Abstract
Objective
This study tested the effectiveness of a brief, learner-centered, breaking bad news (BBN) communication skills training module using objective evaluation measures.
Methods
This randomized control study (N=66) compared intervention and control groups of students (n=28) and residents' (n=38) objective structured clinical examination (OSCE) performance of communication skills using Common Ground Assessment and Breaking Bad News measures.
Results
Follow-up performance scores of intervention group students improved significantly regarding BBN (colon cancer (CC), p=.007, r=-.47; breast cancer (BC), p=.003, r=-.53), attention to patient responses after BBN (CC, p < .001, r=-.74; BC, p=.001, r=-.65), and addressing feelings (BC, p=.006, r=-.48). At CC follow-up assessment, performance scores of intervention group residents improved significantly regarding BBN (p=.004, r=-.43), communication related to emotions (p=.034, r=-.30), determining patient's readiness to proceed after BBN and communication preferences (p=.041, r=-.28), active listening (p=011, r=-.37), addressing feelings (p<.001, r=-.65), and global interview performance (p=.001, r=-.51).
Conclusion
This brief BBN training module is an effective method of improving BBN communication skills among medical students and residents.
Practice Implications
Implementation of this brief individualized training module within health education programs could lead to improved communication skills and patient care.
Keywords: breaking bad news, communication skills training, stories, narrative, common ground assessment, qualitative, cancer, objective structured clinical examination (OSCE), education, empathy
1. Introduction
Historically patients with cancer were routinely left uninformed regarding their diagnosis [1,2]. This was done largely with the belief that informing patients was harmful and caused undue stress. As cancer treatments improved in the late 1970's, physician-centered models of care evolved to an increased focus on autonomy and most physicians more fully informed their patients about their cancer diagnosis [3]. However, with this change, came new communication challenges to both the patient and the treating physician [4-6].
“Bad news” has been defined by Buckman [7] as, “any news that drastically and negatively alters the patient's view of his or her future.” Examples of bad news include: cancer diagnosis, cancer recurrence, and treatment failure. Doctor-patient encounters involving breaking bad news (BBN) are important. When bad news is delivered poorly, it can negatively impact both patient and physician. Negative patient outcomes can include stress and anxiety [8]; miscommunication regarding diagnosis, treatment, and prognosis [9]; and poorer overall health outcomes [10]. Negative physician outcomes can include increased stress [11,12], anxiety [13], and burnout [14].
The Toronto and Kalamazoo Consensus Statements [15,16] made recommendations regarding communication skills in general practice. Recommendations involving challenging communication skills such as those found when delivering bad news were offered by Baile et al. [17] who described a six-step protocol, while Girgis and Swanson-Fisher [20] provided consensus guidelines. Training activities for BBN come in a variety of formats. Among these are lecture and small group discussion using role-play and/or standardized patients, instructional videos, and objective structured clinical examinations (OSCEs) [4,17-21].
BBN training is often labor intensive and time consuming, therefore many medical schools provide few formal learning experiences [10,17]. Where BBN training has been reported, these approaches can require up to forty hours [4,22-25].
Initial studies concerning BBN relied largely on participant self-report of increased knowledge and/or confidence while giving bad news [26]. Consequently, conclusions regarding the expression of BBN communication skills were limited. Although they are difficult to create and expensive to implement, OSCEs have been used in several studies [26-28]. More recently, randomized controlled studies evaluating the efficacy of BBN communication skills training have been conducted [25,29-32].
Recognizing these challenges to implementation and education, our study tested the effectiveness of a brief, self-paced, skill-focused BBN training module using objective evaluation measures. This module was developed using cancer stories from patients. It was the result of an interdisciplinary effort involving faculty from the East Tennessee State University (ETSU) Graduate Storytelling Program and the departments of Family and Internal Medicine.
2. Methods
2.1 Intervention
Training materials for the BBN module were developed using qualitative methods for discovering a variety of challenging experiences reported among patients with cancer. Semi-structured interviews were conducted, video recorded, transcribed verbatim, checked for accuracy by the original interviewer, and analyzed [33-34]. Each interview began with the statement, “Please begin by sharing any stories or personal experiences that might help others to appreciate what it has been like for you to deal with cancer.” After a patient shared their story, interviewers asked 1) questions to clarify issues related to communication (e.g. If the patient did not spontaneously mention something such as how the diagnosis was given, then the interviewer would inquire.) and 2) questions based on previous research and communication consensus reports (e.g. breaking bad news, end-of-life, decision-making, spirituality, etc.).
Transcripts were independently examined by at least two reviewers. Key concepts and themes that emerged from the data were coded. These reviewers compared and contrasted their independent coding and came to a consensus regarding the emerging themes. Following guidelines suggested by Kuzel [35], theme saturation was achieved after approximately 15 interviews. It was important from a pedagogic perspective that a representative variety of cancer types and exemplary quotes be obtained. Accordingly, a total of 112 interviews were transcribed, coded, and entered into NVivo 8 qualitative data analysis software [36]. Reliability and validity were maximized using four maneuvers: 1) interviews were transcribed verbatim, 2) interviewers took field notes during interviews to improve accuracy of data interpretation, 3) at least two reviewers independently examined and analyzed the data before this was presented to the module development team, and 4) member checking occurred for a sub-sample of the interview participants and the research team met for further synthesis and interpretation of the themes. This approach determined relationships between themes and provided exemplar quotes demonstrating the themes. The research team used these themes and quotes to develop the modules.
Five main themes emerged: 1) breaking bad news, 2) living through treatment, 3) palliative care and end-of-life care, 4) spirituality, and 5) family. Each theme became the emphasis of a training module designed to improve communication skills with patients with cancer. These modules were designed to be brief (60 minutes) and to actively engage learners. Interactivity between learners and modules was enhanced through video clips of patients, physicians, and family in the introduction of various communication skills. They also reinforced content themes, and evoked patient-centered, empathic responses among learners. These clips were selected by their authors as being salient to the goals and learning objectives of respective training modules.
The BBN module incorporated recommendations found within the literature [4,17,20,21] as well as selected video recordings of twenty-seven actual cancer patients who described challenging communications situations involving BBN. For example, one video clip presented a female patient who described feelings of shock, fear, and confusion upon hearing that she had cancer during the “delivery phase” [37] of this encounter. During this time she reported experiencing a “deafening silence”. This intense emotional response limited her ability to process information. This video clip highlighted the importance of pausing after delivering bad news in order to attend to a patient's emotional response before sharing additional information. In order to keep learners engaged, quiz questions were included every 5-10 minutes. Quizzes asked learners to imagine how they would respond to a patient in a challenging communication situation: “How would you respond to this patient? What would you say and do?” Simulated patient interviews using actors portraying doctors and patients were included to help learners identify effective communication skills during doctor-patient interactions. Annotations were used to emphasize communication techniques. Learners viewed the training module on a CD-ROM or website. Viewing time averaged 60 minutes.
