Abstract
Background
Reasons for the increased incidence of cesarean delivery among women with inflammatory bowel disease remain unclear. We assessed cesarean delivery incidence and factors influencing mode of delivery in women with inflammatory bowel disease.
Methods
We performed a 10-year retrospective cohort study of nulliparous women who delivered a singleton infant at our institution. We compared risk for each mode of delivery in women with Crohn's disease and ulcerative colitis to women without inflammatory bowel disease. We assessed mode of delivery indications for patients with inflammatory bowel disease and whether cesarean deliveries were planned.
Results
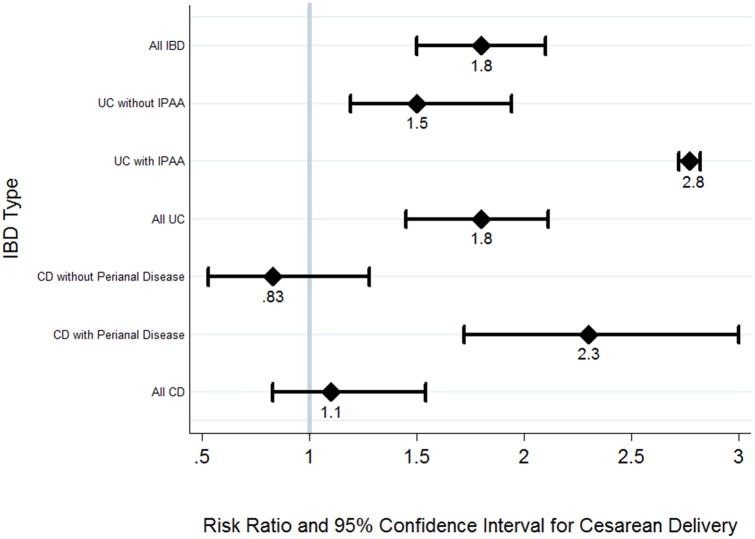
The overall incidence of cesarean delivery among women with Crohn's disease (24/59; 40.7%) was similar to women without inflammatory bowel disease (7868/21805; 36.1%) (RR 1.1 [95% CI: 0.83,1.5]; p=0.46), but was increased in the subgroups with active and inactive perianal disease (RR 2.3; p<0.01). Women with ulcerative colitis had a 1.8-fold increased relative risk of cesarean delivery (41/65; 63.1%) (95% CI 1.5, 2.1; p<0.01), with highest incidence in patients with ileal pouch-anal anastomosis. Forty-nine percent of ulcerative colitis and 66.7% of Crohn's disease cesarean deliveries were unplanned, with only one unplanned delivery performed for active inflammatory bowel disease. Most unplanned deliveries were for arrest of descent/dilation and non-reassuring fetal heart tracings. Seventy-five percent of planned cesarean deliveries were for inflammatory bowel disease-related indications.
Conclusions
Women with ulcerative colitis and perianal Crohn's disease have an increased incidence of cesarean delivery. At least half of cesarean deliveries are unplanned.
Keywords: Crohn's disease, ulcerative colitis, cesarean delivery, pregnancy, childbirth
Introduction
Inflammatory bowel disease (IBD) affects many women of reproductive age, making the interaction of this disease with pregnancy and childbirth an important consideration. Previous studies have suggested that patients with ulcerative colitis (UC) and Crohn's disease (CD) have a higher incidence of cesarean delivery compared to women without IBD1-9. Population-based studies have shown that this increased risk of cesarean delivery exists for both unscheduled and scheduled procedures3, 7. In contrast to these observations, recent data and expert consensus suggest that vaginal delivery is safe for most patients, and mode of delivery should be determined by obstetric indications and patient preference10-14. Current European14 and Toronto13 guidelines designate only active perianal disease as a definite indication, and ileal pouch-anal anastomosis (IPAA) as a relative indication for cesarean delivery. It is unclear if these sub-populations alone drive the increased incidence of cesarean delivery in patients with IBD, or if there are other risk factors for cesarean delivery in the IBD population.
