Abstract
Introduction
The aim of this study was to evaluate the acquisition of basic ureteroscopic skills with and without Roboflex Avicenna by subjects with no prior surgical training.
Material and methods
Ten medical students were divided in two groups: Group 1 was trained with Roboflex Avicenna and Group 2 with flexible ureteroscope alone, using the K-box® simulator model. Participants were scored on their ability to perform or not two exercises, recording the time. In addition, the participants were evaluated on the quality of their performance for the following parameters: respect of the surrounding environment, flow of the operation, orientation, vision centering and stability.
Results
The first exercise was completed only by three and four out of five of students in Group 1 and Group 2, respectively. Stability with the scope was significantly more accurate in the first group compared with the second (P = 0.02). There were no differences in timing, flow or orientation between groups. Although not significant, a tendency of respecting the surrounding tissue and maintaining centered vision was perceived more in the first group. As for the second exercise, there were no differences between groups in regard of orientation, flow, respecting the surrounding tissue, stability or the ability of maintaining centered vision. Although not significant, the second group had a tendency of performing the exercise faster.
Conclusions
According to these preliminary results, the acquisition of basic ureteroscopic skills with and without robotic fURS in the K-box® simulator, by subjects with no prior surgical training, is similar.
Keywords: education, learning curve, flexible ureteroscopy, robotic flexible ureteroscopy
INTRODUCTION
In the last few years, improvements in the endourological armamentarium together with the downsizing of flexible ureteroscopes, the advent of digital technology, and the increasing number of requests for minimally invasive procedures have made the use of flexible ureteroscopy (fURS) for renal calculi increasingly attractive, even for stones larger than 2 cm in diameter [1] including the most difficult clinical scenarios [2].
Recently, Roboflex Avicenna, a new robotic system, has been introduced for assisting fURS, showing good outcomes in terms of stone free rate (SFR) and safety, with significant improvements in ergonomics [3]. To date, no information exists about the learning curve of Roboflex Avicenna compared to fURS without the robotic device. The use of flexible ureterorenoscopes demands specific skills acquisition during a training period. It has been demonstrated that surgeons can become familiar with a specific surgical procedure and improve their skills through simulators by repetitive training in a stress-free environment [4].
Recently, it has been showed that a new simulator for ureteroscopy, the Kidney-box (K-box®, Porgès-Coloplast), represents a valid training model for initiate medical students to flexible ureteroscopy [5].
The aim of this study was to evaluate the acquisition of basic ureteroscopy skills with and without Roboflex Avicenna by subjects with no prior surgical training, using the K-box® simulator.
MATERIAL AND METHODS
Ten 5th-year medical students were voluntarily recruited from Pierre and Marie Curie University of Paris. Informed consent was obtained from all the students to participate in the study.
Subjects were randomized in block fashion to include 5 medical students in each group; Group 1 was trained with Avicenna Roboflex and Group 2 with a standard flexible ureteroscope. The flexible ureteroscope used in both groups was URF-V2 (Olympus) and the simulator for training the students was the K-box® (Porgès-Coloplast) [6].
All the exercises were assessed with the boxes closed (non-transparent simulators).
Under supervision of a trained endourological instructor, all students received didactic teaching for 10 lessons in 10 days, at 10 minutes for each session. The instructor was responsible for correcting students’ mistakes, answering and explaining the participants’ questions and doubts.
All participants were evaluated by an experienced surgeon (OT), blinded to the randomization table, through two different exercises in the K-box® (Figures 1, 2), both aimed to discover the small spheres present in the simulator.