2.2 Case Scenarios
The widely used OSCE format was chosen because it allowed for the simulation of multiple doctor-patient meetings in a standardized setting. It has demonstrated good reliability and validity with medical encounters found in general practice [38,39]. The OSCEs used in this study involved challenging scenarios found when delivering bad news with particular attention to communication skills recommended through consensus statements and guidelines specific to cancer [17,20,40]. Two 15-minute OSCE stations (breast cancer and colon cancer) were developed.
2.3 OSCE Standardized Patients and Raters
Standardized patient (SP) OSCE training was conducted by ETSU's SP Coordinator. SPs who delivered at least 90% of the OSCE clues accurately were assigned to the BBN OSCE. This level of reliability is similar to those reported in previous studies [39,41,42]. Each OSCE lasted approximately 15 minutes (7 minutes of chart review and 8 minutes of female SP interview). Three independent raters were recruited from this pool of SPs. Raters were assigned OSCE video recordings after they reached an a priori accuracy of 90%. Raters were blind to the participant's level of education, the OSCE interview sequence (baseline or follow-up), and group status (intervention or control).
2.4 OSCE Evaluation Measures
Communication skills were assessed using performance ratings in two OSCE scenarios. Two communication skills rating forms were used: the Breaking Bad News Skills rating form checklist (BBN Skills) which is a measure of specific BBN-related skills and the Common Ground Assessment Summary form (CGAS) [39], a validated measure of general communication skills.
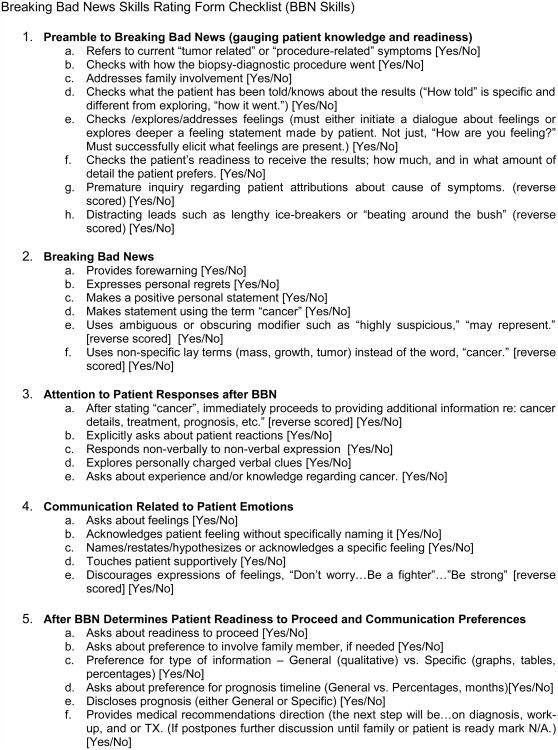
Figure 1 displays the BBN Skills form, a checklist comprised of five measures. Each measure is composed of several checklist items (no=0, yes=1) corresponding to the BBN training module learning objectives. The five measures are: 1. Preamble to Breaking Bad News (gauging patient knowledge and readiness), 2. Breaking Bad News, 3. Attention to Patient Responses after BBN, 4. Communication Related to Patient Emotions, and 5. After BBN Determines Patient Readiness to Proceed and Communication Preferences. The Preamble to Breaking Bad News measures the introduction portion of the interview in the context of a BBN visit. It determines whether and how an interviewer might avoid difficult issues. Breaking Bad News focuses on skills used while the bad news is delivered, but before the interview transitions into the information-sharing stage. It assesses whether forewarnings are used as well as how the bad news is expressed. Attention to Patient Responses after BBN examines interviewer's interactive behaviors related to patient's prior experiences, emotions, thoughts, and preferences before providing additional medical information. Communication Related to Patient Emotions determines whether and how the interviewer addressed emotions expressed by the SP throughout the OSCE. After BBN, Determines Patient Readiness to Proceed and Communication Preferences examines interview skills related to timing and the exploration and incorporation of patients' communication preferences, including the involvement of family or other supportive persons.
Figure 1. Breaking Bad News Skills Rating Form Checklist (BBN Skills).
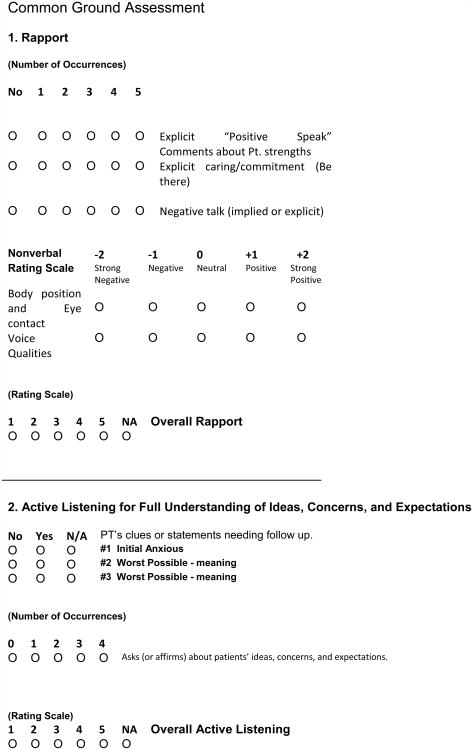
The CGAS (Figure 2) contains five summary scales (Overall Rapport, Overall Active Listening, Overall Deals with Feelings, Overall Closing, and Overall Global Interview). Lang et al. [39] reported that this measure provided “a reliable and valid assessment of patient-centered communications skills for everyday office visits, consistent with the expectations of the Toronto and Kalamazoo consensus statements.” The CGAS scales use a 5-point rating (1=needs improvement, 2=marginal, 3=competent/adequate, 4=very effective, 5=exemplary). As a means of increasing precision, raters were instructed to score half-point increments between rating points described by the scale.
Figure 2. Common Ground Assessment.
2.5 Research Participants and Procedure
The ETSU Institutional Review Board approved this study. All patient participants provided their written consent to use their personal cancer stories and experiences that demonstrate effective and ineffective cancer communication as part of educational modules to educate doctors to communicate more effectively with cancer patients.