The concern regarding vaginal delivery following IPAA is that it may lead to occult anal sphincter injury and worsen fecal incontinence15, 16. Several studies, however, have yielded conflicting results regarding these outcomes14, 17-20. The presence of active perianal disease is also of concern in vaginal delivery, as a vaginal trauma or laceration at the time of delivery may hypothetically lead to progressive perianal symptoms or non-healing fistula in a patient with active perianal CD. As such, cesarean delivery is recommended for patients with active perianal disease13, 14. Ilnychyj et al.3 found that among women with CD, all of the women with active perianal disease at the time of vaginal delivery (4 of 15) reported subjective worsening of perianal symptoms post-partum. The women with inactive perianal disease (11 of 15) had no relapse of disease within one-year post-partum3. Patients with inactive perianal disease are not considered at increased risk for fistula development or disease flare if they undergo a vaginal delivery, and mode of delivery is often left up to the treating obstetrician.
We undertook this study to compare the incidence of cesarean delivery between women with UC and CD and women without IBD, and to identify indications for cesarean delivery among women with IBD to better assess the underlying driving factors for mode of delivery. We evaluated whether cesarean deliveries were planned or unplanned.
Materials and Methods
We performed a retrospective cohort study of all nulliparous women (women who had not previously given birth) who delivered a singleton infant at our medical center from 2003 through 2013. Women who had previously given birth and those pregnant with more than one fetus were excluded from the study, as these factors are independent risk factors for cesarean delivery. However, women with previous pregnancies (non-primigravid) who had never given birth (i.e. experienced spontaneous or planned abortions) were included. We identified women with IBD by ICD-9 codes (556.x and 555.x). Women identified as having IBD were excluded if they did not have gastroenterology chart documentation or if they were diagnosed with IBD after delivery. All patients included were assessed by a gastroenterologist at minimum prior to pregnancy and after delivery. Clinical assessments during pregnancy and at delivery were made by gastroenterology and/or obstetrics at variable time points based on clinical need and practice.
We obtained demographic information, obstetric provider, and mode of delivery from medical records for all women. For women with IBD we also extracted data on comorbidities known to be associated with cesarean delivery (including diabetes and smoking), pregnancy course, planned and actual mode of delivery, and indication for cesarean delivery. Additionally, we retrieved IBD-specific data including location and type of IBD; medications and disease activity before pregnancy (within six months before conception), during pregnancy (anytime during pregnancy or at time of delivery), and after pregnancy (within three months of delivery); and whether the gastroenterologist was a generalist or IBD subspecialist. The charts were reviewed to determine disease activity, defined as active versus inactive by the treating physician.
A cesarean delivery was classified as planned if that was the intended mode of delivery, regardless of whether the delivery occurred on the originally planned date. All other cesarean deliveries were deemed unplanned. The indication for cesarean delivery was noted, and each indication was categorized into one of ten encompassing IBD- or non-IBD-related indication groups.
We used the chi-square or Fisher's exact test to compare categorical data and a t-test or Wilcoxon rank sum test to compare continuous data, depending on normality of the distribution. We used modified Poisson regression21 to calculate risk ratios (RR) and 95% confidence intervals (CI). We considered demographic characteristics, medication use, and disease activity before and during pregnancy, as well as at time of delivery, as potential confounders. Variables that altered the risk ratio by more than 10% were retained in the model. All tests were two sided, and p-values <0.05 were considered statistically significant.
Ethical Considerations
Our institutional review board approved the study.
Results
Baseline characteristics
During the 10-year study period 21929 nulliparous women delivered singleton infants at our institution. Of these women, 176 (0.8%) had IBD. Thirty-six women without sufficient gastroenterology chart documentation to assess disease status and 16 women diagnosed with IBD after delivery were excluded, yielding 124 subjects with IBD (59 with CD and 65 with UC). Women with CD and UC were more likely to be non-Hispanic white (89.8% and 80.0%, respectively) compared to women without IBD (55.3%; both p<0.01). Compared to women without IBD (77.7%), women with UC were more likely to be primigravid (89.2%; p=0.03). In addition, women with CD were more likely to have private insurance (89.8% vs. 77.1%; p=0.02). See Table 1 for baseline characteristics.
