Abstract
Objectives
To examine rates of smoking and tobacco treatment utilization by insurance coverage status (Medicaid, commercial, exchange) among newly enrolled patients in the post ACA era.
Methods
We examined new members who enrolled in Kaiser Permanente Northern California (KPNC) through Medicaid, the California exchange, or non-exchange commercial plans (N=122,298) in the first six months of 2014 following ACA implementation. We compared these groups on smoking prevalence and tested whether smokers in each group differed on sociodemographic characteristics and in their utilization of tobacco treatment (pharmacotherapy and counseling) in 2014.
Results
Smoking prevalence was higher among Medicaid (22%) than exchange (13%) or commercial (12%) patients (p<.0001). Controlling for key sociodemographic and clinical characteristics, Medicaid (OR=1.49, 95% CI=1.29–1.73) smokers had greater odds of tobacco treatment use than commercial smokers. Other groups at risk for underuse included men, younger patients, Asians and Latinos.
Conclusions
In this cohort of newly enrolled patients after ACA implementation, Medicaid patients were more likely to be smokers compared to exchange and commercial patients, but they were also more likely to use tobacco treatment. Low tobacco treatment use among exchange and commercial plan smokers, as well as younger men, Asians and Latinos poses a significant obstacle to improving public health and additional targeted outreach strategies may be need to engage these patients with available health services.
Keywords: Smoking, tobacco treatment, healthcare reform, Affordable Care Act, integrated healthcare
Smoking remains the leading cause of preventable mortality in the United States.(1) In California, nearly 4 million people smoke, resulting in over $18 billion annually in direct health care costs and indirect costs due to smoking-related premature death, illness, and lost productivity.(2) Although most smokers want to quit smoking,(3) effective tobacco treatments are underused due to a variety of barriers. These challenges apply particularly to medically underserved and low-income populations, who typically smoke at disproportionately high rates, lack access to appropriate treatment, and cannot afford cessation medications.(3)
The 2010 Patient Protection and Affordable Care Act (ACA),(4) had major implications for increasing access to tobacco treatment, by expanding benefits for underserved and low-income smokers. Specifically, the ACA-mandated comprehensive coverage for tobacco treatment, including counseling and U.S. Food and Drug Administration-approved medications,(5) was implemented for most private health plans and newly eligible Medicaid beneficiaries in California. ACA implementation in California in January 2014,(5–8) including Medicaid expansion, exchange coverage, and comprehensive coverage for tobacco treatments without cost-sharing or prior authorization, has been associated with the reduction in uninsured population from 22% to 11%(6) and with bringing high-priority populations for tobacco control into the healthcare system,(6, 9) including the 1.4 million individuals who gained private insurance through the California insurance exchange and 2.4 million who enrolled in Medicaid in 2014.(6, 8) Populations with the greatest gains in healthcare coverage through the ACA in California were adults aged 19–34, men, and low-income enrollees,(6) —the same subgroups disproportionately represented among California’s smokers.(3, 10, 11)
The ACA has the potential to increase access to tobacco treatment for previously medically underserved subgroups of smokers with possible pent up demand for such services. For example, previous studies have demonstrated that Medicaid recipients, while more likely to smoke, are less likely to use tobacco treatment.(12–14) However, it is not clear whether expansion of coverage is sufficient to improve utilization of these services. In particular, Medicaid recipients and other vulnerable subgroups may face unique barriers to tobacco treatment use not related to coverage, such as difficulty navigating the healthcare system, lack of knowledge of benefits,(15) or competing medical and psychiatric healthcare needs.
In this study, we examine risk factors for smoking among newly enrolled patients following ACA implementation and the role of insurance status (i.e., Medicaid, exchange, commercial coverage) as a predictor of tobacco treatment use (medication, counseling) among smokers post-ACA. To our knowledge, the current study is one of the first to use an extensive electronic health record (EHR) with population-based smoking screening to characterize smokers post-ACA in a multi-specialty health care system.
METHODS
Setting
KPNC is a nonprofit, multi-specialty healthcare delivery system providing comprehensive health services to more than 3.9 million members(16) and covering >40% of the region’s commercially insured population.(17) KPNC has 24 hospitals, 47 medical centers, and >7,000 physicians who practice exclusively with KPNC. KPNC provides integrated medical and behavioral health treatment and is a recognized leader in establishing tobacco quality of care standards.(18) The membership is largely employed, racially and socio-economically diverse, and highly representative of the population from its geographic area.(19) The study protocol was approved by the KPNC Institutional Review Board.
