most cost-effective development actions (Horton and Hoddinott 2015). A 2013 study estimated that every dollar invested in programs to reduce stunting would generate US$18 in economic returns (Hoddinott et al. 2013).
In 2015, 159 million children under five were stunted (UNICEF et al 2015) revealing a massive global health and development failure. The world’s governments have recognized this failure and endorsed a set of global nutrition targets, including one to reduce the number of stunted children under five by 40% by 2025. This global target has since been enshrined within Sustainable Development Goal 2, target 2: ‘By 2030, end all forms of malnutrition, including achieving, by 2025, the internationally agreed targets on stunting and wasting in children under 5 years of age, and address the nutritional needs of adolescent girls, pregnant and lactating women and older persons’ (United Nations et al. 2015).
Ending stunting is critical for development. However, while the investment case for nutrition is strong, efforts to reach the SDG stunting target are constrained by a range of factors including insufficient funding, which in turn is compounded by major gaps in knowledge regarding the cost and financing needs required to scale up nutrition interventions. Two earlier studies have estimated the cost of expanding the coverage of nutrition interventions (Horton et al. 2010; Bhutta et al. 2013). However, they did not provide estimates of the cost of reaching the global nutrition targets. Furthermore, they did not focus on stunting but rather estimated the cost of a number of evidence-based interventions affecting a number of different aspects of child undernutrition (stunting, wasting, micronutrient deficiencies). No prior study has presented a comprehensive global estimate of donor and national government investments in nutrition or in stunting prevention. Furthermore, while some efforts to assess global expenditure or budget allocations for nutrition investments are under way (International Food Policy Research Institute 2015), there exist no estimates of the shortfall between what is required and what is being spent to reduce stunting at the global level.
Without an understanding of current nutrition investments, future needs, their impact, and ways to mobilize the required funds, it is unlikely that adequate resources will be invested and the nutrition targets will be met. This article aims to close these gaps in the literature and current state of knowledge by estimating the cost of achieving the global stunting target, linking costs with impact estimates, assessing current financing and proposing financing scenarios to reach the global stunting target.
Methods
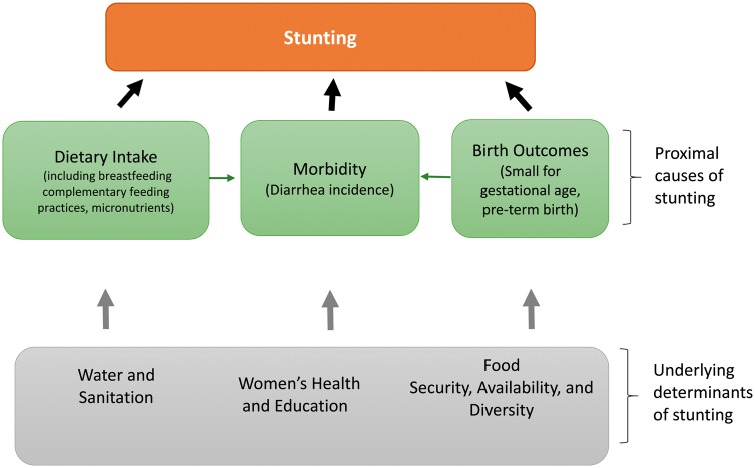
Our analysis is based on the conceptual model of the determinants of malnutrition shown in (Figure 1), which is adapted from the 1990 ICN conceptual framework for nutrition.
Figure 1.
Simplified conceptual model of the causes of stunting
The analysis focuses on nutrition-specific interventions for which there is strong evidence of effectiveness in reducing stunting, either directly or indirectly, through affecting various stunting risk factors (Bhutta et al. 2013). The interventions include: complementary feeding education, public provision of complementary foods, prophylactic zinc supplementation for children, breastfeeding promotion, vitamin A supplementation, multiple micronutrient supplementation in pregnancy, balanced energy-protein supplementation for pregnant women and intermittent preventive treatment of malaria (IPTp) for pregnant women (see Table 1). We refer to these as the ‘Key Intervention Package for Stunting’ (KIPS).
Table 1.
Target population, description and summary of the evidence of effectiveness of the interventions included in the analyses
| Intervention | Target population | Description | Evidence of effectiveness |
|---|---|---|---|
| Vitamin A supplementation | Children 6–59 months | Distribution of two doses per year (100 000 international units [IU] for children 6–11months old and 200 000 IU for children 12–59 months old) either through mass campaigns or in health facilities | Vitamin A indirectly affects stunting through influencing diarrhoeal incidence and mortality. Vitamin A supplementation has been shown to reduce diarrhoea-specific incidence [RR 0·85, 95% CI 0·82–0·87; 13 studies] and mortality [RR 0·72, 95% CI 0·57–0·91; 7 studies].a |
| Breastfeeding & complementary feeding counselling | Mothers of children 0–23 months | Individual counselling sessions to promote exclusive breastfeeding & timely introduction of complementary foods | Education on complementary feeding alone improved height-for-age Z scores [SMD 0·23, 95% CI 0·09–0·36; 5 studies], and decreased stunting risk [RR 0·71, 95%CI: 0·60–0·76; 6 studies]. However, there was no significant impact on height gain [SMD 0·23, 95% CI –0·00, 0·45; 6 studies].b |
| Public provision of complementary foods | Children 6–23 months living under the poverty line ($1·25/day) | Food supplementation for children (100–1500 kcal per day), typically including micronutrients | The provision of complementary foods, with or without education increased height-for-age Z score [SMD 0·39, 95% CI 0·05–0·73; 7 studies].c |
| Prophylactic zinc for children | Children 6–-59 months | Zinc (10 mg/day); 120 packets per child per year; Currently, no delivery platforms exist at scale. Cost estimates are based on multiple micronutrient powder supplementation programs | Supplementation with 10 mg zinc/day for 24 weeks increased mean gain in height (cm) [0·37, 95% CI 0·12–0·62; 16 studies] compared to a placebo intervention.d Zinc supplementation also reduced diarrhoeal incidence [RR 0·87, 95% CI 0·81–0·94] in the intervention group compared to a control group.e |
| Multiple micronutrient supplementation for pregnant women | Pregnant women | Broadly defined as a micronutrient supplementation that contains iron and at least two or more micronutrients. The cost was calculated for supplementation containing 15 micronutrients/vitamins including iron and folic acid, for 180 days per pregnancy | When compared to placebos or supplements with fewer than two micronutrients, the UNICEF UNIMAP supplement which contains 14 micronutrients, including iron and folic acid, showed significant effects on low birthweight [RR 0·88, 95% CI 0·85–0·91], small-for-gestational age [RR 0·89, 95% CI 0·83–0·96] and preterm birth [RR 0·97, 95% CI 0·94–0·99].f |
