Abstract
Mothers with histories of alcohol and drug addiction have shown greater difficulty parenting young children than mothers with no history of substance misuse. This study was the second randomized clinical trial testing the efficacy of Mothering from the Inside Out (MIO), a 12-week mentalization-based individual therapy designed to address psychological deficits commonly associated with chronic substance use that also interfere with the capacity to parent young children. Eighty-seven mothers caring for a child between 11 and 60 months of age were randomly assigned to receive 12 sessions of MIO versus 12 sessions of Parent Education (PE)—a psychoeducation active control comparison. Maternal reflective functioning, representations of caregiving, mother-child interaction quality, and child attachment were evaluated at baseline and post-treatment and 3-month follow up. Mother-child interaction quality was assessed again at 12-month follow up. In comparison with PE mothers, MIO mothers demonstrated a higher capacity for reflective functioning and representational coherence at post-treatment and 3-month follow up. At 12-month follow up, compared to PE cohorts, MIO mothers demonstrated greater sensitivity, their children showed greater involvement, and MIO dyads showed greater reciprocity. As addiction severity increased, MIO also appeared to serve as a protective factor for maternal reflective functioning, quality of mother-child interactions, and child attachment status. Results demonstrate the promise of mentalization-based interventions provided concomitant with addiction treatment for mothers and their young children.
Although quality of caregiving varies widely, as a group, mothers who have histories of chronic substance use are at greater risk than mothers with no substance use history for losing custody of their young children (Choi & Ryan, 2007; Department of Health and Human Services, 1999; Grant, Huggins, Graham, Ernst, Whitney, & Wilson, 2011). In developmental studies (e.g., Burns, Chetik, Burns, & Clark, 1997; Hans, Bernstein, & Henson, 1999), mothers with substance use disorders have also shown lower levels of sensitivity and responsiveness to their infant’s cues and marked oscillation between intrusive, overcontrolling behaviors and passive withdrawal.
Although addiction severity among childrearing women seeking treatment for drug addiction has increased significantly in recent years (Greenfield, Back, Lawson, & Brady, 2010), addiction treatment programs rarely address parenting deficits. Moreover, parenting interventions designed for the general population (e.g., Triple P, Sanders, 1999; The Incredible Years, Webster-Stratton & Reid, 2010) fail to address the parenting problems of parents with addictive disorders, who often drop out prematurely or require more intensive and extensive clinical efforts. Reviews of clinical trials testing psychoeducational parenting interventions with this vulnerable population have generally shown little to no efficacy for improving parenting behavior, parent-child relationships, or children’s well-being (for a review, see Kerwin, 2005; Suchman, Pajulo, DeCoste, & Mayes, 2006).
Recent developments in the neuroscience of addiction and parenting suggest a significant overlap in the neural circuitry involved with chronic drug use and parenting (Rutherford, Williams, Moy, Mayes, & Johns, 2011; Strathearn, Fonagy, Amico, & Montague, 2009; Strathearn, 2011). Chronic drug use appears to co-opt the same dopaminergic neural pathways recruited during caregiving, decreasing reward sensitivity, heightening stress activation and potentially increasing vulnerability to relapse during caregiving activities.
Increasingly, heroin and opioids are being used at younger ages more broadly across socioeconomic strata (Jones, 2008; Seelye, 2015). Moreover, increasing purity of available heroin has led to alarming rates of overdose (Buckley, 2009). As they move into childbearing years, substance users are at greater risk for experiencing diminished reward and heightened distress as they transition to parenthood.
Taken together, these findings suggest the need for parenting interventions provided during addiction treatment that target the emotional consequences of a hijacked stress-reward system, especially those related to the parenting role. Supporting the parent’s emerging skills and capacities to manage challenging emotional experiences of parenthood concomitantly with addiction treatment may be a critical first step toward better parenting and may also promote relapse prevention. Moreover, understanding how addiction severity interacts with response to parenting interventions is also critical because it can help clarify which parenting interventions are the best match for parents with greater addiction severity.
The Mothering from the Inside Out (MIO) Intervention
Mothering from the Inside Out (MIO) is a manualized 12-session individual therapy developed to enhance a mother’s capacity for mentalization or reflective functioning (RF) in the parenting role (Suchman & Bers, 2015). Reflective functioning refers to the capacity to recognize and make sense of mental (especially emotional) states—that is, how they influence behavior and their possible impact on relationships (Fonagy, Steele, Steele, Leigh, Kennedy, Mattoon, & Target. (1995). MIO is based on the Mentalization-Based Therapy (MBT) model developed by Allen, Fonagy, and Bateman (2008), which emphasizes the restoration of mentalizing capacities under conditions of arousal by engaging in explicit, guided mentalization practice (Bateman & Fonagy, 2012).
Parental reflective functioning refers to a parent’s capacity to make sense of her own mental and emotional experiences in the parenting role and to make sense of the mental and emotional states that drive her child’s behavior. Parental RF has many immediate and practical benefits: It enables a parent to make sense of a young child’s mental and emotional experiences, which in turn may help the parent respond sensitively to the infant’s emotional and physical needs (Slade, 2005). It also enables the parent to recognize, understand and manage her own mental and emotional experiences and their impact on the child and caregiving relationship. This latter capacity is particularly relevant to mothers in addiction treatment because heightened distress and limited coping skills make them more vulnerable to emotional dysregulation and relapse.
MIO explicitly targets parental RF so that mothers can better manage emotional distress in the absence of neural reward that is common during chronic substance use episodes and early recovery from addiction. The short-term goals of MIO are to: (1) provide a positive experience in a therapeutic relationship in which the mother’s thoughts and emotions are taken seriously so that she can feel supported and understood and (2) begin a process of helping the mother make sense of her own and her child’s underlying affective experiences and think about how these experiences are related to individual need, behavior, and development. The long term goals of MIO are to: (1) support the mother’s developing capacity for emotional regulation, (2) restore the mother’s own capacity to engage in human attachment (e.g., replace attachment to a substance with attachment to the child), and (3) promote the mother’s capacity to engage with and enjoy her child, tolerate her child’s emotional distress, understand her child’s emotional needs and support her child’s developing regulatory capacities.
During each MIO session, the mother determines the focus of the discussion. If the child is not the immediate topic, the therapist will bring the child into mind when timing seems appropriate. Stressful situations—particularly those where the mother’s capacity for reflective functioning is challenged—are considered in detail. The therapist invites the mother to re-engage in the process of reflective functioning; that is, to consider thoughts, feelings and intentions in herself, her child and others as the therapist and parent review the stressful situation together. The therapist is careful not to shift the focus to the child too early. Often, the focus begins with recognizing the mother’s own affective distress and understanding its mental and emotional antecedents. In this way, MIO emphasizes engagement in a mentalizing process rather than specifying a particular content. The therapist provides relevant developmental guidance when the mother’s expectations for the child appear to be unrealistic. The therapist also suggests parenting strategies that are likely to promote secure attachment. The therapist’s curious, inquisitive, not-knowing stance is considered essential to the therapeutic process because of the opaque and transient nature of mental states and to encourage the mother to remain actively engaged in a mentalizing process (for further details about the MIO intervention, see Suchman, DeCoste, Ordway, & Bers, 2013). In this study, MIO was delivered by two Ph.D.-level clinical psychologists, including author N.S.
First Randomized Trial
We previously reported findings from the first randomized, controlled trial with 47 mothers enrolled in substance abuse treatment and caring for a child between birth and three years of age. In this trial, we tested MIO in comparison with Parent Education (PE), a 12-session individual psychoeducational comparison intervention where developmental guidance and parenting strategies were provided by an individual counsellor (see Suchman, DeCoste, McMahon, Rounsaville, & Mayes, 2011). At the end of 12 sessions, in comparison with mothers who received PE, those who received MIO demonstrated higher levels of RF, representational coherence and caregiving behavior, and these differences were sustained at a 6-week follow up. At the 6 week follow up, both groups also had significantly reduced psychiatric symptoms and substance use. MIO children showed clearer communication bids with their mother at post-treatment and these differences were also sustained at the 6-week follow up. A test of treatment mechanisms (see Suchman, DeCoste, Rosenberger, & McMahon, 2012) showed that improvement in maternal RF capacity was directly related to improvement in maternal caregiving behavior.
Current Investigation
Here we report findings from the second randomized, controlled trial testing MIO in comparison with Parent Education (PE) in a sample of 87 mothers enrolled in substance abuse treatment and caring for a child between 11 months and five years of age. The aims of this second trial, in addition to replicating the first trial in a larger sample, were to (a) determine if results would be replicated in a sample of mothers caring for children in a wider age range (up to five years old), (b) measure treatment impact on child attachment, (c) examine treatment outcomes at 3-month and 12-month follow-up, and (d) explore potential moderating effects of addiction severity.
We predicted that, in comparison with mothers enrolled in PE, mothers enrolled in MIO would demonstrate: (1) greater capacity for mentalizing and more coherent caregiving representations at the end of treatment with group differences sustained at the 3-month follow up, (2) more sensitive caregiving behavior by the end of treatment with group differences sustained at the 3-month and 12-month follow up visits, and (3) lower levels of relapse to substance use and lower levels of psychiatric distress at the 3-month follow up.
We also predicted that, in comparison with children of mothers enrolled in PE, children with mothers enrolled in MIO would demonstrate: (1) more secure attachment at post-treatment, and (2) better communication, involvement and dyadic reciprocity with their mothers at the end of treatment, with group differences sustained at the 3-month and 12-month follow up visits.
With regard to addiction severity, we expected that MIO would confer a protective benefit to mothers and children. Specifically, for mothers with greater addiction severity, MIO would demonstrate a greater protective function than PE for levels of maternal reflective functioning, quality of mother-child interactions and child attachment security.
Method
Overview
This trial was conducted on site at a substance abuse treatment center located in a small northeastern city where many of its clients are exposed to urban problems (e.g., crime, poverty, minimal affordable housing) typically identified with larger cities. Interested mothers enrolled in outpatient services at the treatment center who were caring for a child between 11 and 60 months of age and eligible to participate were randomized to 12 sessions of a manualized intervention: Mothering from the Inside Out (MIO) or 12 sessions of Parent Education (PE) – a manualized, individual, psychoeducational active control comparison developed for this study. The study included a 6-week baseline assessment, a 12-week intervention, and a 3-month and 12-month follow up assessment. Treatment fidelity was measured using a scale developed during the first randomized trial. Treatment outcomes included maternal reflective functioning, representational coherence, maternal psychiatric symptoms, maternal substance abuse, mother-child interaction quality, and child attachment status. All procedures were approved by the Yale University School of Medicine Institutional Review Board.
Recruitment and Consent Procedures
Mother-child dyads were eligible to participate if the mother was enrolled in the outpatient treatment program for her substance abuse, English speaking, and caring for a child between 11 and 60 months of age. Dyads were excluded if the mother had severe mental health problems (e.g., suicidality, psychosis), significant cognitive impairment, or required inpatient hospitalization or detoxification. Dyads were also excluded if the target child had a serious illness or significant developmental delay.
Mothers were recruited via clinician referrals, research assistant visits to clinic medication lines and group meetings, research interest forms, and flyers posted throughout the treatment clinic and word-of-mouth. Interested mothers were screened for eligibility by research assistants either in person or by phone. Mothers who met eligibility criteria met individually with a research assistant to complete informed consent procedures. Mothers caring for more than one eligible child were allowed to choose which child would participate with them. Mothers who had a child living with a relative were permitted to enroll if they had regular contact with the child (e.g., 3 – 4 days per week). In this case, the relative or legal guardian of the child provided consent for the child’s participation. During the informed consent meeting, permission was asked to access program clinical records to ascertain information about attendance and relapses to substance use. Limits of confidentiality and the protection of research records under a Certificate of Confidentiality were explained. The compensation schedule for research assessments was also reviewed.