A volunteer group of health professional students who were paid $100 participated in this study. They were enrolled in the colleges of medicine, pharmacy, or nursing and had completed the Communications Skills for Health Professionals course. A second group of participants was comprised of family medicine and internal medicine residents who completed the OSCEs as part of their usual academic exercises at the beginning of their first year of training. Their prior experience with communications skills training was unknown. The students and residents provided their written consent to video-record OSCE sessions with a standardized patient, and to complete a training module and a quiz on communication effectiveness.
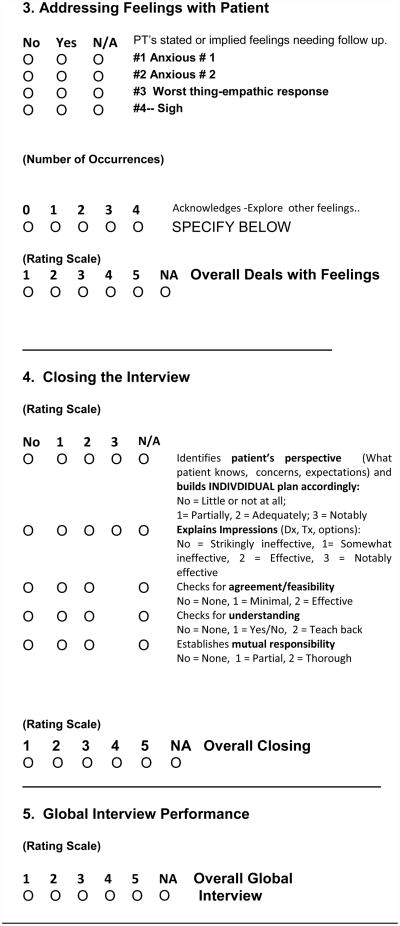
All 66 participants were randomly assigned to either an intervention group or a waiting list control group (Figure 3). To control for a possible order effect, students received a counterbalanced presentation of the OSCE (breast vs. colon cancer). The students assigned to the intervention arm of this study received the follow-up OSCE within seven days of their completion of BBN training module. The training of students in the control group was delayed for two weeks. Residents received the colon cancer scenario in both the baseline and follow-up OSCE. Residents assigned to the intervention group completed the training module one week after they completed the baseline OSCE and the follow-up OSCE within one month of the baseline OSCE. Training was delayed for residents assigned to the control group. They received each OSCE, spaced one month apart, before receiving the training module. OSCEs were rated using the CGAS and the BBN Skills Form. Differences in length of time between baseline OSCEs and follow-up OSCEs for students and residents were due to scheduling limitations within the residency programs and student availability. Ideally, students would have been assessed on schedule with residents (30 days between baseline and follow-up).
Figure 3. Data Collection Timeline and Demographics.
2.6 Analysis
The measures comprised within the BBN Skills Form were developed by summing the categorical checklist items within each of the scales. Although less than one percent of the data was missing, where this did occur, missing data from within the BBN Skills measures were imputed using the formula: (sum score of scale / number of valid items in scale multiplied by the number of total expected items in scale). Change scores for each measure were determined by subtracting the baseline OSCE score from the follow-up OSCE score. Mann-Whitney U tests were employed to compare change scores found between the intervention and control groups. The direction of change between intervention and control groups was hypothesized to be positive for all measures, so all statistical tests examining OSCE performance were one-tailed with an alpha level of .05. Effect sizes were calculated to determine the magnitude of the differences between baseline scores and follow-up scores. All statistical tests on demographic characteristics were two-tailed with an alpha level of .05. The analyses were performed with SPSS version 21 for PC [43].
3. Results
3.1 Participant Demographic Data and Baseline Assessment
The student group of 12 females and 16 males had an average age of 25.4 (Figure 3). As is typical of the demographic makeup of this region, most of this group self-identified as Caucasian (86%). Two students self-identified as Asian (7%) and two students Black (7%). No significant within group differences were detected based on student age [t (19.37) = 1.67, p = .111] or gender [χ2 (1) = .191, p = .662].
The resident group, 20 males and 18 females had an average age of 29.6. Twenty-one members of this group self-identified as Caucasian (55%), 14 Asian (37%), 2 Hispanic (5%), and 1 Native American (3%). A comparison of the intervention and the control groups of the residents, yielded no significant differences based on age [t (34) = -.27, p = .788] or gender [χ2 (1) = .12, p = .732]. However, residents were significantly older than students [t (62) = 3.34, p = .001] and were more likely to claim a non-Caucasian ethnic identifier [χ2 (1) = 6.89, p = .009].
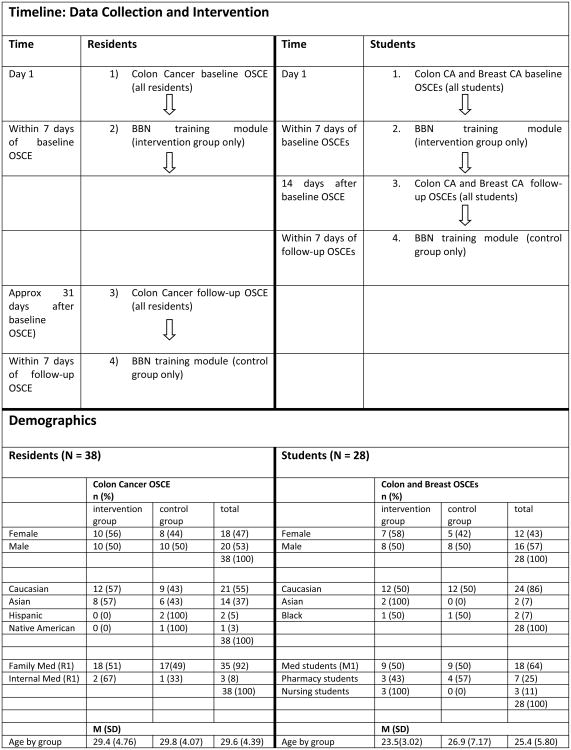
Table 2 provides a baseline assessment and comparison of students and residents using the BBN Skills rating measures and the Common Ground Assessment. Residents scored significantly higher than students on two of the ten measures: Preamble to Breaking Bad News (p <.001) and Rapport (p = .015).
Table 2.
