Abstract
In this review, we introduce the topic of transgender medicine, aimed at the non-specialist clinician working in the UK. Appropriate terminology is provided alongside practical advice on how to appropriately care for transgender people. We offer a brief theoretical discussion on transgenderism and consider how it relates to broader understandings of both gender and disease. In respect to epidemiology, while it is difficult to assess the exact size of the transgender population in the UK, population surveys suggest a prevalence of between 0.2 and 0.6% in adults, with rates of referrals to gender identity clinics in the UK increasing yearly. We outline the legal framework that protects the rights of transgender people, showing that is not legal for physicians to deny transgender people access to services based on their personal beliefs. Being transgender is often, although not always, associated with gender dysphoria, a potentially disabling condition in which the discordance between a person’s natal sex (that assigned to them at birth) and gender identity results in distress, with high associated rates of self-harm, suicidality and functional impairment. We show that gender reassignment can be a safe and effective treatment for gender dysphoria with counselling, exogenous hormones and surgery being the mainstay of treatment. The role of the general practitioner in the management of transgender patients is discussed and we consider whether hormone therapy should be initiated in primary care in the absence of specialist advice, as is suggested by recent General Medical Council guidance.
Keywords: Transgender, gender identity, gender dysphoria, gender reassignment, transition, primary care, general practitioner
Introduction
Transgender people, whose gender identities, expressions or behaviours differ from those predicted by their sex assigned at birth, are receiving increased attention both in the media and in the scientific press. Recent guidelines in the UK have proposed placing much of the responsibility of care for transgender patients on primary care physicians and their teams.1 With waiting lists for most gender identity clinics extending beyond 12 months and increasing numbers of patients coming forward for treatment, hospital doctors are also likely to encounter transgender patients in their clinical practice.
Research in the area of transgender health is limited, but the emerging consensus is that many people identify as transgender, and that some of these individuals will suffer from an often distressing associated condition, gender dysphoria.2 Appropriate treatment can lead to profound improvements in well-being.2 Treatment is also largely safe and well tolerated but has some risks.2 Transgender individuals may have unique health needs and expectations that health professionals need to be aware of to provide optimal care. In this essay, we introduce and outline this emerging field for physicians, not specialised in this area, aiming largely at a British audience but with relevance to non-specialists outside the UK.
Methods
This was a non-systematic review, utilising Google Scholar and PubMed searches to locate publications deemed to be relevant to the aims of this review, namely to provide a practical introduction to the field of transgender health for the non-specialist clinician. Both our literature search and decisions regarding what was included in the final manuscript were guided by discussions with general practitioners with experience managing transgender patients, gender identity specialists, public health professionals, academics working in the field of transgender studies and transgender patients with experience being treated in the NHS.
Terminology
It is important to know the accepted terminology when discussing gender identity and also to be aware that terms have changed throughout time and will continue to do so. A recent study of 166 medical students in the UK demonstrated a significant positive correlation between familiarity with relevant terminology and positive attitudes towards Lesbian, Gay, Bisexual, Trans, and Queer patients.3 Further studies demonstrate improvement in attitudes towards transgender individuals amongst healthcare professionals after education, suggesting that familiarity with terminology might help overcome negative preconceptions.4 We provide a list of terms derived from the National Centre for Transgender Equality, split based on whether they are preferred at time of writing (Box 1).5
There is an important distinction between transgender and the Disorders of Sex Developmenta (alternatively known as ‘intersex’), which is a term from the Diagnostic and Statistical Manual of Mental Disorders (DSM) 5.a Intersex encompasses a range of conditions where individuals are born with sexual anatomy and/or chromosomal or hormonal patterns not fitting stereotypical definitions of ‘male’ or ‘female’. In general, transgender individuals should be referred to by the pronoun of their current identified gender rather than their assigned gender at birth. If there is any confusion, it is sensible to clarify with a simple question such as ‘which pronouns do you use?’2 The answer may include gender-neutral pronouns such as ‘they’ or ‘ze’ rather than ‘she’ or ‘he’.