Sample
Mothers
One hundred mothers caring for a child between 11 and 60 months of age consented to participate. Of these mothers, 87 completed the initial intake evaluation and were randomized to treatment (40 MIO, 47 PE), constituting the Intention-to-Treat (ITT) sample (n = 87). On average, mothers were 29.68 (SD = 5.37) years old, had completed 12.39 (SD = 2.16) years of education, and were caring for 1.67 (SD = .97) children under 16 years of age. Mothers’ verbal intelligence (Mean standardized score = 91.48, SD = 10.35) and non-verbal intelligence (Mean standardized score = 97.47, SD = 12.87) fell within the range considered normal. Most of the mothers were Caucasian (77%), 13.8% were African American, 3.4% were Hispanic or Latino, and 5.7% were of mixed race. A large percentage of the mothers had never been married (42.5%), 34.5 percent were cohabitating with a partner, 13.8% were married, 6.9% were divorced, and 2.3% were separated. 69.8% were living independently, 35.6% depended on family or friends for housing, and 4.6% were homeless at the time of enrollment. Approximately one-third (32.2%) of children were involved with the Child Protective Services. Most mothers (89%) carried a primary diagnosis of heroin or non-prescription opioid dependence, 6.1% were met criteria for alcohol dependence, 3.7% were diagnosed with cocaine dependence and 1.2% cannabis dependence. Most (72.4%) were enrolled in methadone-maintenance and 12.6% were enrolled in suboxone treatment. A majority of mothers had significant family histories of substance abuse including their own mother (53.5%) and father (75.9%) and the target child’s father (76.7%). On average, cannabis and alcohol use was initiated in early teens and other drug use (e.g., heroin, opioids, cocaine, and hallucinogens) was initiated in later teens or early 20s. All mothers reported having experienced withdrawal and dependence symptoms at some point in their substance use history. On average, mothers reported clinically-significant levels of psychiatric distress (BSI Global Severity Index mean T score = 60.37, SD = 10.06). As shown in Table 1, the only significant group difference in baseline maternal characteristics involved cocaine use during pregnancy; more MIO than PE mothers reported use.
Table 1.
Baseline characteristics of mothers, fathers and target children
| Mean (SD) or Percentage | t/X2 | da/ϕ or Vb | ||
|---|---|---|---|---|
| Maternal demographic factors | MIO (n=40) | PE (n=47) | ||
| Age | 29.89 (5.10) | 29.43 (5.73) | .40 | .06 |
| Education (years) | 12.10 (1.87) | 12.64 (2.38) | 1.16 | .17 |
| Unemployed | 75.00 | 85.10 | 1.40 | .13 |
| Ethnicity | .44 | .07 | ||
| Caucasian | 80.00 | 74.50 | ||
| Hispanic/Latino | 2.50 | 4.30 | ||
| African American | 12.50 | 14.90 | ||
| Other | 5.00 | 6.40 | ||
| Intelligence | ||||
| Standardized Verbal | 91.60 (11.84) | 91.39 (9.25) | −.07 | .01 |
| Standardized Non-Verbal | 95.04 (14.50) | 99.30 (11.37) | 1.26 | .23 |
| Marital status | 2.23 | .16 | ||
| Never married | 50.00 | 36.20 | ||
| Cohabitating | 32.50 | 36.20 | ||
| Divorced | 5.00 | 8.50 | ||
| Separated | 2.50 | 2.10 | ||
| Married | 10.00 | 17.00 | ||
| Domicile | 3.03 | .19 | ||
| Independent | 50.00 | 68.10 | ||
| Dependentc | 45.00 | 27.70 | ||
| Homeless | 5.00 | 4.30 | ||
| Biological children | 1.90 (1.15) | 2.04 (1.08) | .60 | .09 |
| DCF-involved (current) | 35.00 | 29.80 | .27 | .06 |
|
| ||||
| Substance use history | ||||
| Primary Diagnosis | 8.28† | .31 | ||
| Heroin/opioids | 89.5 | 83.0 | ||
| Alcohol | 2.6 | 8.5 | ||
| Cocaine | 0.0 | 6.4 | ||
| Cannabis | 0.0 | 2.1 | ||
| PCP | 7.9 | 0.0 | ||
|
| ||||
| Opiate replacement therapy | ||||
| Methadone | 74.5 | 70.0 | .22 | 05 |
| Suboxone | 15.0 | 10.6 | .37 | .07 |
|
| ||||
| Addiction Severity | 9.95 (2.36) | 10.38 (2.25) | −.63 | |
| Family history of substance abuse | ||||
| Own mother | 59.0 | 48.9 | .86 | .10 |
| Own father | 76.3 | 74.4 | .04 | .02 |
| Target child’s father | 79.5 | 73.5 | .36 | .07 |
| Early initiation | ||||
| Alcohold | 42.5 | 42.6 | .00 | .00 |
| Cannabisd | 55.3 | 52.5 | .07 | .03 |
| Heroine | 47.5 | 51.1 | .11 | .04 |
| Opioidse | 67.5 | 70.2 | .07 | .03 |
| Cocainee | 72.5 | 55.3 | 2.74 | .18 |
| Withdrawal symptoms | 100.0 | 100.0 | n/a | n/a |
| Dependence symptoms | 100.0 | 97.9 | .86 | .10 |
| Psychiatric distress (T ≥ 60) | 65.0 | 57.4 | .52 | .08 |
| Moderate depression (BDI ≥ 14) | 62.5 | 51.1 | 1.15 | .12 |
|
| ||||
| Target child’s father characteristics | ||||
| Age | 34.30 (8.02) | 34.26 (7.14) | −.02 | .00 |
| Living at home | 42.5 | 48.9 | .36 | .06 |
| Employed | 60.9 | 66.7 | .15 | .06 |
| History of substance use | 73.5 | 79.5 | .36 | .07 |
|
| ||||
| Pre- and Post-natal history (with target child) | ||||
| Substances used during pregnancy | ||||
| Cigarettes | 84.2 | 76.1 | .85 | .10 |
| Cocaine | 28.9 | 8.7 | 5.82* | .26 |
| Heroin | 17.9 | 15.2 | .11 | .04 |
| Opioids | 20.5 | 6.5 | 3.67† | .21 |
| Cannabis | 15.8 | 10.9 | .44 | .07 |
| Alcohol | 10.5 | 6.5 | .44 | .07 |
| Hallucinogens | 5.3 | 1.0 | 2.48 | .17 |
| Infant birth weight | 6.73 (1.48) | 7.16 (1.44) | 1.13 | .21 |
| Infants requiring detox at birth | ||||
| Methadone detoxf | 84.2 | 68.0 | 1.51 | .19 |
| Suboxone detoxg | 37.5 | 33.3 | .04 | .03 |
| Days hospitalized | 16.61 (15.24) | 12.37 (11.98) | −1.19 | .04 |
| Age at pediatric visit (months) | 2.92 (3.01) | 2.21 (2.23) | −1.01 | .22 |
|
| ||||
| Target child characteristics | ||||
| Age (months) | 27.83 (15.75) | 27.45 (13.97) | −.12 | .02 |
| Male | 52.5 | 55.3 | .07 | .03 |
| Lives with… | .03 | .02 | ||
| mother | 95.0 | 95.7 | ||
| another relative | 5.0 | 4.3 | ||
| Developmental assessment | ||||
| Bayley (11–36 months) n=40c | ||||
| Cognitive | 1.32 | .18 | ||
| Competent | 80 | 90 | ||
| Emerging risk | 15 | 10 | ||
| At risk | 5 | 0 | ||
| Receptive Communication | 2.26 | .25 | ||
| Competent | 72.2 | 78.9 | ||
| Emerging risk | 16.7 | 21.1 | ||
| At risk | 11.1 | 0.0 | ||
| Expressive Communication | .01 | .01 | ||
| Competent | 83.3 | 84.2 | ||
| Emerging risk | 16.7 | 15.8 | ||
| At risk | 00.0 | 00.0 | ||
| Early Screening Profile (37–60 months) n = 19 | ||||
| Cognitive/Language | .78 | .20 | ||
| Above average | 37.5 | 36.4 | ||
| Average | 62.5 | 54.5 | ||
| Below average | 0.0 | 9.1 | ||
Effect size d: .20 = small, .50 = medium, .80 = large (Cohen, 1988)
Cramer’s ϕ was used for two categories and Cramer’s V was used for > 2 categories, .10 = small, .30 = medium, .50 = large
living in supervised housing or in the home of a family member
≤ 13 years of age
≤ 18 years of age
children of methadone-maintained mothers only
children n of suboxone-prescribed mothers only
p < .10,
p < .05, two-tailed
Fathers
Per mothers’ reports, fathers of target children were 34.28 years old (SD = 7.48), on average, and 54.0% were living separately from the mother and target child. A majority of fathers were employed (63.4%) but also had histories of substance use (76.7%). As shown in Table 1, there were no significant group differences in paternal characteristics.
Target children
Pregnancy with the target child was generally unplanned (79.7%) and mothers reported learning about their pregnancy and attending their first prenatal visit at week 7.34 (SD = 4.82). A majority of mothers (96.6%) reported they continued to receive prenatal care throughout their pregnancy. A majority of mothers (83.1%) reported using nicotine during pregnancy, 25% reported using cocaine, 16.9% reported using heroin, 15.3% reported using cannabis, 10.2% reported using other opioids, 10.2% reported using alcohol and 1.7% reported using hallucinogens. The average birth weight of target children was 6.96 (SD = 1.46) pounds. 77.8% of the target children whose mothers were enrolled in methadone-maintenance required a methadone detox at birth and a 37.5% of the children whose mothers were prescribed suboxone treatment required a suboxone detox. Many mothers and infants (48.1%) were separated at birth and infants remained in the hospital for an average of 14.38 (SD = 11.39) days. All mothers who were separated reported visiting their infants in the hospital; 30% reported visiting daily, 30% reported visiting nightly, 35% reported visiting every day and night and 5% reported visiting some days and nights. Almost all mothers (98.3%) reported that their infants had an assigned pediatrician and the average age of first pediatric visit was 2.55 (SD = 2.62) months. At baseline, 28.8% of mothers expressed developmental concerns about the target child.
Target children were 27.62 (SD = 14.73) months of age, on average, and 54% were male. A large majority (95.4%) lived with their mother at baseline whereas 4.6% lived with another family member and had frequent visits with the mother (e.g., 3 – 4 days per week). On the Bayley Developmental Screen Cognitive Scale, 12.5% of children between 11 to 26 months of age scored as emerging risk and 2.5% scored at risk. On the Bayley Receptive Communication Scale, 18.9% scored as emerging risk and 5.4% scored at risk. On the Bayley Expressive Communication screen, 16.2% scored as emerging risk and 0% scored at risk. On the Early Screening Profile Cognitive/Language Scale, 5.3% of children between 37 and 60 months scored below average. As shown in Table 1, there were no significant group differences in target child characteristics.
Assessment Procedures
Baseline
Following consent, the mother and participating child were scheduled for six weekly baseline assessment visits (1 – 2 hour duration) during which the mother completed a battery of assessments including an initial intake interview as well as measures of reflective functioning, mental representations of caregiving, psychiatric symptoms, substance use and intelligence (see Table 2 for assessment schedule). She and her child also completed assessments measuring interaction quality, child developmental status and child attachment status. Mothers received compensation and children received a developmentally-appropriate toy for each completed assessment. Immediately following the intake interview, in the second baseline week, mothers were randomized to treatment and introduced to their assigned MIO therapist or PE specialist. Early randomization was considered important for building a working alliance, preventing attrition and processing any emotional distress triggered by the assessments.