Table 1. Baseline characteristics.
| Characteristic | No IBD n=21805 |
Crohn's Disease n=59 |
p | Ulcerative Colitis n=65 |
p |
|---|---|---|---|---|---|
| Maternal Age (years) | 30.9 ±5.4 | 31.5 ±4.3 | 0.30 | 32.0 ± 5.5 | 0.11 |
| Race/Ethnicity | <0.01 | <0.01 | |||
| Non-Hispanic white | 12055 (55.3) | 53 (89.8) | 52 (80.0) | ||
| Non-Hispanic black | 2150 (9.9) | 1 (1.7) | 4 (6.2) | ||
| Hispanic | 1038 (4.8) | 2 (3.4) | 1 (1.5) | ||
| Other | 4489 (20.6) | 2 (3.4) | 5 (7.7) | ||
| Unknown | 2073 (9.5) | 1 (1.7) | 3 (4.6) | ||
| Obstetric Provider Type | <0.01 | <0.01 | |||
| Generalist obstetrician | 19989 (91.7) | 37 (62.7) | 36 (55.4) | ||
| Maternal-fetal medicine specialist | 1816 (8.3) | 22 (37.3) | 29 (44.6) | ||
| Gravidity | 0.72 | 0.03 | |||
| 1 | 16945 (77.7) | 47 (79.7) | 58 (89.2) | ||
| ≥2 | 4860 (22.3) | 12 (20.3) | 7 (10.8) | ||
| Insurance Type | 0.02 | 0.28 | |||
| Private | 16817 (77.1) | 53 (89.8) | 55 (84.6) | ||
| Public | 4139 (19.0) | 3 (5.1) | 7 (10.8) | ||
| Uninsured | 44 (0.2) | 0 (0.0) | 0 (0.0) | ||
| Other | 805 (3.7) | 3 (5.1) | 3 (4.6) |
Data are presented as mean ± SD or n (%)
IBD: Inflammatory bowel disease
Half (49.2%) of women with CD had ileocolonic involvement, and 18.6% had a history of perianal disease. Most women with UC had left-sided disease (32.3%) or pancolitis (36.9%), and 15.4% had undergone IPAA. Twenty-four percent of women with CD and 41.5% of women with UC had active disease during pregnancy. Four of 11 patients (36.3%) with perianal disease experienced active disease during pregnancy. Other disease characteristics of the women with IBD are presented in Table 2.
Table 2. Disease characteristics among women with IBD.
| Characteristic | Crohn's Disease n (%) n=59 |
Ulcerative Colitis n (%) n=65 |
|---|---|---|
| Extent/Location of Disease | ||
| Proctitis (UC) | 9 (13.9) | |
| Left-sided (UC) | 21 (32.3) | |
| Pan-colitis (UC) | 24 (36.9) | |
| Unknown (UC) | 11 (16.9) | |
| Ileal (CD) | 10 (17.0) | |
| Colonic (CD) | 15 (25.4) | |
| Ileocolonic (CD) | 29 (49.2) | |
| Unknown (CD) | 5 (8.5) | |
| Perianal CD | 11 (18.6) | |
| Ileal pouch-anal anastomosis | 10 (15.4) | |
| Other abdominal surgery for IBD | 16 (27.1) | 1 (1.5) |
| Medications during pregnancy | ||
| None | 12 (20.3) | 15 (23.1) |
| Maintenance therapy | ||
| Rectal 5-ASA monotherapy | 0 (0.0) | 9 (13.8) |
| Oral 5-ASA monotherapy | 19 (32.2) | 11 (16.9) |
| Rectal + oral 5-ASA | 1 (1.7) | 11 (16.9) |
| Thiopurine monotherapy | 7 (11.9) | 4 (6.2) |
| Thiopurine + 5-ASA | 11 (18.6) | 9 (13.8) |
| Anti-TNF Monotherapy | 5 (8.5) | 0 (0.0) |
| Thiopurine + anti-TNF | 3 (5.1) | 1 (1.5) |
| Thiopurine + anti-TNF + 5-ASA | 1 (1.7) | 0 (0.0) |
| Steroid enemas* | 2 (3.4) | 4 (6.15) |
| Any systemic steroid use* | 3 (5.1) | 5 (7.7) |
| Antibiotics* | 1 (1.7) | 3 (4.6) |
| Gastroenterologist | ||
| General | 23 (39.0) | 21 (32.2) |
| Inflammatory bowel disease | 33 (55.9) | 34 (52.3) |
| None | 0 (0.0) | 5 (7.7) |
| Unknown | 3 (5.1) | 5 (7.7) |
| Disease activity | ||
| Active disease | ||
| Before pregnancy | 9 (15.3) | 18 (27.7) |
