Abstract
Objectives
To report the complications occurring following TORS and to identify the factors predictive of complications.
Methods
Following IRB approval a retrospective analysis of all TORS operations at our institution was performed. Postoperative complications within 45 days were collected and graded with the Clavien-Dindo system. Complications were categorized into groups: all complications, not related to TORS and TORS related. Unadjusted odds ratios were calculated to test association between patients with and without a complication.
Results
122 TORS operations were carried out between June 2010 and August 2015. 77% were male, with a median age of 57. There were 92 primary tumor resections, 10 second head and neck primary resections, 13 salvage procedures and 7 other indications. Surgical resection involved 1, 2 or >3 sub-sites in 36%, 28% and 36% patients, respectively.
Overall, there were 107 complications (66 TORS related, 41 non-TORS related) that occurred in 57 patients (47%). A major complication occurred in 23 patients (18%). 19 patients had a TORS related major complication and 6 patients experienced a non-TORS related major complication. There was a temporal trend in TORS related major complication rate decreasing from 33% in 2010 to 10% in 2015.
Statistical analysis showed that the odds of having any complication were 3 times greater in patients over 60 years old (p=0.017), and 2.5 times greater when there were more than 2 subsites resected (p=0.022).
Conclusions
Age over 60 years and a larger extent of resection were the significant factors predictive of major complications.
Keywords: Trans oral robotic surgery, complications, postoperative care, oropharyngeal cancer
Introduction
Since FDA approval of transoral robotic surgery (TORS), the publication of TORS related complications has not equaled reports of oncological outcomes. It is important to know the incidence and severity of complications associated with TORS when counseling patients regarding modality of treatment especially when nonsurgical treatment options are available. The introduction of the da Vinci robot (Intuitive Surgical Inc, Sunnyvale, CA, USA) was initially developed in urology and cardiac surgical specialties. The first reported use of the da Vinci robot in Head and Neck surgery was by Melder et al, in which a resection of a vallecular cyst was performed in 2005(1). The first application for a head and neck malignancy was reported by Weinstein et al at the University of Pennsylvania in 2006(2). This group is responsible for the majority of early research and coined the term TORS (Trans Oral Robotic Surgery). Since then, FDA approval for the use in the head and neck was granted in 2009 and TORS has been adopted throughout the world.
TORS has emerged as a transoral approach that offers an alternative to open surgery and primary non-surgical treatments(3). The advantages of TORS are the ability to operate without line of site restrictions that limits other trans oral endoscopic or microscopic approaches. It also allows resection of tumors that would traditionally require a pharyngotomy or mandibulotomy. Other advantages of this technology include instruments with six degrees of freedom, motion scaling, instrument stabilization and tremor reduction(4). The binocular and magnified endoscopic vision also allows for accurate 3 dimensional visualization.
TORS has been shown to achieve excellent oncological results across a number of indications and subsite but these are mostly from single institutional studies and in the oropharynx(5, 6). There have also been promising functional outcomes of TORS with appropriate adjuvant therapy(7). A multi-institutional study has recently reported a 3 year survival rate of 92.5% and a 3 year recurrence rate of 88.8% (8).
In contrast to the number of case series reporting outcomes, there are few studies showing detailed analysis of complications. The understanding of complications is important because patients who are suitable for TORS are also good candidates for primary non-surgical treatment and other surgical approaches. To fully inform patients and treating physicians, we aim to report detailed institutional complication rates, types of complications and identify potential predictive factors.
Methods
Patient cohort
Memorial Sloan Kettering Cancer Center institutional review board approval was granted for a retrospective study of all TORS procedures at our institution. All patients receiving a TORS operation were included. Procedures were performed between June 2010 and August 2015. The TORS procedures were carried out by 4 surgeons who had all received adequate training and proctorship.
Data collection
Patients were identified through the institutional operation room database using CPT codes indicating robotic surgery. The patient record was accessed to record demographics, clinical characteristics, health behaviors, oncologic characteristics, surgical details, outcomes and complications. Staging was recorded according to the American Joint Committee on Cancer Staging Manual 7th Edition(9). Patient data was stored on an institutional network using the oncological database software, Caisis (Biodigital), with access available only to authors.
Complications reporting and analysis
Post-operative complications were defined using the Dindo and Clavien definition, “any deviation from the normal post-operative course”(10). The process of identification and recording of complications was as described by previous work at our institution(11, 12). All events that occurred in the patient’s record within 45 days of surgery, either in medical, nursing, anesthetic or allied health professional documentation was compared to the definition of a post-operative complication. Complications were graded according to the “Clavien-Dindo Classification of Surgical Complication” (13). A summary of the grading system is shown in Table 1. For analysis, the severity of complications was further summarized as major (grades 3, 4 and 5) and minor (grades 1 and 2).
Table 1.