Table 2.
Assessment Schedule
| Measure | BL | Wkly | Mnthly | Post | FU1 | FU2 |
|---|---|---|---|---|---|---|
| Intake Evaluation | x | |||||
| Kaufman Brief Intelligence Test | x | |||||
| 11 – 36 months: The Bayley Scales of Infant and Toddler Development Screening Test | x | |||||
| 37 – 60 months: Early Screening Profiles | x | |||||
| Parent Development Interview | x | x | x | |||
| Working Model of the Child Interview | x | x | x | |||
| Curiosity Box Paradigm | x | x | x | x | ||
| Strange Situation Paradigm | x | x | ||||
| Beck Depression Inventory | x | |||||
| Brief Symptom Inventory | x | |||||
| Timeline Follow Back Interview | x | |||||
| Weekly Checklist of Services | x |
Table 3.
Baseline scores for parenting and child outcome measures
| Maternal reflective functioning | MIO | PE | F | d |
|---|---|---|---|---|
| Mean RF | 3.08 (.50) | 3.12 (.49) | .38 | .06 |
| Potential RF | 4.39 (.90) | 4.57 (.73) | .89 | .16 |
| Maternal working model of the child | ||||
| Overall Coherence | 2.47 (.31) | 2.60 (.40) | 1.54 | .26 |
| Psychiatric Symptoms | ||||
| BDI Depression Score | 15.78 (10.21) | 15.04 (11.92) | −.30 | .05 |
| BSI Global Symptom (T-Score) | 60.38 (10.10) | 60.36 (10.14) | −.01 | .00 |
| Mother-child dyadic adjustment | ||||
| Curiosity Box | ||||
| Maternal Sensitivity | 3.55 (.70) | 3.47 (.77) | −.50 | .08 |
| Child Involvement | 3.41 (.63) | 3.40 (.64) | −.06 | .01 |
| Dyadic Reciprocity | 3.58 (.94) | 3.38 (1.03) | −.93 | .14 |
| Child Attachment | ||||
| Strange Situation | 3.45 | .24 | ||
| Secure | 57.1 | 58.1 | ||
| Insecure | 21.4 | 35.5 | ||
| Disorganized | 21.4 | 6.5 |
Effect size d: .20 = small, .50 = medium, .80 = large (Cohen, 1988)
covariates included child age and sex
Cramer’s ϕ: .10 = small, .30 = medium, .50 = large (source?)
p < .05;
p < .01;
p < .001, two-tailed
p < .05, two-tailed
Treatment
During the 12-week treatment phase, mothers met weekly for a one hour individual session with their assigned MIO therapist or PE specialist and completed brief surveys about their recent substance use and additional services received in the community. Brief psychiatric symptom questionnaires were completed every four weeks.
Post-treatment
At the end of the 12 treatment sessions, mothers completed four post-treatment visits (1 – 2 hour duration) during which maternal measures of reflective functioning, mental representations of caregiving, psychiatric symptoms, and substance use were repeated. Mothers and target children also repeated assessments of interaction quality and child attachment status.
Follow up
During the first 3 months following the post-treatment assessments, mothers were scheduled for brief (30 minute) twice-monthly visits to complete assessments of psychiatric symptoms, substance use and additional services received. Then, during follow up weeks 12 through 15, maternal measures of reflective functioning, mental representations of caregiving, psychiatric symptoms and substance use were repeated. Mothers and target children also repeated assessments of interaction quality. On the one year anniversary of study completion, mothers returned with the target child for a follow-up visit to repeat one assessment of interaction quality and mothers were also interviewed about any changes they experienced in the areas of parenting, education, employment, housing, and legal involvement (mother-child interaction findings are reported here; follow-up interview results are forthcoming).
Child care
Developmentally-informed child care was available to all target children in the study at every visit. Research staff received weekly supervision from the developmental specialist to discuss concerns about child safety and development. On average, MIO children received 49.96 (SD = 23.30) hours and PE children received 41.04 (SD = 23.72) hours of child care per study month and group differences were not significant (t = 1.76, p = .08, d = .27).
Compensation and attendance incentives
Procedures used to minimize potential barriers to participation (e.g., providing a child-friendly environment with developmentally-informed child care, offering healthy snacks, diapers, spare clothing and bus passes, providing graduate certificates upon completion) are described in detail elsewhere (see Suchman et al., 2013). Economic compensation for research visits were also structured to maximize motivation for assessment completion. Payment for assessment completion increased incrementally from baseline ($10 – $15 per assessment) through follow-up ($35 – $40 per assessment). Bonus payments of $5 to $10 were also provided for on time assessment completion. Target children received a small developmentally-appropriate toy for their participation in all assessments.
Attendance
Of the 87 randomized mothers, 70 (80%) completed baseline assessments and continued to treatment. Reasons for attrition included transportation problems, relocation, family issues, substance use relapse, illness and discharge or withdrawal from the addiction program. On average, MIO mothers attended 71% of their clinical appointments and 81% of their research appointments whereas PE mothers attended 75% of their clinical appointments and 84% of their research appointments. There were no significant group differences in clinical (t = 1.18, p = .24, d = .06) or research (t = 1.75, p = .08, d = .06) attendance.
Parent Education Comparison
Parent Education (PE) was designed and manualized (DeCoste, Dalton, de las Heras Kuhn, & Dennehy, 2010) to represent psychoeducational parenting programs that are typically available in community settings. PE was designed as an individual intervention tailored to the specific interests and concerns of the parent in order to control for treatment dose and the opportunity to form a working alliance. PE is a structured intervention that provides developmental guidance and parenting strategies for challenges that are typically encountered by parents with young children (e.g., child tantrums, bed wetting, sleep habits, limit setting, developmental milestones) and challenges that are typical for parents in substance abuse treatment (e.g., keeping children safe, self-care). Mothers met weekly with their assigned PE specialist to review a pamphlet chosen by the mother. Pamphlets were written at a 4th grade reading level.
Constructs and Measures
Treatment integrity
The Revised MIO/PE Adherence Rating Scale (Suchman, Rosenberger, & DeCoste, 2010) was used to measure treatment integrity. The scale contains Generic items measuring alliance-building efforts that were expected to occur equally in both MIO and PE and Unique MIO and PE items measuring behaviors that were expected to occur primarily in MIO or PE, respectively. To streamline rating procedures and insure that items were robust, the original 23-item scale (Suchman, Rosenberger, & DeCoste, 2006) was reduced to 18 items by combining those that overlapped. Next, three independent raters trained by author N.S. rated 36 randomly selected sessions to establish interrater reliability. Interclass correlations for 7 of the 18 items were considered inadequate (< .70) and these items were omitted. Interclass correlations for the remaining 11 items comprising the final scale ranged from .74 (p < .05) to .96 (p < .001). Raters coded 428 sessions from a randomly selected pool of 37 subjects (MIO = 15 and PE = 22) who attended 11 sessions, on average.
Total scale scores were computed by summing items on each subscale scale. For each session, a score ≥ 3 on the Generic scale (Range = 0 – 6) is considered adequate. For MIO sessions, a score ≥ 2 on the Mentalizing for Child and Relationship subscale (Range = 0 – 6) and a score ≥ 3 on the Mentalizing for Self subscale (Range = 0 – 6) are considered adequate fidelity. For PE sessions, a score ≥ 2 on the Unique PE scale (Range = 0 – 4) is considered adequate. As shown in Table 4, MIO and PE clinicians achieved adequate fidelity to their respective interventions.
Table 4.
MIO and PE Fidelity Scale item factor loadings and mean comparisons
| Scale item | Factor Loadings | Mean (SD) | t | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 1 | 2 | 3 | 4 | 5 | MIO | PE | |||
| UNIQUE TO MIO | |||||||||
|
| |||||||||
| • MENTALIZING FOR CHILD AND RELATIONSHIP | 2.06 (.84) | 1.48 (.61) | 2.42* | ||||||
| 1. Developmental guidance about child’s emotional needs and attachment-based parenting strategies | .12 | .79 | .43 | .20 | −.08 | ||||
| 2. Explores thoughts and emotions underlying the child’s behavior | .44 | .79 | .13 | .09 | .03 | ||||
| 3. Explores mother’s mental representations of her child and their relationship | .32 | .76 | .13 | −.06 | .07 | ||||
|
| |||||||||
| • MENTALIZING FOR SELF | 3.48 (1.49) | .86 (.66) | 6.38*** a | ||||||
| 4. Explores thoughts and emotions underlying mother’s behaviors | .92 | .21 | .07 | .06 | .08 | ||||
| 5. Helps mother make sense of her own thoughts and emotions | .90 | .19 | −.10 | .14 | −.10 | ||||
| 6. Explores how mother’s thoughts and emotions might affect the child | .79 | .46 | .13 | −.00 | −.03 | ||||
|
| |||||||||
| UNIQUE TO PE | 1.63 (.64) | 2.24 (.90) | −2.40* | ||||||
| 7. Developmental guidance about child behavior and behavior-based parenting strategies. | .02 | .20 | .97 | −.00 | −.03 | ||||
| 8. Developmental guidance about child’s physical safety. | .03 | .21 | .97 | .05 | −.04 | ||||
|
| |||||||||
| GENERIC | 4.00 (.06) | 3.98 (.14) | .49 | ||||||
| 9. Builds alliance through listening and making encouraging, supportive statements | .12 | .08 | .15 | .86 | .14 | ||||
| 10. Remains neutral during descriptions reflecting questionable parenting attitudes and strategies. | .04 | .03 | −.08 | .89 | .11 | ||||
| 11. Assists mother to address concrete, practical problems or immediate crises when asked. | −.03 | .03 | −.07 | .25 | .96 | ||||
Equal variances not assumed
p < .05;
p < .01;
p < .001, two-tailed
To confirm intervention construct validity, a principal components analysis was conducted first, extracting Eigenvalues greater than 1. A scree plot indicated a five-factor solution as the best fit. Next, a Varimax rotation was used in a second factor analysis with extraction restrained to five factors. As shown in Table 4, five robust factors were identified with two factors representing the MIO intervention, one factor representing the PE intervention, and two factors representing Generic interventions.
Discriminant validity was confirmed using independent t tests and results are reported in Table 4. MIO clinicians scored significantly higher than PE clinicians on both Unique MIO subscales and PE clinicians likewise scored significantly higher than MIO clinicians on the Unique PE scale. MIO and PE clinicians were not expected to differ in fidelity to Generic interventions and this absence of difference is reflected in the non-significant t test results.
Intake interview
A 1.5 hour structured clinical interview was used to gather information about the mother’s developmental and family history, substance use (including during pregnancy), psychiatric and trauma history, medical, legal and employment history, and pre- and post-natal history of the target child. Information from this interview was used to establish primary substance use and psychiatric diagnoses, determine addiction severity, and identify baseline demographic and psychosocial characteristics of the sample.
Maternal addiction severity
A 15-item binary scale representing cumulative risk for severe addiction was computed to serve as a moderator, using items from the intake evaluation and psychiatric survey. Scale item domains included (a) family history of substance abuse and mental illness, (b) early onset of substance use initiation (e.g., alcohol and cannabis before age 13, heroin and cocaine use before age 18), (c) higher than average endorsement of triggers and withdrawal and dependence symptoms, (d) higher than average endorsement of exposure to traumatic events, and (e) endorsement of clinically significant levels of psychiatric distress. The scale sum (range = 0 – 15) was used to represent overall addiction severity.
Maternal intelligence
The Kaufman Brief Intelligence Test (K-BIT; Kaufman & Kaufman, 1990) was used to characterize the sample in terms of IQ. The KBIT is a brief (30 min) standardized intelligence screening measure with good reliability and concurrence with other widely used intelligence measures (Miller, 1995; Young, 1995).
