Abstract
Background
Since 2010, the Champlain BASE (Building Access to Specialist Advice through eConsultation) has allowed primary care providers (PCPs) to submit clinical questions to specialists through a secure web service. The study objectives are to describe questions asked to Infectious Diseases specialists through eConsultation and assess impact on physician behaviors.
Methods
eConsults completed through the Champlain BASE service from April 15, 2013 to January 29, 2015 were characterized by the type of question asked and infectious disease content. Usage data and PCP responses to a closeout survey were analyzed to determine eConsult response time, change in referral plans, and change in planned course of action.
Results
Of the 224 infectious diseases eConsults, the most common question types were as follows: interpretation of a clinical test 18.0% (41), general management 16.5 % (37), and indications/goals of treating a particular condition 16.5% (37). The most frequently consulted infectious diseases were as follows: tuberculosis 14.3% (32), Lyme disease 14.3% (32), and parasitology 12.9% (29). Within 24 hours, 63% of cases responded to the questions, and 82% of cases took under 15 minutes to complete. In 32% of cases, a face-to-face referral was originally planned by the PCP but was no longer needed. In 8% of cases, the PCP referred the patient despite originally not planning to make a referral. In 55% of cases, the PCP either received new information or changed their course of action.
Conclusions
An eConsult service provides PCPs with timely access to infectious disease specialists’ advice that often results in a change in plans for a face-to-face referral.
Keywords: access, eConsultation, electronic referral, infectious diseases, wait times
The increasing importance of inappropriate antibiotic use, emergence of antimicrobial resistance, and rapid diagnostic tests in microbiology have created growing demand for the expertise of infectious diseases specialists with antimicrobial stewardship as top priority [1, 2]. To meet demand, technology platforms have been used to improve access and reduce costs, especially for patients in remote communities.
Several studies have demonstrated the role for Telemedicine in Infectious Diseases [2, 3]. Telemedicine in Infectious Diseases is done via a secured video interface that allows patient-to-physician virtual interaction [3, 4]. Although telemedicine has the ability to provide access in otherwise underserved areas, it requires expensive equipment and relies on the presence of the primary care provider (PCP) or delegate, patient, and the specialist at the same time, which makes synchronization of the encounter challenging at times [5].
The use of an electronic consultation (eConsultation) connects PCPs directly to specialists for a fast, secure answer to a patient problem. eConsults may replace the need for a face-to-face referral or allow investigations to be completed before the specialist visit [6–9]. eConsult services have demonstrated improved timely access, better quality of communication between providers, lower cost delivery, and high provider satisfaction [7, 10–15]. Because there is no interaction between the patient and specialist, suggestions that are provided from the specialist are expected to be applied or interpreted by the PCP [6, 16].
Although there are several large eConsult systems internationally that include infectious diseases, there is only 1 published study of eConsults directed to infectious disease specialists, which was completed at the Mayo Clinic. This service was primarily used for specialist to specialist consultation and not primary care [16, 17]. The Champlain BASE (Building Access to Specialists through eConsult) eConsult service was developed in Ottawa, Canada in 2010 [6, 7]. As of November 30, 2016, 1145 PCPs (including 970 family doctors and 175 nurse practitioners) have access to advice from 97 different specialty groups, including infectious disease. More than 20300 eConsults have been completed. This service has been shown to improve cost-effective, timely access to specialist advice, which is well accepted by patients [6, 7]. The purpose of this paper is to describe the utilization of the Infectious Disease specialty service available through Champlain BASE eConsult service including types of questions asked and the impact on PCP behavior.
METHODS
Local Health Integration Networks (LHIN) are 14 regional health authorities in the province of Ontario that integrate and fund healthcare in their region as delegated by the provincial government. The Champlain LHIN region is in Eastern Ontario, Canada with a population of 1.2 million, with all Infectious Diseases consultants being located at 1 of 2 centers in Ottawa. Typically, there are more than 500 new outpatient referrals for infectious diseases per month, and the estimated wait times are 1 to 2 months for nonurgent consults.
The Champlain BASE eConsult service has been described in detail elsewhere [6, 7, 13, 15]. In brief, it is a secure web-based service that allows a PCP (family doctor or nurse practitioner) to submit patient-specific clinical questions to specialists using a standardized electronic form. Supplementary patient information, such as laboratory results, digital images, and health history, can be attached. For each eConsult, depending on the request and information provided, the specialist can accomplish the following: (1) provide recommendations; (2) request additional information before being able to provide advice; and (3) recommend a face-to-face referral, in which case any additional diagnostic tests or courses for treatment could be suggested and initiated before the appointment.