Clavien Dindo classification
| Clavien Dindo classification | |
|---|---|
| Grades | Definition |
| Grade I: | Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions. |
| Allowed therapeutic regimens are: drugs as antiemetics, antipyretics, analgetics, diuretics and electrolytes and physiotherapy. This grade also includes wound infections opened at the bedside. | |
| Grade II: | Requiring pharmacological treatment with drugs other than such allowed for grade I complications. Blood transfusions and total parenteral nutrition are also included. |
| Grade III: | Requiring surgical, endoscopic or radiological intervention |
| Grade III-a: | intervention not under general anesthesia |
| Grade III-b: | intervention under general anesthesia |
| Grade IV: | Life-threatening complication (including CNS complications)‡ requiring IC/ICU-management |
| Grade IV-a: | single organ dysfunction (including dialysis) |
| Grade IV-b: | multi organ dysfunction |
| Grade V: | Death of a patient |
| Suffix ‘d’: | If the patients suffers from a complication at the time of discharge the suffix “d” (for ‘disability’) is added to the respective grade of complication. This label indicates the need for a follow-up to fully evaluate the complication. |
Complications were also grouped into domains, previously generated from the large study of post-operative complications in oral cancer(12). This included complications local to surgery, either in the neck (cranial nerve paresis, infection, hematoma, wound breakdown/dehiscence, lymphatic leak, seroma), related to the oropharynx (wound breakdown/dehiscence, hemorrhage, necrosis, infection, burn/trauma and hematoma), in the head and neck (trismus, fistula, orbital complication, hoarseness/stridor, salivary gland infection, epistaxis and TMJ dislocation), resulting from a feeding tube (cellulitis, bowel perforation/necrosis, upper gastrointestinal bleeding, wound breakdown/dehiscence) and from tracheostomy (hemorrhage, fistula, subcutaneous emphysema, displacement).
Systemic complications were grouped into the following domains; pulmonary (pneumonia, pulmonary edema, foreign body, atelectasis, respiratory failure), nervous system (delirium, cerebrovascular accident), cardiac (congestive heart failure, myocardial infarction, atrial fibrillation), hematologic (venothromboembolism, coagulopathy) and infection (catheter, systemic). Long term complications were recorded (tracheostomy, feeding tube, nutritional supplement, trismus, oral intake, aesthetic concerns, mobility, weight loss, osteoradionecrosis, pharyngeal stricture, speech and velopharyngeal insufficiency).
Complications related to local effects of surgery were classified as a TORS related complications and complications unrelated to local effects of surgery were classified as non TORS related complications, see Table 2.
Table 2.
TORS and non TORS complications groups
| TORS related complications: | Non-TORS related complications: |
|---|---|
| Bleeding | Infections outside of oropharynx |
| Dysphagia | Tube and line complications |
| Local oropharyngeal | Cardiopulmonary |
| Aspiration related infections | Haematological |
| Local pain | Others |
Statistical analysis
Unadjusted odds ratios of clinical and pathologic factors predictive of complications were calculated. Multivariable analysis was not possible because the number of events in the major categories would not support a robust model. Statistical analysis was performed using SPSS (IBM Company Headquarters, Chicago, IL, USA).
Results
Patient, tumor and treatment characteristics (Table 3)
Table 3.
Patient demographics, comorbidities and treatment
| Variable | No. patients | % | |
|---|---|---|---|
| Sex | Male | 93 | 76.2 |
| Female | 29 | 23.8 | |
| Age | ≤60 yrs old | 75 | 61.5 |
| >60 yrs old | 47 | 38.5 | |
| Tobacco | Never to less than 1 yr | 52 | 42.6 |
| 1–9.9 yrs | 16 | 13.1 | |
| 10–19.9 yrs | 16 | 13.1 | |
| ≥ 20 yrs | 37 | 30.3 | |
| Unknown | 1 | ||
| Never | 51 | 41.8 | |
| Ever | 71 | 58.2 | |
| Alcohol | Never, occasional, discontinued use | 44 | 35.8 |
| 1–12 drinks per month | 38 | 30.9 | |
| 13–29 drinks per month | 19 | 15.4 | |
| >30 drinks per month | 19 | 15.4 | |
| Unknown | 2 | 1.6 | |
| Never | 25 | 20.5 | |
| Ever | 91 | 79.5 | |
| Previous Malignancy | No | 87 | 71.3 |
| Head and Neck | 11 | 9.0 | |
| Other | 24 | 19.7 | |
| ASA Grades | 1 | 1 | 0.8 |
| 2 | 32 | 26.2 | |
| 3 | 83 | 68.0 | |
| 4 | 6 | 4.9 | |
| Indication | Benign | 3 | 2.4 |
| Primary | 92 | 75.4 | |
| Secondary | 10 | 8.2 | |
| Relapse | 13 | 10.7 | |
| Revision | 4 | 3.3 | |
| Tumor sites | Base of tongue | 52 | 42.6 |
| Hard Palate | 1 | 0.8 | |
| Larynx | 2 | 1.6 | |
| Nasopharynx | 1 | 0.8 | |
| Parapharyngeal | 5 | 4.1 | |
| Posterior pharyngeal wall | 2 | 1.6 | |
| Soft Palate | 1 | 0.8 | |
| Tongue | 2 | 1.6 | |
| Tonsil | 56 | 45.9 | |
| Pathology | Squamous Cell Carcinoma | 106 | 86.9 |
| Salivary | 8 | 6.6 | |
| Thyroid | 4 | 3.3 | |
| Other | 4 | 3.3 | |
| Subsites resected | 1 Subsite | 44 | 36.0 |
| 2 Subsites | 34 | 27.9 | |
| More than 2 subsites | 44 | 36.0 | |
| Neck dissection type | No Neck dissection | 28 | 23.0 |
| Modified Radical Neck Dissection | 11 | 9.0 | |
| Selective Neck dissection | 65 | 53.3 | |
| Cervical Biopsy | 18 | 14.8 |
Between June 2010 and August 2015 there were 122 procedures that met the inclusion criteria. The majority of patients were male (93, 76.2%) with 47 (38.5%) being over 60 years old. The majority of procedures were indicated for the treatment of a primary tumor in 92 (75.4%), for a head and neck second malignancy in 10 (8.2%), for recurrent disease in 13 (10.7%), for revision in 4 (3.3%) and as a diagnostic procedure in 3 (2.4%) cases.