| Balanced energy-protein supplementation | Pregnant women living under the poverty line ($1·25/day) | Food supplementation during pregnancy (with no more than 25% energy content contributed by proteins) | Indirect impact on stunting through reduced risk of low-birth weight infants and infants born small-for-gestational age. When compared with the control group, BEPS resulted in a positive impact in birthweight [mean difference (MD) 73 g, 95% CI 30–117], with effects more clearly pronounced in undernourished women (12 studies) than women with adequate nutrition (7 studies). BEPS also reduced the risk of small-for-gestational age babies [RR 0·66, 95% CI 0·49–0·89; 9 studies], stillbirths [RR 0·62, 95% CI 0·40–0·98; 4 studies] and increased birth length (cm) [MD 0·16, 95% CI 0·02–0·16; 7 studies].h |
| Intermittent preventive treatment in pregnancy | Pregnant women (in malaria endemic areas only) | Two doses of sulfadoxine-pyrimethamine (SP) during pregnancy | Among first and second births, supplementation with IPTp-SP led to higher birthweight [Weighted MD 126·70, 95% CI 88·64–164·75; 8 trials; 2648 participants] compared to those with placebo or no intervention. The intervention also decreased risk of low birthweight [RR 0·57, 95% CI 0·46–0·72; 6 trials; 2350 participants], increased mean birth weight [MD 92·72, CI 95% CI 62·05–123·39; 9 trials]i and decreased low birthweight [RR 0·73, 95% CI 0·61–0·87; 8 trials] among first and second births.j |
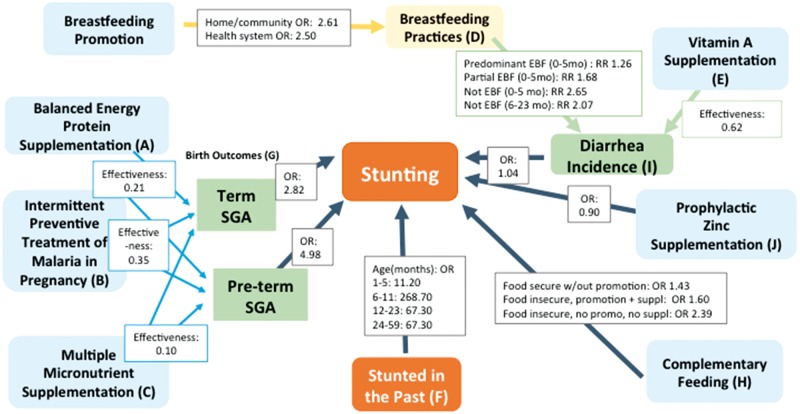
The impact of the interventions was modeled using Lives Saved Tool (LiST) (Lives Saved Tool, 2015). (Figure 2) shows the pathways and the estimated impact of each intervention on the likelihood of stunting, illustrating how the effects of interventions were modelled. The impact estimates are based on the most recent meta-analyses and systematic literature reviews. In the model we have used, three interventions: education on correct complementary feeding practices, public provision of complementary foods targeting children in food insecure contexts, and prophylactic zinc supplementation directly affect the likelihood of stunting (see Yakoob et al. 2011; Bhutta et al. 2013). The other interventions are modelled to have an indirect impact by reducing the prevalence of risk factors that are known to increase the risk of childhood stunting. More specifically, balanced energy protein supplementation in pregnancy, intermittent preventive treatment for malaria in pregnancy and multiple micronutrient supplementation in pregnancy reduce the risk of pre-term birth and the risk of a child being born small-for-gestational age, which are in turn, risk factors for stunting. Similarity, breastfeeding promotion and vitamin A supplementation, do not directly impact stunting (Singha et al. 2015; Victora et al. 2016), but lower the incidence of diarrhoea, which is a stunting risk factor (see Singha et al. 2015 and Victora et al. 2016).
Figure 2.
Path model of the impact of impact of the key interventions to prevent stunting on stunting prevalence. Notes: Sources of effect sizes: (A) Balanced energy supplementation–Imdad and Bhutta (2011) (B) IPTp–Eisele et al. (2010) (C) Multiple micronutrient supplementation–Haider et al. (2011); Pena-Rosas et al. (2015); Haider and Bhutta (2015) (D) Breastfeeding practices–Victora et al. (2016); Singha et al. (2015) (E) Vitamin A supplementation–Imdad et al. (2011) (F) Past stunting–LiST default values based on expert opinion (G) Birth outcomes–LiST default values based on expert opinion. (H) Complementary feeding–Imdad et al. (2011) (I) Diarrhoea incidence–Bhutta et al. (2008) (J) Zinc supplementation–Yakoob et al. (2011); Bhutta et al. (2013)
Because the KIPS are usually delivered through the health system, via facility or community delivery platforms, scale-up costs of the KIPS were estimated from the health system perspective. We estimated the cost for a sample of 37 countries, which included 20 countries with the highest absolute number of stunted children and 17 smaller countries with stunting prevalence above 40%1 (see Supplementary data S1). For each intervention in each country in the sample, we estimated the additional cost of scale-up from the current coverage level to 100%. For costing purposes, we assumed that the coverage would increase in a linear fashion from the current levels to 100% over the first 5 years (2016–20), and then be maintained at 100% during the following 5 years (2021–25).2 The 37 countries account for 84.3% of the global stunting burden. The cost estimate for all low and middle income countries was extrapolated from the sample by multiplying the sample cost estimate by an adjustment factor of 1.186 calculated as the inverse of the number of stunted children in the 37 sample countries as a proportion of the number of stunted children in all low and middle income countries (1/0.843).Costs were calculated in 2015 US dollars and were not discounted.
To account for potential increases in marginal costs as program coverage approaches 100% (e.g. higher costs to access the hardest-to-reach groups) and the fact that reaching 100% coverage of any public health intervention may not be possible, we estimated the impact of reaching only 90% of the beneficiaries. To the total cost we also added 9% for capacity development, 2% for monitoring and evaluation and 1% for policy development (Horton et al. 2010).
We modelled the reductions in stunting prevalence resulting from scaling up the interventions from the current coverage to 90% separately for each of the 37 countries in the sample. We combined country-specific results to obtain a population-weighted reduction in the overall prevalence in the sample of countries. We assumed the same relative prevalence change in low and middle income countries outside the sample. We calculated the global reduction in stunting by applying this relative reduction in the number of stunted children in the sample (84.3% of the global burden of stunting) to the 2015 baseline estimate of 159 million children stunted worldwide (UNICEF et al. 2015).