For all eConsults, data are prospectively collected, stored securely, and then retrospectively accessed for analysis. This includes provider type, age and gender of patient, length of time taken to complete the case, time to receive response, and survey results. The specialists are paid a prorated hourly rate of $200.00 per hour based on 5-minute intervals up to 20 minutes.
All eConsults submitted to Infectious Disease specialists between April 17, 2013 and January 29, 2015 were reviewed and categorized retrospectively by clinical topic and type of question by 2 raters. G.R., an Infectious Diseases specialist, and R.M., an Infectious Diseases Fellow, were the raters in this study. The infectious disease content coding scheme was based on the International Classification for Primary Care (ICPC-2) taxonomy and finalized by consensus. A total of 32 different clinical topics were included, and an additional “other category” for topics that were otherwise unclassifiable. The question type (for example, diagnosis or management) was coded using a generalized validated taxonomy [18]. To ascertain agreement on the categorization of each eConsult, a random selection of 20 eConsults were independently reviewed by each of the 2 raters, and disagreements were resolved through discussion until consensus was reached. The remaining 204 cases were divided by G.R. and R.M. and reviewed independently. Any difficult-to-classify consults were discussed and a consensus was reached by the 2 raters.
Upon completion, and before a case can be officially closed, the PCP completes a mandatory close-out survey containing 5 questions. The first question solicits information on the eConsult’s outcome. Primary care providers can choose whether the eConsult (1) confirmed their originally chosen course of action, (2) suggested a new or additional course of action, (3) was not very useful, or (4) none of the above. The second question asks whether the eConsult changed the PCP’s intentions to refer the patient for a traditional, face-to-face referral. The choices include the following: whether a referral was originally contemplated but now avoided (avoided referral), referral was originally contemplated and is still needed, referral was not originally contemplated and is still not needed, and referral was not originally contemplated, but eConsult process resulted in a referral being initiated. The survey allows PCPs to choose from 6 different options identifying whether or not they (1) had originally contemplated a referral and (2) ultimately referred the patient based on the advice they received from the eConsult. The third and fourth questions ask PCPs to rank the eConsult’s value for their patients and themselves, respectively, using a 5-point Likert scale. The fifth question provides an optional free-text field allowing PCPs to leave any additional comments they may have. These questions and comments are used to assess the impact on PCP behavior.
RESULTS
The Champlain BASE service received a total of 4531 eConsultations from April 17, 2013 to January 29, 2015, 224 (5%) of which were directed to Infectious Disease. The 224 cases were submitted by 60 different PCPs, 84% of whom were physicians and 16% of whom were nurse practitioners.
The mean length of time between the submission of the case by the PCP and the response by the specialist was 8 hours and 38 minutes, with 63% of cases receiving their first response within 24 hours. The specialists reported it took <10 minutes in 52% of cases, 10–15 minutes in 30% of cases, 15–20 minutes in 13% of cases, and over 20 minutes in 5% of cases to complete the eConsult.
Type of Questions Asked
There were 33 different clinical topics included in the eConsults with 32 that could be categorized; 7 cases (3.1%) could not be categorized and formed the 33rd category of Other. All topics with greater than or equal to 5 eConsult cases are presented in Table 1. The diseases and conditions that were most frequently consulted about were as follows: tuberculosis 14.3% (32), Lyme disease 14.3% (32), and parasite questions not otherwise specified 12.9% (29) (Table 1).
Table 1.
Clinical Topics for Which eConsults Were Requesteda
| Infectious Disease Reason for eConsultation | Percent of Total (%) | n (=224) |
|---|---|---|
| Tuberculosis | 14.3 | 32 |
| Lyme disease | 14.3 | 32 |
| Parasite infections NOS | 12.9 | 29 |
| Vaccination-general | 10.3 | 23 |
| Skin and soft tissue infection | 7.6 | 17 |
| Hepatitis | 6.3 | 14 |
| Herpesviruses (HSV/VZV/EBV/CMV/HHV) | 3.1 | 7 |
| Unclassified by provided list | 3.1 | 7 |
| Sexually transmitted disease NOS | 2.7 | 6 |
| Osteomyelitis | 2.7 | 6 |
| Diarrhea | 2.2 | 5 |
| All other topicsb | 20.5 | 46 |
Abbreviations: CMV, cytomegalovirus; CNS, central nervous system; EBV, Epstein-Barr virus; HHV, human herpes virus; HIV, human immunodeficiency virus; HSV, herpes simplex virus; NOS, unspecified; SIRS, systematic inflammatory response syndrome; VZV, varicella zoster virus.