Tumors were most commonly located in the oropharynx, with 52 (42.6%) in the base of tongue, 56 (45.9%) in the tonsil and 1 (0.8%) in the soft palate. This cohort of TORS patients also includes resections from other subsites such as 2 (1.6%) laryngeal resections, 1 (0.8%) nasopharyngeal and 5 (4.1%) resections from the parapharyngeal space. Squamous cell carcinoma was the most common histological diagnosis, accounting for 106 (86.9%) of patients. Salivary gland cancers, thyroid metastasis and other diagnoses were seen in 8 (6.6%), 4 (3.3%) and 4 (3.3%) cases respectively. Immunohistochemical staining for p16 was positive in 81 cases (66.4%).
94 (77%) patients undergoing a TORS procedure received a neck dissection.
There were 11 (9%) modified radical neck dissections and 65 (53.3%) selective neck dissections performed. The size of surgical resection was recorded based on the number of subsites resected. A procedure with more subsites resected demonstrates a more complex resection with higher likelihood of exposing neurovascular structures and a larger defect. There were 44 (36%) resections involving a single subsite, 34 (27.9%) involving 2 subsites and 44 (36%) involving more than 2 subsites.
71 (58.2%) had a smoking history with 43.4% having more than 10 pack-years. Alcohol use was reported in 79.5% of patients, with 15.4% drinking more than 30 units a month. The American Society of Anesthesiology (ASA) physical status classification system(14) was used to grade patients pre-operatively and 33 (27%) were graded either 1 or 2 and 89 (73%) were graded 3 or 4.
Complications
57 patients (47%) experienced a complication following TORS. 19 patients (16%) experienced both a TORS related and non-TORS related complication. In total, there were 107 complications of all grades reported (66 were TORS related and 41 non-TORS related). 43 patients (35%) had a TORS related complication and 32 (26%) experienced a non-TORS related complication. The number of major complications, those requiring invasive intervention to correct the complication, is of more interest in understanding the morbidity of this procedure. A major complication occurred in 23 patients (19%). 19 patients (16%) had a major complication that was TORS related and 6 patients (4.9%) experienced a non-TORS related major complication. 2 patients (1.6%) had both a TORS related and non-TORS related major complication.
Trends in post-operative TORS complications
The temporal trends in complications are described in Figures 1 and 2. In the initial year of TORS surgery there was a relatively high incidence of complications, with up to 56% of patients receiving a complication of any grade in 2010. There was a 33% incidence of major complications (grade 3,4,5) in 2010. As experience with this technique improved the incidence of major complications reduced. In years 2013, 2014 and 2015 there was an incidence of major complications of 16%, 16% and 15%. Major TORS related complications (grades 3,4,5) also showed a downward trend with increasing experience (Figure 2). Initially 33% of patients experienced a TORS related major complication but by 2015 this decreased to 10%.
Figure 1.
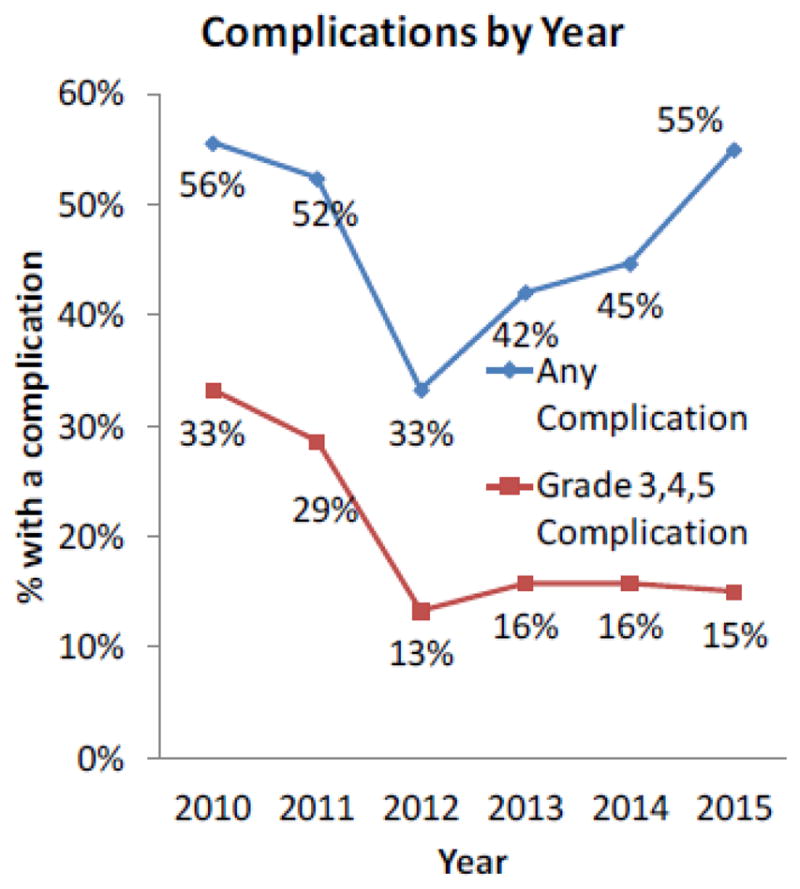
Percentage of patients experiencing complication by year of surgery. Complications of any grade and complications of grade 3,4 and 5 are reported.
Figure 2.