We assumed that the decline due to KIPS scale-up would take place in addition to reductions resulting from a parallel expansion of nutrition-sensitive actions that affect the underlying determinants of undernutrition (see Figure 1), including food availability and diversity, women’s health, education, and empowerment, and water, sanitation, and hygiene (WASH) (UNICEF 1990).3 Evidence regarding the effectiveness of nutrition-sensitive interventions, with the exception of WASH, is insufficient to allow for modelling of impact or estimation of intervention costs (Ruel et al. 2013). Therefore, we modelled plausible reductions in an indirect way based on the impact estimates from Smith and Haddad (2015). Smith and Haddad used a country-level regression model to assess the impact of food availability (measured as average daily kilocalories consumed per capita), food diversity (measured as the % of total diet from non-staples), women’s education (measured as female secondary enrollment rate) and women’s health and empowerment (measured as female-to-male life expectancy ratio) on country-level stunting prevalence. For each of the 37 countries in the sample, we calculated a trend in each of the four variables based on the changes over the previous 5 years (2011–15) and assumed that the same trend will continue over the 10 year period between 2016 and 2025. Using the regression coefficients reported in Smith and Haddad, we calculated the expected reductions in stunting during 2016–25 if previous 5-year trend continued. Data on women’s secondary enrollment and female-to-male life expectancy ratio were obtained from the World Development Indicators (WDI) data base. Data on food availability and diversity were extracted from the FAO food balance sheets.
We estimated the impact of five WASH interventions (handwashing with soap, improved water source, improved sanitation, water connection at home and hygienic disposal of children’s stool) directly using LiST. For the WASH interventions, we followed the strategy used to model the impact of the nutrition-specific interventions. For each of the 37 countries in the sample, we modelled a linear expansion of coverage from the current level to 90% in 2016 and maintenance of the coverage at 90% through 2025. We did not model the cost of those interventions because they will likely be incurred by sectors other than health.
We employed the program experience costing approach, which relies on reported actual costs of programs in countries. Summary measures of the unit costs by interventions are shown in Table 2. Unit cost data were obtained from peer-reviewed publications, grey literature, costed national nutrition plans, and data collected by the World Bank as part of a series of nutrition costing studies (Shekar et al. 2014, 2015a, 2015b). If unit cost data were unavailable for a given intervention in a given country, unit costs for a neighbouring country in the same region were used. If no unit cost data were available for any country in a given region, we used the average from Sub-Saharan Africa, where the largest number of unit cost data points was available, and applied WHO CHOICE regional multipliers based on Horton et al. (2010) to account for difference in income levels and the cost of service provision.
Table 2.
Minimum, maximum and population-weighted average unit cost used to estimate the cost of scale-up in a sample of 37 high burden countries (USD)
| Intervention | Minimum (USD) | Maximum (USD) | Population-weighted average unit cost (USD) |
|---|---|---|---|
| Vitamin A supplementation | $0.03 | $4.81 | $0.32 |
| Breastfeeding and complementary feeding counselling | $0.07 | $12.00 | $6.62 |
| Public provision of complementary foods | $29.03 | $115.28 | $42.93 |
| Prophylactic zinc | $2.40 | $6.19 | $3.89 |
| Multiple micronutrient supplementation for pregnant women | $1.80 | $7.55 | $2.80 |
| Balanced energy-protein supplementation for pregnant women | $16.93 | $54.72 | $24.07 |
| Intermittent preventive treatment in pregnancy | $2.27 | $2.27 | $2.27 |
Population and population growth estimates were obtained from the UNDP World Population Prospects (United Nations et al. 2015). Current intervention coverage data were extracted from the most recent Demographic and Health Surveys. We assumed 0% current coverage for prophylactic zinc, multiple micronutrient supplementation and balanced energy-protein supplementation for pregnant women because those interventions have not been implemented at scale. Cost and impact of IPTp were estimated only for sub-Saharan Africa, where malaria incidence is high enough to justify this intervention.
Estimates of the current spending on KIPS were generated by combining data from the three sources of financing: (1) country governments; (2) external support provided by bilateral and multilateral organizations and private foundations and (3) household contributions.4
We obtained data on government nutrition spending from public expenditure reviews for health, national budgets, the Global Health Expenditure Database, case studies on nutrition budget analysis, and country-led analyses of national nutrition budget allocations conducted by Scaling Up Nutrition (SUN) countries (IFPRI 2015). When there was a budget line for a broader program such as maternal and child health activities with some nutrition components, we attributed a fraction of the budget to nutrition based on desk review of programs (see Supplementary data S2 for detailed methodology). A mix of both budget allocation and expenditure data was available for 31 countries. A linear regression model based on the available data was used to extrapolate domestic financing for nutrition to all remaining low and middle income countries (see Supplementary data S3).
Data on donor disbursements for nutrition were extracted from the OECD development Creditor Reporting System (OECD CRS). We analysed project descriptions tied to 70% of disbursements to basic nutrition CRS purpose code 12240 in 2013 in countries representing 95% of the global stunting burden, assessing nutrition investments by intervention. When insufficient detail was available through project descriptions in the CRS data base, we supplemented this with desk research of donor and implementing agency websites and annual progress reports. For projects funding multiple interventions (e.g. behaviour change education, growth monitoring and distribution of nutrition supplements) we allocated a share of the reported disbursement to the relevant nutrition interventions. Additionally, we analysed nutrition investments under CRS health purpose codes5 in order to capture nutrition investments that may not have been classified under basic nutrition (Supplementary data S4).
Following the methodology from Horton et al. 2010, we assumed that households in higher income quintiles can pay for some of the commodities such as multiple micronutrient supplements. Though the majority of these commodities are delivered free via public channels, literature shows that more affluent households can purchase nutrition products on the marketplace through pharmacies, kiosks and door to door sellers (Leive and Xu 2008; Siekmann et al. 2012; TEC 2012; Suchdev et al. 2013). Household financing was estimated by calculating the percent of households that spend regularly on these commodities based on the data from the UNICEF Multiple Indicator Cluster Surveys, and applying this share to the annual country cost as a proxy for market size in each country.
To assess financing for nutrition from 2016 through 2025, we considered two future financing scenarios–‘business as usual’ and ‘global solidarity’. For the ‘business as usual’ scenario, we assumed that domestic government and household financing would increase according to projected GDP growth trends and donor financing would increase to meet the commitments made during and following the Nutrition for Growth summit.6
The ‘global solidarity’ scenario assumed that the total cost needed to scale-up the interventions will be covered through a coordinated increase in funding from government and donors, supplemented by innovative financing mechanisms such as Power of Nutrition or Global Financing Facility for Every Woman and Every Child (GFF). We assumed that governments would raise nutrition spending to the median spending of their respective country income group by 2020 (low income, lower-middle income, upper middle income). Countries starting above the median were assumed to increase nutrition spending as a share of total government expenditure by 1% per year. We further assumed that, starting in 2021, low and lower middle income country governments would increase their financial commitments so that by 2025 all low income countries (LICs) were assumed to cover 50% of the total cost, and lower middle income countries (LMICs)–70% of the total cost (see Supplementary data S5 for details). Commitments made by the Power of Nutrition (Power of Nutrition 2015) and other innovative financing mechanisms were assumed to be fully realized and distributed among recipient countries proportionally based on stunting burden. The gap remaining after government and innovative financing commitments was assumed to be filled by the official development assistance.