Maternal representations
Maternal reflective functioning and internal working model of the child were the two representational constructs measured.
Maternal reflective functioning
The 33-item Parent Development Interview (PDI; Slade, Aber, Berger, Bresgi & Kaplan, 2003) was used to measure parental reflective functioning. The PDI is a semi-structured interview that requires parents to describe specific interactions with the target child. Some questions (called “demand” questions) are designed to explicitly probe for mental states in the mother (e.g., “Have you ever been angry as a parent?” “Can you tell me about a time recently when you felt that way?”) or the child (e.g., “Does your child ever get emotionally upset?” “Can you tell me about the last time that happened?”) Other questions (called “permit” questions) that have a more general focus (e.g., “Can you tell me about a time in the last week that you and your child really clicked?”) are designed to permit rather than demand mentalizing activity. For this study, a shorter, 14-item version of the PDI was developed, with permission from the measure’s primary author, in order to minimize assessment burden, avoid overlap with the Working Model of the Child Interview, and include positive emotion items (e.g., “Have you ever felt deeply touched or moved as a parent?”) because mothers with addiction problems sometimes have difficulty mentalizing about positive affect. Each question is followed by a probe about the mother’s and the child’s experience. This version typically required 1 hour to administer.
Interviews were video-recorded and transcribed verbatim by a professional transcription service. Dates, ID numbers and identifying information were masked to keep coders blind to subject and time point. Each PDI interview item is coded on a −1 to 9 scale depending on the amount and quality of apparent mentalizing. A score ≤ 3 is considered ‘pre-mentalizing’ because it represents the absence of awareness of mental states except for vague, unelaborated, cliché-like references (e.g., “He doesn’t have a care in the world”). A score of 5 is considered the benchmark for adequate mentalizing and indicates a demonstrated awareness of mental states and how they influence behaviors and relationships (e.g., “I know when she likes her snack because she smiles and claps her hands … and that makes me proud”). Higher scores indicate more complex and nuanced understanding of the nature of mental states and how they influence behavior and relationships. All PDIs were coded by a colleague at another institution (author J.B.), who was trained by the PDI author and author N.S. and remained blind to all other information about subjects and treatment assignments. A randomly selected sample of ten interviews was used to assess interrater reliability. Interclass correlations for two items were < .70 and the items were therefore omitted. Interclass correlations for the remaining 12 items ranged from .77 (p < .05) to .98 (p < .001). The outcome score of greatest interest was the mean RF score for all 12 items which yielded a .80 Cronbach’s α for this sample. We were also interested in examining the highest level of RF achieved on any single item as an indicator of each subject’s potential for mentalizing (this variable was labeled Potential RF).
Maternal Working Model of the Child
The Working Model of the Child Interview (WMCI; Zeanah & Benoit, 1993) is a semi-structured interview used to assess the content and quality of a parent’s mental representations of children ages birth to six. The interview includes questions about the mother’s perceptions of distinctive characteristics of the child and their relationship, focusing primarily on times when the child’s attachment needs are typically activated (e.g., parent-child separations, child illness or injury). For this study, a 15-item version of the interview was developed with permission from the measure’s primary author to minimize assessment burden and avoid overlap with PDI items. Six 5-point items representing distinct representation characteristics were used to characterize representation quality. The items include Richness (degree of detail and elaboration about child’s personality), Openness (acceptance and flexibility in expectations for the child over time), Coherence (clarity and credibility of narrative), Caregiving Sensitivity (recognition and responsiveness to child’s emotional distress), Acceptance (acknowledgement of parental role and responsibility and child’s dependence on parent for safety and care) and Emotional Involvement (expression of emotional investment in the child and caregiving relationship). A score of 3 on any subscale (range = 1 – 5) is considered the “benchmark” score for adequate though unremarkable quality. Scores ≤ 2 are considered to represent potential risk for the caregiving relationship and child. Interviews were video-recorded and then coded by a clinical psychologist (trained by the senior author, N.S.) who was also a clinical consultant to the research team. A randomly selected sample of 10 interviews was used to assess interrater reliability. Interclass correlations for the six items ranged from .77 (p < .01 to .91 (p < .001). The outcome score of greatest interest for this study was the mean score for all six items – representing overall coherence - which yielded a .88 Cronbach’s α for this sample.
Maternal psychiatric symptoms
Psychiatric symptoms were assessed the a widely used Brief Symptom Index (BSI; Derogatis, 1993) Global Severity Index (Cronbach’s α = .97 for this sample).
Maternal substance use
Substance use was measured with the Timeline Followback interview (TLFB; Sobell & Sobell, 1992, 1996), a widely-used calendar method for assessing substance use. The TLFB uses a calendar to gather retrospective estimates of an individual’s daily substance use over a specified period of time. The TLFB has demonstrated good temporal stability for alcohol and psychoactive substance use (for both general and specific drug classes). The TLFB has also demonstrated convergent and discriminant validity; percentage of days of substance use for different time intervals have had moderate to high correlations with other widely used measures of substance use severity, including urine assay results (Fals-Stewart, O-Farrell, Freitas, McFarlin, & Rutigliano, 2000). In the event of a missed visit, the TLFB is designed to capture data from the missing time interval. For each month of the mother’s participation in the study, she received a score of “0” if she reported no use of the substance and a score of “1” if she reported at least one relapse during that month.
Child developmental screening
Two brief developmental assessments were used to screen for possible delays in target children’s functioning. For children 1 to 36 months of age, The Bayley Scales of Infant and Toddler Development Screening Test (3rd Edition; Bayley, 2006) was used to assess whether they were “on track” in their current cognitive and language functioning. For children between 36 and 60 months of age, The Early Screening Profiles (ESP; Harrison, Kaufman, Kaufman, Bruininks, Rynders et al., 1990) was used to assess cognitive and language functioning. Research assistants were trained and supervised by a developmental consultant to conduct the screenings with target children during the baseline phase so that assessment referrals could be made promptly for children identified as being at-risk.
Mother-child interactions
To examine the quality of mother-child interactions under conditions of mild uncertainty, we used the Curiosity Box Paradigm developed by Mayes and colleagues (CBP; Mayes, Carter, & Stubbe, 1993). During the CBP, the mother and child explore a box with 12 toys in two sequential five minute episodes. The first episode involves familiar toys and is used to acclimate the dyad to the exercise and the second episode involves unfamiliar toys chosen to elicit mild uncertainty in the child (e.g., a realistic rubber snake or plastic bug replica). All sessions were video-recorded and second episodes were coded with Feldman’s system for Coding Interactive Behavior (CIB; Feldman, 1998). The CIB uses a 5-point scale for rating parent, child and dyadic behaviors that are likely to promote or inhibit emotional regulation in the child and dyad. Three composite scales, including the 12-item Maternal Sensitivity Scale (Cronbach’s α = .93), the 8-item Child Involvement Scale (Cronbach’s α = .84), and the 3-item Dyadic Reciprocity Scale (Cronbach’s α = .97 were used to assess interaction quality. All sessions were coded by a rater from Dr. Feldman’s lab who was blind to treatment assignment, time and other subject information. A randomly selected subsample of 10 interactions was also coded by a certified coder on our research team (author C.D.) to assess interrater reliability. Interclass correlations for the 23 items ranged from .77 (p < .05) to .99 (p < .001).
Child attachment classification
The Strange Situation procedure (SSP; Ainsworth, Blehar, Waters, & Wall, 1978) was used to assess child attachment classification. There is no single method for coding attachment classification that covers the age span from 11 to 60 months. However, a commonly accepted approach to measuring young children’s response to attachment-based parenting interventions (see Solomon & George, 2008; Hoffman, Marvin, Cooper, & Powell, 2006; Toth, Rogosch, Manly, & Cicchetti, 2006) in samples of children in this (and broader) age ranges has been to use the Ainsworth SSP (8 episodes, 3 with a stranger; Ainsworth et al., 1978) for children younger than 24 months and the MacArthur Preschool SSP (5 episodes, with no stranger; Cassidy & Marvin, 1992) for children older than 24 months (and up to 54 months) and examine changes in attachment status across three global domains: Secure, Insecure, and Disorganized. Although practice effects are only likely to occur when the SSP is repeated over a very short-term (e.g., 2 – 4 weeks; see Solomon & George, 2008), we took steps to further minimize practice effects by conducting the SSP in a new setting with a new stranger unfamiliar to the child and mother for each visit. We also used objects available for play that the children had likely not seen before (e.g., novel toys, objects and materials). The SSP was video recorded and then coded by two off site consultants who were reliable on both methods. Ten randomly selected SSPs were used to assess interrater reliability for assessment of global attachment classification and the interclass correlation for this domain was .72 (p < .05). Also, when confidence in codes was questionable, the coders conferred to arrive at a common score. Because we were most interested in testing group differences in rates of improvement in attachment classification from baseline to post assessment visits, we created a binary outcome where 0 represents either (a) no pre-to-post treatment change from insecure or disorganized classification or (b) a decline to a more insecure classification (e.g., secure ➔ insecure; disorganized or insecure ➔ disorganized). A score of 1 represents either (a) maintenance of a secure classification or (b) change to a more secure classification (e.g., disorganized ➔ insecure; secure or insecure ➔ secure).
Data analysis
MIO versus PE comparisons
Because we were most interested in testing the efficacy of MIO vs PE after controlling for pre-existing group differences (rather than examining within-subject change; see Gottman & Rushe, 1993; Rogosa, 1995), analysis of variance was considered the best approach for examining outcomes in reflective functioning, mental representation coherence, and mother-child interaction at the end of treatment and follow-up periods, respectively. A graphic representation of these outcomes across time indicated that a linear model from baseline-to-follow-up was not supported, precluding the use of hierarchical linear modeling. Baseline scores were included as covariates in all analyses and child age and gender were also included as covariates in analyses involving mother-child interactions. A GLM repeated measures approach was used to test for Group × Time slope differences in outcomes collected on a weekly (e.g., substance use) or monthly basis (e.g., psychiatric symptoms). A two-tailed significance test and examination of effect size d (where .20 = small, .50 = medium, and .80 = large effect; Cohen, 1988) were used to identify meaningful group differences. Chi square analysis along with Fischer’s Exact Test and Cramer’s phi (where .10 = small, .30 = medium, and .50 = large effect; Cohen, 1988) were used to test for group differences in change in attachment status.
All outcome analyses were conducted with both the intention-to-treat (n = 87) and treatment completer (n = 67) samples. There were no significant group differences (MIO versus PE) in the number or pattern of missing values and therefore bias due to missingness was ruled out. In the first sample, for subjects who completed baseline assessments only, missing values for later time points were replaced with baseline values as a conservative estimate that assumed no improvement. For subjects who completed baseline and post-treatment assessments but missed follow-up assessments (≤ 10% of the intention-to-treat sample), missing values were replaced by the group mean. To insure that mean substitution did not significantly alter (i.e., reduce) variance (see Schafer & Graham, 2002), equivalence of variances was confirmed across the three time points and no significant differences were found. Results for the two samples were then compared and, for all reported outcomes, patterns were similar across the two samples. Therefore, only results for the intention-to-treat sample are reported here. Because the sample size is moderate, we report effect sizes as well as significance test results.