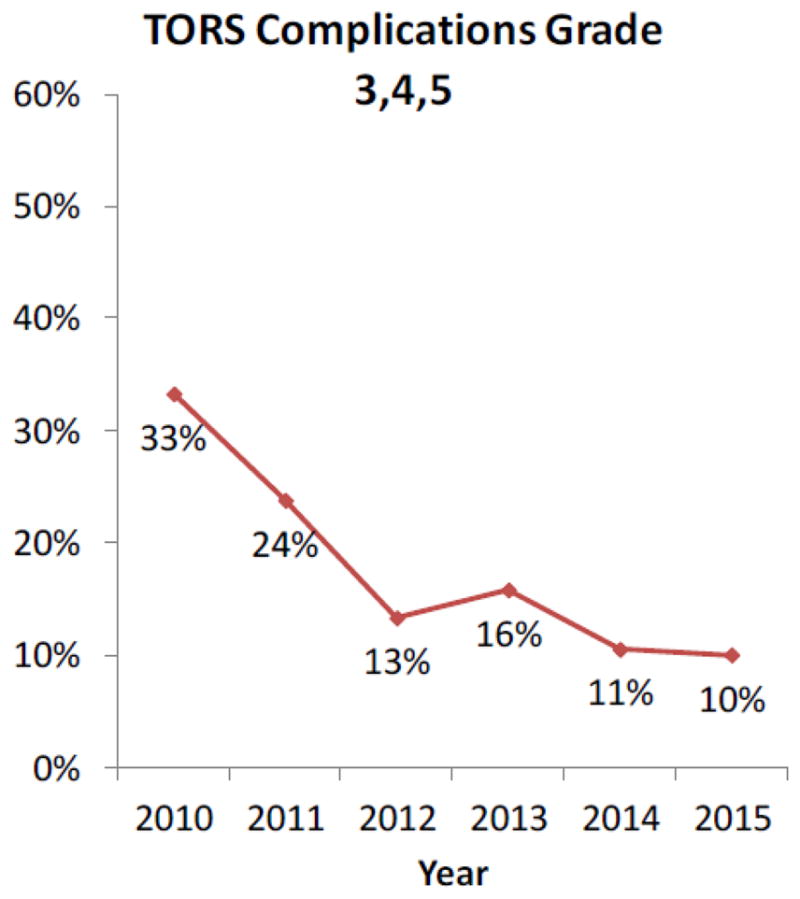
Percentage of patients experiencing complication by year of surgery.
Complications of grade 3,4 and 5 related specifically to TORS technique are reported.
Details of Major Complications
There was 1 post-operative death (grade 5 complication) due to severe congestive cardiac failure. 7 patients had a complication requiring intensive care treatment (grade 4) of which 6 were TORS related (3 cases of aspiration with respiratory compromise and 3 hemorrhages) and 1 non-TORS related (neck infection following neck dissection). Grade 3 complications occurred in 21 patients of which 16 were TORS related (12 swallowing related complications with 1 stricture dilation and 11 gastrostomy insertions, 3 hemorrhages and 1 temporary tracheostomy for emergency airway protection) and 5 non-TORS related complications (3 neck wound hematomas, 1 tracheostomy related complication and 1 post-operative cardiac event). Isolated aspiration events occurred in 3 patients on day 5 (range 4–8) after the TORS procedure. Oral feeding had only been commenced in one patient before the aspiration event.
Factors predictive of all major complications, TORS related major complications and non TORS related major complications are seen in Table 4.
Table 4.
Predictive factors with different groups of complications (All major complications, TORS related major complications and non TORS related major complications). (OR Odds ratio, ASA American association of Anesthesiologists)
| Variable | Overall complications > grade 3 | Unadjusted OR | p value | Non TORS related complications > grade 3 | Unadjusted OR | p value | TORS related complications > grade 3 | Unadjusted OR | p value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age> 60 | >60 | 14/47 | 3.11 (1.22–7.93) | 0.017 | 2/47 | 0.79 (0.14–4.49) | 0.789 | 12/47 | 3.33 (1.20–9.21) | 0.021 |
| <60 | 9/75 | Reference | 4/75 | Reference | 7/75 | Reference | ||||
| Tobacco | Y | 14/71 | 1.15 (0.45–2.90) | 0.773 | 4/71 | 1.46 (0.26–8.31) | 0.668 | 11/71 | 0.99 (0.37–2.66) | 0.977 |
| N | 9/51 | Reference | 2/51 | Reference | 8/51 | Reference | ||||
| Previous cancer | Y | 7/35 | 1.11 (0.41–2.99) | 0.837 | 1/35 | 0.48 (0.05–4.28) | 0.513 | 6/35 | 1.18 (0.41–3.39) | 0.762 |
| N | 16/87 | Reference | 5/87 | Reference | 13/87 | Reference | ||||
| Any Comorbidity | Y | 22/98 | 6.66 (0.85–52.11) | 0.071 | 5/98 | 1.24 (0.14–11.10) | 0.850 | 18/98 | 5.17 (0.66–40.86) | 0.119 |
| N | 1/24 | Reference | 1/24 | Reference | 1/24 | Reference | ||||
| Subsite | Tonsil | 10/56 | 0.81 (0.31–2.10) | 0.817 | 5/56 | 5.00 (0.56–44.31) | 0.340 | 7/56 | 0.60 (0.21–1.71) | 0.626 |
| Base of Tongue | 11/52 | Reference | 1/52 | Reference | 10/52 | Reference | ||||
| Other | 2/14 | 0.62 (0.12–3.20) | 0/14 | 0.006 (0.00–5×1018) | 2/14 | 0.70 (0.13–3.64) | ||||
| ASA | 1,2 | 9/34 | Reference | 0.105 | 0/34 | Reference | 0.563 | 2/33 | Reference | 0.095 |
| 3,4 | 14/85 | 2.90 (0.80–10.50) | 6/85 | 1.90 (0.21–16.94) | 17/89 | 3.66 (0.80–16.81) | ||||
| Neck Dissection | Y | 17/94 | 0.81 (0.28–2.30) | 0.692 | 6/94 | 1566 (0.0–3×1027) | 0.797 | 13/94 | 0.59 (0.20–1.73) | 0.334 |
| N | 6/28 | Reference | 0/28 | Reference | 6/28 | Reference | ||||
| Extent of surgery | 1 | 7/44 | Reference | 0.022 | 3/44 | Reference | 0.96 | 5/44 | Reference | 0.034 |
| 2 | 2/34 | 0.33 (0.06–1.71) | 0/34 | 0 (0–8×1018) | 2/34 | 0.49 (0.09–2.68) | ||||
| >3 | 14/44 | 2.47 (0.88–6.89) | 3/44 | 1.00 (0.19–5.25) | 12/44 | 2.93 (0.93–9.18) |
Pre-operative and operative factors were assessed and unadjusted odds ratios were calculated for each variable. Because of the small number of major complication events, multivariate analysis was not possible. Patient factors that were investigated were age (grouped as 60 and under and more than 60 years old), history of smoking, previous alcohol usage, ASA and a significant comorbidity. Surgical and tumor factors considered were tumor subsite, neck dissection and the extent of surgical resection.