What is transgender?
Although frequently conflated, the terms sex and gender have different meanings. Sex is defined as the anatomical, genetic or gonadal dimorphism that typically allows individuals to be placed in one of two categories, ‘male’ or ‘female’. Gender, in contrast, relates to a person’s internal experience of ‘being masculine, feminine or androgynous. Rather than a binary concept, gender identity includes gradations of masculinity to femininity ... as well as identification as neither essentially male nor female’.6 Although related, a person’s sex and gender are distinct from their sexual orientation – whether they are sexually attracted to men, women, both, neither and so on. In the majority of cases, a newborn is assigned as ‘male’ or ‘female’ at birth and a congruent gender identity and gender role of ‘boy’ or ‘girl’ usually forms, respectively. Gender roles are a set of often-stereotyped social and behavioural norms considered appropriate for persons of a specific sex, though these vary widely between and within cultures. Debate continues on the extent to which these gender roles are socially constructed – do typical men and women actually have inbuilt genetic or physiological differences leading to dimorphic sets of behaviours and personalities, or does differing socialisation usually lead to children internalising and ‘performing’ the correct gender roles?
Box 1.
Terms used in the field of transgender health.
| Preferred terms |
| Gender identity: An individual’s internal (i.e. not visible to others) sense of being male, female or something else. |
| Gender non-conforming/Variant: Individual with gender expression differing from societal expectations related to gender. |
| Transgender: Gender identity, expression or behaviour is different to gender assigned at birth. |
| Cisgender: Gender identity, expression and behaviour conform to that assigned at birth. |
| Gender non-binary: Not conforming to either binary gender forms of ‘male’ or ‘female’. |
| Trans (gender) man: Individual most likely assigned as female at birth but now identifies as a man (‘Female to Male’). |
| Trans (gender) woman: Individual most likely assigned male at birth but now identifies as a woman (‘Male to Female’). |
| Gender dysphoria/Gender identity disorder: Terms used in DSM-5 and ICD-10, respectively, describing conditions whereby gender non-conformity leads to distress. |
| Genderqueer: Individual identifies as neither male nor female. The term ‘queer’ might be viewed as derogatory to some but can also be used to describe a political stance which aligns transgender with lesbian, gay and bisexual activism. |
| Transition: Time over which a person begins to live as gender with which they identify rather than their gender assigned at birth. |
| Crossdresser: Individual who dresses in clothing stereotypically worn by the opposite gender but generally without intent to live full time as the other gender. |
| Drag queen: A man who dresses in female clothing, often for the purpose of entertainment or performance. |
| Drag king: A woman who dresses in male clothing, often for the purpose of entertainment or performance. |
| Non-preferred terms |
| Transsexual: Non-preferred term for transgender. |
| Transvestite: Non-preferred term for cross dresser. |
| Drag queen: When used to refer to transgender women, this can be derogatory and should be avoided. |
Individuals whose gender identity and expression differs from their circumscribed categories of ‘male’ and ‘female’ have clearly existed throughout temporal and sociocultural contexts, and within the field of Western medicine, the term ‘transsexual’ or ‘transvestite’ was historically used to describe such individuals. ‘Transgender’ as a noun and later an adjective first gained prominence in the early 1990s, with the rise of transgender studies, which attempted to critically analyse and give a voice to the experiences of a coherent movement of individuals struggling to overcome marginalisation and political injustice.7 In recent years, various theories of gender identity development have been advanced, ranging from ideas about an innate ‘brain sex’ (e.g. the brain of a trans woman might show more homology with that of a natally assigned woman than a natally assigned man)8 to proposals that for at least some transgender people, the desire to become the ‘other’ gender results from a sense of erotic gratification.9 Notions of binary, ‘biological’ sex may also be seen as social constructions.6 What is clear is that gender identity arises from a complex interaction of biological, social and cultural factors and its aetiology is highly contentious area.