Study Sample
The sample included 122,298 patients aged 18 and older who were newly enrolled in KPNC in the first 6 months of 2014 through Medicaid (including Medicaid expansion), the California exchange, or commercial plans purchased by small or large employers or by individuals outside of the exchange. Because we anticipated that differences in utilization by coverage type (e.g., due to differences in pent up demand) would be greatest in the early post-enrollment period, we limited sample enrollment to the first six months of 2014. Patients who had been enrolled in KPNC the prior six months, and those with Medicare coverage, unknown coverage, missing birth date, missing smoking status, enrollment for <60% of the first six membership months and enrollment gaps of greater than 45 days in the first six months of membership were excluded. Exclusion criteria were derived from the EHR. Of the 122,298 eligible patients, 15,936 were documented in the EHR as current smokers during the first six months of enrollment. Among these, 1,720 enrolled through Medicaid plans, 4,512 enrolled through the California exchange, and 9,704 through commercial plans (Appendix 1).
Measures
Smoking Status
New members who had been to at least one outpatient visit in the first 6 months of enrollment were assessed for smoking status through standardized screening at KPNC Medicine appointments by medical assistants. Our interest was in current smokers. Ninety percent of patients with at least one outpatient visit in the first 6 months of enrollment had their smoking status on record in the EHR. KPNC new members are routinely asked about their smoking status at their first KPNC visit.
Demographic Characteristics
Self-reported age, sex, and race/ethnicity were extracted from the EHR. For ease of interpretability, age was included as a categorical variable, which had no impact on the estimates for the main predictor of interest compared to other strategies for age (e.g., continuous, logarithmic). Median household income was geocoded from census data using patients’ addresses and was dichotomized as 1 (≤ median household salary) or 0 (>median household salary).(20, 21)
Comorbidities
We identified the most common current psychiatric disorders (depressive disorders, anxiety disorders, attention deficit hyperactivity disorders, bipolar spectrum disorders, and psychotic disorders), substance use disorders (alcohol and drug use disorders), and medical comorbidities (arthritis, hypertension, chronic pain, diabetes, asthma, chronic heart disease, and COPD) in our sample based on ICD-9 diagnoses recorded by providers in the EHR during the first six months of KPNC enrollment.
Coverage type
Patients were classified according to the first KPNC plan type in which they enrolled as new members in 2014: Medicaid, California exchange, or commercial (non-exchange) plans purchased by small or large employers or by individuals outside of the California exchange.
Tobacco Treatment Utilization
We coded patients as using tobacco treatment if they used medications or counseling services at any point in 2014; the timeframe for capturing utilization ranged from six months to one year (with allowable gaps). Use of tobacco cessation medication was determined by dispensation of any FDA-approved tobacco cessation medication (i.e., nicotine replacement therapy (NRT) gum, NRT lozenge, NRT inhaler, NRT patch, NRT nasal spray, varenicline, or bupropion) from a KPNC pharmacy at any point in 2014, regardless of date of enrollment. In KPNC, a tobacco dependence diagnosis is required for patients to receive a prescription for bupropion for tobacco dependence. Because bupropion is commonly prescribed to treat depressive disorders, we included it only if it was accompanied by a diagnosis of tobacco dependence. Data were extracted from the KPNC Pharmacy Information Management System database, which contains all data related to prescriptions dispensed at a KPNC inpatient or outpatient pharmacy.
Tobacco cessation counseling included KPNC in-person classes or individual telephone coaching during 2014, recorded in the EHR. Health education classes are offered with clinical health educators and focus on increasing motivation to quit by providing education about nicotine addiction, discussing tobacco cessation medications, and offering additional resources. Individual telephone coaching sessions are also available. Clinical health educators and telephone coaches can request cessation medication prescriptions from a patient’s physician.
Statistical Analysis
First, we examined smoking prevalence by type of coverage among the 122,298 newly enrolled patients. We calculated the number and percentage of smokers in each subgroup and used multivariable logistic regression to assess whether coverage type, age group, race, sex, income, and comorbidities predicted the odds of being a smoker. These covariates were initially considered for inclusion in the models based on their associations with smoking, insurance type, and utilization, as detailed in the literature.(3, 10, 11, 22–25) Final models were specified after running bivariate logistic models (not shown) to ensure associations between covariates and the outcomes of interest. For bivariate comparisons of multinomial outcomes, we used ordinal logistic regression for ordered outcomes (age category) and polytomous logistic regression for unordered outcomes (race). Subsequent analyses used the subsample (n=15,936) of newly enrolled current smokers. Bivariate logistic regression assessed whether the distributions of age group, race, sex, income, comorbidities, and use of tobacco treatment were significantly different among Medicaid or exchange smokers compared to commercial plan smokers. We used the Non-Parametric Krusker-Wallis test to examine differences in the median number of fills in the three coverage groups. Finally, coverage type was modeled as a predictor of the odds of any use of tobacco treatment, as well as the number of prescription fills for tobacco cessation medications (1, 2–3, or 4+ , not shown, adjusting for age group, race, sex, income, and comorbidities in multivariable models. Time enrolled in KPNC in 2014 was also assessed, as patients could have varying lengths of enrollment, leading to differential capture of tobacco cessation utilization. Two-sided p-values were calculated to determine significance of measures, and significance was defined as a p-value <0.05.