For all complications, age over 60 years and a larger surgical resection involving 2 or more subsites had a higher odds of complications, p=0.015 and p=0.012 respectively. The odds of having a complication were 3 times greater for patients over 60 years. And, the odds of having a complication were 2.5 times greater for patients with more than 2 subsites resected.
Age over 60 and surgical resection of 2 or more subsites were associated with a TORS related major complication, p=0.016 and p=0.022 respectively. The odds of having a TORS related major complication were 3.3 times greater in patients older than 60 years compared to patients 60 or younger. Similarly, the odds of having a TORS related major complication was 3 times greater for patients with more than 2 subsites resected. No factors were associated with a non-TORS related major complication (Table 4).
Details of Minor Complications
There were 73 minor complications (grade 1 and grade 2) of which 39 were classified as related directly to TORS. 34 minor complications were considered non TORS related. The most common minor complication was hemorrhage, occurring 14 times. These were events that did not require any medical intervention. Other complications include nasogastric tube problems (4 events), swallowing complications causing a delay of diet resumption (5 events) and pain (11 events). A summary of complications by grade and type can be seen in Table 5.
Table 5.
Summary of complications by grade, type and group
| Number of complications | |||||
|---|---|---|---|---|---|
| Complications groups | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 |
| TORS Related complications | |||||
| Bleeding | 14 | 3 | 7 | ||
| Dysphagia | 3 | 2 | 12 | ||
| Local Oropharynx | 3 | 1 | 1 | ||
| Pneumonia/Aspiration | 2 | 3 | 3 | 1 | |
| Local Pain | 9 | 2 | |||
| Non TORS related complications | |||||
| Infections outside of oropharynx | 8 | 2 | 1 | ||
| Neck Complication | 2 | 3 | |||
| Tube and line complications | 3 | 2 | 1 | ||
| Cardiopulmonary | 2 | 3 | 1 | 1 | |
| Hematologic complications | 1 | 1 | |||
| Other (Nervous system/pain) | 5 | 5 | |||
The incidence of all grades of complications were also analyzed for predictive factors. The results can be seen in Table 6. The odds of having a minor complication were 2.7 times greater in patients older than 60 years. This was true for all complications, p=0.010, and for non TORS related complications, p=0.018, but not for TORS related complication, p=0.119. There were no other statistically significant factors predictive of all grades of complications.
Table 6.
Predictive factors with all grades of complications (All complications, TORS related all complications and non TORS related all complications). (OR Odds ratio, ASA American association of Anesthesiologists)
| Variable | Overall complications Any grade | Unadjusted OR | p value | Non TORS related complications Any grade | Unadjusted OR | p value | TORS related complications Any grade | Unadjusted OR | p value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age> 60 | >60 | 28/47 | 2.70 (1.28–5.73) | 0.010 | 18/47 | 2.70 (1.18–6.18) | 0.018 | 21/47 | 1.83 (0.86–3.89) | 0.119 |
| <60 | 28/75 | Reference | 14/75 | Reference | 23/75 | Reference | ||||
| Tobacco | Y | 33/71 | 0.98 (0.48–2.01) | 0.950 | 18/71 | 0.90 (0.40–2.03) | 0.795 | 24/71 | 0.79 (0.38–1.67) | 0.539 |
| N | 24/51 | Reference | 14/51 | Reference | 20/51 | Reference | ||||
| Previous cancer | Y | 17/35 | 1.11 (0.51–2.43) | 0.795 | 13/35 | 2.11 (0.90–4.97) | 0.086 | 12/35 | 0.90 (0.39–2.04) | 0.795 |
| N | 40/87 | Reference | 19/87 | Reference | 32/87 | Reference | ||||
| Any Comorbidity | Y | 49/98 | 2.00 (0.78–5.10) | 0.147 | 29/98 | 2.94 (0.81–10.64) | 0.100 | 37/98 | 1.47 (0.56–3.89) | 0.434 |
| N | 8/24 | Reference | 3/24 | Reference | 7/24 | Reference | ||||
| Subsite | Tonsil | 25/56 | 0.87 (0.41–1.86) | 0.907 | 14/56 | 0.90 (0.38–2.14) | 0.953 | 21/56 | 1.04 (0.48–2.28) | 0.822 |
| Base of Tongue | 25/52 | Reference | 4/14 | Reference | 4/14 | Reference | ||||
| Other | 7/14 | 1.08 (0.33–3.52) | 14/52 | 1.09 (0.29–4.03) | 19/52 | 0.69 (0.19–2.52) | ||||
| ASA | 1,2 | 12/33 | Reference | 0.165 | 6/33 | Reference | 0.223 | 9/33 | Reference | 0.221 |
| 3,4 | 45/89 | 1.79 (0..79–4.07) | 26/89 | 1.86 (0.69–5.03) | 35/89 | 1.73 (0.72–4.15) | ||||
| Neck Dissection | Y | 46/94 | 1.48 (0.63–3.50) | 0.370 | 28/94 | 2.55 (0.81–8.02) | 0.110 | 34/94 | 1.02 (0.42–2.46) | 0.965 |
| N | 111/28 | Reference | 4/27 | Reference | 10/28 | Reference | ||||
| Extent of surgery | 1 | 22/44 | Reference | 0.136 | 13/44 | Reference | 0.661 | 16/44 | Reference | 0.053 |
| 2 | 11/34 | 0.48 (0.19–1.21) | 7/34 | 0.62 (0.22–1.77) | 7/34 | 0.45 (0.16–1.28) | ||||
| >3 | 22/44 | 1.2 (0.52–2.77) | 12/44 | 0.89 (0.35–2.26) | 21/44 | 1.60 (0.68–3.75) |
Discussion