Comparison between Student Group and Resident Group Baseline Scores on BBN Rating Form Scales and Common Ground Assessment (CGAS).
| Rating Scale | Students N = 28 | Residents N = 38 | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline scores M (SD) | Mean rank | Baseline scores M (SD) | Mean rank | U | Z | r (effect-size) | p | |
| Colon - BBN OSCE Rating Form Scales | ||||||||
| 1. Preamble to Breaking Bad News | 2.37 (0.63) | 23.35 | 3.11 (0.97) | 39.86 | 252.50 | -3.66 | -.45 | <.001*** |
| 2. Breaking Bad News | 3.46 (0.90) | 28.10 | 3.83 (0.99) | 35.51 | 379.50 | -1.65 | -.20 | .100 |
| 3. Attention to Patient Responses After BBN | 1.92 (1.43) | 30.65 | 2.16 (1.04) | 34.67 | 449.50 | -.871 | -.11 | .384 |
| 4. Communication Related to Patient Emotions | 2.93 (1.11) | 33.57 | 2.89 (0.90) | 32.59 | 497.50 | -.217 | -.03 | .828 |
| 5. After BBN, Determines Patient Readiness to Proceed and Communication Preferences | 3.02 (1.38) | 34.89 | 2.60 (1.09) | 31.66 | 462.00 | -.690 | -.08 | .491 |
| Colon - Common Ground Assessment Scales | ||||||||
| 1. Rapport | 2.72 (.68) | 26.41 | 3.16 (.57) | 37.68 | 335.00 | -2.44 | -.30 | .015* |
| 2. Active Listening | 2.72 (.58) | 37.15 | 2.50 (.52) | 30.05 | 401.00 | -1.55 | -.19 | .121 |
| 3. Addressing Feelings with Patient | 2.91 (.69) | 29.83 | 3.07 (.45) | 35.25 | 427.50 | -1.20 | -.15 | .229 |
| 4. Closing the Interview | 2.67 (.57) | 27.74 | 2.97 (.53) | 35.97 | 371.00 | -1.86 | -.23 | .063 |
| 5. Global Interview Performance | 2.67 (.67) | 29.52 | 2.84 (.55) | 35.47 | 419.00 | -1.31 | -.16 | .198 |
Note:
p <.05,
p <.01,
p <.001.
All tests were two-tailed using Mann-Whitney U test.
3.2 Effects of BBN Training on Student and Resident OSCE Performance
Most OCSE change scores of students were significantly higher for the intervention group as compared to the control group. Statistically significant differences were found in both the colon and the breast cancer OSCEs (Table 1). On the colon cancer OSCE, significant improvement was found on two of the BBN Skills measures: Breaking Bad News (p = .007; effect size r = -.47) and Attention to Patient Responses after BBN (p < .001; r = -.74). On the breast cancer OSCE, significant improvement was found on three of the BBN Form measures: Breaking Bad News (p = .003; r = -.53), Attention to Patient Responses after BBN (p = .001; r = -.65), and Communication Related to Patient Emotions (p = .043; r = -.33). Using the CGAS, the Addressing Feelings scale was significantly higher in the intervention group on the breast cancer OSCE (p = .006; r = -.48). Although students who received the breast cancer OSCE had significantly higher scores than the control group on the Communication Related to Patient Emotions and Addressing Feelings with Patient scales, these differences were not significant with students who completed the colon cancer OSCE.
Table 1. BBN OSCE Results for Students and Residents.
| BBN Colon Cancer and Breast Cancer OSCEs for Students (N = 28) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control Group n = 13 | Intervention Group n = 15 | Mann-Whitney test Change Scores: Control vs. Intervention | ||||||||||
| Rating Scale | baseline M (SD) | follow-up M (SD) | change score | Change Scores Mean rank | baseline M (SD) | follow-up M (SD) | change score | change scores mean rank | U | Z | r (effect-size) | p |
| Colon - BBN Skills Rating Form | ||||||||||||
| 1. Preamble to Breaking Bad News | 2.31(.48) | 2.31(.63) | .00 | 12.15 | 2.43(.76) | 2.80(.86) | .37 | 15.71 | 67.00 | -1.31 | -.25 | .095 |
| 2. Breaking Bad News | 3.38(.77) | 3.27(.97) | -.11 | 9.92 | 3.54(1.05) | 4.60(.74) | 1.06 | 17.08 | 38.00 | -2.48 | -.47 | .007** |
| 3. Attention to Patient Responses After BBN | 2.29(1.22) | 2.25(.1.27) | -.04 | 7.96 | 1.57(1.55) | 3.38(1.24) | 1.81 | 19.61 | 12.50 | -3.92 | -.74 | <.001*** |
| 4. Communication Related to Patient Emotions | 2.69(.95) | 2.85(.99) | .16 | 14.54 | 3.14(1.23) | 3.23(1.14) | .11 | 13.50 | 84.00 | -.36 | -.07 | .361 |
| 5. After BBN, Determines Patient Readiness to Proceed and Communication Preferences | 3.40(1.32) | 3.23(1.22) | -.17 | 11.65 | 2.67(1.39) | 3.27(1.46) | .60 | 16.18 | 60.50 | -1.49 | -.28 | .069 |
| Colon - Common Ground Assessment Scales | ||||||||||||
| 1. Rapport | 2.54(.69) | 2.65(.92) | .11 | 13.31 | 2.89(.66) | 3.13(.58) | .24 | 14.64 | 82.00 | -.45 | -.09 | .325 |
| 2. Active Listening | 2.81(.48) | 2.92(.40) | .11 | 11.65 | 2.64(.66) | 3.07(.55) | .43 | 15.35 | 60.50 | -1.31 | -.25 | .095 |
| 3. Addressing Feelings with Patient | 2.77(.56) | 3.08(.45) | .31 | 13.88 | 3.04(.80) | 3.32(.42) | .24 | 13.12 | 79.50 | -.27 | -.05 | .392 |
| 4. Closing the Interview | 2.58(.61) | 2.85(.66) | .27 | 12.50 | 2.75(.55) | 3.20(.56) | .45 | 15.39 | 71.50 | -.99 | -.19 | .163 |
| 5. Global Interview Performance | 2.50(.58) | 2.65(.77) | .15 | 11.81 | 2.82(.72) | 3.25(.55) | .43 | 15.19 | 62.50 | -1.16 | -.22 | .123 |
| Breast - BBN Skills Rating Form | ||||||||||||
| 1. Preamble to Breaking Bad News | 2.74(1.64) | 2.53(.66) | -.21 | 14.00 | 2.53(.64) | 2.80(.86) | .27 | 14.93 | 91.00 | -.33 | -.06 | .371 |