Bias analyses
We conducted a bias analysis to address the potential impact of the large proportion of patients who were missing information on smoking status, as described in Appendix 2. All statistical analyses were performed using SAS 9.3.
RESULTS
Correlates of Smoking
Medicaid patients were more likely to be current smokers (22%) than exchange (13%) (p<.0001) or commercial plan (12%) patients (p<.0001). Adjusting for covariates, Medicaid and exchange coverage were associated with statistically significant higher odds of smoking relative to commercial coverage (OR=1.74, 95% CI=1.63–1.85 and OR=1.07, 95% CI=1.03–1.11, respectively) (Table 1). Adults aged 35 or older, with non-White race/ethnicity, female gender, and higher income had significantly lower odds of smoking relative to those aged 34 or younger, with White race/ethnicity, male gender and lower income (p<.0001 for each). Compared to patients with no comorbidities, those with psychiatric disorders, substance use disorders, and medical comorbidities had greater odds of smoking (p<.0001 for each).
Table 1.
Multivariable logistic regression modeling odds of smoking among newly enrolled KPNC members in 2014
| Variable | N (%) Smokers | OR (95% CI) | P-value |
|---|---|---|---|
| Coverage Type | |||
| Commercial (ref) | 9,704 (12) | - | - |
| California Exchange | 4,512 (13) | 1.07 (1.03, 1.11) | 0.0018 |
| Medicaid | 1,720 (22) | 1.74 (1.63, 1.85) | <.0001 |
| Age Group | |||
| 18–24 years (ref) | 1,914 (14) | - | - |
| 25–34 years | 4,839 (13) | 0.94 (0.89, 1.00) | 0.057 |
| 35–44 years | 3,393 (13) | 0.88 (0.83, 0.94) | <.0001 |
| 45–54 years | 3,345 (13) | 0.86 (0.81, 0.92) | <.0001 |
| 55+ years | 2,445 (12) | 0.69 (0.64, 0.74) | <.0001 |
| Race | |||
| Non-Hispanic White (ref) | 7,931 (15) | - | - |
| AHPI | 2,443 (9) | 0.65 (0.62, 0.69) | <.0001 |
| Black | 1,444 (18) | 1.08 (1.02, 1.16) | 0.017 |
| Hispanic | 2,795 (10) | 0.61 (0.58, 0.64) | <.0001 |
| Other | 379 (15) | 0.95 (0.85, 1.07) | 0.409 |
| Sex | |||
| Male (ref) | 9,220 (17) | - | - |
| Female | 6,713 (10) | 0.49 (0.47, 0.51) | <.0001 |
| Median Incomea | |||
| <=median (ref) | 10,098 (15) | - | - |
| > median | 5,767 (11) | 0.68 (0.66, 0.71) | <.0001 |
| Comorbidities | |||
| Psychiatric Disorder | |||
| No (ref) | 12,683 (12) | - | - |
| Yes | 3,253 (19) | 1.42 (1.35, 1.49) | <.0001 |
| Substance Use Disorder | |||
| No (ref) | 15,024 (13) | - | - |
| Yes | 912 (43) | 3.45 (3.14, 3.79) | <.0001 |
| Medical Comorbidity | |||
| No (ref) | 9,412 (12) | - | - |
| Yes | 6,524 (15) | 1.17 (1.13, 1.22) | <.0001 |
Notes. Ref = Reference Group; AHPI = Asian, Hawaiian, or Pacific Islander; Other = multiracial or Native American;
=Income estimated from median household income of census blocks.
Characteristics of Smokers
Medicaid smokers were older, less likely to be Hispanic, Asian, Hawaiian or Pacific Islander, or other race/ethnicity, more likely to be Black or female, and had a lower income than commercial plan smokers, while exchange smokers were older and less likely to be Black or Hispanic than commercial plan smokers (p<.0001 for each) (Table 2).
Table 2.