aDiseases represented include all diseases where there were equal to or greater than 5 eConsults.
bIncludes the following: bacterial infections NOS, articular/periarticular infections, upper respiratory tract, zoonoses NOS, Clostridium difficile, respiratory tract infection, vaccination—travel, odontogenic infections, fungal infections NOS, urinary tract infection, viral disease NOS, diabetic foot wounds, malaria, HIV, CNS infections, fever, blood/body fluid exposure, genital infection, fever/leukocytosis/SIRS, dental prophylaxis, chronic fatigue, infectious mononucleosis, and nontuberculous mycobacteria.
Table 2 lists the frequency of types of questions asked. The most common types of questions asked were as follows: diagnosis-interpretation of a clinical test, 18.0% (41); management-general management question, 16.5% (37); and drug treatment-indications/goals of treating a particular condition, 16.5% (37).
Table 2.
Question Types Asked Through eConsultation Platform: All Categories Represented
| Clinical Question | Percent of Total (%) | n (=224) |
|---|---|---|
| Diagnosis-interpretation of a laboratory test | 18.3 | 41 |
| Management-general management question | 16.5 | 37 |
| Drug Treatment-indications/goals of treating a particular condition | 16.5 | 37 |
| Diagnosis-what test to choose | 13.8 | 31 |
| Drug Treatment- drug of choice | 8.9 | 20 |
| Drug Treatment-how to prescribe a particular drug | 8.5 | 19 |
| Management-should I refer | 5.4 | 12 |
| Drug Treatment-adverse effects of drugs | 4.0 | 9 |
| Diagnosis-interpretation of clinical finding | 3.6 | 8 |
| Diagnosis-interpretation of an image report | 1.3 | 3 |
| Drug Treatment–other | 0.9 | 2 |
| Epidemiology-etiology/risk factors | 0.9 | 2 |
| Drug Treatment-interactions between drugs | 0.4 | 1 |
| Procedure-preparation | 0.4 | 1 |
| More than one question (unclassifiable) | 0.4 | 1 |
Impact on Behavior
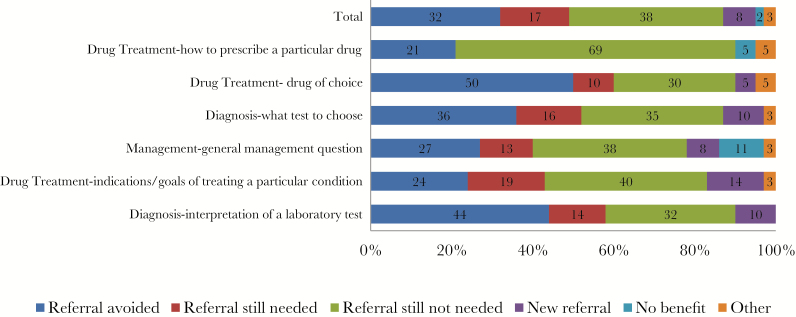
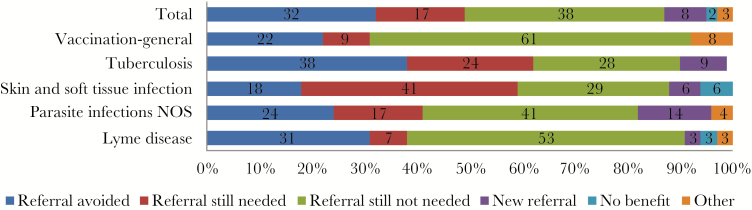
We assessed the impact on PCP behavior based on the completed surveys and decisions made regarding referrals after the eConsult was completed. In 32.1% (72) of the total submitted cases, a traditional referral was originally contemplated by the PCP but was now avoided. In addition, 7.6% [17] of new referrals were generated as a result of the eConsult, and 17% (38) of the referrals were still needed after the eConsult. To analyze PCP behavior further, Figure 1 displays referral decisions based on the most frequent consult types. Figure 2 displays referral decisions based on clinical topics.