Results
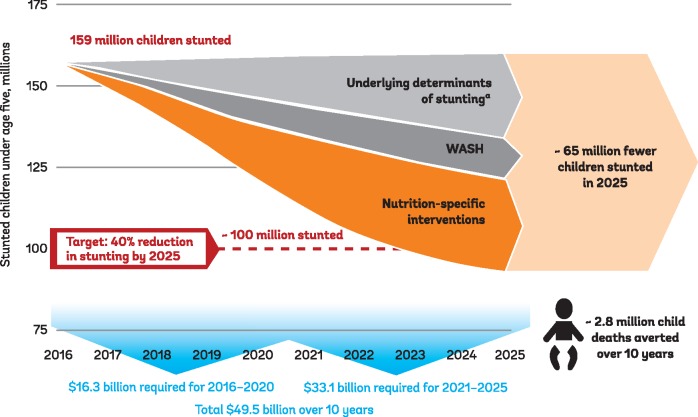
Together, scaling up the KIPS to 90% coverage and expected improvements in the underlying determinants of malnutrition were estimated to lead to about a 40% decline in the number of stunted children in low and middle income countries by 2025, enabling the achievement of the global stunting target (Figure 3). Scaling up of KIPs would result in a reduction of 19.5% in the number of stunted children by 2025.5 Improvements in the underlying determinants through the scale-up of nutrition-sensitive actions would drive the remaining decline. This would translate into 65 million fewer children stunted in 2025 compared to the baseline of 159 million in 2015.
Figure 3.
Projected reductions in the numbers of stunted children resulting from KIPS and from improvements in the underlying determinants of malnutrition 2016–25 (millions)
The total cumulative 10 year financing needs for scaling up the KIPS to meet the global stunting target are estimated at US$49.5 billion (Table 3). This includes US$44.2 billion in direct service delivery costs and additional US$5.3 billion for monitoring and evaluation, capacity and policy development. Of this, US$16.3 billion is projected to be required during the first 5 year scale-up phase (2016–20) and an additional US$33.1 billion during the maintenance phase (2021–25). Prophylactic zinc supplementation and public provision of complementary food together account for about 60% of the intervention costs (32% and 29%, respectively). Balanced energy protein supplementation and breastfeeding and complementary feeding counselling each represent a little over 15% percent of the total and multiple micronutrient supplementation for pregnant women, vitamin A supplementation and IPTp all contribute 5% or less to the total cost.
Table 3.
Global financing needs estimates for the 10-year scale-up of kips in low and middle income countries worldwide (USD million)
| Intervention | Total 10-year Intervention costs | Share of total 10-year cost |
|---|---|---|
| Vitamin A supplementation | 716 | 2% |
| Breastfeeding promotion, complementary feeding education and promotion of good infant and young child nutrition practices: | 6823 | 15% |
| Public provision of complementary foods | 12 750 | 29% |
| Prophylactic zinc supplementation | 14 212 | 32% |
| Multiple micronutrient supplementation for pregnant women | 2309 | 5% |
| Balanced energy-protein supplementation | 6949 | 16% |
| Intermittent preventive treatment for malaria in pregnancy | 416 | 1% |
| Subtotal | 44 175 | 100% |
| M & E | 883 | |
| Policy development | 442 | |
| Capacity strengthening | 3976 | |
| 10 year total | 49 476 |
Two countries–India and China–account for about a quarter of the overall global financing needs (15·3% and 10·5%, respectively) due to their large populations. Almost half (47%) of the estimated global needs is for Sub-Saharan Africa, with South Asia accounting for 22% of the global total. Over the 10-year period, annual financing needs would decrease in South Asia and other regions due to projected declines in the under-five population, but rise in Africa due to expected population growth. LICs accounted for 31% of global costs, LMICs for 51% and UMICs the remaining 18%.
Our analysis suggests that at present, country governments and donors spend approximately US$3.9 billion annually on all nutrition-programs. Within this total, an estimated US$2.6 billion is currently being directed to KIPS. The largest share of current spending on KIPS comes from domestic sources––US$2.2 billion, of which 71% is contributed by the 37 highest stunting burden countries. The amount spent on KIPS per child under five increases by income group: on average, LIC governments spend US$0.85 per child, MICS US$4.67 per child, and UMICs US$8.14. We further estimate that donors spent a little less than US$1 billion on all nutrition activities in 2015, of which about 35% (US$347 million) was invested in KIPS.
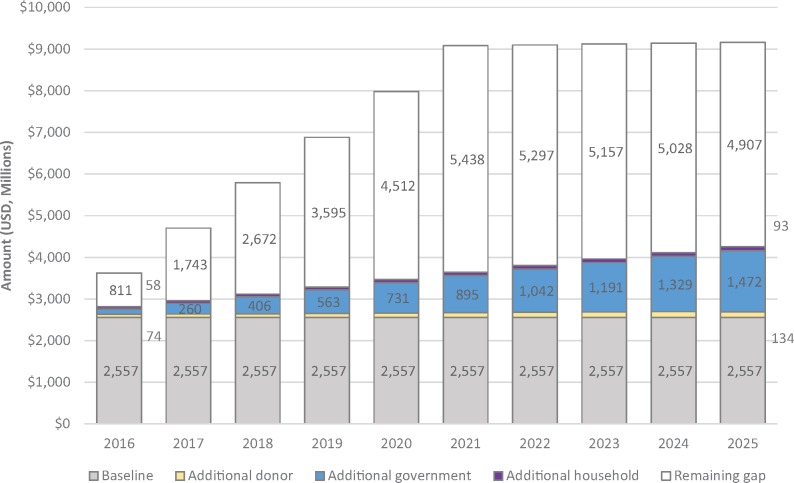
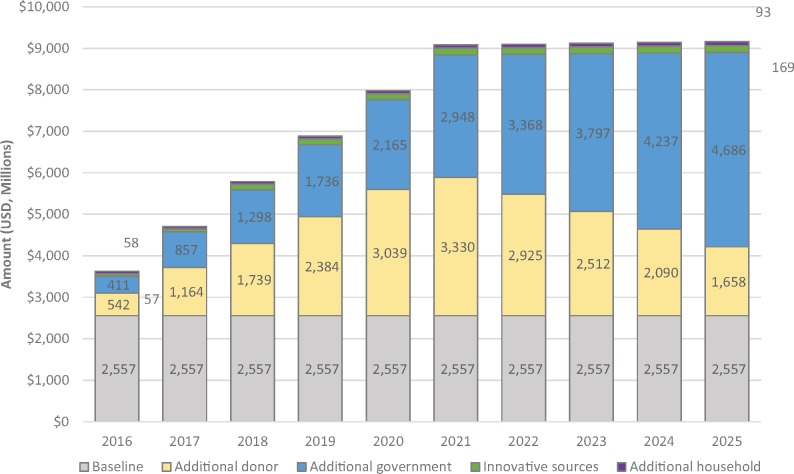
Based on these estimates of current expenditure, if the global goal is to be achieved, financing for KIPS would have to more than quadruple to about US$7.4 billion a year on average in order to mobilize the additional $49.5 billion required over a decade. About US$2.45 billion per year would be required to maintain current financing levels and about US$4.9 billion a year on average would be needed to cover the cost of the scale-up of KIPS (about US$3.2 billion of additional financing on average during the first 5 years and about US$6.6 billion on average during the following 5 years). However, under the business as usual scenario only US$9.8 billion more would be mobilized over 10 years, leaving a funding shortfall of US$39.2 billion (Figure 4).