Characteristics of newly enrolled smokers, by coverage type (N=15,936)
| Patient Characteristics | Medicaid | California Exchange | Commercial |
|---|---|---|---|
| Age Group, n (%)a | |||
| 18–24 years | 191 (11) | 379 (8.4) | 1,344 (14) |
| 25–34 years | 468 (27) | 1,051 (23) | 3,320 (34) |
| 35–44 years | 379 (22)* | 821 (18)* | 2,193 (23) |
| 45–54 years | 419 (24) | 1,118 (25) | 1,808 (19) |
| 55+ years | 263 (15) | 1,143 (25) | 1,039 (11) |
| Mean Age (SD) | 40.69 (12.45)* | 43.81 (12.95)* | 37.96 (11.82) |
| Race/Ethnicity, n (%) | |||
| Non-Hispanic White | 813 (49) | 2397 (56.8) | 4,721 (52) |
| Hispanic | 254 (15)* | 656 (16)* | 1,885 (21) |
| Black | 380 (23)* | 267 (6)* | 797 (9) |
| AHPI | 140 (8)* | 809 (19) | 1,494 (16) |
| Other | 76 (5)* | 90 (2) | 213 (2) |
| Missing | 57 | 293 | 594 |
| Sex, n (%) | |||
| Female | 903 (53)* | 1,878 (42) | 3,932 (41) |
| Missing | 0 | 1 | 2 |
| Median Incomeb ($) (IQR) | 45,927 (28,582)* | 60,123 (36,953) | 58,684 (37,437) |
| Missing | 7 | 7 | 57 |
| Psychiatric Disorders, n (%) | |||
| Depressive Disorders | 380 (22)* | 475 (11) | 896 (9) |
| Anxiety Disorders | 374 (22)* | 501 (11) | 1,116 (12) |
| Attention Deficit Hyperactivity Disorders | 40 (2) | 63 (1) | 145 (2) |
| Bipolar Spectrum Disorders | 127 (7)* | 105 (2) | 209 (2) |
| Psychotic Disorders | 54 (3)* | 24 (0.5) | 34 (0.4) |
| Any of the Above | 621 (36)* | 866 (19) | 1,766 (18) |
| Substance Use Disorders, n (%) | |||
| Alcohol Use Disorder | 83 (5)* | 167 (4)* | 268 (3) |
| Drug Use Disorder | 152 (9)* | 125 (3) | 262 (3) |
| Alcohol or Drug Use Disorder | 211 (12)* | 243 (5) | 458 (5) |
| Medical Comorbidities, n (%) | |||
| Arthritis | 459 (27)* | 744 (16)* | 1,330 (14) |
| Hypertension | 395 (23)* | 908 (20)* | 1,290 (13) |
| Chronic Pain | 368 (21)* | 342 (8) | 654 (7) |
| Diabetes | 176 (10)* | 415 (9)* | 546 (6) |
| Asthma | 257 (15)* | 323 (7) | 660 (7) |
| Chronic heart disease | 58 (3)* | 117 (3)* | 130 (1) |
| COPD | 93 (5)* | 159 (4)* | 168 (2) |
| Any of the Above | 1,015 (59)* | 2,003 (44)* | 3,506 (36) |
Notes. AHPI = Asian, Hawaiian, or Pacific Islander; Other = multiracial or Native American; COPD = Chronic obstructive pulmonary disease;
=Single p-value for multinomial outcome calculated using ordinal regression;
=Estimated from median household income of census blocks, and tested using Kruskal-Wallis test;
Significantly different from commercial (p<.05).
Medicaid smokers had the highest prevalence of comorbidities. More than a third (36%) had a psychiatric comorbidity diagnosis, whereas the prevalence among exchange and commercial plan smokers was 19% and 18%, respectively; depressive disorders and anxiety disorders were the most commonly diagnosed psychiatric comorbidities. Medicaid smokers were also more likely than commercial plan smokers to have a substance use disorder (12% versus 5%, respectively) and to have one or more medical comorbidities (59% versus 36%, respectively) (p<.0001 for each). Relative to commercial smokers, exchange smokers were more likely to have an alcohol use disorder (4% versus 3%, respectively) and to have one or more medical comorbidities (44% versus 36%, respectively) (p<.0001 for each).
Tobacco Treatment Utilization
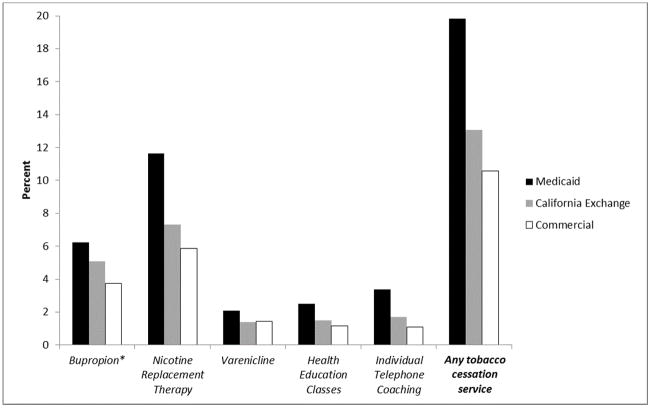
Overall, Medicaid smokers were the most likely to use each type of tobacco treatment in 2014 (Figure 1). Twenty percent of Medicaid smokers versus 13% of exchange smokers and 11% of commercial plan smokers used at least one type of treatment (p<.0001 for each). Pharmacotherapy, including NRT medications, varenicline, and bupropion, accounted for most treatment. The median number of tobacco cessation medication fills did not vary substantially by coverage type: Medicaid (median 2.0, IQR = 3.0), exchange (median = 2.0, IQR = 3.0), and commercial (median = 2.0, IQR = 2.0), though the distributions of number of fills were significantly different between the three groups (p<.0001, results not shown).
Figure 1.