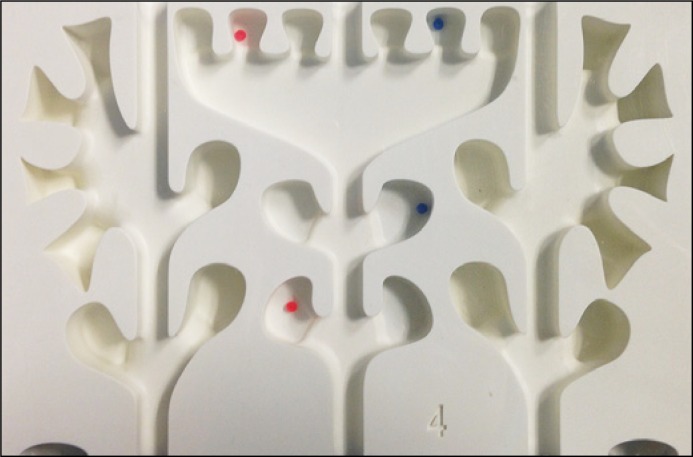
Figure 1.
Exercise 1: spheres to be found by fURS in the K-box®.
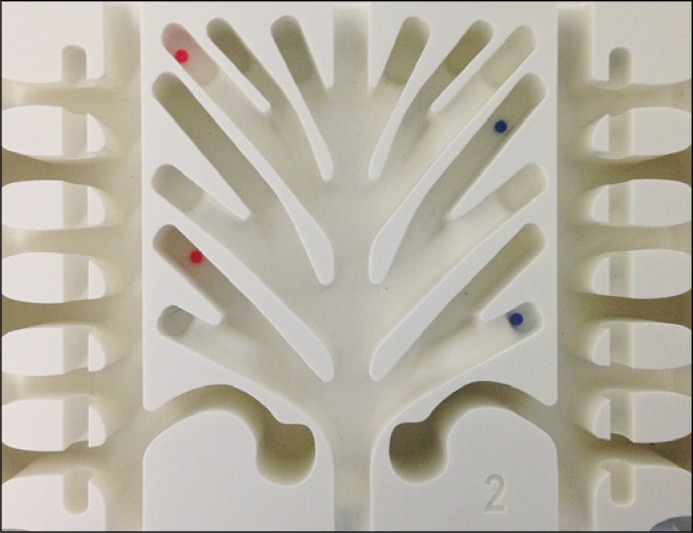
Figure 2.
Exercise 2: spheres to be found by fURS in the K-box®.
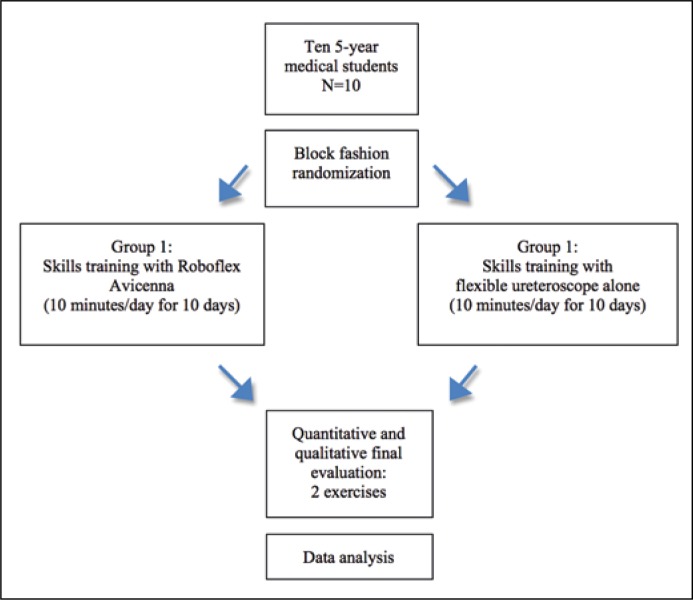
While the exercise was done with real time endoscopic vision transmission, the evaluation was performed simultaneously in a separate room in order not to be influenced by the device used. The study flow chart is shown in Figure 3.
Figure 3.
Study’s flow diagram.
Using an objective structured assessment of technical skills (OSATS) according to previous evaluations in a simulator model performed by Hu et al. [7] and Chou et al. [8] all participants were scored on their global ability to perform, or not, the exercises recording their times analyzing the knowledge of the procedure, the instrument handling and the trainees’ competence [9].
