Abstract
Objective:
The objective was to estimate the age of onset (AOO) for all anxiety disorders and for specific subtypes. Gender differences in the AOO of anxiety disorders were examined, as were the influence of study characteristics on reported AOOs.
Methods:
Seven electronic databases were searched up to October 2014, with keywords representing anxiety disorder subtypes, AOO, and study design. The inclusion criteria were studies using a general population sample that provided data on the AOO for all anxiety disorders, or specific anxiety disorders, according to DSM-III-R, DSM-IV, or ICD-10 criteria.
Results:
There were 1028 titles examined, which yielded 24 studies meeting the inclusion criteria. Eight studies reported the AOO and gender. Meta-analysis found a mean AOO of all anxiety disorders of 21.3 years (95% CI 17.46 to 25.07). Separation anxiety disorder, specific phobia, and social phobia had their mean onset before the age of 15 years, whereas the AOO of agoraphobia, obsessive-compulsive disorder, posttraumatic stress disorder, panic disorder, and generalized anxiety disorder began, on average, between 21.1 and 34.9 years. Meta-analysis revealed no difference in the AOO between genders. A prospective study design and higher developmental level of the study country were associated with an earlier AOO.
Conclusions:
Results from this meta-analysis indicate that anxiety disorder subtypes differ in the mean AOO, with onsets ranging from early adolescence to young adulthood. These findings suggest that prevention strategies of anxiety disorders should be directed towards factors associated with the development of anxiety disorder subtypes in the age groups with the greatest vulnerability for developing those disorders.
Keywords: anxiety disorders, age of onset, meta-analysis, gender differences, general population sample
Abstract
Objectif:
Estimer l’âge de début (ADD) de tous les troubles anxieux, et de sous-types spécifiques. Les différences selon le sexe de l’ADD des troubles anxieux ont été examinées. ainsi que l’influence des caractéristiques de l’étude sur les ADD déclarés.
Méthode:
Sept bases de données électroniques ont été recherchées jusqu’en octobre 2014, avec des mots clés représentant les sous-types des troubles anxieux, l’ADD et la méthode de l’étude. Les critères d’inclusion étaient des études utilisant un échantillon dans la population générale qui fournissait des données sur l’ADD pour tous les troubles anxieux, ou des troubles anxieux spécifiques, selon le DSM-III-R, le DSM-IV ou les critères de la CIM-10.
Résultats:
Mille vingt-huit titres ont été examinés, ce qui a produit 24 études qui satisfaisaient aux critères d’inclusion. Huit études mentionnaient l’ADD et le sexe. La méta-analyse a révélé un ADD moyen pour tous les troubles anxieux de 21,3 ans (IC à 95% 17,46 à 25,07). Le trouble d’angoisse de séparation, la phobie spécifique et la phobie sociale avaient un début moyen avant l’âge de 15 ans, alors que l’ADD de l’agoraphobie, le trouble obsessionnel-compulsif, le trouble de stress post-traumatique, le trouble panique et le trouble d’anxiété généralisée commençaient en moyenne entre 21,1 et 34,9 ans. La méta-analyse n’a révélé aucune différence de l’ADD entre les sexes. La méthode de l’étude prospective et le niveau de développement élevé du pays de l’étude étaient associés à un ADD plus précoce.
Conclusions:
Les résultats de cette méta-analyse indiquent que les sous-types de troubles anxieux ont un ADD moyen différent, les commencements s’échelonnant du début de l’adolescence au jeune âge adulte. Ces résultats suggèrent que les stratégies de prévention des troubles anxieux devraient être axées sur les facteurs associés au développement des sous-types des troubles anxieux dans les groupes d’âge présentant la plus grande vulnérabilité à développer ces troubles.
Clinical Implications
The AOO of anxiety disorders presented in this meta-analysis may assist professionals to recognize the emergence of anxiety disorders.
Differences in the AOO emphasize that preventive strategies need to be directed towards specific vulnerability periods of anxiety disorder subtypes.
Despite the gender differences in prevalence rates of anxiety disorders, the AOO of anxiety disorders does not differ across genders.