Figure 4.
Future financing projections for nutrition under assumptions of business as usual (USD millions)
In order to close the funding gap, under the assumption of the ‘global solidarity’ scenario, country governments would need to provide an additional US$25.5 billion over 10 years, traditional donors would need to contribute an extra US$21.4 billion, households would need to provide US$0.7 billion more, and innovative sources–another US$1.4 billion. This would require high burden country governments to increase their share of projected government health spending for the KIPS from 0.7% to 3.2%, while donors would need to increase expenditures for KIPS from an average of 0.3% to 2.1% of estimated total ODA by 2021, after which donor spending for nutrition would taper to 1.1% of total aid by 2025 (see Figure 5; Supplementary data S5 for details).
Figure 5.
Future financing projections for nutrition under assumptions of global solidarity (USD million)
Discussion
This paper–part of a larger effort to develop a global financing framework for nutrition (Shekar et al. 2016), makes two important contributions to the extant literature. First, it provides estimates of the financing needed to reach the global stunting target by calculating the cost of scaling up key nutrition-specific intervention and linking them to the expected impact they may be expected to have on stunting prevalence in low and middle income countries. Second, it develops scenarios for scaling up financing to reduce stunting. This analysis shows that significant investments in both KIPS and the enabling environment are required in order to achieve the target.
Our cost estimates are consistent with the extant literature (Horton et al. 2010; Bhutta et al. 2013). However, unlike previous studies, which estimated the cost of scaling up from current coverage to 90% in a comparative statics context (without a time dimension), we model a scale-up over 10 years, which we believe is more realistic form programming perspective and allows us to incorporate population change dynamics. Furthermore, we model the declines in stunting prevalence over 10 years, rather than assume a given level of decline. In contrast to previous studies, our estimates show higher costs for Sub-Saharan Africa than for South Asia. It is so for three reasons. First, we exclude the cost of interventions targeting the treatment of wasting, of which countries in South Asia bear a greater burden. It should be noted that the treatment of severe wasting accounts for a large proportion of the cost in both Bhutta et al. (2013) and Horton et al. (2010) estimates (27% and 22%, respectively) and, in both studies, accounts for a substantial proportion of the overall mortality reductions.
Second, the average unit costs of the interventions extracted from the literature and program documentation tend to be higher in Sub-Saharan Africa. Third, the estimated target populations for the two of the three most costly interventions–public provision of complementary foods and balanced energy-protein supplementation are actually larger in absolute terms in Africa than in South Asia. Furthermore, population growth rate projections are higher for Africa than for South Asia, which means that even with the same scale up, the total cost will increase faster in Africa.
Our study includes three interventions which currently are not implemented at scale: prophylactic zinc supplementation, balanced energy protein supplementation and multiple micronutrient supplementation in pregnancy. We included these interventions, because without them it would not be possible to reach the global stunting target. However, it needs to be emphasized that currently, they are not ready for scale-up. Appropriate delivery platforms need to be identified for prophylactic zinc supplementation. Balanced energy-protein supplementation for vulnerable women and multiple micronutrient supplementation can be delivered through existing platforms (e.g. social safety nets and ante-natal care, respectively). However, international and national guidelines need to be developed and adopted to make scale-up possible.
The impact of zinc supplementation was modelled based on the systematic literature review by Yakoob and colleagues (Yakoob et al. 2011). More recent reviews show smaller effects on all-cause mortality (Mayo-Wilson et al. 2014) and inconsistent effects on cognitive development (Gogia and Sachdev 2012). Furthermore, effectiveness of delivery platform other than community distribution (e.g. water fortification, staple fortification, bio-fortification) is currently being investigated (e.g. Fink and Heitner 2014). Because prophylactic zinc supplementation is a significant cost driver and accounts for a substantial proportion of the modelled reductions in stunting prevalence, future studies should further explore the impact of zinc supplementation on linear growth and examine viability, cost and cost-effectiveness of different methods of delivering this intervention at scale.
Other interventions that are not ready for scale-up are those for which evidence for impact on stunting is not clear (such as de-worming or such as calcium supplements for women). These were not included in this study, but can be added to our estimates as the evidence base grows.
We assumed the unit costs of nutrition interventions to be fixed over the coming decade. Some studies suggest that marginal costs of providing child health services change with scale and over time (Johns et al. 2013). However, to date there has been no empirical studies of changes in unit cost of nutrition interventions either at the facility or at the country-level. Future analyses should assess how unit cost change over time, and how new delivery models and technologies could increase efficiency and reduce cost of delivering nutrition interventions. It is especially important to improve technical efficiency (making these interventions cheaper to deliver) of the most costly interventions and to ensure efficiency by appropriate allocation of funding across different interventions in a way that maximizes their impact while minimizing the costs.
The additional financing required under the ‘global solidarity’ scenario to achieve the global stunting target will require large efforts by all stakeholders. For the governments in high burden countries, it will be challenging to allocate, on average, 3% of their health budgets to stunting-related nutrition activities. While this level of domestic spending is ambitious, we see it as achievable. High burden countries have 10 years to gradually boost their budget shares for KIPS, so if they start early and sustain their efforts, the year-on-year rate of increase is manageable.