| 2. Breaking Bad News | 2.92(1.19) | 3.46(.66) | .54 | 10.00 | 2.73(1.22) | 4.73(.59) | 2.00 | 18.40 | 39.00 | -2.78 | -.53 | .003** |
| 3. Attention to Patient Responses After BBN | 2.98(.89) | 2.90(1.47) | -.08 | 8.85 | 1.61(1.11) | 4.02(1.01) | 2.41 | 19.40 | 24.00 | -3.43 | -.65 | .001** |
| 4. Communication Related to Patient Emotions | 3.23(.73) | 3.38(1.12) | .15 | 11.69 | 3.07(.96) | 4.13(.99) | 1.06 | 16.93 | 61.00 | -1.72 | -.33 | .043* |
| 5. After BBN, Determines Patient Readiness to Proceed and Communication Preferences | 2.98(1.35) | 3.10(1.42) | .12 | 12.19 | 2.17(1.17) | 3.43(1.62) | 1.26 | 16.50 | 67.50 | -1.39 | -.26 | .083 |
| Breast - Common Ground Assessment Scales | ||||||||||||
| 1. Rapport | 2.62 (.68) | 2.85(.83) | .23 | 13.00 | 2.87(.61) | 3.40(.66) | .53 | 15.80 | 78.00 | -.92 | -.17 | .179 |
| 2. Active Listening | 2.88(.42) | 3.04(.66) | .16 | 12.42 | 2.57(.56) | 3.10(.57) | .53 | 16.30 | 70.50 | -1.29 | -.24 | .099 |
| 3. Addressing Feelings with Patient | 3.35(.47) | 3.31(.63) | -.04 | 10.58 | 3.10(.47) | 3.73(.56) | .63 | 17.90 | 46.50 | -2.53 | -.48 | .006** |
| 4. Closing the Interview | 2.69(.52) | 2.96(.72) | .27 | 13.23 | 2.90(.66) | 3.40(.83) | .50 | 15.60 | 81.00 | -.785 | -.15 | .216 |
| 5. Global Interview Performance | 2.62(.55) | 2.92(.86) | .30 | 11.92 | 2.80(.56) | 3.50(.53) | .70 | 16.73 | 64.00 | -1.58 | -.30 | .057 |
| BBN Colon Cancer OSCE for Residents (N = 38) | ||||||||||||
| Control Group n = 18 | Intervention Group n = 20 | Mann-Whitney test Change Scores: Control vs. Intervention | ||||||||||
| Rating Scale | baseline M (SD) | follow-up M (SD) | change score | Change Scores Mean rank | baseline M (SD) | follow-up M (SD) | change score | change scores mean rank | U | Z | r (effect-size) | p |
| Colon - BBN Skills Rating Form | ||||||||||||
| 1. Preamble to Breaking Bad News | 2.92 (.80) | 3.63(.97) | .71 | 21.39 | 3.28 (1.10) | 3.61(1.12) | .33 | 17.80 | 146.00 | -1.02 | -.17 | .153 |
| 2. Breaking Bad News | 3.86 (1.11) | 3.61(1.14) | -.25 | 14.58 | 3.80 (.89) | 4.85(.88) | 1.05 | 23.93 | 91.50 | -2.67 | -.43 | .004** |
| 3. Attention to Patient Responses After BBN | 2.04 (1.24) | 2.42(1.35) | .38 | 18.92 | 2.28 (.85) | 2.94(1.17) | .66 | 20.03 | 169.50 | -.31 | -.05 | .378 |
| 4. Communication Related to Patient Emotions | 3.01 (1.00) | 3.31 (.71) | .30 | 16.11 | 2.79 (.82) | 3.74(1.11) | .95 | 22.55 | 119.00 | -1.83 | -.30 | .034** |
| 5. After BBN, Determines Patient Readiness to Proceed and Communication Preferences | 2.46 (1.26) | 2.61 (.79) | .15 | 16.19 | 2.73 (.94) | 3.56(1.27) | .83 | 22.48 | 120.50 | -1.74 | -.28 | .041* |
| Colon - Common Ground Assessment Scales | ||||||||||||
| 1. Rapport | 3.14 (.64) | 3.14 (.56) | .00 | 16.61 | 3.18 (.52) | 3.48 (.77) | .30 | 22.10 | 128.00 | -1.60 | -.26 | .056 |
| 2. Active Listening | 2.44 (.45) | 2.50 (.49) | .06 | 15.22 | 2.55 (.58) | 3.23 (.70) | .68 | 23.35 | 103.00 | -2.31 | -.37 | .011** |
| 3. Addressing Feelings with Patient | 3.06 (.45) | 2.94 (.34) | -.12 | 12.17 | 3.08 (.47) | 3.80 (.59) | .72 | 26.10 | 48.00 | -3.99 | -.65 | <.001*** |
| 4. Closing the Interview | 3.00 (.35) | 2.94 (.50) | -.06 | 13.44 | 2.95 (.65) | 3.63 (.60) | .68 | 23.73 | 75.50 | -2.98 | -.48 | .002** |
| 5. Global Interview Performance | 2.89 (.40) | 2.97 (.32) | .08 | 13.86 | 2.80 (.66) | 3.55 (.71) | .75 | 24.58 | 78.50 | -3.12 | -.51 | .001** |
Note:
p <.05,
p <.01,
p <.001.
All tests were one-tailed.
Among residents, most of the BBN Skills and CGAS scales were significantly higher for the intervention group than the control group. Using the colon cancer OSCE, three of the five BBN Skills measures were significantly higher in the intervention group: Breaking Bad News (p = .004; r = -.43), Communication Related to Emotions (p = .034; r = -.30), and After BBN, Determines Patient Readiness to Proceed and Communication Preferences (p = .041; r = -.28). The resident intervention group also had significantly higher scores on four of the five CGAS scales: Active Listening (p = .011; r = -.37), Addressing Feelings with Patients (p < .001; r = -.65), Closing the Interview (p = .002; r = -.48), and Global Interview Performance (p = .001; r = -.51).
4. Discussion and Conclusion
4.1 Discussion
This study evaluated the effectiveness of a brief (60 minute) BBN communication training module with students and residents. Communication skills of both student and resident intervention group participants significantly improved in a variety of areas. These included skills which occurred during the initial moments of breaking bad news, the provision of forewarnings before BBN, attention to patient responses immediately after BBN, using the word “cancer” rather than vague terms like “growth” or tumor”, communication related to emotions, determining readiness to proceed, assessing for preferred method of communication, active listening, and closing the interview (identifying patient perspective, explaining impressions, checking for agreement understanding and feasibility, and establishing mutual responsibility). The effect sizes for these improvements ranged from medium to large, suggesting that this brief BBN module can be an effective method for teaching students and residents.