Limitations
The effect of sample age on the AOO was not examined because most studies did not report these descriptives.
Several studies could not be included in the present meta-analysis as they did not report sufficient statistical summary measures.
Numerous community surveys have shown that anxiety disorders are the most common mental disorders worldwide.1 Anxiety disorders are debilitating and often cause impairment in social and occupational functioning.2,3 Anxiety disorders cause more disability than all other mental health disorders.4 Economic losses arising from anxiety disorders have been estimated at around US$42 billion annually in the United States and €41 billion in Europe.5,6 Childhood anxiety symptoms often persist into adulthood,7 and the early identification as well as treatment of children at risk for anxiety disorders may prevent the development of more severe disorders.8–12
The age of onset (AOO) of mental disorders is a vital statistic in the formulation of mental health policy.13 Several studies have compared the outcomes of early versus late onset of anxiety disorders. Early (childhood) onset has been associated with more severe psychopathology and comorbidity,14–16 more avoidance behaviour,17 and even higher rates of suicide.18 Although outcomes of early anxiety disorder onset demonstrate the need for accurate information about the AOO, there is wide variation in the reported mean AOO between studies and for anxiety disorder subtypes.
Two previous reviews19,20 have reported on the AOO of a range of mental health disorders in the general population, including anxiety disorders. They found that some anxiety disorders, particularly phobias, have their onset in childhood, whereas other anxiety disorder subtypes begin later, usually in early adult life. However, these review studies did not systematically estimate the AOO of different anxiety disorders and did not examine factors that might have influenced reported AOOs. First, the reliability of the retrospective recollection of AOOs may be affected by recall bias,21 and prospective studies may provide more reliable information on AOOs. Second, as prevalence rates vary between countries22 and individual studies report differences in the AOO for males and females,18 both the country of origin and gender may influence the AOO. To our knowledge, there are no studies that have used meta-analyses to estimate the AOO of all anxiety disorders and the AOO of specific anxiety disorders. Meta-analysis has the advantage of combining data from a number of studies, improving the accuracy of the final estimate of the AOO. Meta-regression can examine factors that influence the AOO, reducing the probability of type I error.
The present study aimed to conduct a systematic review and meta-analysis of published studies to estimate the AOO of all anxiety disorders and subtypes of anxiety disorder. In addition, we aimed to examine the influence of gender differences and study characteristics on the AOO of anxiety disorders.
Methods
Data Sources
The following databases were searched from inception on October 17, 2014: Excerpta Medica dataBASE (EMBASE), MEDLINE (OvidSP), Web of Science, PsycINFO (OvidSP), Cochrane, PubMed (as supplied by publisher), and Google Scholar. Titles and abstracts were searched with a combination of the following keywords (adjusted for the specific database): “Anxiety disorder” (i.e., anxiety disorder, acute stress disorder, generalized anxiety disorder, agoraphobia, [specific/isolated] phobia, social phobia, obsessive-compulsive disorder, posttraumatic stress disorder, adjustment disorder, separation anxiety disorder, stress disorder, panic disorder), “Age of onset” (i.e., onset age, AOO, age at onset), and “Study design” (i.e., cohort, longitudinal, prospective, retrospective). Searches were limited to studies published in English.
Study Selection
First, 2 master psychologists (J.d.L. and C.Z.) independently reviewed the title and abstract of the articles for relevance. We included studies using a complete sample from the general population that reported on AOO, prevalence, incidence, lifetime occurrence, or epidemiology of anxiety, psychiatric, or mental disorders and that were published in a peer-reviewed, indexed scientific journal. We excluded studies that did not examine a representative sample of the general population, reviews of other studies, and studies that reported on subclinical anxiety (i.e., no diagnosis).
Second, the full texts of articles found eligible in the first step were screened by the 2 psychologists independently for both the inclusion and exclusion criteria mentioned above and for the following additional criteria: 1) anxiety disorders were classified by either DSM-III-R, DSM-IV, or ICD-10; 2) AOO was defined as the age at which the first symptoms of an anxiety disorder were experienced; and 3) there was an availability of summary statistics or projections (i.e., Kaplan-Meier) of the location (i.e., mean or median) and/or spread (i.e., SD or interquartile range [IQR]) for the AOO of anxiety disorders.