In addition, the participants were evaluated on the quality of their performance, using a 5-point Likert rating scale from 1 (poor) to 5 (excellent) exclusively made for endoscopic evaluations. The scale contains the following parameters: respect of the surrounding environment, flow of the operation, orientation, centered vision and stability (Table 1). The qualitative assessment had a potential maximum score of 35 points. Time to complete the exercise was measured; the students had a 2 minute timeframe to perform each exercise.
Table 1.
The rating scale used to assess the quality of students’ performance
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Respect for surrounding environment | Scope frequently pushed into the artificial channel wall | Scope occasionally pushed into the artificial channel wall | Few episodes of inadvertent contact with the artificial channel | One episode of inadvertent contact with the artificial channel | No contact with the artificial channel wall |
| Flow of operation | Frequently stopped and seemed unsure of next move | Occasionally stopped and seemed unsure of next move | Demonstrated some forward planning with reasonable progression | Demonstrated forward planning with only one unsure episode | Well planned operation with effortless flow of movement |
| Orientation | Frequently loss of the orientation into the artificial channel | Occasionally loss of the orientation into the artificial channel | Few episodes of loss of the orientation | One episode of loss of the orientation | Excellent orientation in the artificial channel |
| Centered vision | Frequently the vision is not centered | Occasionally the vision is not centered | Few episodes of not centered vision | One episode of not centered vision | Excellent centered vision |
| Stability | Poor | Fair | Good | Very good | Excellent |
Statistical analysis was performed with SPSS version 20.0 (Statistical Package for the Social Sciences, SPSS Inc, Chicago, IL) for Mac OS X. Data extracted from our database was automatically converted into SPSS.
Normality testing (D’Agostino and Pearson test) was performed to determine whether data were sampled from a Gaussian distribution. Chi-square and Fisher’s exact test were used to analyze proportions, as appropriate. Student’s t test and the Mann-Whitney U-test were performed to compare continuous parametric and non-parametric variables, respectively.
All the tests were 2-sided and statistically significant difference was considered for p <0.05.
RESULTS
All ten students completed the training. According to the OSATS evaluation, the global quality of performance was correct in all students. The first exercise was completed only by three out of five of students in Group 1 (robotic training) and by four out of five students in Group 2 (fURS alone). Stability with the scope was significantly more accurate in the first group compared with the second, 4.6 +/- 0.5 points vs. 3.0 +/- 0.7 (P = 0.02) respectively. There were no differences in timing, flow or orientation between groups. Although not significant, a tendency of respecting the surrounding tissue and maintaining centered vision was observed more in the first group.
As for the second exercise, there were no differences between groups in regard of orientation, flow, respecting the surrounding tissue, stability or the ability of maintaining centered vision. Although not significant, the second group had a tendency of performing the exercise faster. Results are summarized in Table 2.
Table 2.
Results
| Exercise 1 | Group 1 | Group 2 | P value |
|---|---|---|---|
| Completed (N) | 3 (60.0%) | 4 (80.0%) | >0.99 |
| Time (min) | 1.9 ±0.3 | 1.4 ±1.0 | >0.99 |
| Respect of surrounding tissue | 4.4 ±0.5 | 3.2 ±0.8 | 0.08 |
| Flow | 4.6 ±0.5 | 3.6 ±0.9 | 0.14 |
| Orientation | 4.4 ±0.5 | 3.8 ±0.8 | 0.39 |
| Vision centered | 4.4 ±0.5 | 3.4 ±0.5 | 0.08 |
| Stability | 4.6 ±0.5 | 3.0 ±0.7 | 0.02 |
| Exercise 2 | |||
| Completed (N) | 5 (100%) | 5 (100%) | |
| Time (min) | 1.6 ±0.6 | 0.7 ±0.4 | 0.008 |
| Respect of surrounding tissue | 3.4 ±0.5 | 3.8 ±0.4 | 0.52 |
| Flow | 4.0 ±0.7 | 4.6 ±0.5 | 0.36 |
| Orientation | 4.0 ±0.7 | 4.4 ±0.5 | 0.64 |
| Vision centered | 3.6 ±0.9 | 3.6 ±0.5 | >0.99 |
| Stability | 4.0 ±0.7 | 3.4 ±0.5 | 0.36 |
DISCUSSIONS
Nowadays, the technological advances combined with healthcare and ethic law standards have made urologists explore the use of surgical simulators to overtake the first steps in the learning curve of certain procedures [10, 11].