Use of Tobacco Treatment in 2014 by Coverage Type
*Buproprion fills recorded only for patients with a Tobacco Dependence diagnosis in 2014
Adjusting for covariates, Medicaid smokers had greater odds of using at least one type of tobacco treatment than commercial plan smokers (OR = 1.49, 95% CI=1.29–1.73) (Table 3). Older age and female gender were significantly associated with greater odds of tobacco treatment utilization (p<.0001 for each), and Hispanic and Asian smokers had significantly lower odds of utilization compared to white smokers (p<.0001 for each). Co-occurring substance use disorders (OR = 1.61, 95% CI=1.35–1.92), psychiatric disorders (OR = 1.80, 95% CI=1.60–2.01), and medical comorbidities (OR = 1.38, 95% CI=1.24–1.53) were associated with greater odds of tobacco treatment use.
Table 3.
Multivariate logistic regression modeling odds of any tobacco treatment use in 2014 among smokers (N = 15,936)
| Variable | OR (95% CI) | P-value |
|---|---|---|
| Coverage Type (ref = Commercial) | ||
| Medicaid | 1.49 (1.29, 1.73) | <.0001 |
| California Exchange | 1.11 (0.99, 1.25) | 0.080 |
| Age Group (ref = 18–24 years) | ||
| 25–34 years | 2.16 (1.69, 2.76) | <.0001 |
| 35–44 years | 3.03 (2.36, 3.88) | <.0001 |
| 45–54 years | 3.47 (2.71, 4.44) | <.0001 |
| 55+ years | 3.55 (2.75, 4.59) | <.0001 |
| Race (ref = Non-Hispanic White) | ||
| AHPI | 0.76 (0.65, 0.88) | 0.0005 |
| Black | 1.04 (0.88, 1.22) | 0.662 |
| Hispanic | 0.57 (0.49, 0.67) | <.0001 |
| Other | 0.83 (0.61, 1.14) | 0.244 |
| Sex (ref = Male) | ||
| Female | 1.23 (1.11, 1.37) | <.0001 |
| Median Income ($)a (ref = ≤ median) | 0.97 (0.87, 1.08) | 0.564 |
| Comorbidities | ||
| Psychiatric Disorder | 1.80 (1.60, 2.01) | <.0001 |
| Substance Use Disorder | 1.61 (1.35, 1.92) | <.0001 |
| Medical Comorbidity | 1.38 (1.24, 1.53) | <.0001 |
| Days of enrollment in 2014 | 1.002 (1.001, 1.003) | <.0001 |
Notes. Ref = reference group; AHPI = Asian, Hawaiian, or Pacific Islander; Other = multiracial or Native American;
=Income estimated from median household income of census blocks.
Medicaid smokers had greater odds of filling multiple tobacco cessation prescriptions than commercial smokers (OR = 1.49, 95% CI=1.15–1.92), and exchange smokers had slightly greater (but not significant) odds (OR = 1.16, 95% CI=0.95–1.42) (results not shown). Older smokers and those with psychiatric disorders also had significantly greater odds of filling multiple prescriptions relative to younger smokers and those without psychiatric comorbidities, while Hispanic smokers had 45% lower odds of filling multiple prescriptions relative to white smokers. Substance use disorders and gender were not associated with number of prescription fills.
Bias Analyses
Results of the sensitivity analyses suggested that model estimates were modestly to negligibly biased towards the null (1–5% change in ORs); the only exception was the crude OR estimating the effect of Medicaid (vs. commercial) coverage on tobacco treatment utilization, which was estimated to be biased ~30% towards the null. Using these results, we can reasonably conclude that our results are valid estimates, with some instances of under-estimation and no crossover bias.
DISCUSSION
We evaluated risk factors for smoking among newly enrolled patients following the implementation of the ACA and examined the role of insurance status (i.e., Medicaid, CA exchange, commercial coverage) as a predictor of tobacco treatment use (medication, counseling) among smokers post-ACA. This is one of the first studies to use an extensive EHR with population-based smoking screening to characterize smokers post-ACA in a multi-specialty health care system.
As we anticipated, smoking prevalence was substantially higher among new patients with Medicaid coverage relative to new patients with commercial coverage. Smokers with Medicaid coverage were more likely to be female, less likely to be non-Hispanic White, and more likely to have low income and psychiatric, substance use, and medical comorbidities. Medicaid smokers were significantly more likely than commercial plan smokers to use tobacco treatments, including pharmacotherapy and counseling, even after adjustment for demographic and clinical characteristics. Medicaid coverage was also associated with filling a greater number of tobacco cessation prescriptions than commercial coverage. These results are consistent with the expectation of pent-up demand among new Medicaid enrollees, and support prior research indicating that Medicaid enrollees file more claims and have greater intensity of care in their first six months of enrollment after the ACA.(26) Our findings suggest that implementation of the ACA may provide opportunities for reducing long-standing disparities in access to smoking cessation services for the most vulnerable segments of the population with the highest smoking rates.