While improvement was demonstrated in most skill areas, some differences were found between students and residents. For example, after training, residents improved active listening skills, were more likely to address patient emotions, and to close the interview effectively by identifying patient perspectives, explaining impressions, establishing mutual responsibility, and checking for understanding, agreement, and feasibility. Residents did not significantly improve on a measure assessing attention to patient responses after breaking bad news. On the other hand, health professional students who completed the BBN module were significantly more likely to wait or pause after the initial announcement that bad news was to follow and were more likely to explicitly ask about how the patient felt after bad news was delivered. Students who used the module were more likely to explore for possible underlying emotions expressed verbally and nonverbally by the OSCE patient. Differences between residents and students may have been because many of the residents trained at foreign medical schools which provided little or no communication skills training. Cultural differences may also have played a role in preferences for communication approaches.
While students significantly improved on the BBN and the Attention to Patient Responses scales using both the colon and breast cancer OSCE, there were some differences based on the type of OSCE used. For example, student performance improved on two sets of skills related on the breast cancer OSCE, but not on the colon cancer OSCE. Both sets of skills were related to patient emotions (Addressing Feelings scale) and Communication Related to Patient Emotions (asking about feelings, acknowledging feelings without specifically identifying the feeling, naming or hypothesizing feelings, and using touch effectively). In addition to unknown differences between these OSCEs, there is the possibility that, because of age similarities or cancer's relative frequency of occurrence, students may have felt greater empathy with standardized patients portraying breast cancer than for the standardized patients depicting colon cancer.
Because of additional training and maturation associated with life and clinical practice experiences, baseline communication skills of residents were anticipated to be higher than those of students. However, baseline scores for residents were higher than students on but two of ten measures (Preamble to BBN and Rapport). This may have been because residents did not attend a medical school where communication training was stressed. Indeed, many residents in this study received their medical school education in foreign medical schools, and have informally reported that communication skills were taught casually and episodically at the bedside during hospital rounds. Another consideration is baseline score differences might have been associated with selection bias: the student group was comprised of volunteers who, recently completing a communication skills course, may also have had special interest in this topic.
This study has several strengths. It is a randomized control trial design which, used a standardized, reproducible, and brief (60 minute) training module that incorporated video-recorded stories from patients who shared their experiences specific to cancer as well as their preferences for communication with physicians. In addition, this study used objective performance measures: standardized patients and OSCEs. Effect-sizes of results are included, which permits interpretability regarding the magnitude of change [44, 45] between baseline and follow-up OSCEs. The BBN module is learner-centered, self-paced, and designed for the training of advanced interviewing skills. Like similar studies [25,29-32], items comprising the BBN Skills are largely based on suggestions from existing literature, expert opinion, and consensus statement guidelines.
This study has several limitations. Generalizability of CGAS results may be limited. Lang et al. [39] found that five OSCEs achieved a high generalizability coefficient of .80, whereas, due to time constraints, this study used but two OSCE cases. Secondly, sample size limitations prevented the use of factor analysis, an approach that may have led to the development of more precise assessment measures. On the other hand, the BBN Skills measures used in this study do possess a high degree of face validity and focus on observable BBN skills measured using a simple “yes or no” checklist. Additionally, consistent with previous studies [25,29-32], BBN Skills items are based on expert opinion, suggestions from existing literature, and consensus statement guidelines. A third limitation is that selection bias may exist among students. Unlike residents, students volunteered and were not required to participate as part of their regular educational coursework. Some students may have participated due to an interest in learning additional communication skills. However, students received a $100 payment which may have incentivized some individuals who would not have normally participated without it, thereby diversifying the student group and likely mitigating self-selection bias introduced by volunteers whose primary motivation was learning new communication skills. Students had just completed training on basic, core communications skills; however these authors are uncertain regarding specific previous communications skills training among residents.
Table 3 compares methods and relevant findings from our study with several others [25,29-32]. Our study used a self-guided module, whereas most others [25,29,31-32] used a combination of lecture, small group learning, role-playing, and feedback. One study [31] used a self-directed training similar to our own; however their method incorporated feedback sessions, whereas ours did not. Our study tested students and residents, whereas others tested medical residents or mid-career oncologists. Our training used minimal time (1 hour) and resources, where others used more (1.3 hours - 40 hours).
Table 3.
Summary Comparison of BBN Communication Skills Training Incorporating OSCEs and Randomized Control Design.
| Authors | Training Method | Participants | Highlights of Significant
Results (Note: Areas of overlap between improvements in communication skills demonstrated in our study and other studies are italicized. Bracketed numbers after skill items correspond to similar skills assessed by our measures.) |
|---|---|---|---|
| Gorniewicz, Floyd, Krishnan, Bishop, Tudiver, and Lang (2016) | Self-directed PowerPoint-based training module
incorporating cancer patient videos (1 hour) Total time: 1 hour |
Students (medical, nursing, and pharmacy) and Medical Residents (family medicine and internal medicine) |
Student group Colon cancer OSCE:
Colon cancer OSCE
|
| [25) Lienard, Merckaert, Libert, et al. (2010) | Lecture and small groups w/ role-playing and
feedback Total time: 40 hours |
Medical Residents |
Open question [6] (p
< .001; RR = 5.79) Open directive questions [6] (p = .003; RR = 1.71) Empathy [2,4] (p = .017; RR = 4.50) Fewer medical words [1] (p < .001; RR = .74) Less information transmission (p = .001; RR = 0.72) |
| [29] Szmuilowicz, el-Jawahri, Chiappetta, et. al (2010) | Lecture and small groups w/ role playing and
feedback Total time: 5 hours |
Medical Residents (internal medicine PGY 2) | Responding to emotion - overall score [2-4] (p = .03) |
| [30] Daetwyler, Cohen, Gracely, et. al (2010) | doc.com online BBN module (1 hour) +
WebEncounter OSCE (10 minutes) w/feedback (10 minutes) Total time: 1.3 hours |
Medical Residents | BBN skills checklist summary score [1-7] (p = .018) |
| [31] Merckaert, Lienard, Libert, et. al (2013) | Lecture and small groups, role-playing and
feedback (30 hours) + stress management training (10
hours) Total time: 40 hours |
Medical Residents (oncology, gynecology, and others) |
Supportive utterances: acknowledgement
[2,4] (p < .001; RR
=1.58) Open directive questions [6] (p < .001; RR =2.14) Decrease in use of medical words by residents [1] (p < .001; RR = 0.81) Checking questions [7] (p = .034; RR =1.66) Decrease in procedural information utterance by residents (p < .047; RR = 0.83) Longer “pre-delivery phase” (p < .001; RR = 3.04) Shorter “post-delivery phase” (p < .001; RR = 0.93) |
| [32] Fujimori, Shirai, Asai, et. al (2014) | Orientation/ice-breaker (30 minutes) +
lecture w/ videos (1 hour) + small group role plays w/
discussion (8 hours) + summary session (30 minutes) Total time: 10 hours |
Oncologists (10 years of experience on average) |
Not beginning bad news without
preamble [1] (p <
.001) Checking to see that patient understands bad news [2,7] (p = .008) Communicating clearly main points of bad news [1] (p = .011) Checking questions [7] (p = .045) Providing reassurance and addressing patient's emotions with empathic Responses [2-4,6] (p = .011) Remaining silent out of concern for patient's feelings [2] (p = .005) Accepting patient's expression of emotions [3] (p < .001) Using words that soothe patient [2-4] (p = .005) Considering how to deliver bad news (p = .001) Setting up supportive environment for interview (p = .002) Greeting patient cordially (p <.001) Asking how much patient knows about his or her illness before breaking bad news (p = .024) Checking to see whether talk is fast paced (p = .005) Providing information on services and support (p = .002) Explaining second opinion (p = .012) |
Our results are consistent with findings of other studies in the literature. Previously developed interventions [25,29-32] have noted significant improvement in aspects of communication related to empathy. Additionally, Deatwyler and colleagues [30] reported overall improvement in BBN skills using a checklist rating form with items similar to our own rating form [Figure 1].