Transgender as a ‘disorder’
Complexities in understanding transgender are reflected in the difficulties labelling and classifying it. At present Diagnostic and Statistical Manual-5 and International Classification of Diseases (ICD)-10 include ‘gender dysphoria’ and ‘gender identity disorder’, respectively, under mental health conditions. However, it is likely International Classification of Diseases-11 will reclassify gender identity disorder as a sexual disorder.10 This represents a profound shift in perspective: the transgender person no longer suffers because of pathological mental processes leading to a desire for an altered physical or social identity. The suffering occurs because non-pathological mental processes occur in the context of the ‘wrong’ physical body and a pathological social response to that body.
Gender dysphoria is, by definition, distressing, causing social and occupational dysfunction, is associated with a significant risk of suicide and self-harm11 and can often be treated either medically or surgically. It is for these reasons that it is labelled as a disorder. But for those calling for the ‘depsychopathologisation’ of transgender, gender variance is viewed as a normal dimension of human experience with much of the suffering experienced by transgender people originating from social perspectives.12 For the non-specialist clinician it is worthwhile bearing in mind that it is an area where numerous perspectives are likely to be encountered. As always sensitivity, empathy and respect when dealing with transgender patients is paramount.
Epidemiology
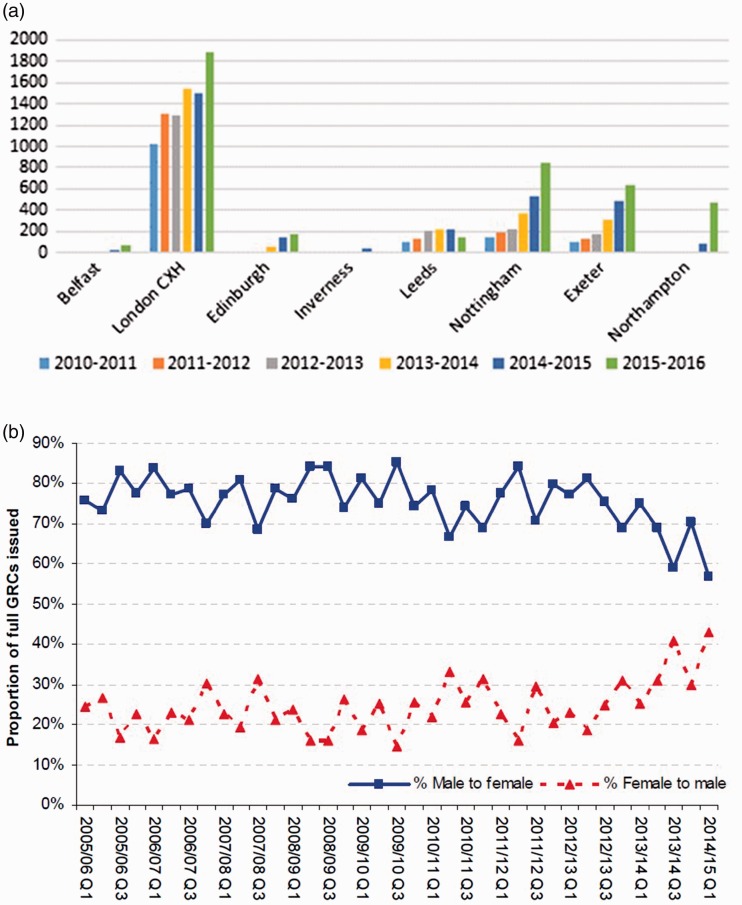
There are only limited data on the prevalence of transgender people. There are also challenges in defining the transgender community. Legally, the transition from one gender to another is formally enshrined through completion of a gender recognition certificate and as of 2014 only 3877 of these certificates had been issued in the UK.13 It is likely however that gender recognition certificate figures grossly underestimate the size of the transgender community in the UK. By the year 2009 it was estimated that between 5000 and 6200 people had undergone gender reassignment surgery in the UK.14 In the past decade, numbers of gender recognition certificate applications have fallen (likely due to cost and a complex administrative process), yet referrals to gender identity clinics have soared15 (Figure 1). In population surveys, estimates of prevalence of transgender in Western populations are higher than might be expected. A survey by Reed et al.14 estimated that 0.2% of the British population in the over-16 age group identify as transgender, although these data did not undergo peer review before publication. In a recent large telephone survey carried out in the Unites States of America, 151,456 respondents were asked ‘do you consider yourself to be transgender?’ A total of 0.53% reported identifying as transgender and, through statistical extrapolation, the authors estimated a population prevalence of 0.6% in the United States (16).