Conversely, smoking prevalence was low among newly insured patients with coverage through the California exchange and among those with traditional commercial plans; use of tobacco treatment was also low in these groups after adjustment for demographic characteristics and comorbidities. Given that half of individuals in the exchange in California were previously uninsured,22 we would expect a high level of pent up demand in this subgroup. The lack of a difference in tobacco treatment utilization in this group relative to newly insured traditional commercial members, suggests that factors other than access may be influencing health services use (e.g., differences in prior experience with treatment).
Despite ACA-mandated coverage for evidence-based tobacco treatments, which includes at least four counseling sessions and 90 days of FDA-approved medications with no cost-sharing, there is evidence of delayed implementation of the benefit for non-exchange enrollees. For example, in 2014, 100% of KPNC patients enrolling through the California exchange and >90% of Medicaid patients received coverage for tobacco cessation medications with no cost-sharing, while 80% of patients with coverage through commercial plans in 2014 still had cost-sharing for tobacco cessation medications. KPNC eliminated cost-sharing in January 2015 for commercial plan members with ACA-compliant plans after the Departments of Health and Human Services, Labor and Treasury issued guidance about the implementation of the ACA mandate for tobacco treatments.(27) Thus, it is possible that greater utilization of tobacco cessation medications among Medicaid versus commercial new member smokers in 2014 may be due in part to differences in cost-sharing. Conversely, despite evidence that exchange enrollees may be particularly price sensitive,(28) California exchange smokers were no more likely to use tobacco cessation medications than commercial plan smokers, even though they were significantly more likely than commercial plan smokers to receive their medications at no cost. Additional research is needed to better understand underuse of tobacco treatment in this subgroup of smokers.
Male smokers, younger smokers, and smokers with Asian or Hispanic race/ethnicity were less likely than female smokers, older smokers, and White smokers to use tobacco treatments, as shown in prior studies.(29, 30) Persistent challenges in engaging these patients, particularly those newly enrolled in healthcare, may indicate a need to develop targeted outreach and education programs. Determining the causes underlying demographic differences in use of tobacco treatments should help us understand the barriers associated with the patient (e.g., low interest in treatment) and the healthcare system (e.g., if providers are less likely to tell certain groups of patients about smoking cessation programs and medications).
KPNC offers a unique opportunity to use data from an established EHR to conduct this study in a real world setting that leverages external validity. However, the current study has several limitations. Our results are not directly generalizable to states with tobacco surcharges or those without Medicaid expansion, although the findings can assist policymakers and health systems in understanding early barriers to use of tobacco treatment mandated as part of health reform. Another limit of our study was that because screening for smoking occurred during routine visits, patients with no visits in the first six months of enrollment had no data on smoking status and thus were excluded. We addressed this issue by conducting bias analyses, and results indicated that any selection bias due to missing data was likely to bias results toward the null. In addition, our measure of over-the-counter and prescription fills for tobacco cessation medications was limited to those dispensed at KPNC pharmacies. While it is unlikely that patients would obtain these medications externally given that 95% of patients have KPNC drug benefits,(31) the use of smoking cessation medications may be underestimated. Our measure of tobacco cessation counseling included KPNC in-person classes or KPNC individual telephone coaching, and may have also underestimated the true use of tobacco cessation counseling (e.g., if patients used the California tobacco quitline). Further, our data systems do not distinguish between Medicaid patients who are newly eligible due to Medicaid expansion and those who are newly enrolled but were previously eligible. Greater use of tobacco treatments in newly enrolled KPNC Medicaid smokers might reflect prior experience with Medicaid and its strong emphasis on smoking cessation interventions.(32) Still, data from our Kaiser Division of Research Strategic Programming Group show a dramatic increase in Medicaid members in 2014 and low rates of disenrollment (written communication, June 2016), suggesting that most Medicaid members in our study were newly eligible for coverage due to the ACA.
Finally, while KPNC has implemented a system-wide approach to combat smoking, including routine assessment of tobacco use status, advice to quit, referrals to cessation programs, and clinician education about the ACAs tobacco provisions, it is possible that potential differences in sites of care among the three cohorts of insured smokers and minor variations in provider practice patterns could partially account for the differences in tobacco cessation medication utilization. We do not have data on clinician practices (e.g., whether they advised their patient to quit, conducted brief practical counseling during the office visit). However, clinicians in KPNC are typically not aware of the type of insurance that their patients have and thus, it is highly unlikely that differential treatment by clinicians would contribute to increased treatment utilization in Medicaid patients.