For external funders, meeting the stunting target financing needs will require a greater emphasis on allocation and budgeting decisions. In the ‘global solidarity’ scenario, donors are projected to raise substantially their share of development assistance for health devoted to stunting reduction. For some donors like Japan and Canada which already contribute over 11% of health ODA for basic nutrition, the challenge will be easier to meet. At present, 13 OECD donors are providing less than US$1 million each in direct bilateral aid for nutrition,7 and may thus need to shift their priorities toward investments in stunting reduction. New and innovative sources of external financing, including Power of Nutrition and GFF, which leverage traditional financing to access new philanthropic and private funding, will also be crucial to help fill the gap.
While the additional US$49.5 billion for KIPS scale-up over the next 10 years represents a large price tag to achieve the global goal, the recent history of global resource mobilization for the fight against HIV/AIDS can serve as an instructive precedent . In 1998, when the AIDS epidemic was raging, low and middle income countries were spending around US$500 million annually to fight the disease. Fifteen years later, nearly US$20 billion is being spent each year in these countries on HIV control, more than half of which is from LMIC governments (UNAIDS 2013).
It needs to be noted that increases in the international funding for HIV/AIDS were unprecedented. Furthermore, they were, perhaps to a large extent, motivated by arguments that uncontrolled HIV/AIDS epidemic in Africa and the developing world would pose a direct threat to the developed countries. Finally, recent estimates suggest that ODA has plateaued and will likely increase by only about 1.2% per year over the next three decades (Dieleman et al. 2016). Therefore, the historical trajectory of HIV/AIDS financing may not be directly applicable to nutrition. Nevertheless, this paper makes an argument that increases in ODA for are necessary if the SDG stunting target is to be met.
There are some important limitations to our study. Estimated financing needs do not include the costs of nutrition-sensitive interventions in agriculture, education, social protection and other sectors. In our study, we explicitly modelled the impact of WASH interventions targeting hygiene behaviors (handwashing with soap, hygienic disposal of children’s stool) and improvements in access to water and sanitation (access to improved sanitation and improve water sources and water connection at home). The cost of scaling up those interventions has been calculated elsewhere–Hutton and Varughese (2016) estimate that reaching the SGD WASH targets would require USD 28.4 billion per year between 2016 and 2030. We did not include them here, because our cost estimates have been developed from the health system perspective while WASH costs will likely be borne by water and infrastructure sectors as part of achieving the SDG water and sanitation targets.
Because the evidence of the impact of nutrition-sensitive interventions in other sectors, including agriculture and food security, education, and women’s health and empowerment is limited and impact modelling was not possible, we did not include them directly in our study. Instead, we modelled the impact of the improvements in the underlying determinants of undernutrition, including food availability diversity, and improvements in women’s health, education, and empowerment, assuming that they would result from nutrition-sensitive interventions and programs. However, our analyses clearly indicate that that investments in both nutrition-specific and nutrition-sensitive actions are needed to reach the global stunting target.
This study presents incremental cost of scaling up nutrition-specific interventions in low and middle income countries. It assumes that the coverage expansion will use the existing health systems and that the capacity for the scale up either exists already or will expand sufficiently over the next decade to accommodate this scale-up. However, it needs to be noted that currently, especially in the lower income countries, health system capacity is severely constrained and without health system strengthening, a rapid expansion of nutrition interventions will not possible.
The impact estimates used in our analysis are based on controlled experiments, which are usually conducted at a small scale and devote significant resources to ensuring high quality of service delivery, high fidelity to treatment protocols, and additional training and supervision for health workers. It is likely that the impact of the interventions provided at scale through public health and nutrition systems will be smaller than the modelling results presented here. Nevertheless, we believe that the results presented above can be interpreted as a reasonable upper bound estimates based on the most up-to-date scientific evidence.
Finally, data on government financing for nutrition remains limited despite recent efforts, with data currently available for only 31 countries, derived mainly from aspirational plans or budgets rather than actual expenditures. Furthermore, government and donor financing estimates are rarely disaggregated to the intervention level. We have addressed this problem by estimating the proportion of spending that is currently contributed to KIPS based on the review of national plans and donor project documentation. However, it is clear that allocation and expenditure tracking for nutrition needs to be improved both at the national and at the international levels.
Conclusions
Child stunting is a silent emergency of a magnitude as large as that of the AIDS epidemic, affecting 159 million children with negative consequences in terms of greater risk of illness and death, reduced cognitive ability, poor learning outcomes and poverty. The benefits of reducing child stunting can more than offset the extra cost, with a return of US$18 for every dollar invested (Hoddinott et al. 2013). As we stand at the cusp of the new SDGs, with global poverty rates having declined to < 10% for the first time in history (World Bank 2015), we now have an unprecedented opportunity to save children’s lives, build future human capital and drive faster economic growth by improving nutrition and tackling stunting. The cost is nearly US$50 billion over 10 years, but the costs of inaction are likely significantly larger.
Supplementary data
Supplementary data are available at HEAPOL online.
Supplementary Material
Acknowledgements
The funding for this work was provided by the Bill and Melinda Gates Foundation, Children’s Investment Fund Foundation, and World Bank. We are grateful to our partner Lucy Sullivan and her team at 1000 Days. We thank all members of the Technical Advisory Group for their valuable guidance: Victor Aguayo, Obey Assery, Robert Black, Hugh Bagnall-Oakeley, Helen Connolly, Kaia Engesveen, Patrizia Fracassi, Lawrence Haddad, Sue Horton, Ramanan Laxminarayan, Ferew Lemma, Saul Morris, Sandra Mutuma, Kelechi Ohiri, Ellen Piwoz, Amanda Pomeroy, and Bill Winfrey. Additionally, we are grateful to Robert Greener and Clara Picanyol for their contributions to the global government spending analysis and to Thu Do for her assistance on the household spending analysis.
Conflict of interest statement. None declared.
Notes
The following countries were included in the sample: Sub-Saharan Africa: Benin, Burundi, Central African Republic, Democratic Republic of the Congo, Eritrea, Ethiopia, Kenya, Liberia, Madagascar, Malawi, Mozambique, Niger, Nigeria, Rwanda, Sierra Leone, Somalia, Sudan, Tanzania, Uganda, Zambia; East Asia and the Pacific: Cambodia, China, Indonesia, Lao People’s Democratic Republic, Myanmar, Papua New Guinea, Philippines, Timor Leste, Vietnam; Latin America and the Caribbean: Guatemala, Mexico; Middle East and North Africa: Egypt, Yemen; South Asia: Bangladesh, India, Nepal, Pakistan.
This scale-up scenario was used to allow for the full accrual of the benefits of the interventions affecting stunting, which are delivered during the first 5 years of a child’s life. In particular, full program coverage needed to be maintained for 5 years in order for the impact model (LiST) to take into account the cohort effect. LiST uses a cohort model, in which the likelihood of stunting depends on interventions, risk factors, and whether or not the child was stunted in the previous year. Because of this, in a given year, a child benefits from all interventions it received in this year (direct impact of interventions) and in all previous years (indirect impact of interventions through reduced risk of stunting in previous years). Therefore, once all interventions are scaled up to maximum coverage (100%), it will take 5 years for the cohort of 0–5 year-olds to accrue full benefits of the interventions.