Data Extraction Process
Author contact
All corresponding authors of the articles that were included after the second step of study selection were contacted by email and asked to send means and SDs (or medians and IQRs) and corresponding sample sizes for the AOO of anxiety disorders in general and subtypes. In addition, all authors were asked to send these results for males and females separately.
Sample overlap
When studies were based on an identical sample, only one study was included based on the following hierarchical rules: 1) the statistical, most usable AOO characteristics; 2) for prospective studies, the study conducted over the longest duration; and 3) the study with most information about the AOO (i.e., subtypes, gender differences).
Data extraction
The study design (retrospective or prospective) and sample characteristics (total sample size, % males, age range at the time of the study, and classification system used [DSM-III-R, DSM-IV, or ICD-10]) were extracted. The Human Developmental Index (HDI) was used to quantify the level of development of a country and represents a summary measure of average life expectancy, education, and income.23 The following AOO characteristics were extracted: number of participants with a lifetime history of an anxiety disorder, summary statistics (differentiated by gender if available), AOO assessment instrument, number of subtypes covered by the assessment instrument, and definition of AOO defined by the assessment instrument. When the number of participants with a lifetime history of an anxiety disorder was not reported, the sample size was calculated based on the prevalence rates of anxiety disorders as reported by the study. For AOO characteristics, preference was given to data that were provided by email by authors if the data either qualitatively or quantitatively (i.e., subtypes) outperformed data from the original article.
Statistical Analysis
The statistical program Comprehensive Meta-Analysis24 was used for meta-analysis. A random-effects model was employed because of the high likelihood of between-study heterogeneity. The method of moments was chosen for meta-regression. Medians of the AOO were transformed to means and SDs as described by Wan et al25 in which both the IQR (25th and 75th percentiles) and sample size related to the median are taken into account.
First, the mean AOO was estimated for anxiety disorders in general (ANX) and for the following subtypes: separation anxiety disorder (SAD), specific phobia (SP), social phobia (SOP), agoraphobia without panic disorder (AwP), obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), panic disorder (PD), and generalized anxiety disorder (GAD). Second, meta-analyses were performed to test for gender differences in the AOO. Third, meta-regressions were performed to examine the impact of moderator variables on the reported AOO measures. Study design, number of anxiety disorders covered, and HDI were entered as moderators.