Figure 1.
Epidemiological trends: (a) Bar chart demonstrating increased referral to gender identity clinics across the UK, 2010–2016. The data were compiled as a part of a Guardian special report; data obtained from all gender identity clinics in UK except for Aberdeen under the Freedom of Information Act (15) and (b) government statistics demonstrate an increasing proportion of female to male vs female to male requests for gender recognition certificates between years 2005 and 2014.13
There is pronounced variation in the prevalence of transgender people based on locality. For instance, rates of attendance to gender identity clinics in Sussex per head of the population are double that compared with the rest of the country.2 Whether this is due to differences in attitudes towards transgender individuals, or the effect of patterns of migration remains unclear. Furthermore, while estimates suggest that the median age at which individuals undergo transition is 42 years,14 there has been a large increase in the number of referrals to child and adolescent gender identity clinics in recent years.16 A retrospective study of transgender adults suggests that 76% (92/121) knew that their gender identity differed from their assigned gender by the time they had left primary school.16 In the US telephone survey noted above, a greater proportion of people aged 18–24 were estimated to identify as transgender (0.66%) than those in the 25–64 (0.58%) and the over 65 (0.5%) age brackets.17 It is possible that with increased media discussion of transgender issues, people now feel comfortable to openly identify as transgender at a younger age. It must be noted however that despite positive (Western) media attention, transgender people remain disproportionately at much higher risk of abuse, hate crime, suicide and have a lower average income than non-transgender people.17,18
To address gaps in knowledge, well-conducted epidemiological research into the transgender population is needed. This research would improve the capacity of the NHS to plan services effectively according to need and also aid the transgender community’s campaign for further rights and support. One possibility would be to have information on gender identity incorporated into national statistics, so that gender identity sits alongside race, social class and age as a key measure of population variation.
Legislation
In 2004, the Gender Recognition Act19 was passed in the UK, allowing individuals to be issued with a gender recognition certificate, legalising an individual’s change in gender from the gender they were assigned at birth. In the 2010 Equality Act, ‘gender reassignment’ was designated as a ‘protected characteristic’ and individuals are legally protected against any discrimination and harassment.20 The NHS constitution also supports the right of individuals to seek gender reassignment without discrimination.2 Physicians therefore do not have a legal right to deny transgender people access to services based on their own personal beliefs.
Gender reassignment – treatment options
Gender reassignment involves healthcare professionals from multiple disciplines including primary care, psychology, psychiatry, social services, endocrinology and surgery, according to the wishes of an individual patient. Gender reassignment is safe and effective for most patients but outcome studies are limited by poor follow-up and inadequate study design.1,2 However, not all transgender individuals will desire all, or indeed, any of the available medical and surgical interventions.
The mainstay of pharmacological management is hormone replacement therapy. Until recently, an adult person was required to undergo a period of ‘real life experience’ where they would spend a significant time period (typically three months or more) living as their preferred gender with relevant changes to social, legal and health documents before receiving hormonal therapies.2 During this time, they would ideally receive counselling and psychological support. In the most recent guidelines from the World Professional Association for Transgender Health, which sets global standards of care, a period of real life experience is no longer essential,21 though it remains desirable. All that is required is a letter of support from a gender identity specialist, hence the importance for rapid referral to a gender identity clinic by general practitioner.