| During pregnancy and/or delivery | 14 (23.7) | 27 (41.5) |
| Inactive disease | 41 (69.5) | 32 (49.2) |
N (%)calculated separately than from maintenance therapies
Incidence of cesarean delivery in patients with IBD
Mode of delivery in patients without IBD, with UC, and with CD is shown in Table 3. Of 21805 patients without IBD, 7868 (36.1%) underwent cesarean delivery. Women with UC were significantly more likely to have a cesarean delivery (41/65; 63.1%) compared to women without IBD (p<0.001), yielding a nearly two-fold increased risk (RR: 1.8; 95% CI: 1.5-2.1). All women with UC and an IPAA underwent cesarean delivery, and therefore had a notably higher incidence of cesarean delivery compared with women without IBD. Though fewer women with UC without IPAA underwent cesarean delivery (54.7%), this incidence was also higher than among women without IBD (p<0.01). Adjusting for maternal age, race, insurance status, rectal medication use, and gravidity did not appreciably alter the associations. Crude associations are presented in Figure 1.
Table 3. Mode of Delivery.
| Outcome | No IBD n=21805 |
Crohn's Disease n=59 |
p | Ulcerative Colitis n=65 |
p |
|---|---|---|---|---|---|
| Mode of delivery | 0.46 | <0.001 | |||
| Vaginal | 13937 (63.9) | 35 (59.3) | 24 (36.9) | ||
| Cesarean | 7868 (36.1) | 24 (40.7) | 41 (63.1) |
Data presented as n (%)
Figure 1. Crude risk ratios for cesarean delivery among women with IBD compared to women without IBD.
Among women with CD, 24/59 (40.7%) had a cesarean delivery, which was similar to the incidence among women without IBD (36.1%; p=0.46), yielding a RR of 1.1 (95% CI: 0.83-1.5). The majority (83.3%) of women with CD and a history of perianal disease (either active or inactive during pregnancy) had a cesarean delivery, which was significantly higher than among women without IBD (p=0.03). Only two women in this cohort had active perianal disease at the time of delivery. Among those without a history of perianal disease, the incidence of cesarean delivery (37.0%) was similar to women without IBD (p=0.89). As with the UC models, adjusting for potential confounders did not appreciably alter the associations. Crude associations are presented in Figure 1.
Indications and risk factors for cesarean delivery in women with IBD
The indications for cesarean delivery amongst women with IBD are shown in Table 4. Of the 41 cesarean deliveries in women with UC, 21 (51.2%) were planned and 20 (48.8%) were unplanned. Just over half (52.4%) of the planned cesarean deliveries for UC were for an IBD-related indication, with 28.6% for a history of IBD (not active at the time of delivery), and 23.8% for history of IPAA. In contrast, none of the unplanned cesarean deliveries were for an IBD-related indication, with 9 (45.0% of unplanned deliveries) for arrest of descent/dilation, 10 (50.0%) for non-reassuring fetal heart tracings, and 1 (5%) for non-vertex presentation. No patients underwent cesarean delivery for active UC.
Table 4. Indications for cesarean delivery by type of inflammatory bowel disease.