Figure 1.
Referral outcomes organized by consult type. Categories represented are those that were greater than 2% of all consultations.
Figure 2.
Referral outcomes organized by clinical topics. Diseases represented include all diseases where there were 10 or more eConsults. Abbreviation: NOS, unspecified.
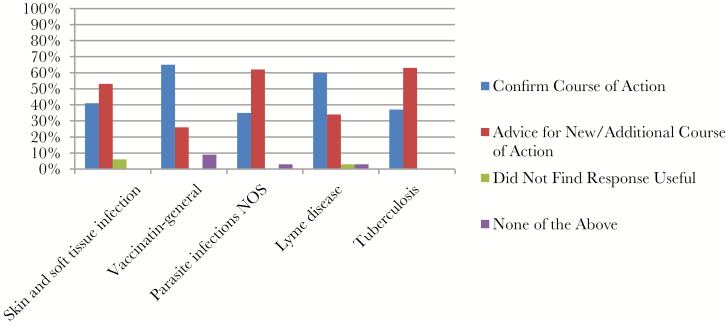
Overall, in 55% of cases, PCPs believed they received new advice or additional information directly impacting on patient care. In 40.6% of cases, the PCP’s course of action was confirmed by the specialist’s suggestion. In only 2% of cases, PCPs found the specialists’ opinion not very useful. Figure 3 displays the clinical topics with over 10 or more topics and the PCP’s interpretation of the advice given from the eConsult.
Figure 3.
Course of action based on primary care provider feedback regarding eConsult advice. Diseases represented include all diseases where there were 10 or more eConsults. Abbreviation: NOS, unspecified.
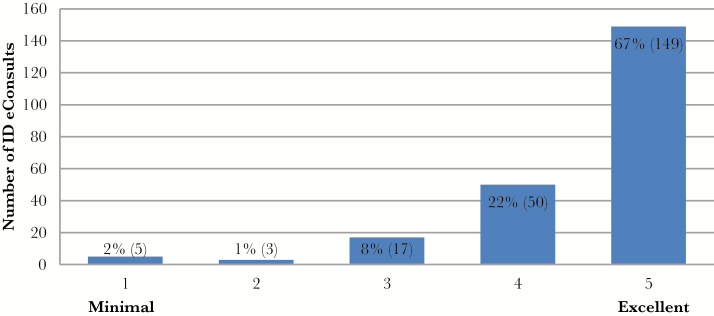
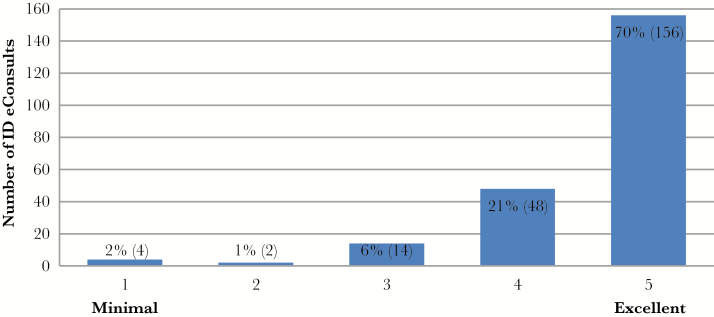
Finally, when the PCPs were asked to assess the overall value of the consultation for their patients, 89% rated the service greater at least 4 or greater on a 5-point Likert scale (Figure 4). Ninety-one percent of physicians rated the service at least 4 or greater on the same scale in reference to the overall value of the consult for the PCP themselves (Figure 5).
Figure 4.
Overall value of the eConsult rated on a scale from minimal [1] to excellent [5] as determined by primary care provider for patients. Abbreviation: ID, infectious diseases.
Figure 5.
Overall value of the eConsult rated on a scale from minimal [1] to excellent [5] as determined by primary care provider for themselves. Abbreviation: ID, infectious diseases.
DISCUSSION
Primary care providers have improved access to Infectious Disease specialists through Champlain BASE, which directly changes the management of patients, including a change in the need for a face-to-face referral. This is the first report of the types of questions PCPs ask Infectious Diseases specialists through an eConsult platform. This timely access is highly regarded by the providers and prevents weeks to months of waiting that might occur for specialist input via a face-to-face consultation.