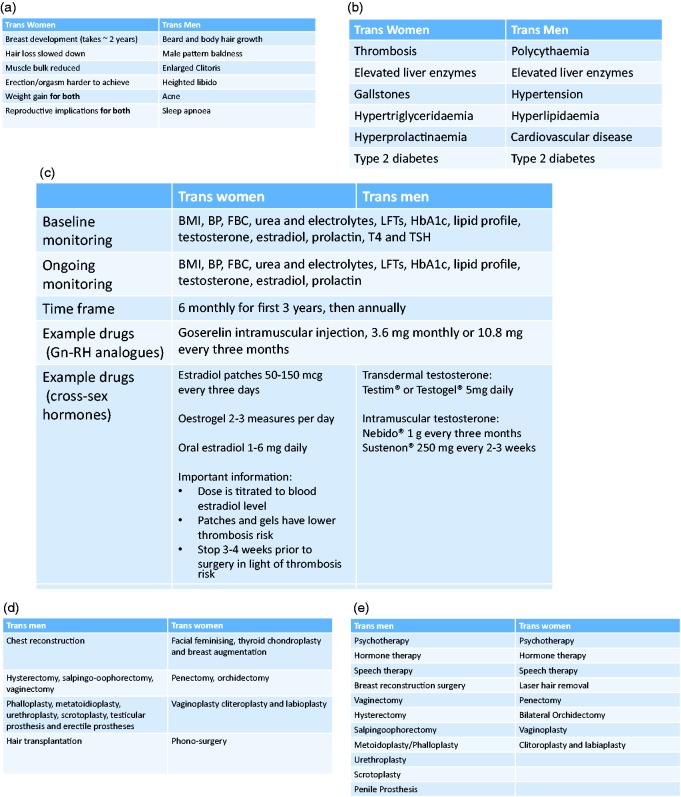
Hormonal therapy in gender reassignment is often referred to as ‘cross-sex hormone therapy’,22 where estrogens are prescribed for trans women and testosterones for trans men. The forms in which these drugs can be prescribed, their effects, risk profiles and necessary monitoring investigations are outlined in Figure 2. In some cases, it might also be necessary to block endogenous sex hormone production with a gonadotropin releasing hormone analogue. The use of a five alpha-reductase inhibitor might also be indicated in trans women to prevent androgenic pattern balding. Current evidence suggests hormone treatments in transgender patients are safe, if correct monitoring is performed and treatment is not associated with either an increased mortality or increased risk of cancer.22–24 Long-term follow-up studies with large cohorts are however lacking24 and should be the focus of future research.
Figure 2.
Boxes demonstrating (a) the effects of cross-sex hormonal medications for trans men and women (whether these are desirable or unwanted will depend on individual patient preference), (b) risks of hormone medications, (c) recommended monitoring if cross-sex hormone medications are prescribed,1,21,25 (d) surgical options for gender reassignment25 and (e) non-surgical and surgical treatment options recommended for funding by the NHS.26
It is not uncommon for transgender patients to self-medicate with unregulated and unlicensed hormonal preparations, often bought online. Uncertainties around contaminants, dosage, quality of medications and lack of monitoring make these potentially harmful. It is important to ascertain how the patient is administering these preparations and enquire about the use of sterile needles and needle sharing if applicable.1 The General Medical Council recommends that self-medication is a reason for general practitioners to initiate hormone therapy without input from a specialist1 (see below).