Robotic surgery is an emerging technology that is gaining support and wider application in head and neck surgery. There are numerous publications on the indications, techniques and outcomes(7, 8, 15). However, complications following surgery have not been thoroughly examined. This study was conducted to identify complications post-operatively after TORS surgery. Understanding complications and investigating predictive factors is an important aspect of the counselling and decision making process in any surgical procedure. This has become of increased importance in head and neck surgery because a common indication for TORS is local advanced oropharyngeal cancer. As the demographics of this disease are changing, with the emergence of HPV driven cancers, the traditional treatment approaches are being questioned(16) and new strategies and techniques are being examined. Accurate information on outcomes and complications is therefore of importance in balancing these decisions.
In this study the Clavien-Dindo grading system was used to allow comparison to other treatment approaches and studies. We found that 18% (23/121) of patients experienced a Clavien-Dindo grade 3, 4 or 5 complication after TORS. There was 1 post-operative death, attributable to a pre-existing comorbid condition and not specific to the surgical procedure or technique. Most of the major complications (Grades 3, 4 and 5) were attributable to the local effects of the surgical procedure. The majority of minor complications were also related to local effects of the surgical procedure. We analysed the complication rate of TORS related major complications over time and report a reduction from 33% in 2010 to 10% in 2015. This temporal trend is reflective of a learning curve with a reduction in major complications with improvements of surgical technique.
Comparing to other studies, a multi-center study of 177 TORS cases reported no intraoperative or perioperative fatalities(3). There was a 16 % rate of serious complications (readmission/intervention), comparable to the 18% major complication rate seen in our study. An analysis of the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) was performed to assess the safety of TORS for oropharyngeal malignancies(17). A complication rate of 7.9% is reported with 2 post-operative deaths in this cohort of 305 patients. The NASQIP collects a predefined set of complications and this study focuses on oropharyngeal malignancies which may account for the small differences seen in complications rates. A single site study from Australia reporting outcomes in 35 patients undergoing TORS and describes 2 patients receiving a major post-operative complication(18). These were bleeding and pulmonary embolism. This study highlights the difficult in complications reporting, as post-operative gastrostomies were required in 11.4% of patients. In our study these were classified as a complication, as return to oral diet was expected. Therefore, it is possible to see the definition of a complication varies and can affect reported complication rates. The use of a validated reporting system for complications, such as the Clavien Dindo system can improve the robust reporting of complications(10, 13).
In a multi-center review of 178 patients in France(19), 12 intraoperative complications were observed (6 hemorrhage, 3 pharyngeal fistulas and 3 external surgical conversions). In the postoperative period 33 hemorrhages, 27 aspiration pneumonias, 9 tracheostomies, 2 pharyngocutaneous fistulae, 2 episodes of cervical spondylitis and 2 deaths were reported. If reported using the Clavien-Dindo classification, the incidence of grade 3, 4 and 5 complications would be 49% (87/178). The severity grading of complications is not well described and this may explain the discrepancy between complication rates of this study and ours.
In an electronic survey completed by 45 surgeons in North America concerning their experience of TORS in 2015 procedures, bleeding was the most common complication (n= 62, 3.1%)(20). There were 6 deaths (0.3%) reported within 30 days of TORS, all attributed to postoperative hemorrhage. The risk of post-operative hemorrhage has been identified as a concern following transoral surgery previously and continues to be a serious complication in TORS(21). In our series there were 24 episodes of post-operative hemorrhage with 7 cases (5.7%) requiring an invasive intervention such as return to operating room or embolization. There were no deaths related to hemorrhage in the post-operative period. This compares well to other reported rates of major post-operative hemorrhage, where rates of 9.8%(22), 5.4%(21) and 7.5% (23) have been reported.
Other complications such as dehydration (n = 26, 1.3%), tooth injury (n= 29, 1.4%), percutaneous endoscopic gastrostomy (PEG) dependency at 6 months (n= 21, 1.0%), temporary hypoglossal nerve injury (n = 18, 0.9%) and lingual nerve injury (n = 11, 0.6%) were reported(20). These complications are not comparable as the grade or severity was not indicated.