| Crohn's Disease | Ulcerative Colitis | |
|---|---|---|
| Planned | n=8 | n=21 |
|
| ||
| History of IBD | 5 (62.5) | 6 (28.6) |
| IBD flare | 1 (12.5) | 0 (0.0) |
| IPAA | 0 (0.0) | 5 (23.8) |
| Previous abdominal surgery | 0 (0.0) | 1 (4.8) |
| Acute non-IBD medical comorbidity | 1 (12.5) | 1 (4.8) |
| Non-vertex presentation | 0 (0.0) | 5 (23.8) |
| Anatomic abnormality | 1 (12.5) | 1 (4.8) |
| Elective | 0 (0.0) | 2 (9.5) |
|
| ||
| Unplanned | n=16 | n=20 |
|
| ||
| Arrest of descent/dilation | 7 (43.8) | 9 (45.0) |
| Non-reassuring FHT | 5 (31.3) | 10 (50.0) |
| Non-vertex presentation | 1 (6.3) | 1 (5.0) |
| Anatomic abnormality | 2 (12.5) | 0 (0.0) |
| IBD flare | 1 (6.3) | 0 (0.0) |
Of the 24 cesarean deliveries amongst women with CD, 8 (33.3%) were planned and 16 (66.7%) were unplanned. Six (75%) of the planned cesarean deliveries were for an IBD-related indication (62.5% for a history of perianal CD and 12.5% for active disease at the time of delivery), while only 1 (6.3%) of the unplanned cesarean deliveries was for an IBD-related indication (p=0.001). Most unplanned cesarean deliveries in patients with CD were for arrest of descent/dilation (43.8% of unplanned deliveries) and non-reassuring fetal heart tracings (31.3%). The one unplanned cesarean delivery for an IBD-related indication occurred in a woman with a Crohn's flare and clinical evidence of peritonitis.
The incidence of cesarean delivery was not related to disease activity. Among women with UC, 17 (63.0%) of those who had active disease during pregnancy had a cesarean delivery compared to 23 (62.2%) of those who did not have active disease (p=0.95). Of the 17 women who had a cesarean delivery and active disease during pregnancy, 9 (52.9%) had an unplanned cesarean delivery, none for the indication of IBD. Although this incidence was higher than the incidence among the 23 women with UC and without active disease (43.5%), the difference was not statistically significant (p=0.79). Among women with CD, 8 (57.1%) of those who had active disease during pregnancy had a cesarean delivery compared to 15 (36.6%) of those without active disease (p=0.41). Of the 8 women with active disease during pregnancy who had a cesarean delivery, 4 (50.0%) had an unplanned cesarean delivery, which was not significantly different from the proportion among women with CD who did not have active disease (73.3%; p=0.42). Only one unplanned cesarean delivery in women with CD was for the indication of IBD.
Discussion
Several studies have specifically examined the effect of perianal CD and IPAA on mode of delivery3, 11, 12, 15, 18, but, to our knowledge, this is the first U.S. study to examine the full distribution of indications for cesarean delivery amongst women with IBD and whether they were planned or unplanned. We confirmed a higher rate of cesarean delivery amongst patients with UC (with or without IPAA) and patients with perianal CD (inactive or active), but not in all patients with CD. At our academic medical center, the majority of cesarean deliveries among women with IBD were performed for medical reasons unrelated to IBD. Furthermore, nearly half of cesarean deliveries in patients with UC and two-thirds of cesarean deliveries in patients with CD were unplanned. Most unplanned cesarean deliveries occurred for non-reassuring fetal heart tracings, arrest of descent, and arrest of dilation. The reason for the high rate22, 23 of these events in this population remains unclear. We did not detect an association between disease activity and mode of delivery; one may hypothesize that a subclinical increase in inflammatory milieu may increase the risk for other maternal conditions that would lead to unplanned cesarean delivery. It is equally possible that other unmeasured factors play an important role in decisions regarding mode of delivery within this population. Future studies comparing mode of delivery in patients with IBD to another chronic inflammatory disorder may help elucidate this issue.
Consistent with current guidelines13, 14 where IPAA is a relative indication for cesarean delivery, all patients with an IPAA underwent cesarean delivery. Both patients with active perianal disease at the time of delivery underwent cesarean delivery as well. However, 5 of 8 (62.5%) patients with CD underwent planned cesarean delivery for a history of inactive perianal CD, and 6 of 21 (28.6%) patients with UC underwent planned cesarean delivery for a history of IBD, though they experienced no active disease during pregnancy. The indication for these deliveries diverges from current guidelines, though the extent of divergence appears consistent with other recent findings of cesarean delivery for IBD. In a recent study by Cheng et al.24 50 (82%) of 61 patients with perianal CD underwent cesarean delivery, though only three were noted to have active perianal disease during pregnancy. This data provides a real-world assessment of adherence to delivery guidelines in IBD. In this population, we are unable to conclude if cesarean deliveries that diverged from guidelines were avoidable, as there may have been clinical factors in this tertiary care population for which we could not account that impacted clinical decision making.