Moderation analyses
Regression analysis was used to test for presence of significant Addiction Severity × Treatment interactions in relation to improvement in reflective functioning, maternal sensitivity, child involvement, dyadic reciprocity, and child attachment status. Because simple change scores calculated with continuous scores (i.e. subtracting the baseline score from the post-treatment) contain inherent bias due to baseline scores, we followed methods recommended by Cohen & Cohen (1983, pp.413–425) to remove baseline score bias. (Again, we were most interested in examining efficacy in terms of treatment group differences after controlling for baseline scores.) For continuous outcomes, post-treatment and follow-up scores were regressed on baseline scores and the residual variance (with baseline variance partialed out) was used to represent change. This method provides a reliable estimate of outcome that is not affected by correlations between baseline and outcome scores. Next, the Addiction Severity × treatment interaction term was computed with centered addiction severity scores. Finally, for continuous dependent variables, treatment condition, addiction severity score and the interaction term were entered simultaneously into a standard linear regression analysis. Interactions with small-to-moderate or larger effect sizes (f2 ≥ .02; Cohen, 1988) were further probed using linear regression analysis of simple slopes and t-tests to examine interaction patterns.
For the binary outcome – change in attachment status – we used the binary scores described above. In a binary logistic regression analysis, change in attachment classification served as the outcome variable, with binary score 0 representing no change in insecure attachment or deterioration to a more insecure attachment, and binary score 1 representing maintenance of or improvement toward a secure classification. Significant interactions were further probed with Chi Square analyses to examine interaction patterns.
Results
MIO versus PE Comparisons
Maternal RF and representations
As shown in Table 5, compared to PE mothers, MIO mothers had marginally higher mean RF scores at the end of treatment (d = .20) and significantly higher mean RF scores at the end of the 3-month follow-up period (d = .36). MIO mothers’ Potential RF was significantly higher at post-treatment (d = .34) and follow-up (d = .82) visits compared with PE mothers, with MIO mothers’ Potential RF scores approaching the benchmark of 5 that indicates adequate RF.
Table 5.
Results of primary treatment outcome analyses of covariance controlling for baseline scores
| Post | Follow-up | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| 3 month | 12 month | |||||||||||
|
| ||||||||||||
| Estimated Mean (SE) | da | F | Estimated Mean (SE) | da | F | Estimated Mean (SE) | da | F | ||||
|
|
||||||||||||
| Reflective functioning | MIO | PE | MIO | PE | ||||||||
| Mean RF | 3.25 (.06) | 3.14 (.06) | .20 | 1.90 | 3.23 (.05) | 3.06 (.05) | .36 | 5.57* | – | – | – | – |
| Potential RF | 4.88 (.13) | 4.48 (.12) | .34 | 4.85* | 4.82 (.06) | 4.36 (.06) | .82 | 32.91** | – | – | – | – |
|
| ||||||||||||
| Working model of the child | ||||||||||||
| Overall Coherence | 2.73 (.05) | 2.56 (.04) | .41 | 6.95* | 2.78 (.04) | 2.58 (.04) | .54 | 12.07** | – | – | – | – |
|
| ||||||||||||
| Curiosity Boxb | ||||||||||||
| Maternal Sensitivity | 3.51 (.09) | 3.47 (.08) | .05 | .12 | 3.54 (.10) | 3.35 (.09) | .21 | 2.06 | 3.73 (.08) | 3.41 (.07) | .46 | 9.13* |
| Child Involvement | 3.55 (.08) | 3.37 (.07) | .37 | 2.87† | 3.43 (.08) | 3.33 (.08) | .13 | .72 | 3.57 (.07) | 3.40 (.06) | .28 | 3.51† |
| Dyadic Reciprocity | 3.46 (.12) | 3.40 (.11) | .06 | .13 | 3.45 (.14) | 3.23 (.13) | .21 | 1.37 | 3.73 (.10) | 3.33 (.09) | .45 | 8.54* |
|
| ||||||||||||
| Attachment status | ||||||||||||
| Remained or become more secure | 64.3 | 58.1 | ϕc | X2 | – | – | – | – | – | – | – | – |
| Remained or become insecure or disorganized | 35.7 | 41.9 | .06 | .24 | – | – | – | – | – | – | – | – |
Effect size d: .20 = small, .50 = medium, .80 = large (Cohen, 1988)
covariates included child age and sex
Cramer’s ϕ: .10 = small, .30 = medium, .50 = large (source?)
p < .05;
p < .01;
p < .001, two-tailed
As shown in Table 5, MIO mothers had significantly higher Overall Coherence scores than PE mothers at post-treatment (d = .41) and 3-month follow-up (d = .54) with scores approaching the benchmark score of 3, indicating absence of risk and adequate though unremarkable representation quality.
Maternal psychiatric symptoms
As shown in Table 6, after controlling for baseline scores, PE mothers (d = −.64) showed a marginally lower levels of psychiatric distress than MIO mothers in global psychiatric distress (d = −.39) although, by the end of 3- month follow-up, mothers in both groups were approaching normative levels (i.e. T = 50) of psychiatric distress and low levels of depression.
Table 6.
Repeated measures analyses testing group differences in psychiatric stress substance use over time
| Month | dab | F | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | 6 | Group × Time | ||||||||
| MIO | PE | MIO | PE | MIO | PE | MIO | PE | MIO | PE | MIO | PE | ||
| Psychiatric distress | 58.99 (1.00) |
59.99 (.91) |
58.34 (1.20) |
56.62 (1.09) |
56.86 (1.36) |
55.13 (1.23) |
57.51 (1.41) |
52.69 (1.28) |
54.17 (1.76) |
52.06 (1.60) |
−.39 | −.64 | 4.91† |
| Heroin | .10 (.03) |
.02 (.03) |
.07 (.03) |
.05 (.03) |
.04 (.02) |
.01 (.02) |
.00 (.00) |
.00 (.00) |
.05 (.03) |
.08 (.03) |
−.19 | .21 | 2.20† |
| Opioid | .00 (.00) |
.00 (.00) |
.00 (.00) |
.00 (.00) |
.00 (.00) |
.02 (.02) |
.03 (.02) |
.00 (.00) |
.00 (.00) |
.00 (.00) |
.00 | .00 | 1.30 |
| Cocaine | .08 (.04) |
.09 (.03) |
.10 (.03) |
.09 (.03) |
.08 (.03) |
.07 (.03) |
.05 (.03) |
.09 (.03) |
.07 (.03) |
.12 (.06) |
−.03 | .07 | .90 |
effect size for difference from month 2 to 6
d .20 = small, .50 = medium, .80 = large
p < .05, two-tailed
Maternal substance use
As shown in Table 6, after controlling for baseline scores, a marginally significant group × time interaction suggested that rate of heroin relapse differed for MIO and PE mothers. MIO mothers showed a moderate decrease in proportion of heroin relapses (d = −.29) from month 2 to month 6 whereas PE mothers showed a small increase (d = .21). Rates of relapse to other opioids remained low-to-nil in both groups across time and there were no significant group differences over time. Rates of relapse to cocaine use remained similar for both groups across time.
Mother-child interactions
As shown in Table 5, at the end of treatment, MIO children showed marginally higher levels of engagement with their mothers corresponding to a medium effect (d = .37). There were no notable group differences in maternal sensitivity or dyadic reciprocity. At the end of the 3-month follow-up, although findings were not statistically significant, a small effect was found favoring MIO over PE mothers for sensitivity (d = .21) and dyadic reciprocity (d = .21). At the end of the one year follow-up, in comparison with PE mothers, MIO mothers showed significantly greater sensitivity (d = .46), MIO children showed marginally greater involvement with mothers (d = .28) and MIO dyads showed significantly greater reciprocity (d = .45).
Child attachment status
As shown in Table 5, at the end of treatment, there were no significant group differences in the percentage of children whose attachment status either remained secure or became more secure at post-treatment (Cramer’s ф = .06).
Moderation effects of addiction severity
Maternal reflective functioning
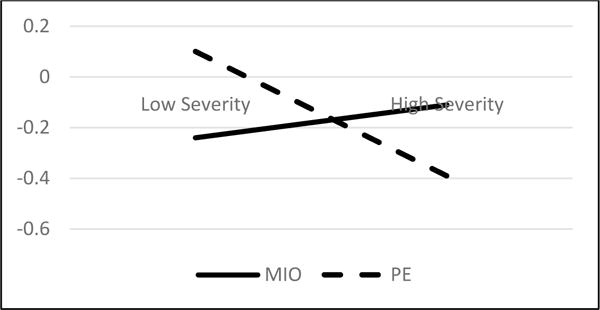
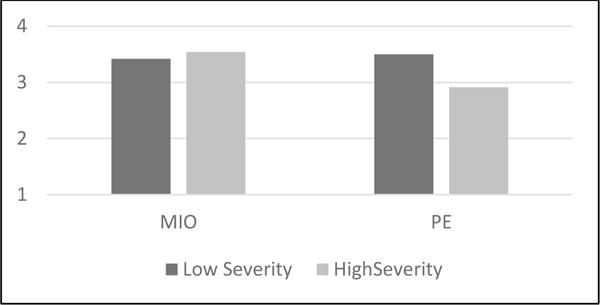
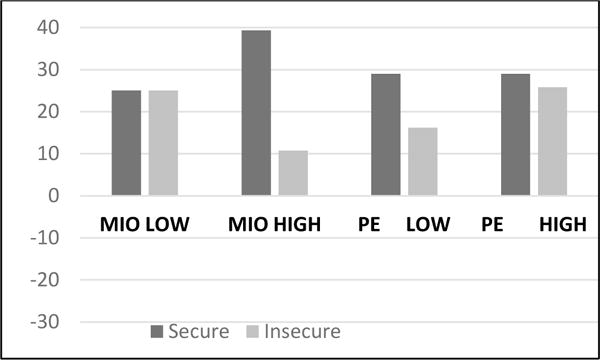
Addiction severity did not moderate associations between treatment and mean RF at post-treatment (t = 1.00, p = .32) or follow-up (t = .93, p = .11). The addiction severity × treatment interaction was marginally significant for Potential RF at post-treatment (t = 1.83, p = .07), f2 = .04) but not significant at follow-up (t = 1.70, p = .09). The interaction pattern for Potential RF at post-treatment (using actual change scores) is plotted in Figure 1. Further probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for MIO mothers (R2 = .16, β = .16, p = .02) but not for PE mothers (R2 = .01, β = −.03, p = .69) indicating that, for MIO mothers only, as addiction severity increased, Potential RF scores were higher, whereas for PE mothers, as addiction severity increased, Potential RF scores did not vary. Simple t-tests were also conducted within condition to probe for differences in Potential RF between low and high addiction severity levels (Figure 2). For PE mothers, the difference in Potential RF between low (M = 4.61, SD = .85) versus high (M = 4.42, SD = .90) addiction severity groups was not statistically significant (t = .66, p = .51, d = .15). For MIO mothers, however, the difference in Potential RF scores between low (M = 4.53, SD = .54) versus high (M = 5.19, SD = .54) addiction severity was significant with a large effect (t = 2.98, p = .006, d = .86). Together, these findings suggest that MIO served a protective function for mothers with more severe addiction in that they showed higher levels of Potential RF at the end of treatment than their counterparts with low addiction severity. PE did not confer the same advantage.
Figure 1.
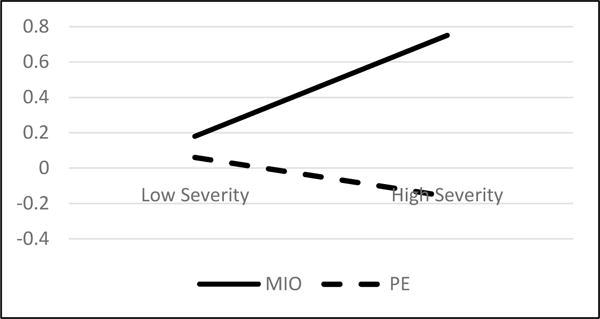
Addiction Severity × Treatment interaction for change in Potential RF at post-treatment
Figure 2.