In non-robotic head and neck procedures a large review of the National Hospital Data Survey database between 1995 and 1997 including 3932 patients(24) looked at patients having operations of the pharynx for malignancy. The major complication rate was 9.3% and a mortality rate of 2.33% was reported(12). In patients receiving chemo-radiation, 43% of patients suffered from a severe toxicity with older age and T stage being important predictive factors of complications(25). A study using the Maryland Health Service Cost Review database examined 1534 non-robotic oropharyngeal cancer operations performed between 1990 and 2009. This showed a wound complication rate of 7.4 % and an in-hospital death rate of 1.0%(26). These are comparable to all the TORS studies discussed and also our findings.
In our study we examined a number of possible predictive factors of complications following TORS. Age over 60 years and a larger extent of surgical resection were the two significant factors predictive of major complications (Grade 3,4 and 5) following TORS in our study. TORS for benign processes such as obstructive sleep apnoea and advanced comorbidity have been shown to affect the time to oral diet resumption and length of stay(27).
In other head and neck surgical studies following non robotic surgery age and the type and extent of surgery have been identified as the important risk factors for morbidity. In a study of 1,201 patients receiving major surgical interventions for head and neck malignancies in the Netherlands, age was the only factor predictive of medical complications. Tumor stage (surrogate for size and extent of surgery) was the only predictive factor of surgical complications on multivariable analysis(28).
This study describes the experience of a large Head and Neck Cancer department with TORS. However, it does have some limitations. This was a retrospective study and it is therefore subject to bias in reporting/documentation of complications. Major complications are more likely to be reported than minor complications. The recording of complications depends on the accurate documentation within the medical record. Complications outside of the hospital network, treated by a different provider might not be captured if the treating hospital is not informed. Patient selection for surgery was determined by discussion between surgeon, oncologist and patient. FDA approval guidelines were also followed, selecting early stage tumors (T1 and T2). This means the data is only generalizable to similar stage tumors. As a new procedure, bias in patient selection for comorbidities, tumor characteristics and other factors is also possible and would not be controlled for in a retrospective study.
Prospective collection of complications information and data would improve the accuracy of this study and similar studies like this. As the current prospective TORS studies, such as ECOG 3311 (16), are completed the data collected during these will offer valuable information on complications and outcomes. New procedures also have a learning curve for the surgeon and this is clearly shown in our study where we report a temporal reduction in TORS related major complications from 2010 to 2015. This data includes the initial experience of TORS. A formal study within a trial setting reporting complications with credentialed surgeons may help standardize treatments.
Conclusion
18% (22/122) of patients experienced a Clavien-Dindo grade 3, 4 or 5 complication after TORS. There was a temporal trend in TORS related major complication rate decreasing from 33% in 2010 to 10% in 2015. This was reflective of a learning curve with a reduction in major complications with improvements of surgical technique. Age over 60 years and a larger extent of surgical resection were the two significant factors predictive of complications following TORS. This study represents the experience of a large Head and Neck service specifically recording all complications and analyzing for predictive factors to help inform decision making.
Highlights.
122 TORS operations were carried out between June 2010 and August 2015
A major complication occurred in 23 patients (18%)
There was a temporal trend in TORS related major complication rate decreasing from 33% in 2010 to 10% in 2015.
Odds of complication were 3 times greater in patients over 60 years old (p=0.017)
Odds of complication were also 2.5 times greater when more than 2 subsites were resected (p=0.022).
Acknowledgments
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748
Footnotes
Disclosures
No conflicts of interest.
Ashley Hay received a travel fellowship grant from The Countess Eleanor Peel Dowager fund to undertake overseas study for a period of one year.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McLeod IK, Melder PC. Da Vinci robot-assisted excision of a vallecular cyst: a case report. Ear Nose Throat J. 2005;84(3):170–2. [PubMed] [Google Scholar]
- 2.Weinstein GS, O’Malley BW, Jr, Snyder W, Sherman E, Quon H. Transoral robotic surgery: radical tonsillectomy. Arch Otolaryngol Head Neck Surg. 2007;133(12):1220–6. doi: 10.1001/archotol.133.12.1220. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein GS, O’Malley BW, Jr, Magnuson JS, Carroll WR, Olsen KD, Daio L, et al. Transoral robotic surgery: a multicenter study to assess feasibility, safety, and surgical margins. Laryngoscope. 2012;122(8):1701–7. doi: 10.1002/lary.23294. [DOI] [PubMed] [Google Scholar]
- 4.Grillone GA, Jalisi S. Robotic surgery of the head and neck: a comprehensive guide. xvii. New York: Springer; 2015. p. 160. illustrations (chiefly colour); 27 cm. p. [Google Scholar]