The opportunity to identify recurring questions, especially those eConsults that lead to a change in PCP behavior, should be harnessed to inform continuing professional development activities. The most commonly asked questions were in the areas of tuberculosis, parasitology and Lyme disease, which is different than what is reported from the Mayo Clinic. In their setting, urinary tract infections, Lyme disease, mycobacteria, and candidal infections were most prevalent [16]. The majority of their eConsults came from other specialists, which may explain some of the difference. Specialists may generate eConsults in the Champlain BASE program, but they are a small minority of users. Further studies, in other regions and healthcare systems, are needed to fully understand the most common clinical scenarios in which PCPs seek specialist advice through eConsult.
Those topics that were most likely to result in a change in behavior should be a focus for continued professional development opportunities. For example, looking at the tuberculosis outcomes (Figure 3), in over 60% of cases, there was new advice or a different course of action that was offered through eConsults, and with eConsults one third of potential new referrals that were avoided (Figure 2). Not only does this present itself as a helpful tool for PCP questions, but it also identifies a potential area for education surrounding the topic. In contrast, when looking at vaccinations, the majority of PCPs believed that their course of action was supported, and in the majority of cases a referral was still not needed (Figure 2). Further study is needed to explore how this information can be best used. There may be a role for further opportunities in Continuing Medical Education for PCPs as questions and data are collected from such electronic platforms.
Applying eConsults to infectious diseases requires an understanding of certain limitations and opportunities. Although an eConsult service is useful, clearly not all infectious disease patient problems can be managed this way. Certain acute infections must be managed urgently with face-to-face consultations [19]. Ruotsalainen et al [20] demonstrated that 90-day mortality for telephone-consultation patients with Staphylococcus aureus bacteremia was higher than bedside consultation. On the other hand, there may be a larger role for eConsults for more severe illness in rural settings. Assimacopoulos et al [21] demonstrated that, among rural patients, comparing telehealth infectious diseases consultation with in-person consultation for neutropenic fever, bacterial pneumonia, or bacterial wound infection, there were no statistically significant mortality outcomes; however, there were shorter durations of antimicrobials used in the Telehealth population. Although this is in reference to Telehealth, there may be a role for future studies to extrapolate these data to eConsults in infectious diseases. In another study, electronic sharing of digital imaging demonstrated no significant difference in wound care management. Discrepancies were only in assessing wound drainage with eConsults as opposed to bedside evaluation [22].
There may also be a role for eConsults to assist in the growing field of antimicrobial stewardship. For example, in a small community hospital in Brazil, an email- and text-based mode of communication between the hospital and infectious disease specialist led to perfect compliance with suggested prescriptions [2]. In this instance, a formal email platform could provide the additional benefit of patient privacy and confidentiality while still fulfilling the needs of the peripheral hospital.
Our study has several limitations. It is one service that is primary localized to 1 health region, and it may not be generalizable to other populations or healthcare systems. We are unable to compare the number and type of questions asked through eConsults to those asked through in-person referrals to the Infectious Diseases clinic. We also cannot determine whether the PCP followed the advice provider or whether there was any impact to patient outcomes.
It remains clear, however, that an overwhelming number of PCPs recognize the value of eConsults for themselves and their patients, and they appreciate the timely access to specialist advice eConsult services provide and the opportunity to continue to improve the delivery of Infectious Disease services in a practical, timely way.
CONCLUSIONS
Infectious disease services, for some conditions, can be delivered through eConsults effectively. Exploring their applicability in different situations such as antimicrobial stewardship is needed. Studies to further define the types of questions asked, impact on patient outcomes, and healthcare costs are needed.
Acknowledgments
We thank Lesley Ananny for her assistance with the database and statistical analysis.
Financial support. This work was funded by the Department of Medicine at the University of Ottawa and the Royal College of Physicians and Surgeons of Canada.