These data must be interpreted in the context of the study design and patient population. Despite a 10-year follow-up period, the number of singleton births in nulliparous women with IBD in this single-center study was low, limiting the power of our study to detect differences across outcomes. The majority of our participants were Caucasian, and a large proportion was cared for by maternal-fetal medicine providers at our tertiary care center, possibly limiting the generalizability of our findings. Patients appear to have had relatively mild disease, marked by the low proportion of patients followed by an IBD specialist as compared to general gastroenterologist. Anti-tumor necrosis factor therapy use also was low in our cohort, which may reflect the overall severity of disease in this cohort or concern regarding medication use in pregnancy. Though our demographic, pregnancy-related, and medication variables could be abstracted from medical records, our ability to define and capture active disease or flare was solely based on expert physician impression on chart review. The incidence of unplanned cesarean deliveries in the IBD population was higher than expected22, 23, but we are unable to further evaluate this finding as we do not have similar data for women without IBD.
In summary, patients with UC (with and without IPAA) and active or inactive perianal CD are at increased risk of cesarean delivery in comparison to the general population. Most planned cesarean deliveries were for the indication of IBD. However, more than half of cesarean deliveries were unplanned, with only one unplanned cesarean delivery performed in our population for the indication of IBD. Subclinical inflammation or other unmeasured factors may account for the high rate of unplanned cesarean delivery and should be addressed in future studies.
Acknowledgments
Guarantor of article: Kristin E. Burke
Source of Funding: Declaration of funding interests: This work was supported by the Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers.
Footnotes
- Authors' declaration of personal interests:
- Adam Cheifetz has consulted for Janssen, Abbvie, UCB, Prometheus, Pfizer, and Takeda.
- The remaining authors declare no conflicts of interest.
- Kristin E. Burke - Study conception and design, data acquisition, drafting manuscript, critically revising manuscript
- Miriam J. Haviland - Analysis and interpretation of data, critically revising manuscript
- Michele R. Hacker - Analysis and interpretation of data, critically revising manuscript
- Scott A. Shainker – Data acquisition, critically revising manuscript
- Adam S. Cheifetz - Study conception and design, critically revising manuscript
References
- 1.Manosa M, Navarro-Llavat M, Marin L, et al. Fecundity, pregnancy outcomes, and breastfeeding in patients with inflammatory bowel disease: a large cohort survey. Scand J Gastroenterol. 2013;48:427–32. doi: 10.3109/00365521.2013.772229. [DOI] [PubMed] [Google Scholar]
- 2.Fonager K, Sorensen HT, Olsen J, et al. Pregnancy outcome for women with Crohn's disease: a follow-up study based on linkage between national registries. Am J Gastroenterol. 1998;93:2426–30. doi: 10.1111/j.1572-0241.1998.00698.x. [DOI] [PubMed] [Google Scholar]
- 3.Ilnyckyji A, Blanchard JF, Rawsthorne P, et al. Perianal Crohn's disease and pregnancy: role of the mode of delivery. Am J Gastroenterol. 1999;94:3274–8. doi: 10.1111/j.1572-0241.1999.01537.x. [DOI] [PubMed] [Google Scholar]
- 4.Kornfeld D, Cnattingius S, Ekbom A. Pregnancy outcomes in women with inflammatory bowel disease--a population-based cohort study. Am J Obstet Gynecol. 1997;177:942–6. doi: 10.1016/s0002-9378(97)70298-9. [DOI] [PubMed] [Google Scholar]
- 5.Mahadevan U, Sandborn WJ, Li DK, et al. Pregnancy outcomes in women with inflammatory bowel disease: a large community-based study from Northern California. Gastroenterology. 2007;133:1106–12. doi: 10.1053/j.gastro.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 6.Norgard B, Fonager K, Sorensen HT, et al. Birth outcomes of women with ulcerative colitis: a nationwide Danish cohort study. Am J Gastroenterol. 2000;95:3165–70. doi: 10.1111/j.1572-0241.2000.03290.x. [DOI] [PubMed] [Google Scholar]