We did not estimate the cost of these improvements because they are more general and more difficult to cost than specific interventions and because they will likely occur independently of direct investments in nutrition. For recent cost estimates of scaling up WASH see: Hutton, G. 2015. Benefits and Costs of the Water and Sanitation Targets the Post-2015 Development Agenda. Copenhagen Consensus Center Working Paper. [Accessed December 1, 2015].
While it is included in the cost estimates, the estimates for financing and the following financing scenarios do not include financing for intermittent preventive treatment in pregnancy. This exclusion is due to the fact that these interventions are typically funded outside of nutrition programs.
The additional CRS codes reviewed included: 12220 Basic health care; 12250 Infectious disease; 12261 Health education; 12281 Health personnel development; 13020 Reproductive health; 13081 Personnel development for population & reproductive health; 51010 General budget support-related aid; 52010 Food aid/food security programmes; 53030 and 53040 Import support; 72010 Material relief assistance and services; 72040 Emergency food aid; 72050 Relief co-ordination; 73010 Reconstruction relief and rehabilitation; 74010 Disaster prevention and Preparedness.
At the Nutrition for Growth (N4G) Summit in 2013, donors pledged US$4.15 billion in support of nutrition-specific programs by 2020. We assumed about half of the commitments for nutrition-specific investments made at N4G 2013 are realized (US$2.07 billion). We then attributed financing for KIPS proportional to current donor investments within the basic nutrition code.
Austria, Czech Republic, Finland, Greece, Iceland, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, South Korea, Switzerland. International Food Policy Research Institute. 2015. Global Nutrition Report 2015: Actions and accountability to advance nutrition and sustainable development. Washington, DC. http://dx.doi.org/10.2499/9780896298835.
References
- Bhutta ZA, Ahmed T, Black RE. et al. 2008. What works? Interventions for maternal and child undernutrition and survival. The Lancet 371: 417–40. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Das JK, Rizvi A. et al. 2013. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet 382: 452–77. [DOI] [PubMed] [Google Scholar]
- Rannan-Eliya R.P., Anuranga C, Chandrasiri R, Hafez R, Kasthuri G, Wickramasinghe R, Jayanthan J. 2012. Impact of out-of-pocket expenditures on families and barriers to use of maternal and child health services in Asia and the Pacific: Evidence from national household surveys of healthcare use and expendituressummary technical report. Mandaluyong City, Philippines: Asian Development Bank. https://www.adb.org/sites/default/files/publication/30345/impact-oop-expenditures-mnch-services-asia-pacific.pdf. [Google Scholar]
- Eisele TP, Larsen D, Steketee RW.. 2010. Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. International Journal of Epidemiology 39: i88–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink G, Heitner J.. 2014. Evaluating the cost-effectiveness of preventive zinc supplementation. BMC Public Health 14: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner P, Gülmezoglu AM.. 2006. Drugs for preventing malaria in pregnant women. Cochrane Database of Systematic Reviews 4, (CD000169) doi: 10·1002/14651858. CD000169. pub2. [DOI] [PubMed] [Google Scholar]
- Gogia S, Sachdev HS.. 2012. Zinc supplementation for mental and motor development in children. Cochrane Databasre of Systematic Reviews doi: 10·1002/14651858. CD007991. pub2. [DOI] [PubMed] [Google Scholar]
- Haider BA, Bhutta ZA.. 2015. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 14: CD004905.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider BA, Yakoob MY, Bhutta ZA.. 2011. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public Health 11(Suppl 3): S19.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S.. 2013. The economic rationale for investing in stunting reduction. Maternal and Child Nutrition 9: 69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott J, Maluccio J, Behrman JR. et al. 2011. The Consequences of Early Childhood Growth Failure over the Life Course. Washington, DC: International Food Policy Research Institute Discussion Paper 1073. [Google Scholar]
- Hoddinott J, Maluccio JA, Berhman JR, Flores R, Martorell R.. 2008. Effects of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. The Lancet 371: 411–6. [DOI] [PubMed] [Google Scholar]
- Horton S, Hoddinott J.. 2015. Benefits and Costs of the Food and Nutrition Targets for the Post-2015 Development Agenda. Copenhagen Consensus Center Working Paper.http://www.copenhagenconsensus.com/sites/default/files/food_security_and_nutrition_perspective_-_horton_hoddinott_0.pdf, accessed 1 December 2015.
- Horton S, Shekar M, McDonald C, Mahal A, Brooks JK.. 2010. Scaling Up Nutrition: What Will it Cost? Washington, DC: The World Bank. [Google Scholar]
- Horton S, Steckel R.. 2013. Global Economic Losses Attributable to Malnutrition 1900–2000 and Projections to 2050 In: Lomborg B. (ed). The Economics of Human Challenges. Cambridge, U.K: Cambridge University Press, 247–72. [Google Scholar]
- Hutton G. 2015. Benefits and costs of the water and sanitation targets for the post-2015 development agenda. Copenhagen Consensus Center Working Paper, accessed 1 December 2015.
- Hutton G, Varughese M.. 2016. The Costs of Meeting the 2030 Sustainable Development Goal Targets on Drinking Water, Sanitation, and Hygiene. Water and Sanitation Program Technical Paper 103171. http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2016/02/08/090224b08415 bdca/1_0/Rendered/PDF/The0costs0of0m0itation00and0hygiene.pdf.
- Imdad A, Bhutta ZA.. 2011. Effect of balanced protein energy supplementation during pregnancy on birth outcomes. BMC Public Health 11: S17.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imdad A, Bhutta ZA.. 2011. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: a meta-analysis of studies for input to the lives saved tool. BMC Public Health 11: S22.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imdad A, Bhutta ZA.. 2012. Maternal nutrition and birth outcomes: effect of balanced protein-energy supplementation. Paediatric and Perinatal Epidemiology 26: 178–90. [DOI] [PubMed] [Google Scholar]
- Imdad A, Herzer K, Mayo-Wilson E, Yakoob MY, Bhutta ZA.. 2010. Vitamin A supplementation for preventing morbidity and mortality in children from 6 months to 5 years of age. Cochrane Database of Systematic Reviews 12: (CD008524). [DOI] [PubMed] [Google Scholar]
- Imdad A, Yakoob MY, Bhutta ZA.. 2011. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health 11: S25.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imdad A, Yakoob MY, Sudfeld CR. et al. 2011. Impact of vitamin A supplementation on infant and childhood mortality. BMC Public Health 11: S20.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Food Policy Research Institute. 2015. Global Nutrition Report 2015. Washington, DC: Actions and Accountability to Advance Nutrition and Sustainable Development, http://dx.doi.org/10.2499/9780896298835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns B, Munthali S, Walker D, Masanjala W, Bishai D.. 2013. A cost function analysis of child health services in four districts of Malawi. Cost Effectiveness and Resource Alocation 11: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi ZS, Zahid GS, Das JK, Bhutta ZA.. 2013. Impact of complementary food and education on complementary food on growth and morbidity of children less than 2 years of age in developing countries: a systematic review. BMC Public Health 13: S13.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leive A, Xu K.. 2008. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bulletin of the World Health Organization 86: 849–56C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lives Saved Tool (LiST). 2015. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health. http://livessavedtool.org/. accessed 31 December 2015.