- 5.de Almeida JR, Byrd JK, Wu R, Stucken CL, Duvvuri U, Goldstein DP, et al. A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review. Laryngoscope. 2014;124(9):2096–102. doi: 10.1002/lary.24712. [DOI] [PubMed] [Google Scholar]
- 6.Kelly K, Johnson-Obaseki S, Lumingu J, Corsten M. Oncologic, functional and surgical outcomes of primary Transoral Robotic Surgery for early squamous cell cancer of the oropharynx: a systematic review. Oral Oncol. 2014;50(8):696–703. doi: 10.1016/j.oraloncology.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Hutcheson KA, Holsinger FC, Kupferman ME, Lewin JS. Functional outcomes after TORS for oropharyngeal cancer: a systematic review. Eur Arch Otorhinolaryngol. 2015;272(2):463–71. doi: 10.1007/s00405-014-2985-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Almeida JR, Li R, Magnuson JS, Smith RV, Moore E, Lawson G, et al. Oncologic Outcomes After Transoral Robotic Surgery: A Multi-institutional Study. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1043–51. doi: 10.1001/jamaoto.2015.1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edge SB American Joint Committee on C. AJCC cancer staging manual. 7. xiv. New York: Springer; 2010. p. 648. ill., port.; 28 cm. + 1 CD-ROM (4 3/4 in.) p. [DOI] [PubMed] [Google Scholar]
- 10.Dindo D, Clavien PA. What is a surgical complication? World J Surg. 2008;32(6):939–41. doi: 10.1007/s00268-008-9584-y. [DOI] [PubMed] [Google Scholar]
- 11.Awad MI, Palmer FL, Kou L, Yu C, Montero PH, Shuman AG, et al. Individualized Risk Estimation for Postoperative Complications After Surgery for Oral Cavity Cancer. JAMA Otolaryngol Head Neck Surg. 2015;141(11):960–8. doi: 10.1001/jamaoto.2015.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Awad MI, Shuman AG, Montero PH, Palmer FL, Shah JP, Patel SG. Accuracy of administrative and clinical registry data in reporting postoperative complications after surgery for oral cavity squamous cell carcinoma. Head Neck. 2015;37(6):851–61. doi: 10.1002/hed.23682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 14.Dripps R. New classification of physical status. Anesthesiol. 1963;24:111. [Google Scholar]
- 15.Sansoni ER, Gross ND. The role of transoral robotic surgery in the management of oropharyngeal squamous cell carcinoma: a current review. Curr Oncol Rep. 2015;17(3):432. doi: 10.1007/s11912-014-0432-y. [DOI] [PubMed] [Google Scholar]
- 16.Byrd JK, Ferris RL. Is There a Role for Robotic Surgery in the Treatment of Head and Neck Cancer? Curr Treat Options Oncol. 2016;17(6):29. doi: 10.1007/s11864-016-0405-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su HK, Ozbek U, Likhterov I, Brant J, Genden EM, Urken ML, et al. Safety of transoral surgery for oropharyngeal malignancies: An analysis of the ACS NSQIP. Laryngoscope. 2016;126(11):2484–91. doi: 10.1002/lary.26024. [DOI] [PubMed] [Google Scholar]
- 18.Hirshoren N, Ruskin O, Fua T, Kleid S, Magarey M, Dixon B. Transoral robotic surgery: implementation as a tool in head and neck surgery - a single-centre Australian experience. ANZ J Surg. 2016 doi: 10.1111/ans.13801. [DOI] [PubMed] [Google Scholar]
- 19.Aubry K, Vergez S, de Mones E, Moriniere S, Choussy O, Malard O, et al. Morbidity and mortality revue of the French group of transoral robotic surgery: a multicentric study. J Robot Surg. 2016;10(1):63–7. doi: 10.1007/s11701-015-0542-z. [DOI] [PubMed] [Google Scholar]
- 20.Chia SH, Gross ND, Richmon JD. Surgeon experience and complications with Transoral Robotic Surgery (TORS) Otolaryngol Head Neck Surg. 2013;149(6):885–92. doi: 10.1177/0194599813503446. [DOI] [PubMed] [Google Scholar]
- 21.Pollei TR, Hinni ML, Moore EJ, Hayden RE, Olsen KD, Casler JD, et al. Analysis of postoperative bleeding and risk factors in transoral surgery of the oropharynx. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1212–8. doi: 10.1001/jamaoto.2013.5097. [DOI] [PubMed] [Google Scholar]
- 22.Mandal R, Duvvuri U, Ferris RL, Kaffenberger TM, Choby GW, Kim S. Analysis of post-transoral robotic-assisted surgery hemorrhage: Frequency, outcomes, and prevention. Head Neck. 2016;38(Suppl 1):E776–82. doi: 10.1002/hed.24101. [DOI] [PubMed] [Google Scholar]
- 23.Asher SA, White HN, Kejner AE, Rosenthal EL, Carroll WR, Magnuson JS. Hemorrhage after transoral robotic-assisted surgery. Otolaryngol Head Neck Surg. 2013;149(1):112–7. doi: 10.1177/0194599813486254. [DOI] [PubMed] [Google Scholar]
- 24.Bhattacharyya N, Fried MP. Benchmarks for mortality, morbidity, and length of stay for head and neck surgical procedures. Arch Otolaryngol Head Neck Surg. 2001;127(2):127–32. doi: 10.1001/archotol.127.2.127. [DOI] [PubMed] [Google Scholar]
- 25.Machtay M, Moughan J, Trotti A, Garden AS, Weber RS, Cooper JS, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol. 2008;26(21):3582–9. doi: 10.1200/JCO.2007.14.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gourin CG, Forastiere AA, Sanguineti G, Marur S, Koch WM, Bristow RE. Impact of surgeon and hospital volume on short-term outcomes and cost of oropharyngeal cancer surgical care. Laryngoscope. 2011;121(4):746–52. doi: 10.1002/lary.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richmon JD, Feng AL, Yang W, Starmer H, Quon H, Gourin CG. Feasibility of rapid discharge after transoral robotic surgery of the oropharynx. Laryngoscope. 2014;124(11):2518–25. doi: 10.1002/lary.24748. [DOI] [PubMed] [Google Scholar]
- 28.Peters TT, van Dijk BA, Roodenburg JL, van der Laan BF, Halmos GB. Relation between age, comorbidity, and complications in patients undergoing major surgery for head and neck cancer. Ann Surg Oncol. 2014;21(3):963–70. doi: 10.1245/s10434-013-3375-x. [DOI] [PubMed] [Google Scholar]