As a complement to medication, speech and language therapists might be involved and trans women/non-binary patients may also want to undergo facial and body hair removal. Electrolysis is the preferred method due to its permanence. Surgical reassignment procedures are manifold and are summarised in Figure 2(d).25 Many of these surgical procedures form part of the core list of therapies recommended by NHS England for public funding summarised in Figure 2(e).26 Additional surgical interventions, such as breast augmentation or thyroid chondroplasty, are considered on a case-by-case basis by local clinical commissioning groups.26 General practitioners might play a role in supporting applications for surgery (normally two supporting opinions are required). As a number of procedures involve removal of gonadal tissues, collection and freeze storage of gametes prior to any surgery is recommended in some cases.2 In the case of children and adolescents under 16, hormonal and surgical gender reassignment cannot be initiated, but hormone blocking therapy (e.g. gonadotropin releasing hormone analogues) might be used from ages 12 to 16 to stall pubertal changes while a decision is made regarding preferred gender.2 This is likely to be an area of future ethical debate, given the controversy regarding age at which gender identity is determined.27
Gender reassignment – the role of the general practitioner
General Medical Council guidance published in 2016 recommended that general practitioners play a key role in the care of transgender patients.1 This includes counselling or appropriate referral (which can be done directly by general practitioners, without an interim referral to general psychiatry) but also, in some cases, the initiation and maintenance prescription of hormone therapy. If a patient is self-medicating from non-verified sources or is suicidal due to gender dysphoria, the General Medical Council and Royal College of General Practitioners argue that a primary care physician should start cross-sex hormonal therapy as a bridge treatment until the patient is seen in the specialist gender identity clinic,1 with or without additional referral to general psychiatry. The guidance recommends general practitioners should initiate therapy if advised to do so by a specialist, provide maintenance prescriptions and ensure any screening and monitoring blood tests are carried out.1
The British Medical Association’s General Practitioner Committee has raised concerns that the General Medical Council guidelines may force some general practitioners to prescribe beyond their level of competence,28 while others have argued that the guidelines are appropriate given the low-risk profile of the hormone therapies.23 In our view, it is unreasonable to require general practitioners to prescribe medications that they feel are outside their area of competence. At the same time, it is clear that gender identity clinics are currently too overstretched to adequately address the needs of transgender people in a timely fashion. Hence, NHS commissioners at both local and national level must invest in an expansion of capacity in specialist clinics so that access is improved, waiting times to see specialists reduced and specialist services have much greater ability to provide support to both non-specialist clinicians and patients.
Expanding the capacity of the NHS to manage this group of patients will also require the provision of adequate training to non-specialist physicians, including general practitioners (see e-learning module25). Innovative approaches to provision of specialist advice to general practitioners in the community might also be beneficial, e.g. telephone, video or email consultation with a specialist. Further roles for general practitioners include optimising fitness before gender reassignment surgery (e.g. smoking cessation, weight loss, improving diabetic control) and ensuring successful post-operative rehabilitation while monitoring for any complications. Development of primary care-based services could be through the implementation of an optional ‘Enhanced Service’, responding locally to increased demands for service provision beyond what is required under the core general practitioner contract. The specification for such an enhanced service would need to define the role of the general practitioner, including guidance on prescribing and monitoring, as well as payment for providing the service.
At the same time, specialist clinics also need to play a greater role in supporting patients in the community. For example, one reason commonly given by specialists as to why general practitioners should prescribe for this group of patients is that they can then have their prescription dispensed at a local pharmacy. Specialists who make this argument seem unaware that hospital specialists can also issue FP10s (the prescription form used to obtain medication from a community pharmacy).29 Furthermore, the NHS Electronic Prescription Service now makes it straightforward to send prescriptions electronically to almost any community pharmacy in England,29 and this should make it possible for specialists to take on a greater role in long-term prescribing.
Screening in transgender patients
Transgender patients, at whatever stage of their transition, should continue to be included in appropriate national screening programmes. The best principle is to screen the target organ, not the gender.2 This might mean a trans man (assuming he has not undergone surgery to remove the cervix) would continue to receive regular cervical smears to reduce his risk of advanced cervical cancer, or a 65-year-old trans woman would have screening for an abdominal aortic aneurysm, given that she will to retain the risk of her natal sex for developing this condition. Steps must be taken to ensure that patients are not removed from relevant recall systems after legal gender and name changes.
Although screening programmes promote health on a population level, being invited or included in screening can provoke intense dysphoria for transgender people, which may make them reluctant or unable to participate. In general, be sensitive but explicit when asking questions about gendered anatomy, genitalia or secondary sexual characteristics; if such questioning is medically necessary, explain the reasons for inquiring. The individual should be asked which healthcare professional they would prefer to perform the procedure and how it could best be adapted to their comfort. As an example, a trans man may have specific preferences about the size of speculum used for the cervical smear.