- Lu WP, Lu MS, Li ZH, Zhang CX.. 2014. Effects of multimicronutrient supplementation during pregnancy on postnatal growth of children under 5 years of age: a meta-analysis of randomized controlled trials. PLoS One 9: e88496.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martorell R, Horta BL, Stein AD. et al. 2010. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analysis from 5 birth cohorts from low- and middle-income countries. Journal of Nutrition 140: 348–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo-Wilson E, Junior JA, Imdad A. et al. 2014. Zinc Supplementation for Preventing Death and Disease, and for Growth, in Children Aged Six Months to 12 Years of Age. Cochrane Database of Systematic Reviews. [DOI] [PubMed]
- Pena-Rosas JP, De-Regil LM, Garcia-Casal MN. et al. 2015. Daily oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 12: CD004736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power of Nutrition. 2015. Our Investments. http://www.powerofnutrition.org/our-investments/, accessed 31 December 2015.
- Radeva-Petrova D, Kayentao K, ter Kuile FO, Sinclair D, Garner P.. 2014. Drugs for preventing malaria in pregnant women in endemic areas: any drug regimen versus placebo or no treatment. Cochrane Database of Systematic Reviews 10: (CD000169). doi: 10.1002/14651858.CD000169. pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rannan-Eliya R.P., Anuranga C, Chandrasiri R, Hafez R, Kasthuri G, Wickramasinghe R, Jayanthan J. 2012. Impact of out-of-pocket expenditures on families and barriers to use of maternal and child health services in Asia and the Pacific: Evidence from national household surveys of healthcare use and expenditures—summary technical report. Mandaluyong City: Philippines: Asian Development Bank; https://www.adb.org/sites/default/files/publication/30345/impact-oop-expenditures-mnch-services-asia-pacific.pdf. [Google Scholar]
- Ruel M, Aldernal H. the Maternal Child Nutrition Study Group 2013. Nutrition-sensitive interventions and programmes: how can they help accelerate progress in improving maternal and child nutrition? The Lancet 382: 66–81. [DOI] [PubMed] [Google Scholar]
- Scaling Up Nutrition (SUN). 2014. Planning and costing for the acceleration of actions for nutrition: experiences of countries in the Movement for Scaling up Nutrition. http://scalingupnutrition.org/wp-content/uploads/2014/05/Final-Synthesis-Report.pdf. accessed 31 December 2015.
- Shekar M, Kakietek J, Dayton Eberwein J, Walters D.. 2016. An Investment Framework for Nutrition. Washington DC: The World Bank Group. [Google Scholar]
- Shekar M, McDonald C, Subandoro A, Dayton Eberwein J, Mattern M, Akuoku J.. 2014. Costed plan for scaling up nutrition: Nigeria Health, Nutrition and Population (HNP) Discussion Paper. Washington, DC: The World Bank Group. [Google Scholar]
- Shekar M, Mattern M, Laviolette L, Dayton Eberwein J, Karamba W, Akuoku J.. 2015a. Scaling Up Nutrition in the DRC: What Will It Cost? Health, Nutrition and Population (HNP) Discussion Paper. Washington, DC: The World Bank Group. [Google Scholar]
- Shekar M, Mattern M, Eozenou P. et al 2015b. Scaling up nutrition for a more resilient mali: nutrition diagnostics and costed plan for scaling up Health, Nutrition and Population (HNP) Discussion Paper. Washington, DC: The World Bank Group. [Google Scholar]
- Siekmann J, Timmer A, Irizarry L.. 2012. Home Fortification Using Market-Based Approaches to Complement Free Public Distribution of Micronutrient Powders. Washington (DC: ): Home Fortification Technical Advisory Group; 5p. Supported by the World Food Programme. [Google Scholar]
- Singha B, Chowdury R, Sankar MJ. et al. 2015. Interventions to improve breastfeeding outcomes: a systematic review and meta-analysis. Acta Pediatrica 104: 114–34. [DOI] [PubMed] [Google Scholar]
- Smith LC, Haddad L.. 2015. Reducing child undernutrition: past drivers and priorities for the post-MDG Era. World Development 68: 180–204. [Google Scholar]
- Suchdev PS, Shah A, Jefferds ME. et al. 2013. Sustainability of market‐based community distribution of Sprinkles in western Kenya. Maternal & Child Nutrition 1 9: 78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF. 1990. A UNICEF Policy Review: Strategy for Improved Nutrition for Children and Women in Developing Countries. New York: UNICEF. [Google Scholar]
- UNICEF, WHO and World Bank. 2015. Joint child malnutrition estimates. Global Database on Child Growth and Malnutrition. http://www.who.int/nutgrowthdb/estimates2014/en/. accessed October 2015.
- United Nations, Department of Economic and Social Affairs, Population Division. 2015. World Population Prospects: The 2015 Revision, Key Findings and Advance Tables. Working Paper No. ESA/P/WP.241 and United Nations, Department of Economic and Social Affairs, Population Division. 2015. World Population Prospects: The 2015 Revision, custom data acquired via website: http://esa.un.org/unpd/wpp/DataQuery/.
- United Nations Programme on HIV/AIDS (UNAIDS). 2013. Global Report: UNAIDS report on the global AIDS epidemic 2013. WHO Library Cataloguing-in-Publication Data.
- Victora C, Bahl R, Barros A. et al. 2016. Breastfeeding in the 21st Century: epidemiology, mechanisms and lifelong effect. The Lancet 287: 475–90. [DOI] [PubMed] [Google Scholar]
- World Bank. 2015. Global Monitoring Report 2015 http://www.worldbank.org/en/publication/global-monitoring-report. accessed 31 December 2015.
- Yakoob MY, Theodoratou E, Jabeen A. et al. 2011. Preventive zinc supplementation in developing countries: impact on mortality and morbidity due to diarrhea, pneumonia and malaria. BMC Public Health 11: S23.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.