It is known that untrained medical students, residents and skilled surgeons (even tutors) can become familiar with a specific surgical procedure and efficiently improve their skills through simulation technology by repetitive training in a stress-free environment.
Endourology simulators such as virtual reality, cadaveric, artificial models and animal models [11, 12] are being widely and effectively used to master the learning curve of an evolving technology such as fURS.
The learning curve for fURS is necessary to achieve good proficiency.
It has been published and estimated that a surgeon must perform at least 50 fURS to achieve surgical competence [13]. Simulators can actively improve surgeons’ skills and may possibly accelerate this path. When comparing simulation vs non-simulation fURS training, Hu et al. showed in a cohort of 36 medical students, that those participants with previous training experience in transparent and non-transparent models performed objectively better than those without it. The analysis also showed an even better performance in the group with transparent simulators, with all differences being statistically significant [7]. A comparison between virtual reality and animal models reported that after a two month training period, all of their 36 participants evaluated by an objective qualitative scale, acquired adequate skills to perform a basic fURS independently of the simulator used [7].
In this study we used the K-box® simulator (Porgès-Coloplast) which is an artificial model made of four different boxes that reproduces all anatomic variability of the upper urinary tract. This is a non-transparent model that permits the trainee to handle the actual ureteroscope while looking at a monitor with real time vision transmission.
The K-box® has proven to be a valid simulator to learn fURS in a prospectively randomized study that compared a non-trained control group with trainees that underwent a ten day practice experience (five days to learn the flexible ureteroscope handling and five more days to practice how to catch and release stones with a nitinol basket) [5]. The comparison between groups made by an experienced endourologist with the objective endoscopic skill scale used in this paper (Table 1), revealed that all scores obtained by trained students were significantly higher compared to non-trained students. Also, trained students performed the exercises significantly faster than the control group.
As for the recent introduction of robotic fURS [3], there is no evidence in the literature about the learning curve of this technique. Also there is no evidence about simulation of neither the newly robotic fURS nor comparisons between skills gained comparing robotic and standard fURS simulations.
We conducted the first prospective randomized trial in the literature comparing the simulation between robotic and standard fURS. In our study, ten medical students after ten training sessions were able to acquire good ureteroscopic skills in a simulator model both in robotic and standard fURS. The skills were evaluated according the validation tool: Objective Structured Assessment of Technical Skills for surgical residents (OSATS) that analyzes the knowledge of the procedure, the instrument handling and the trainees’ competence [8].
The results demonstrate the rapid acquisition of ureteroscopic skills for trainees with no prior surgical training, and therefore the efficacy of training models in fURS.
Moreover, no major significant differences were seen between the groups, except for the stability item that was better in the robotic group for the first exercise, although it took the same group longer time to perform the second exercise.
These data potentially suggest similar learning curves for robotic and standard fURS in a training model that may later maximize the surgeons’ skills and support the trainers’ proficiency and excellence. Nevertheless, these results should be considered with caution because our study certainly presents some limitations due to low numbers of students in each group and, consequently, a lack of adequate statistical power; but to our best knowledge, this is the first study that compares the acquisition of endourological skills with and without Roboflex Avicenna in a simulator model.
Further investigation with a wider cohort of participants is needed to establish the real lack of statistical differences in the acquisition of basic ureteroscopic skills with and without robotic fURS.