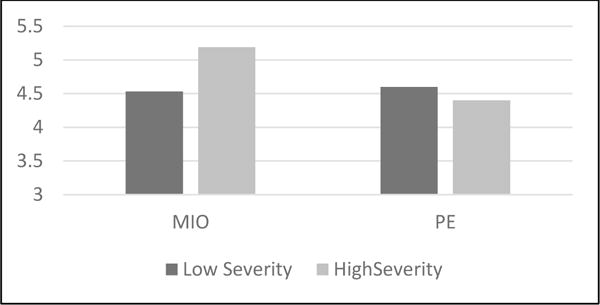
Potential RF scores at post-treatment for mothers with low and high addiction severity
Mother-child interactions
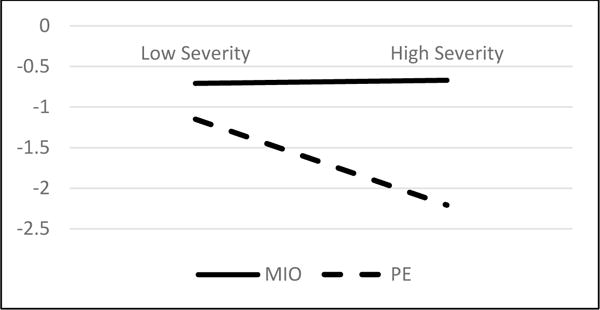
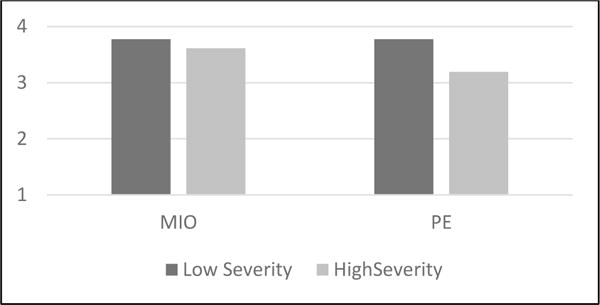
At post-treatment, addiction severity did not moderate associations between treatment and improvement in maternal sensitivity (t = 1.30, p = .20) or child involvement (t = 1.57, p = .12). However, the addiction severity × treatment interaction was marginally significant for dyadic reciprocity (t = 1.77, p = .08). The interaction pattern is plotted in Figure 3 (using actual change scores). Further probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for PE dyads (R2 = .09, β = −.14, p = .049) but not for MIO dyads (R2 = .01, β = .04, p = .59) indicating that, for PE dyads only, as addiction severity increased, dyadic reciprocity became worse, whereas for MIO dyads, dyadic reciprocity did not vary with addiction severity. Simple t-tests were also conducted within condition to probe for differences in dyadic reciprocity scores between low and high addiction severity levels (Figure 4). For PE dyads, the difference in dyadic reciprocity between low (M = 3.60, SD = 1.14) and high (M = 3.11, SD = 1.00) addiction severity groups was marginally significant and corresponded to a medium effect (t = 1.53, p = .13, d = .32). For MIO dyads, however, the difference in dyadic reciprocity between low (M = 3.51, SD = .85) and high (M = 3.53, SD = .80) addiction severity was non-significant (t = −.07, p = .94, d = .02). Together, these findings suggest that MIO was protective for dyads where mothers reported more severe addiction in that their reciprocity was not compromised in the same way that it was for their PE counterparts at the end of treatment.
Figure 3.
Dyadic reciprocity at post-treatment for mothers with low and high addiction severity
Figure 4.
Dyadic reciprocity scores at post-treatment for mothers with low and high addiction severity
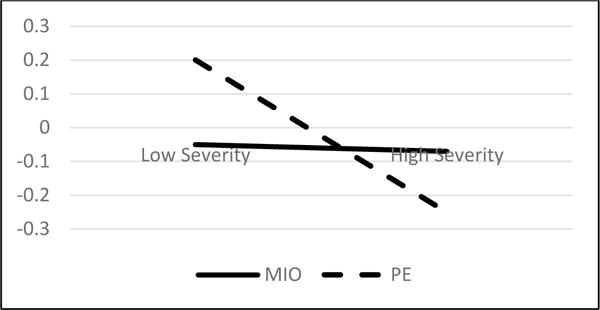
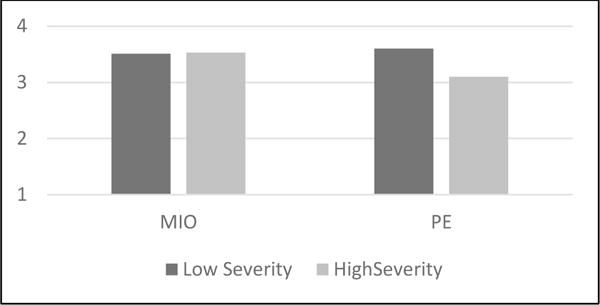
At the 3-month follow-up, addiction severity did not moderate associations between treatment and improvement in maternal sensitivity (t = 1.31, p = .20) or child involvement (t = 1.48, p = .14). However, the addiction severity × treatment interaction was marginally significant for dyadic reciprocity (t = 1.78, p = .08, f2 = .04). The interaction pattern is plotted in Figure 5 (using actual change scores). Further probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for PE dyads (R2 = .14, β = −.16, p = .01) but not for MIO dyads (R2 = .00, β = .01, p = .88) indicating that, for PE dyads only, as addiction severity increased, dyadic reciprocity became worse, whereas for MIO dyads, dyadic reciprocity did not vary with addiction severity. Simple t-tests were also conducted within condition to probe for differences in dyadic reciprocity scores between low and high addiction severity levels (Figure 6). For PE dyads, the difference in dyadic reciprocity between low (M = 3.50, SD = 1.21) and high (M = 2.91, SD = .84) addiction severity groups was marginally significant and corresponded to a medium effect (t = 1.90, p = .07, d = .40). For MIO dyads, however, the difference in dyadic reciprocity between low (M = 3.42, SD = .79) and high (M = 3.54, SD = .84) addiction severity was non-significant (t = −.45, p = .66, d = −.10). Together, these findings suggest that MIO was protective for dyads where mothers reported more severe addiction in that their reciprocity was not compromised in the same way that it was for their PE counterparts at the 3-month follow-up.
Figure 5.
Dyadic reciprocity at 3-month follow-up for mothers with low and high addiction severity
Figure 6.
Dyadic reciprocity scores at 3-month follow-up for mothers with low and high addiction severity
12-month follow-up
At the 12-month follow-up, addiction severity significantly moderated associations between treatment and magnitude of change in maternal sensitivity (t = 2.12, p = .05, f2 = .05), child involvement (t = 2.01, p =.048, f2 = .05), and dyadic reciprocity (t = 2.07, p = .042, f2 = .05). Because interaction patterns were similar across the three domains, only those for maternal sensitivity are plotted in Figure 7 (using actual change scores).
Figure 7.
Addiction Severity × Treatment interaction for change in maternal sensitivity at 12-month follow-up
Maternal sensitivity
Further probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for PE mothers (R2 = .15, β = −.18, p =.009) but not for MIO mothers (R2 = .00, β =.02, = .72) indicating that, for PE mothers only, as addiction severity increased, maternal sensitivity decreased, whereas, for MIO mothers, as addiction severity increased, maternal sensitivity did not vary. Simple t-tests were also conducted within condition to probe for differences in maternal sensitivity scores between low and high addiction severity levels (Figure 8). For PE mothers, the difference in maternal sensitivity between low (M = 3.61, SD = .71) and high (M = 3.19, SD = .70) addiction severity was marginally significant and corresponded to a medium effect (t = 1.97, p =.055, d = .42). For MIO mothers, the difference in maternal sensitivity scores between low (M = 3.77, SD = .45) versus high (M = 3.72, SD = .36) addiction severity was not significant (t = .42, p =.68). Together, these findings suggest that, addiction severity was (a) more likely to compromise rates of change in maternal sensitivity for PE mothers than for MIO mothers, and (b) marginally more likely to compromise maternal sensitivity levels for PE mothers than for MIO mothers at the 12-month follow-up. Together, these findings suggest that MIO was protective for mothers who reported more severe addiction in that their sensitivity was not compromised in the same way that it was for their PE counterparts at the 12-month follow-up.
Figure 8.
Maternal sensitivity scores at 12-week follow-up for mothers with low and high addiction severity
Child involvement
Further probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for PE mothers (R2 = .12, β = −.15, p = .02) but not for MIO mothers (R2 = .01, β =.04, p = .56) indicating that, for PE mothers only, as addiction severity increased, child involvement became lower, whereas, for MIO mothers, as addiction severity increased, change in child involvement did not vary. Simple t-tests were also conducted within condition to probe for differences in child involvement scores between low and high addiction severity levels. For PE mothers, the difference in child involvement between low (M = 3.49, SD =.63) and high (M = 3.32, SD = .37) addiction severity was not significant and corresponded to a small effect (t = 1.15, p = .26, d = .23). For MIO mothers, the difference in child involvement between low (M = 3.53, SD = .45) and high (M = 3.61, SD = .34) addiction severity was also non-significant (t = −.59, p =.56, d = −.14). Together, these findings suggest that MIO was protective for children of mothers who reported more severe addiction in that their involvement was not compromised in the same way that it was for their PE counterparts at the 12-month follow-up.
Dyadic reciprocity
Probing of individual slopes using simple regression analyses (Aiken & West, 1991) revealed a significant slope for PE mothers (R2 = .13, β = −.16, p = .015) but not for MIO mothers (R2 = .01, β =.03, p > .10) indicating that, for PE dyads only, as addiction severity increased, dyadic reciprocity became worse, whereas for MIO dyads, as addiction severity increased, dyadic reciprocity did not vary. Simple t-tests were also conducted within condition to probe for differences in child involvement scores between low and high addiction severity levels. For PE mothers, the difference in dyadic reciprocity between low (M = 3.51, SD = .99) and high (M = 3.09, SD = .67) addiction severity was marginally significant and corresponded to a medium effect (t = 1.69, p = .095, d = .35). For MIO mothers, the difference in dyadic reciprocity between low (M = 3.76, SD = .59) and high (M = 3.77, SD = .53) addiction severity was non-significant (t = −.06, p = .95, d = −.01). Together, these findings suggest that MIO was protective for dyads where mothers reported more severe addiction in that their dyadic was not compromised in the same way that it was for their PE counterparts at the 12-month follow-up.
Child attachment classification
Compared to the base model, the full tested model (with main effects and interaction terms entered in a single block) significantly improved explanatory power (X2 = 4.37, p = .037), increasing prediction accuracy from 61% to 68%. The Hosmer and Lemeshow test indicated good model fit (X2 =6.06, p = .53), and the Nagelkerke R2 of .15 suggested that the full model explained 15% of the variance in attachment status change. As shown in Table 7, the odds ratio for the interaction effect indicated that, for each point of increase in MIO mothers’ addiction severity, the odds of the target child’s attachment status either remaining or becoming more secure doubled. Chi-square analyses were then conducted to probe for differences in percentage of children whose attachment status remained or became secure between low versus high addiction severity levels within condition (Figure 9). Within PE, 64.3% of children whose mothers’ addiction severity was low and 52.9% of children whose mothers’ addiction severity was high either remained secure or moved toward greater security at the end of treatment and this difference was non-significant (X2 = .41, Fisher’s Exact Test p = .72, Cramer’s ф = .11) and corresponded to a small effect. Within MIO, 50% of children whose mothers’ addiction severity was low and 78.6% of children whose mothers’ addiction severity was high either remained secure or moved toward greater security at the end of treatment. Although this difference was non-significant (X2 = 2.49, Fisher’s Exact Test p = .24, Cramer’s ф = .30), the corresponding effect size of is considered medium. Together, these findings suggest that MIO served a protective function for children of mothers with more severe addiction in that they showed more maintenance of or improvement toward a secure attachment classification. PE did not confer this same advantage for children of mothers with more severe addiction.