Conclusions
Tobacco treatment can dramatically reduce smoking and tobacco-related diseases and lead to measurable short- and long-term reductions in overall health expenditures,(33) yet effective treatments have been underused by low-income groups, who often lack access to appropriate treatment or cannot afford cessation medications.(3, 34) Our findings indicate low-income smokers may have improved access to healthcare and tobacco treatments post-ACA, possibly related to reduced barriers to utilization. Our findings can help clinicians, policy makers and health plan leadership understand which patients continue to be at risk for smoking and under-treatment for smoking post-ACA. As historically medically underserved patients are increasingly treated in accountable care organizations and other multi-specialty and integrated health care systems, it will be important to develop tailored outreach, education, and enrollment efforts to and engage newly insured smokers.(35) Continued monitoring of the association of insurance coverage with use of tobacco treatments and subsequent smoking cessation will help determine whether the promise of health reform for reducing disparities in tobacco use has been met.
Supplementary Material
Acknowledgments
This study was supported by a grant from the Tobacco-Related Disease Research Program (24XT-0008), a Kaiser Permanente Community Benefit Health Policy and Disparities Grant, and a grant from the National Institute on Drug Abuse (R21/R33 DA035645).
Footnotes
Disclosures:
The authors have no conflicts of interest to declare.
References
- 1.Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. [Accessed June 24, 2016];Smoking & Tobacco Use. Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/
- 2.Max W, Sung HY, Shi Y, et al. The cost of smoking in California, 2009. San Francisco, CA: Institute for Health & Aging, School of Nursing, University of California, San Francisco; 2014. [Google Scholar]
- 3.Tobacco Use and Dependence Guideline Panel. [Accessed December 22, 2016];Treating Tobacco Use and Dependence: 2008 Update. 2008 Available at: http://www.ncbi.nlm.nih.gov/books/NBK63952/
- 4. [Accessed August 11, 2016];Patient Protection and Affordable Care Act, 42 U.S.C. § 18001. Public Law 111–148. 2010 Available at: https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm.
- 5.McAfee T, Babb S, McNabb S, et al. Helping smokers quit--opportunities created by the Affordable Care Act. New England Journal of Medicine. 2015;372:5–7. doi: 10.1056/NEJMp1411437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reichard J. Survey shows drop in California’s uninsured, but with new cost concerns. [Accessed November 18, 2014];Washington Health Policy Week in Review. 2014 Aug 4; Available at: http://www.commonwealthfund.org/publications/newsletters/washington-health-policy-in-review/2014/aug/aug-4-2014/survey-shows-drop-in-californias-uninsured.
- 7.Satre DD, Altschuler A, Parthasarathy S, et al. Implementation and operational research: Affordable Care Act implementation in a California health care system leads to growth in HIV-positive patient enrollment and changes in patient characteristics. J Acquir Immune Defic Syndr. 2016;73:e76–e82. doi: 10.1097/QAI.0000000000001188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covered California’s historic first open enrollment finishes with projections exceeded; agents, counselors, community organizations and county workers credited as reason for high enrollment in California. [Accessed July 20, 2016];Covered California. 2014 Apr 17; Available at: http://news.coveredca.com/2014/04/covered-californias-historic-first-open.html.
- 9.Satre DD, Altschuler A, Parthasarathy S, et al. Affordable Care Act implementation in a California health care system leads to growth in HIV-positive patient enrollment and changes in patient characteristics [published online October 3, 2016] Journal of Acquired Immune Deficiencies Syndrome. 2016 doi: 10.1097/QAI.0000000000001188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention, Office of Surveillance, Epidemiology, et al. Prevalence and trends data: California - 2013 tobacco use. [Accessed November 20, 2014];Behavioral Risk Factor Surveillance System. 2014 Available at: http://nccd.cdc.gov/brfssprevalence/rdPage.aspx?rdReport=DPH_BRFSS.ExploreByLocation&rdProcessAction=&SaveFileGenerated=1&islLocation=06&islClass=CLASS17&islTopic=Topic15&islYear=2013&hidLocation=06&hidClass=CLASS17&hidTopic=Topic15&hidTopicName=Current+Smoker+Status&hidYear=2013&irbShowFootnotes=Show&iclIndicators_rdExpandedCollapsedHistory=&iclIndicators=_RFSMOK3&hidPreviouslySelectedIndicators=&DashboardColumnCount=2&rdShowElementHistory=&rdScrollX=0&rdScrollY=0&rdRnd=8722.
- 11.Butler D, Aboelata M, Cohen L, et al. Advancing Health Equity in Tobacco Control: California Health Equity Summit Proceedings. California Health Equity Summit; Sacramento, California. 2013. [Google Scholar]
- 12.Cokkinides VE, Ward E, Jemal A, et al. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med. 2005;28:119–122. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Ku L, Bruen BK, Steinmetz E, et al. Medicaid tobacco cessation: big gaps remain in efforts to get smokers to quit. Health Aff (Millwood) 2016;35:62–70. doi: 10.1377/hlthaff.2015.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singleterry J, Jump Z, DiGiulio A, et al. State Medicaid coverage for tobacco cessation treatments and barriers to coverage - United States, 2014–2015. MMWR Morb Mortal Wkly Rep. 2015;64:1194–1199. doi: 10.15585/mmwr.mm6442a3. [DOI] [PubMed] [Google Scholar]
- 15.McMenamin SB, Halpin HA, Bellows NM. Knowledge of Medicaid coverage and effectiveness of smoking treatments. Am J Prev Med. 2006;31:369–374. doi: 10.1016/j.amepre.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 16.Kaiser Permanente. Fast facts about Kaiser Permanente. [Accessed June 24, 2016];Kaiser Permanente Share. 2011 Available at: http://xnet.kp.org/newscenter/aboutkp/fastfacts.html.