Unique to our study is the successful implementation of a self-directed training module that 1) does not require expert feedback in order to improve communication skills, 2) incorporates memorable and emotionally resonant video-recorded stories from patients with cancer, 3) requires less time and resources than other training methods, and 4) is effective with student learners.
4.2 Conclusion
Our results demonstrate that students and residents who used this module significantly improved their communication skills based upon measures designed to assess skill acquisition in a variety of areas. Future research could examine the effectiveness of using this module in other educational training settings. This study used individual, self-paced learning for training. It is unknown whether other settings, such as a small group led by a facilitator or a short lecture/discussion, would yield similar results. There is also a need for future research examining the effectiveness for each of the four other modules (living through treatment, palliative care/end-of-life care, spirituality, and family) developed through this grant. Similarly, other research methodologies, such as the one described by Lienard [25] examining residents' verbal content and quantity of speech, could be highly illuminating. Additional research could also study the transfer of skills into actual clinical communication with real patients as well as their effect on clinical patient outcomes.
4.3 Practice Implications
Implementation of this brief training module within medical schools, residency training, and/or continuing education programs could lead to improved communication skills, patient care, and quality of life.
Highlights.
We interviewed patients with cancer to learn about their communication experiences.
We created/tested a breaking bad news (BBN) communication skills training module.
The brief training module used video-recorded segments from our patient interviews.
Intervention group students and residents significantly improved their BBN skills.
Health education programs could use this to improve communication and patient care.
Acknowledgments
The authors would like to gratefully acknowledge the following individuals for their insight and assistance during module development and/or assessment: Catherine McMaken, MA; Joel Richards, MA; Bruce Behringer, MPH.; Robert Enck, MD; Harsha Vardhana, MD; Joseph Sobol, PhD; Marjorie K. Smith, MA; Perry Ann Butler, BA; and Bill Linn, BFA.
Research Support: This research was supported by a grant from the National Cancer Institute (NIH, R25CA111698).
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
Informed Consent and Patient Details: “I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Oken D. What to tell cancer patients - a study of medical attitudes. J Amer Med Assoc. 1961;175:1120–8. doi: 10.1001/jama.1961.03040130004002. [DOI] [PubMed] [Google Scholar]
- 2.Friedman HJ. Physician management of dying patients: an exploration. Psychiatry Med. 1970;1:295–305. doi: 10.2190/qhye-h6gw-ym2j-tpc6. [DOI] [PubMed] [Google Scholar]
- 3.Novack DH, Plumer R, Smith RL, Ochitill H, Morrow GR, Bennett JM. Changes in physicians' attitudes toward telling the cancer patient. J Amer Med Assoc. 1979;241:897–900. [PubMed] [Google Scholar]
- 4.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;263:312–9. doi: 10.1016/S0140-6736(03)15392-5. [DOI] [PubMed] [Google Scholar]
- 5.Schmid Mast M, Kindlimann A, Langewitz W. Recipients' perspective on breaking bad news: how you put it really makes a difference. Patient Educ Couns. 2005;58:244–51. doi: 10.1016/j.pec.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Lienard A, Merckaert I, Libert Y, Delvaux N, Marchal S, Boniver J, et al. Factors that influence cancer patients' anxiety following a medical consultation: impact of a communication skills training programme for physicians. Ann Oncol. 2006;17:1450–8. doi: 10.1093/annonc/mdl142. [DOI] [PubMed] [Google Scholar]
- 7.Buckman R. Breaking bad news: why is it still so difficult? Br Med J (Clin Res Ed) 1984;288:1597–9. doi: 10.1136/bmj.288.6430.1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford S, Fallowfield L, Lewis S. Can oncologists detect distress in their out-patients and how satisfied are they with their performance during bad news consultations? Br J Cancer. 1994;70:767–70. doi: 10.1038/bjc.1994.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ptacek JT, Eberhardt TL. Breaking bad news - a review of the literature. J Amer Med Assoc. 1996;276:496–502. [PubMed] [Google Scholar]
- 10.VandeKieft GK. Breaking bad news. Am Fam Physician. 2001;64:1975–8. [PubMed] [Google Scholar]
- 11.Fallowfield L. Giving sad and bad news. Lancet. 1993;341:476–8. doi: 10.1016/0140-6736(93)90219-7. [DOI] [PubMed] [Google Scholar]
- 12.Ptacek JT, Ptacek JJ, Ellison NM. “I'm sorry to tell you …” physicians' reports of breaking bad news. J Behav Med. 2001;24:205–17. doi: 10.1023/a:1010766732373. [DOI] [PubMed] [Google Scholar]
- 13.Sykes N. Medical students' fears about breaking bad news. Lancet. 1989;334:564. doi: 10.1016/s0140-6736(89)90688-0. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM, Leaning MS, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–9. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simpson M, Buckman R, Stewart M, Maguire P, Lipkin M, Novack D, et al. Doctor-patient communication: the Toronto consensus statement. Br Med J. 1991;303:1385–7. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med. 2001;76:390–3. doi: 10.1097/00001888-200104000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES - A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–11. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 18.Haq C, Steele DJ, Marchand L, Seibert C, Brody D. Integrating the Art and Science of Medical Practice: Innovations in Teaching Medical Communication Skills. Fam Med. 2004;36:S43–50. [PubMed] [Google Scholar]