Table 7.
Results of binary logistic regression analysis testing moderator effects of addiction severity on change in attachment classification from pre- to post-treatment
| Variable | B | Wald | Exp (B) |
|---|---|---|---|
| Condition (MIO = 1, PE = 0) | .24 | .17 | 1.27 |
| Addiction Severity | −.06 | .11 | .94 |
| Condition × Addiction Severity | .62 | 3.90* | 1.87 |
p < .05, two-tailed
Figure 9.
Percentage of children whose attachment status remained or approached secure versus insecure by condition and addiction severity (high versus low)
Discussion
In this paper, we reported results from the second randomized clinical trial testing the efficacy of Mothering from the Inside Out, a 12 session manualized individual mentalization-based therapy for mothers enrolled in substance abuse treatment. MIO was compared with Parent Education (PE), a manualized individual psychoeducational intervention that was comparable to MIO in terms of treatment dose, individualized approach, and the chance to form a working alliance but provided psychoeducation about developmental guidance and parenting strategies. The aims of the study were to (1) determine whether a mentalization-based approach would lead to better parental reflective functioning and representation coherence, reduction in psychiatric distress and relapse to substance use, better parent-child interactions and more secure child attachment and (3) examine the potential protective role of MIO in relation to the impact of addiction severity on parenting and children’s well-being. The implications of our findings for clinical work, and prevention and attachment science are discussed, in turn, below.
Implications for Clinical Interventions
Maternal reflective functioning and representations
Mothers in MIO showed significantly greater potential for RF by the end of the 12-session treatment and significantly greater overall RF by the end of the 3-month follow-up. Importantly, at post-treatment and 3-month follow-up, MIO mothers’ potential RF capacity approached the benchmark score of 5, indicating an adequate capacity to recognize and make sense of mental (especially affective) experiences. These findings are consistent with those reported in the first randomized trial (Suchman et al., 2011). Likewise, at the end of treatment and the 3-month follow-up, mental representations of the child and the caregiving relationship were significantly more coherent in mothers who received MIO. In other words, MIO mothers were more likely to express greater openness to their children’s unique personalities and emotional needs and to have more realistic and balanced views of their children’s capacities and personality characteristics. At both time points, MIO mothers’ scores were approaching the benchmark of 3, which is considered average. Together, these findings indicate the strong potential of relatively brief-but-intensive mentalization-based interventions for addressing the psychological deficits (e.g., impulsivity, emotional reactivity, low distress tolerance) associated with chronic substance use and maladaptive parenting. The findings also underscore the importance of providing mentalization-based interventions for mothers concomitantly with their addiction treatment so that emotional regulation challenges inherent in the demands of being a parent in recovery can be targeted as they arise. Moreover, it seems reasonable to expect that, as mothers’ mentalizing capacities improve, the transmission of this capacity to their young children is more likely.
MIO also proved to be protective for mothers with greater addiction severity at post-treatment. In fact, we were surprised that these mothers showed higher levels as well as greater improvement in Potential RF than their counterparts with low addiction severity. We expected that mothers with greater addiction severity would have more to gain from an intervention focused on mentalizing but were puzzled as to why their Potential RF scores were higher (i.e. RF score of 5.19 versus 4.53). It may be that MIO is best suited to mothers with the most chronic and severe substance use disorders whereas a combined focus on mentalization and developmental guidance might work better for mothers with less severe addiction problems.
Maternal psychiatric symptoms and substance use
Contrary to expectations, PE mothers showed a faster rate of decline in psychiatric distress than MIO mothers, although, by the end of the 3-month follow-up, both groups had moved out of the clinically-significant and into the normal range. In retrospect, it may be that asking mothers to pay closer attention to stressful situations and concomitant affective experiences results in slower alleviation of psychiatric distress. In the first trial (see Suchman et al., 2012), improvement in maternal depression was found to have a unique impact on caregiving behavior (even after improvement in maternal RF was taken into account). It will be important to examine further whether rate of decline in psychiatric distress might influence response to MIO.
A large majority of mothers in both conditions (at least 90%) were not using any substances during the study and this is likely due to their ongoing enrollment in outpatient addiction treatment. However, among the 10% of MIO mothers who acknowledged using heroin at the beginning of the study, there was a notable decline in relapse rate, whereas PE mothers’ heroin relapse rate increased from 2% to 8% by the end of the 3-month follow up. In light of recent increases in heroin use among adolescents and young adults in the United States, this finding has important implications, not only for parenting interventions but also for addiction treatment more broadly. Further examination of mechanisms of action are needed to determine whether improvement in mentalizing capacity leads to a reduction in relapse. If this turns out to be the case, introducing mentalization-based approaches to addiction treatment more broadly may help to improve relapse rates in the general treatment population. Current research (e.g., Rutherford, Potenza, & Mayes, 2013) examining caregiving-related triggers, cravings and relapse may also help identify the mechanisms by which mentalization-based therapy leads to better abstinence rates. Mechanisms notwithstanding, the benefits MIO mothers experienced in heroin abstinence further underscores the importance of providing mentalization-based parenting interventions and addiction treatment concomitantly. It is also critically important to recognize the potential risk in providing parenting programs that fail to address the unique emotional stressors associated with chronic addiction and parenting as evidenced by the small increase in heroin relapse rates despite PE’s equivalence to MIO in all aspects (e.g., duration, intensity, supervision quality, and chance to form a secure alliance,) except for the mentalizing focus.
Mother-child interactions
Small improvements were observed in MIO children’s involvement at post-treatment and in MIO mothers’ sensitivity and dyadic reciprocity at the 3-month-follow up. However, the greatest differences for MIO did not emerge until the 12-month follow-up when MIO mothers and children showed significantly better scores on all three relational indices (maternal sensitivity, child involvement and dyadic reciprocity). It may take more time than we originally expected for changes in reflective functioning and maternal representations to reach the behavioral level for mothers and children. Future examination of the mediating effects of improved RF and representations in response to MIO will help clarify its mechanisms of change. It may also be important to consider mentalization-based therapy as the first in a series of steps that progress toward developmental and behavioral guidance as mothers become open and ready for constructive suggestions. Further research on alternative intervention progression may help clarify whether or not behavioral change can be accelerated. Likewise, engaging mothers in mentalization-based interventions earlier in their addiction recovery might also help prevent entrenchment in maladaptive parenting habits.
We also found strong evidence that MIO served a protective function for mothers with more severe addictions and their children against poorer interaction outcomes. For dyadic reciprocity at the 3-month follow up and for all three mother-child interaction indices (maternal sensitivity, child involvement and dyadic reciprocity) at the 12-month follow up, we generally found a similar pattern showing that, when mothers with more severe addictions were assigned to PE, the chance for better quality relationships was notably diminished. Again, we believe this finding indicates the potential risk, particularly for mothers with chronic substance abuse histories, in providing parenting programs that fail to address the unique emotional stressors associated with chronic addiction and parenting.
Child attachment status
At the end of treatment, 64.3% of MIO children and 58.1% of PE children either retained their secure status or moved toward a more secure status and 35.7% of MIO children and 41.9% of PE children retained their insecure status or moved toward a less secure status. Although group differences were not significant, these data may signal that, with longer exposure to MIO, group differences might be more pronounced. It is also possible that attachment status was measured prematurely. Like the results from the Curiosity Box, attachment status might not change until changes in maternal RF and representation have time to consolidate. In future work, we are planning to assess attachment status at follow-up visits as well.
Children of mothers with greater addiction severity were twice as likely to remain secure or become more secure in their attachment status if their mothers were assigned to MIO. Again, these findings suggest that children cared for by mothers with histories of severe addiction are more likely to benefit in terms of attachment security when their mothers receive a mentalization-based parenting intervention.
Implications for Intervention and Attachment Research
Findings from this and our previous randomized trial (Suchman et al., 2010, 2011, 2012) highlight the importance of carefully considering mechanisms of change when developing and evaluating interventions for parent populations at the far end of the psychosocial risk spectrum (e.g., parents with chronic addiction and psychiatric disorders). Interventions that directly target change in parenting behavior through psycho-educational instruction and hands-on parent coaching have generally worked well to prevent escalation of conduct problems in children whose parents are experiencing moderate environmental stressors and psychosocial challenges (Sanders, Markie-Dadds, Tully, & Bor, 2000; Webster-Stratton & Reid, 2010). However, to date, none of the evidence-based behavior-targeting interventions have demonstrated promise for parents at the extreme end of the risk spectrum who often leave these interventions prematurely and accumulate experiences of frustration and failure as they continue to draw the attention of child welfare agencies. Our research suggests that, for parents who have more profound difficulties tolerating stress, regulating emotions, and managing impulses, targeting these psychological deficits in a brief-yet-intensive individualized therapy that focuses on ameliorating these issues (i.e., strengthening the mentalizing capacity) may be a more effective route to improving parent-child relationships and preventing the intergenerational transmission of addiction psychopathology. Although it is too early to draw conclusions (e.g., tests of mechanisms need to be replicated), our evidence suggests that targeting a parent’s psychosocial deficits within the context of parenting may help free the parent psychologically and emotionally to engage with her child in a more mutually-rewarding and enjoyable manner that ultimately benefits the child’s experience of emotional security and self-agency.
The concept of mentalization and its observable manifestation in reflective functioning, appears to be a critical mechanism in the transmission of secure attachment across generations that requires further study in high-risk populations. Unlike other complex psychodynamically-grounded constructs (e.g., ego development), mentalization has been operationalized for empirical research (Slade et al., 2003; Luyten, Mayes, Sadler, Fonagy, Nicholls, Crowley, et al., 2009) and has strong theoretical grounding in and empirical association with adult and child attachment (see Katznelson, 2014 for a review). As a measurable human psychological capacity that is increasingly considered critical to interpersonal functioning (see, for example, Gabbard, 2010), and central in many forms of psychopathology, its relevance to intervention and attachment research will likely continue to grow. Ironically, it is a capacity that has been studied more extensively in children (i.e., theory of mind research) than in adults or parents. Our findings along with the others’ (e.g., Pajulo, Pyykkonen, Kalland, Sinkkonen, Helenius, et al., 2012; Sadler, Slade, Close, Webb, Simpson, et al., 2013) point to the critical role of parental mentalizing and reflective functioning starting during (and even before) pregnancy, as parents’ representations of their unborn infants become activated and begin to inform many aspects of their decisions and behaviors.
Conclusions and Future Directions
Substance addiction has a profound impact on adults who find themselves in the parenting role caring for young children and even more profoundly on the young children themselves. Intervention with this vulnerable and often disenfranchised and stigmatized population is very challenging and requires theoretically-grounded approaches that take the unique psychosocial consequences of addiction into account. Here we reported on one such approach that is grounded in attachment and mentalization theory and builds on neuroscientific evidence showing that chronic substance use coopts the same neural circuitry recruited during parenting activities and likely makes the parenting experience more stressful and less enjoyable. The findings reported here support the importance of addressing a mother’s subjective experience of distress in the parenting role while she is in recovery and before addressing her parenting behaviors with her young children. The results bring to mind the oxygen mask metaphor where airline staff instruct parents to place their oxygen mask first on themselves before fixing their child’s mask. Children’s unmet needs cannot be addressed without first meeting the needs of their primary caregivers who are, most typically, their mothers.