- 17.Terhune C. Report: Kaiser tops state health insurance market with 40% share. [Accessed August 16, 2016];Los Angeles Times. 2013 Jan 29; Available at: http://articles.latimes.com/2013/jan/29/business/la-fi-mo-health-insure-market-20130129.
- 18.Goldstein A, Gee S, Mirkin R. Tobacco dependence program: a multifaceted systems approach to reducing tobacco use among kaiser permanente members in northern california. Perm J. 2005;9:9–18. doi: 10.7812/tpp/04-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selby JV, Smith DH, Johnson ES, et al. Kaiser Permanente Medical Care Program. In: Strom BL, editor. Pharmacoepidemiology. New York: Wiley; 2005. pp. 241–259. [Google Scholar]
- 20.Parthasarathy S, Campbell CI. High-deductible health plans: implications for substance use treatment. Health Serv Res. 2016;51:1939–1959. doi: 10.1111/1475-6773.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young-Wolff KC, Kline-Simon AH, Das S, et al. Smoking trends among adults with behavioral health conditions in integrated healthcare: a retrospective cohort study. Psychiatric Services. 2016;67:996–1003. doi: 10.1176/appi.ps.201500337. [DOI] [PubMed] [Google Scholar]
- 22.Levinson AH, Perez-Stable EJ, Espinoza P, et al. Latinos report less use of pharmaceutical aids when trying to quit smoking. Am J Prev Med. 2004;26:105–111. doi: 10.1016/j.amepre.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Levinson AH, Borrayo EA, Espinoza P, et al. An exploration of Latino smokers and the use of pharmaceutical aids. Am J Prev Med. 2006;31:167–171. doi: 10.1016/j.amepre.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 24.Rabius V, McAlister AL, Geiger A, et al. Telephone counseling increases cessation rates among young adult smokers. Health Psychol. 2004;23:539–541. doi: 10.1037/0278-6133.23.5.539. [DOI] [PubMed] [Google Scholar]
- 25.Murphy JM, Mahoney MC, Hyland AJ, et al. Disparity in the use of smoking cessation pharmacotherapy among Medicaid and general population smokers. J Public Health Manag Pract. 2005;11:341–345. doi: 10.1097/00124784-200507000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Fertig AR, Carlin CS, Long SK. The first insurance claim of new ACA enrollees. Research BriefAugust. 2015:1–2. [Google Scholar]
- 27.United States Department of Labor. [Accessed June 24, 2016];FAQs about Affordable Care Act implementation (Part XIX) 2014 May 2; Available at: http://www.dol.gov/ebsa/faqs/faq-aca19.html.
- 28.Joszt L. Exchange enrollees more cost conscious but less satisfied with plans. [Accessed June 25, 2016];AJMCcom. 2015 Aug 21; Available at: http://www.ajmc.com/newsroom/exchange-enrollees-more-cost-conscious-but-less-satisfied-with-plans.
- 29.Fu SS, Sherman SE, Yano EM, et al. Ethnic disparities in the use of nicotine replacement therapy for smoking cessation in an equal access health care system. American journal of health promotion : AJHP. 2005;20:108–116. doi: 10.4278/0890-1171-20.2.108. [DOI] [PubMed] [Google Scholar]
- 30.Cokkinides VE, Halpern MT, Barbeau EM, et al. Racial and ethnic disparities in smoking-cessation interventions: analysis of the 2005 National Health Interview Survey. American journal of preventive medicine. 2008;34:404–412. doi: 10.1016/j.amepre.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Schmittdiel JA, Karter AJ, Dyer WT, et al. Safety and effectiveness of mail order pharmacy use in diabetes. Am J Manag Care. 2013;19:882–887. [PMC free article] [PubMed] [Google Scholar]
- 32.Medi-Cal members. [Accessed June 25, 2016];The California Smokers’ Helpline. 2015 Available at: http://www.nobutts.org/tobacco-users-medi-cal-members.
- 33.Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights. 2015;8:1–35. doi: 10.4137/TUI.S15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Current cigarette smoking prevalence among working adults--United States, 2004–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1305–1309. [PubMed] [Google Scholar]
- 35.Danan ER, Joseph AM, Sherman SE, et al. Does motivation matter? Analysis of a randomized trial of proactive outreach to VA smokers. J Gen Intern Med. 2016;31:878–887. doi: 10.1007/s11606-016-3687-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.