- 19.Hojat M. Ten approaches for enhancing empathy in health and human services cultures. J Health Hum Serv Admin. 2009;31:412. [PubMed] [Google Scholar]
- 20.Girgis A, Sanson-Fisher RW. Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol. 1995;13:2449–56. doi: 10.1200/JCO.1995.13.9.2449. [DOI] [PubMed] [Google Scholar]
- 21.Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R. Efficacy of a cancer research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002;359:650–6. doi: 10.1016/S0140-6736(02)07810-8. [DOI] [PubMed] [Google Scholar]
- 22.Eid A, Petty M, Hutchins L, Thompson R. “Breaking bad news”: standardized patient intervention improves communication skills for hematology-oncology fellows and advanced practice nurses. J Cancer Educ. 2009;24:154–9. doi: 10.1080/08858190902854848. [DOI] [PubMed] [Google Scholar]
- 23.Schildmann J, Kupfer S, Burchardi N, Vollmann J. Teaching and evaluating breaking bad news: a pre-post evaluation study of a teaching intervention for medical students and a comparative analysis of different measurement instruments and raters. Patient Educ Couns. 2012;86:210–9. doi: 10.1016/j.pec.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 24.Senol Y, Ozdogan M, Bozcuk H. Effects and permanency of the training program “communication with cancer patients” on the opinions of students. J Cancer Educ. 2012;27:338–41. doi: 10.1007/s13187-012-0309-4. [DOI] [PubMed] [Google Scholar]
- 25.Lienard A, Merckaert I, Libert Y, Bragard I, Delvaux N, Etienne AM, et al. Is it possible to improve residents breaking bad news skills? A randomised study assessing the efficacy of a communication skills training program. Br J Cancer. 2010;103:171–7. doi: 10.1038/sj.bjc.6605749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenbaum ME, Ferguson KJ, Lobas JG. Teaching medical students and residents skills for delivering bad news: a review of strategies. Acad Med. 2004;79:107–17. doi: 10.1097/00001888-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Baile WF, Kudelka AP, Beale EA, Glober GA, Myers EG, Greisinger AJ, et al. Communication skills training in oncology. Description and preliminary outcomes of workshops on breaking bad news and managing patient reactions to illness. Cancer. 1999;86:887–97. [PubMed] [Google Scholar]
- 28.Rosenbaum ME, Kreiter C. Teaching delivery of bad news using experiential sessions with standardized patients. Teach Learn Med. 2002;14:144–9. doi: 10.1207/S15328015TLM1403_2. [DOI] [PubMed] [Google Scholar]
- 29.Szmuilowicz E, el-Jawahri A, Chiappetta L, Kamdar M, Block S. Improving residents' end-of-life communication skills with a short retreat: a randomized controlled trial. J Palliat Med. 2010;13:439–52. doi: 10.1089/jpm.2009.0262. [DOI] [PubMed] [Google Scholar]
- 30.Daetwyler CJ, Cohen DG, Gracely E, Novack DH. eLearning to enhance physician patient communication: a pilot test of “doc.com” and “WebEncounter” in teaching bad news delivery. Med Teach. 2010;32:e381–90. doi: 10.3109/0142159X.2010.495759. [DOI] [PubMed] [Google Scholar]
- 31.Merckaert I, Lienard A, Libert Y, Bragard I, Delvaux N, Etienne AM, et al. Is it possible to improve the breaking bad news skills of residents when a relative is present? A randomised study. Br J Cancer. 2013;109:2507–14. doi: 10.1038/bjc.2013.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fujimori M, Shirai Y, Asai M, Kubota K, Katsumata N, Uchitomi Y. Effect of communication skills training program for oncologists based on patient preferences for communication when receiving bad news: a randomized controlled trial. J Clin Oncol. 2014;32:2166–72. doi: 10.1200/JCO.2013.51.2756. [DOI] [PubMed] [Google Scholar]
- 33.Borkan J. mmersion/crystallization. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. second. Sage Publications Inc.; Thousand Oaks, USA: 1999. pp. 179–94. [Google Scholar]
- 34.Patton MQ. Qualitative Research and Evaluation Methods. third. Sage Publications Inc.; Thousand Oaks, USA: 2002. [Google Scholar]
- 35.Kuzel A. Sampling in qualitative inquiry. In: Crabtree FF, Miller WL, editors. Doing Qualitative Research. second. Sage Publications Inc.; Thousand Oaks, USA: 1999. pp. 33–45. [Google Scholar]
- 36.QRS International. NVivo 8 software. 2009 [Google Scholar]
- 37.Lienard A, Merckaert I, Libert Y, Bragard I, Delvaux N, Etienne AM, et al. Transfer of communication skills to the workplace during clinical rounds: impact of a program for residents. PLoS One. 2010;5:e12426. doi: 10.1371/journal.pone.0012426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharp PC, Pearce KA, Konen JC, Knudson MP. Using standardized patient instructors to teach health promotion interviewing skills. Fam Med. 1996;28:103–6. [PubMed] [Google Scholar]
- 39.Lang F, McCord R, Harvill L, Anderson DS. Communication assessment using the common ground instrument: psychometric properties. Fam Med. 2004;36:189–98. [PubMed] [Google Scholar]
- 40.Howley L, Szauter K, Perkowski L, Clifton M, McNaughton N. Association of Standardized Patient Educators (ASPE), Quality of standardised patient research reports in the medical education literature: review and recommendations. Med Educ. 2008;42:350–8. doi: 10.1111/j.1365-2923.2007.02999.x. [DOI] [PubMed] [Google Scholar]
- 41.Kroboth FJ, Hanusa BH, Parker S, Coulehan JL, Kapoor WN, Brown FH, et al. The inter-rater reliability and internal consistency of a clinical evaluation exercise. J Gen Intern Med. 1992;7:174–9. doi: 10.1007/BF02598008. [DOI] [PubMed] [Google Scholar]
- 42.Hodges B, Turnbull J, Cohen R, Bienenstock A, Norman G. Evaluating communication skills in the OSCE format: reliability and generalizability. Med Educ. 1996;30:38–43. doi: 10.1111/j.1365-2923.1996.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 43.IBM Corporation. SPSS Statistics for Windows, version 21. 2012 [Google Scholar]
- 44.Field A. Discovering Statistics Using SPSS. third. Sage Publications Inc.; Thousand Oaks, USA: 2009. [Google Scholar]
- 45.Rosenthal R. Meta-Analytic Procedures for Social Research. revised. Sage Publications Inc.; Newbury Park, USA: 1991. [Google Scholar]