Mentalization-based therapy for mothers has now shown promise for improving maternal reflective functioning and caregiving quality in two randomized clinical trials. The next step in our research program (currently underway) involves training addiction counselors to deliver MIO and PE with fidelity and testing whether MIO’s efficacy holds when delivered by addiction counselors in a community-based setting. We are hopeful that training addiction counselors in mentalization-based therapy, child development, and effective parenting strategies will help stem the gap between child guidance and addiction services that parents in recover often fall through. So far, our experience shows us that addiction counselors welcome the additional training and are very well poised to provide this additional support to parents in recovery. Forthcoming results of our Stage III community-based randomized clinical trial will provide the needed empirical evidence that will either support or refute this hypothesis.
Acknowledgments
The investigators would like to acknowledge the National Institute on Drug Abuse for its ongoing funding for this research including R01 DA17294 (Suchman, PI) and K02 DA023504 (Suchman, PI). We would also like to thank our Research Assistants, Laura Ciarleglio, Laura Donald, Lourdes de las Heras Kuhn, Emily Pariseau, Hannah Rasmussen, Lauren and Mayra Vega for their many important contributions to this work. We are grateful for the input we have received from clinical consultants Susan Bers and Lauren Dennehy and guidance from the late Bruce Rounsaville and Patty Rosenberger. Finally, we wish to thank the patients and clinicians at the APT Foundation without whose participation and support this work would not have been possible.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum; 1978. [Google Scholar]
- Allen JG, Fonagy P, Bateman A. Mentalizing in clinical practice. 1st. Arlington, VA: American Psychiatric Publishing; 2008. [Google Scholar]
- Bateman AW, Fonagy P. Handbook of mentalizing in mental health practice. 1st. Arlington, VA: American Psychiatric Publishing; 2012. [Google Scholar]
- Bayley N. Bayley Scales of Infant and Toddler Development Screening Test. 3rd. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- Buckley C. In the city, highly productive drug mills. The New York Times. 2009 Sep 25; Retrieved from http://www.nytimes.com.
- Burns KA, Chethik L, Burns WJ, Clark R. The early relationship of drug abusing mothers and their infants: An assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Marvin RS, with the MacArthur Attachment Working Group . Attachment organization in preschool children: Coding guidelines. 4th. University of Virginia; 1992. Unpublished manuscript. [Google Scholar]
- Choi S, Ryan J. Co-occurring problems for substance abusing mothers in child welfare: Matching services to improve family reunification. Children and Youth Services Review. 2007;29:1395–1410. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum Associates; 1983. [Google Scholar]
- Dalton R, Dennehy L. Parent Education Training Manual. New Haven, CT: Yale University School of Medicine; 2015. [Google Scholar]
- Department of Health and Human Services. Blending perspectives and building common ground: A report to congress on substance abuse and child protection. Washington, DC: DHHS; Apr, 1999. Derogatis, 1993. [Google Scholar]
- DeCoste C, Dalton R, de las Heras Kuhn L, Dennehy L. Parent Education: An individualized psycho-educational program for mothers of children under 5 years of age. New Haven, CT: Yale University School of Medicine; 2010. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. 3rd. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Fals-Stewart W, O-Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Feldman R. Coding interactive behavior manual. Ramat Gan, Tel Aviv, Isreal: Bar-Ilan University; 1998. [Google Scholar]
- Fonagy P, Steele M, Steele H, Leigh T, Kennedy R, Mattoon G, Target M. Attachment, the reflective self, and borderline states: The predictive specificity of the Adult Attachment Interview and pathological emotional development. In: Goldberg S, Muir R, Kerr J, editors. Attachment theory: Social, developmental, and clinical perspectives. Hillsdale, NJ: Analytic Press; 1995. pp. 233–278. [Google Scholar]
- Gabbard GO. Long-term psychodynamic psychotherapy: A basic text. 2nd. Arlington, VA: American Psychiatric Publishing; 2010. [Google Scholar]
- Gottman JM, Rushe RH. The analysis of change: issues, fallacies, and new ideas. Journal of Consulting and Clinical Psychology. 1993;61:907–910. doi: 10.1037//0022-006x.61.6.907. [DOI] [PubMed] [Google Scholar]
- Grant T, Huggins J, Graham JC, Ernst C, Whitney N, Wilson D. Maternal substance abuse and disrupted parenting: Distinguishing mothers who keep their children from those who do not. Children and Youth Services Review. 2011;33:2176–2185. [Google Scholar]
- Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatric clinics of North America. 2010;33:339–355. doi: 10.1016/j.psc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hans LL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development & Psychopathology. 1999;11:957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Harrison PL, Kaufman AS, Kaufman NL, Bruininks RH, Rynders J, Ilmer S, Sparrow SS, Cicchetti DV. AGS Early Screening Profiles. Journal of Psychoeducational Assessment. 1990;13:101–104. [Google Scholar]
- Hoffman KT, Marvin RS, Cooper G, Powell B. Changing toddlers’ and preschoolers’ attachment classifications: the Circle of Security Intervention. Journal of Consulting and Clinical Psychology. 2006;74:1017–1026. doi: 10.1037/0022-006X.74.6.1017. [DOI] [PubMed] [Google Scholar]
- Jones RG. Heroin’s hold on the young. The New York Times. 2008 Jan 13; Retrieved from http://www.nytimes.com.
- Kaufman AS, Kaufman NL. Kaufman Grief Intelligence Test. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- Katznelson H. Reflective functioning: A review. Clinical Psychology Review. 2014;34:107–117. doi: 10.1016/j.cpr.2013.12.003. [DOI] [PubMed] [Google Scholar]
- Kerwin ME. Collaboration between child welfare and substance-abuse fields: Combined treatment programs for mothers. Journal of Pediatric Psychology. 2005;30:581–597. doi: 10.1093/jpepsy/jsi045. [DOI] [PubMed] [Google Scholar]
- Luyten P, Mayes LC, Sadler L, Fonagy P, Nicholls S, Crowley M, Vesper A, Mobley A, Stewart T, Close N, Slade A. The Parental Reflective Functioning Questionnaire-1 (PRFQ-1) University of Leuven; Leuven, Belgium: 2009. Unpublished manual. [Google Scholar]
- Mayes L, Carter A, Stubbe D. Infant differences in exploratory behavior in the second year of life. Infant Behavior and Development. 1993;16:269–284. [Google Scholar]
- Miller MD. Kaufman Brief Intelligence Test. In: Conoley JC, Impara JC, editors. The twelfth mental measurements yearbook. Lincoln, NE: Buros Institute of Mental Measurements; 1995. pp. 533–534. [Google Scholar]
- Pajulo M, Pyykkönen N, Kalland M, Sinkkonen J, Helenius H, Punamäki R, Suchman N. Substance abusing mothers in residential treatment with their babies: importance of focusing in pre-and postnatal maternal reflective functioning. Infant Mental Health Journal. 2012;33:70–81. doi: 10.1002/imhj.20342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosa DR. Myths and methods: “Myths about longitudinal research,” plus supplemental questions. In: Gottman JM, editor. The analysis of change. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1995. pp. 3–65. [Google Scholar]
- Rutherford HJV, Potenza MN, Mayes LC. The neurobiology of addiction and attachment. In: Suchman NE, Pajulo M, Mayes L, editors. Parenting and substance abuse: Developmental approaches to intervention. New York, NY, US: Oxford University Press; 2013. pp. 3–23. [Google Scholar]
- Rutherford HJV, Williams SK, Moy S, Mayes LC, Johns JM. Disruption of maternal parenting circuitry by addictive process: rewiring of reward and stress symptoms. Frontiers in Psychiatry. 2011;2:37. doi: 10.3389/fpsyt.2011.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadler LS, Slade A, Close N, Webb DL, Simpson T, Fennie K, Mayes LC. Minding the Baby: Enhancing reflectiveness to improve early health and relationship outcomes in an interdisciplinary home visiting program. Infant Mental Health Journal. 2013;34:391–405. doi: 10.1002/imhj.21406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders MR. Triple P-Positive Parenting Program: Towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clinical Child and Family Psychology Review. 1999;13:71–90. doi: 10.1023/a:1021843613840. [DOI] [PubMed] [Google Scholar]
- Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology. 2000;68:624–640. [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Seelye KQ. Obituaries shed euphemisms to chronicle toll of heroin. The New York Times. 2015 Jul 11; Retrieved from http://www.nytimes.com.
- Slade A. Parental reflective functioning: An introduction. Attachment and Human Development. 2005;7:269–281. doi: 10.1080/14616730500245906. [DOI] [PubMed] [Google Scholar]
- Slade A, Aber JL, Berger B, Bresgi I, Kaplan M. The Parent Development Interview – Revised. City University of New York; 2003. Unpublished manuscript. [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Solomon J, George C. The measurement of attachment security in infancy and childhood. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 2nd. New York: The Guilford Press; 2008. pp. 383–416. [Google Scholar]
- Strathearn L. Maternal neglect: Oxytocin, dopamine and the neurobiology of attachment. Journal of neuroendocrinology. 2011;23:1054–1065. doi: 10.1111/j.1365-2826.2011.02228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathearn L, Fonagy P, Amico J, Montague PR. Neuropsycopharmacology. 2009;34:2655–2666. doi: 10.1038/npp.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Bers SA. Mothering from the Inside Out: A mentalization-based intervention for mothers in substance use treatment. New Haven, CT: Yale University School of Medicine; 2015. [Google Scholar]
- Suchman N, DeCoste C, McMahon T, Rounsaville B, Mayes L. The Mothers and Toddlers Program, an attachment-based parenting intervention for substance-using women: Results at 6-week follow-up in a randomized clinical pilot. Infant Mental Health Journal. 2011;32:427–449. doi: 10.1002/imhj.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman N, DeCoste C, Ordway M, Bers S. Mothering from the Inside Out: A mentalization-based individual therapy for mothers with substance use disorders. In: Suchman N, Pajulo M, Mayes L, editors. Parenting and substance addiction: Developmental approaches to intervention. NY: Oxford University Press; 2013. pp. 407–433. [Google Scholar]
- Suchman NE, DeCoste C, Rosenberger P, McMahon TJ. Attachment-based intervention for substance using mothers: A preliminary test of the proposed mechanisms of change. Infant Mental Health Journal. 2012;33:360–371. doi: 10.1002/imhj.21311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Pajulo M, DeCoste C, Mayes LC. Parenting interventions for drug dependent mothers and their young children: The case for an attachment-based approach. Family Relations. 2006;55:211–226. doi: 10.1111/j.1741-3729.2006.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Rosenberger P, DeCoste C. The Mothers and Toddlers Program: Therapist Adherence and Coding Procedures Manual. New Haven, CT: Yale University School of Medicine; 2006. [Google Scholar]
- Suchman NE, Rosenberger P, DeCoste C. The Revised MIO/PE Therapist Adherence Rating Scale and Coding Procedures Manual. New Haven, CT: Yale University School of Medicine; 2010. [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: A randomized preventive trial. Journal of Consulting and Clinical Psychology. 2006;74:1006–1016. doi: 10.1037/0022-006X.74.6.1006. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ. The Incredible Years parents, teachers and children training series: A multifaceted treatment approach for young children with conduct problems. In: Weisz J, Kazdin A, editors. Evidence-based psychotherapies for children and adolescents. 2nd. New York: Guilford Publications; 2010. pp. 194–210. [Google Scholar]
- Young JW. Kaufman Brief Intelligence Test. In: Conoley JC, Impara JC, editors. The Twelfth mental measurement yearbook. Lincoln, NE: Buros Institute of Mental Measurements; 1995. pp. 534–535. [Google Scholar]
- Zeanah CH, Benoit D. Clinical applications of a parent perception interview in infant mental health. Infant Psychiatry. 1993;3:539–554. [Google Scholar]