Potential conflicts of interest. G. R. received personal fees from Champlain Local Health Integration Network BASE eConsult Service. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Rameau C, Mahy S, Simonet Lamm AL, et al. Informal consultation at a teaching hospital infectious diseases department. Med Mal Infec 2014; 44:107–11. [DOI] [PubMed] [Google Scholar]
- 2. Deutschendorf C, Carvalho OF, Timm R, Sparenberg A. Antimicrobial stewardship through telemedicine in a community hospital in southern Brazil dos Santos R.P. J Telemed Telecare 2013; 19:1–4. [DOI] [PubMed] [Google Scholar]
- 3. Mackie D, Varghese S, Cooper C. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis 2015; 60:1084–94. [DOI] [PubMed] [Google Scholar]
- 4. Botros J, Dhaliwal S, Clark G, et al. A pilot retrospective cohort study: clinical outcomes of hepatitis C patients treated with pegylated interferon and ribavirin via telemedicine consultation as compared to traditional office visits. Hepatology 2011; 54:588A–9A. [Google Scholar]
- 5. Jacklin PB, Roberts JA, Wallace P, et al. Virtual outreach: economic evaluation of joint teleconsultations for patients referred by their general practitioner for a specialist opinion. BMJ 2003; 327:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liddy C, Rowan MS, Afkham A, et al. Building access to specialist care through e-consultation. Open Med 2013; 7:e1–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Liddy C, Drosinis P, Deri Armstrong C, et al. What are the cost savings associated with providing access to specialist care through the Champlain BASE eConsult service? A costing evaluation. BMJ Open 2016; 6:e010920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim-Hwang JE, Chen AH, Bell DS, et al. Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med 2010; 25:1123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stoves J, Connolly J, Cheung CK, et al. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Qual Saf Health Care 2010; 19:e54. [DOI] [PubMed] [Google Scholar]
- 10. Straus SG, Chen AH, Yee H, Jr, et al. Implementation of an electronic referral system for outpatient specialty care. AMIA Annu Symp Proc 2011; 2011: 1337–46. [PMC free article] [PubMed] [Google Scholar]
- 11. Callahan CW, Malone F, Estroff D, Person DA. Effectiveness of an Internet-based store-and-forward telemedicine system for pediatric subspecialty consultation. Arch Pediatr Adolesc Med 2005; 159:389–93. [DOI] [PubMed] [Google Scholar]
- 12. Wootton R, Menzies J, Ferguson P. Follow-up data for patients managed by store and forward telemedicine in developing countries. J Telemed Telecare 2009; 15:83–8. [DOI] [PubMed] [Google Scholar]
- 13. Keely E, Drosinis P, Afkham A, Liddy C. Perspectives of champlain BASE specialist physicians: their motivation, experiences and recommendations for providing econsultations to primary care providers. Stud Health Technol Inform 2015; 209:38–45. [PubMed] [Google Scholar]
- 14. Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare 2015; 21:323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liddy C, Drosinis P, Keely E. Electronic consultation systems: worldwide prevalence and their impact on patient care-a systematic review. Fam Pract 2016; 33:274–85. [DOI] [PubMed] [Google Scholar]
- 16. North F, Uthke LD, Tulledge-Scheitel SM. Internal e-consultations in an integrated multispecialty practice: a retrospective review of use, content, and outcomes. J Telemed Telecare 2015; 21:151–9. [DOI] [PubMed] [Google Scholar]
- 17. Wrenn K, Catschegn S, Cruz M, et al. Analysis of an electronic consultation program at an academic medical centre: primary care provider questions, specialist responses, and primary care provider actions. J Telemed Telecare 2017; 23:217–24. [DOI] [PubMed] [Google Scholar]
- 18. Ely JW, Osheroff JA, Gorman PN, et al. A taxonomy of generic clinical questions: classification study. BMJ 2000; 321:429–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Honda H, Krauss MJ, Jones JC, et al. The value of infectious diseases consultation in Staphylococcus aureus bacteremia. Am J Med 2010; 123:631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ruotsalainen E, Ollgren J, Jarvinen A. Telephone consultation cannot replace bedside infectious disease consultation in the management of Staphylococcus aureus bacteremia. Clin Infect Dis 2013; 56:527–35. [DOI] [PubMed] [Google Scholar]
- 21. Assimacopoulos A, Alam R, Arbo M, et al. A brief retrospective review of medical records comparing outcomes for inpatients treated via telehealth versus in-person protocols: is telehealth equally effective as in-person visits for treating neutropenic fever, bacterial pneumonia, and infected bacterial wounds? Telemed J E Health 2008; 14:762–8. [DOI] [PubMed] [Google Scholar]
- 22. Trovato MJ, Scholer AJ, Vallejo E, et al. eConsultation in plastic and reconstructive surgery. Eplasty 2011; 11:e48. [PMC free article] [PubMed] [Google Scholar]