- 7.Broms G, Granath F, Linder M, et al. Complications from inflammatory bowel disease during pregnancy and delivery. Clin Gastroenterol Hepatol. 2012;10:1246–52. doi: 10.1016/j.cgh.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen GC, Boudreau H, Harris ML, et al. Outcomes of obstetric hospitalizations among women with inflammatory bowel disease in the United States. Clin Gastroenterol Hepatol. 2009;7:329–34. doi: 10.1016/j.cgh.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 9.Naganuma M, Kunisaki R, Yoshimura N, et al. Conception and pregnancy outcome in women with inflammatory bowel disease: A multicentre study from Japan. J Crohns Colitis. 2011;5:317–23. doi: 10.1016/j.crohns.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 10.McConnell RA, Mahadevan U. Pregnancy and the Patient with Inflammatory Bowel Disease: Fertility, Treatment, Delivery, and Complications. Gastroenterol Clin North Am. 2016;45:285–301. doi: 10.1016/j.gtc.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Ananthakrishnan AN, Cheng A, Cagan A, et al. Mode of childbirth and long-term outcomes in women with inflammatory bowel diseases. Dig Dis Sci. 2015;60:471–7. doi: 10.1007/s10620-014-3353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grouin A, Brochard C, Siproudhis L, et al. Perianal Crohn's disease results in fewer pregnancies but is not exacerbated by vaginal delivery. Dig Liver Dis. 2015;47:1021–6. doi: 10.1016/j.dld.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen GC, Seow CH, Maxwell C, et al. The Toronto Consensus Statements for the Management of Inflammatory Bowel Disease in Pregnancy. Gastroenterology. 2016;150:734–757 e1. doi: 10.1053/j.gastro.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 14.van der Woude CJ, Ardizzone S, Bengtson MB, et al. The Second European Evidenced-Based Consensus on Reproduction and Pregnancy in Inflammatory Bowel Disease. J Crohns Colitis. 2014 doi: 10.1093/ecco-jcc/jju006. [DOI] [PubMed] [Google Scholar]
- 15.Remzi FH, Gorgun E, Bast J, et al. Vaginal delivery after ileal pouch-anal anastomosis: a word of caution. Dis Colon Rectum. 2005;48:1691–9. doi: 10.1007/s10350-005-0124-7. [DOI] [PubMed] [Google Scholar]
- 16.Sultan AH, Kamm MA, Hudson CN, et al. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905–11. doi: 10.1056/NEJM199312233292601. [DOI] [PubMed] [Google Scholar]
- 17.Ilnyckyj A. Surgical treatment of inflammatory bowel diseases and pregnancy. Best Pract Res Clin Gastroenterol. 2007;21:819–34. doi: 10.1016/j.bpg.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Hahnloser D, Pemberton JH, Wolff BG, et al. Pregnancy and delivery before and after ileal pouch-anal anastomosis for inflammatory bowel disease: immediate and long-term consequences and outcomes. Dis Colon Rectum. 2004;47:1127–35. doi: 10.1007/s10350-004-0569-0. [DOI] [PubMed] [Google Scholar]
- 19.Ravid A, Richard CS, Spencer LM, et al. Pregnancy, delivery, and pouch function after ileal pouch-anal anastomosis for ulcerative colitis. Dis Colon Rectum. 2002;45:1283–8. doi: 10.1007/s10350-004-6411-x. [DOI] [PubMed] [Google Scholar]
- 20.Seligman NS, Sbar W, Berghella V. Pouch function and gastrointestinal complications during pregnancy after ileal pouch-anal anastomosis. J Matern Fetal Neonatal Med. 2011;24:525–30. doi: 10.3109/14767058.2010.494745. [DOI] [PubMed] [Google Scholar]
- 21.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 22.Barber EL, Lundsberg LS, Belanger K, et al. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118:29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203:326 e1–326 e10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng AG, Oxford EC, Sauk J, et al. Impact of mode of delivery on outcomes in patients with perianal Crohn's disease. Inflamm Bowel Dis. 2014;20:1391–8. doi: 10.1097/MIB.0000000000000093. [DOI] [PMC free article] [PubMed] [Google Scholar]