It is recommended that trans women are included in national breast cancer screening, in addition to managing the risk of prostate cancer as for natally assigned men.30 For patients who have undergone gonadectomy or stop cross-sex hormonal therapy after a gonadectomy, bone mineral density measurements should be considered; they are also recommended for those with any additional risk factors for osteoporosis.30 Specialist involvement might be required in certain situations, for example when hormone treatments might impact on risk profiling for conditions such as cardiovascular disease or osteoporosis. Therefore, advice from an endocrinologist may need to be sought in some cases.
Conclusions
Gender identity is a complex subject where research is lacking and preconceptions abound. Physicians from all fields should address transgender patients with acceptance, compassion and a non-judgemental approach. Formal education and training on gender identity and reassignment is needed for general practitioners, primary care trainees and clinicians from other specialties who will see an increasing number of such patients. Education can change attitudes for the better, overcome difficulty and confusion for patients and doctors alike. In the interim, innovative approaches are needed to bridge the gap in knowledge between specialist centres and primary care; specialist advice via telephone or email might be a simple but effective solution. Not only would understanding the unmet needs and concerns of transgender patients alleviate suffering for many, but it would also offer unique insights on questions relating to human identity and personality.
Note
Note that some prefer ‘Differences in Sex Development’ as a less stigmatising term than ‘Disorders…’ (implying that one’s self-affirmed identity is somehow defective), though this is somewhat controversial. Those who prefer the latter argue that if these variations represent mere ‘differences’ in sexual characteristics rather than ‘disorders’, there would be no need to medicalise them, and as such, no rationale or role for medical treatment.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethical approval
Not applicable since neither patients nor laboratory testing was involved.
Guarantor
AM.
Contributorship
AJ, CC and AM conceived of the manuscript. AJ wrote the manuscript with help from CC and MH. AM reviewed the manuscript and provided some additional content.
Acknowledgements
Imperial College London is grateful for support from the NW London NIHR Collaboration for Leadership in Applied Health Research & Care, the Imperial NIHR Biomedical Research Centre, and the Imperial Centre for Patient Safety and Service Quality. The views expressed in this article are those of the authors.
Provenance
Not commissioned; peer-reviewed by Iain Morland.
References
- 1.General Medical Council UK. Advice for doctors treating transgender patients. See http://www.gmc-uk.org/guidance/28851.asp (2016, last checked 23 August 2016).
- 2.Douglas N. Trans Guidance for GPs. Brighton and Hove CCG 2016.
- 3. Parameshwaran V, Cockbain BC, Hillyard M and Price J. Is the lack of specific LGBTQ health care education in medical school a cause for concern? Evidence from a survey of knowledge and practice among UK medical students. J Homosex. Epub ahead of print 2016. DOI:. [DOI] [PubMed]
- 4.Redfern J, Sinclair B. Improving healthcare encounters and communication with transgender patients. J Commun Healthc 2014; 7: 25–40. [Google Scholar]
- 5.National Centre for Transequality, USA. Transgender Terminology. See http://www.transequality.org/ (2014, last checked 23 August 2016).
- 6.Fausto-Sterling A. Sexing the Body: Gender Politics and the Construction of Sexuality, New York: Basic Books, 2000. [Google Scholar]
- 7.Stryker S and Whittle S. The Transgender Studies Reader. New York: Routledge, 2006.