CONCLUSIONS
According to these preliminary results, the acquisition of basic ureteroscopic skills with and without robotic fURS in the K-box® simulator, by subjects with no prior surgical training, is similar.
CONFLICTS OF INTEREST
Traxer O: consultant for Coloplast, Rocamed, Olympus, Lumenis, Boston Scientific, Biohealth, EMS.
Giusti G: consultant for Coloplast, Rocamed, Olympus, Lumenis, Boston Scientific, Karl Storz, Cook Medical.
References
- 1.Giusti G, Proietti S, Luciani LG, et al. Is retrograde intrarenal surgery for the treatment of renal stones with diameters exceeding 2 cm still a hazard? Can J Urol. 2014;21:7207–7212. [PubMed] [Google Scholar]
- 2.Giusti G, Proietti S, Peschechera R, et al. Sky is no limit for ureteroscopy: extending the indications and special circumstances. World J Urol. 2015;33:257–273. doi: 10.1007/s00345-014-1345-y. [DOI] [PubMed] [Google Scholar]
- 3.Saglam R, Muslumanoglu AY, Tokatlı Z, et al. A new robot for flexible ureteroscopy: development and early clinical results (IDEAL stage 1-2b) Eur Urol. 2014;66:1092–1100. doi: 10.1016/j.eururo.2014.06.047. [DOI] [PubMed] [Google Scholar]
- 4.Naylor RA, Hollett LA, Valentine RJ, et al. Can medical students achieve skills proficiency through simulation training? Am J Surg. 2009;198:277–282. doi: 10.1016/j.amjsurg.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 5.Villa L, Sener TE, Somani KS, et al. Initial content validation results of a new simulation model for flexible ureteroscopy: the Key-box. J Endourol. 2016 doi: 10.1089/end.2016.0677. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Villa L, Somani BK, Sener TE, et al. Comprehensive flexible ureteroscopy (FURS) simulator for training in endourology: The K-box model. Cent European J Urol. 2016;69:118–120. doi: 10.5173/ceju.2016.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu WG, Feng JY, Wang J, Song, et al. Ureteroscopy and cistoscopy training: comparison between transparent and non-transparent simulators. BMC Med Educ. 2015;15:93. doi: 10.1186/s12909-015-0380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou DS, Abdelshehid C, Clayman RV, et al. Comparison of results of virtual-reality simulator and training model for basic ureteroscopy training. J Endourol. 2006;20:266–271. doi: 10.1089/end.2006.20.266. [DOI] [PubMed] [Google Scholar]
- 9.Faulkner H, Regehr G, Martin J, et al. Validation of an objective structured assessment of technical skill for surgical residents. Acad Med. 1996;71:1363–1365. doi: 10.1097/00001888-199612000-00023. [DOI] [PubMed] [Google Scholar]
- 10.White MA, Dehaan AP, Stephens DD, et al. Validation of a high fidelity adult ureteroscopy and renoscopy simulator. J Urol. 2010;183:673–677. doi: 10.1016/j.juro.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Schout BM, Hendrikx AJ, Scherpbier AJ, et al. Update on training models in endourology: a qualitative systematic review of the literature between January 1980 and April 2008. Eur Urol. 2008;54:1247–1261. doi: 10.1016/j.eururo.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 12.Huri E, Skolarikos A, Tatar İ, et al. Simulation of RIRS in soft cadavers: a novel training model by the Cadaveric Research On Endourology Training (CRET) Study Group. World J Urol. 2016;34:741–746. doi: 10.1007/s00345-015-1676-3. [DOI] [PubMed] [Google Scholar]
- 13.Skolarikos A, Gravas S, Laguna MP, et al. Training in ureteroscopy: a critical appraisal of theliterature. BJU Int. 2011;108:798–805. doi: 10.1111/j.1464-410X.2011.10337.x. [DOI] [PubMed] [Google Scholar]