- 8.Savic I, Garcia-Falgueras A, Swaab DF. Sexual differentiation of the human brain in relation to gender identity and sexual orientation. Prog Brain Res 2010; 186: 41–62. [DOI] [PubMed] [Google Scholar]
- 9.Blanchard R. Varieties of autogynaephilia and their relationship to gender dysphoria. Arch Sex Behav 1993; 22: 241–251. [DOI] [PubMed] [Google Scholar]
- 10.Drescher J, Cohen-Kettenis P, Winter S. Minding the body: situating gender identity diagnoses in the ICD-11. Int Rev Psychiatry 2012; 24: 567–577. [DOI] [PubMed] [Google Scholar]
- 11.Maguen S, Shipherd J. Suicide risk among transgender individuals. Psychol Sex 2010; 1: 34–43. [Google Scholar]
- 12.Robles R, Fresán A, Vega-Ramírez H, Cruz-Islas J, Rodríguez-Pérez V, Domínguez-Martínez T. Removing transgender identity from the classification of mental disorders: a Mexican field study for ICD-11. Lancet 2016; 3: 850–859. [DOI] [PubMed] [Google Scholar]
- 13.Ministry of Justice. Gender Recognition Certificate Statistics. See https://www.gov.uk/government/collections/gender-recognition-certificate-statistics (2004–14, last checked 23 August 2016).
- 14. Reed B, Rhodes S, Schofield P and Wiley K. Gender Variance in the UK: Prevalence, Incidence and Growth and Geographic Distribution. Surrey: Gender Identity Research and Education Society (GIRES) UK, 2009.
- 15.Lyons K. Gender Identity Clinic Services Under Strain as Referral Rates Soar. London: Guardian Media Group, 2016, https://www.theguardian.com/society/2016/jul/10/transgender-clinic-waiting-times-patient-numbers-soar-gender-identity-services.
- 16.Kennedy N, Hellen M. Transgender children: more than a theoretical challenge. GJSS 2010; 7: 25–43. [Google Scholar]
- 17.Crissman HP, Berger M, Graham L, Dalton V. Transgender demographics: a household probability sample of US adults. Am J Public Health 2016; 20: e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calton JM, Cattaneo LB, Gebhard KT, et al. Barriers to help seeking for lesbian, gay, bisexual, transgender and queer survivors of intimate partner violence. Trauma Violence Abuse 2016; 17: 585–600. [DOI] [PubMed] [Google Scholar]
- 19.UK Parliament. Gender Recognition Act, 2004.
- 20.UK Parliament. Equality Act, 2010.
- 21.WPATH Standards of care for the health of transexual, transgender and gender non-conforming people, version 7. Int J Transgenderism 2012; 13: 165–232. [Google Scholar]
- 22.Fabris B, Bernardi S, Trombetta C. Cross-sex hormone therapy for gender dysphoria. J Endocrinol Invest 2015; 38: 269–282. [DOI] [PubMed] [Google Scholar]
- 23.Barrett J. Doctors are failing to help people with gender dysphoria. BMJ 2016; 352: 1694–1694. [DOI] [PubMed] [Google Scholar]
- 24.Weinand JD, Safer JD. Hormone therapy in transgender adults is safe with provider supervision: a review of hormone therapy sequelae for transgender individuals. J Clin Transl Endocrinol 2015; 2: 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Royal College of GPs. E-learning for GPs on Gender Variance. See http://elearning.rcgp.org.uk/course/info.php?popup=0&id=169 (2016, last checked 23 August 2016).
- 26.NHS England. Interim Gender Dysphoria Protocol and Service Guideline 2014. https://www.england.nhs.uk/wp-content/uploads/2013/10/int-gend-proto.pdf (last checked 29 December 2016).
- 27.Korte A, Goecker D, Krude H, Lehmkuhl U, Grüters-Kieslich A, Beier K. Gender identity disorders in childhood and adolescence: currently debated concepts and treatment strategies. Deutsch Ärztebl Int 2008; 105: 834–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Millet D. GMC transgender advice could push GPs to prescribe beyond competence, warns GPC. GP Online 2016.
- 29.NHS Choices. NHS Pharmacy Services Explained: The Electronic Prescription Service. See http://www.nhs.uk/NHSEngland/AboutNHSservices/pharmacists/Pages/eps.aspx (2016, last checked 24 December 2016).
- 30.Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, Gooren LJ, Meyer WJ, Spack NP, Tangpricha V, Montori VM, et al. Endocrine treatment of transsexual persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2009; 94: 3132–3154. [DOI] [PubMed] [Google Scholar]