Results
Study Selection
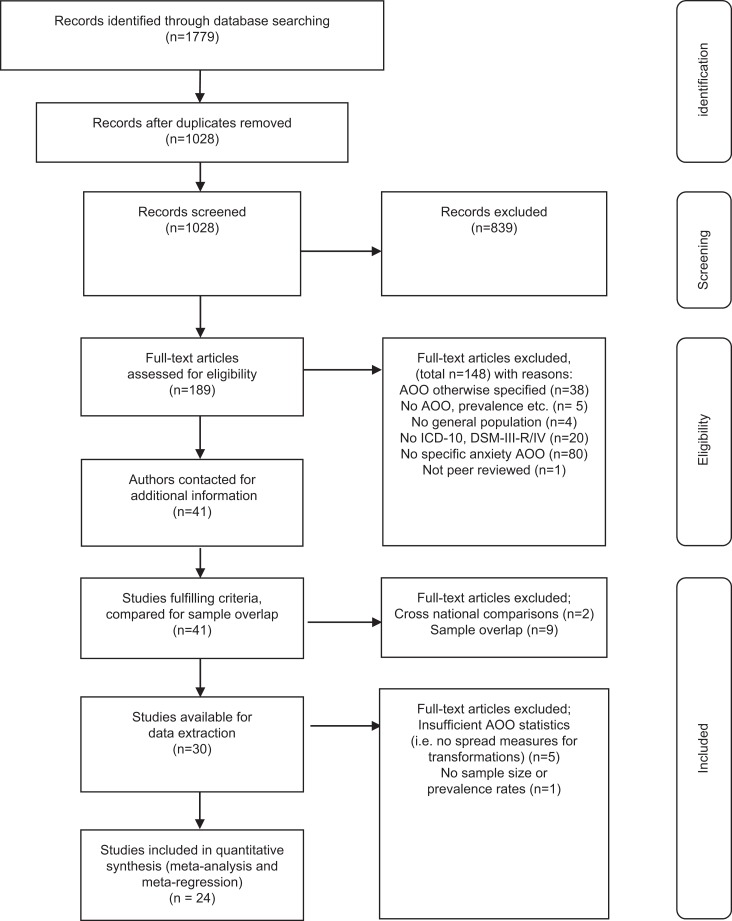
A detailed overview of the study selection process is displayed in Figure 1. In the first step of screening for study inclusion based on the title and abstract, 189 of the 1028 identified studies were eligible (95.9% reviewer consensus). In the second step based on full texts, 41 of the 189 studies were included (92.1% reviewer consensus). The corresponding authors of 8 studies provided additional data by email. After considering priorities of quality and quantity regarding sample overlap, 30 articles were selected for data extraction. Six studies were excluded because they did not report, and we were unable to locate by correspondence with the authors the sample sizes, prevalence rates, or spread measures of the AOO. Twenty-four studies were included in the meta-analysis (see online Appendix 1 for an overview),26–49 of which 8 presented gender-specific AOO data.
Figure 1.
Flowchart of study selection process.
Study Characteristics
Most studies had a retrospective design (70.8%) and used the DSM-III-R or DSM-IV classification (95.8%). The age range of the participants in the studies varied from narrow to broad, and samples ranged from early adolescence until late adulthood. Twelve AOO medians with IQRs were transformed to means and SDs. When studies reported the AOO for both PD with and PD without agoraphobia, these separate estimates were combined in the meta-analysis, together representing PD.
Meta-analyses
Age of onset
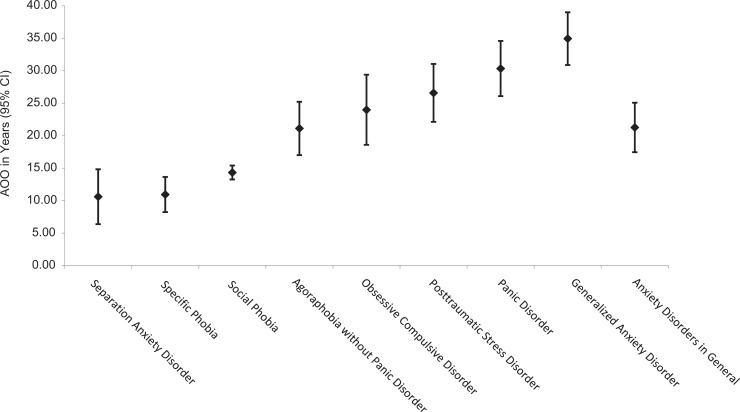
Figure 2 gives an overview of the estimated mean AOO and number of estimates of each anxiety disorder. The meta-analysis for ANX included estimates from 14 nonoverlapping studies with a total sample of 7443 individuals. The estimated mean AOO was 21.3 years (95% CI 17.46 to 25.07). The estimated AOO was lowest for SAD (10.6 years; 95% CI 6.38 to 14.84), followed by SP (11.0 years; 95% CI 8.25 to 13.65) and SOP (14.3 years; 95% CI 13.27 to 15.41). Higher AOOs were estimated for AwP (21.1 years; 95% CI 17.02 to 25.23), OCD (24.0 years; 95% CI 18.57 to 29.41), PTSD (26.6 years; 95% CI 22.13 to 31.06), PD (30.3 years; 95% CI 26.09 to 34.59), and GAD (34.9 years; 95% CI 30.88 to 39.01).
Figure 2.
Mean age of onset estimates for anxiety disorders. Separation anxiety disorder (SAD; 4 studies; n = 388), specific phobia (SP; 11 studies; n = 7207), social phobia (SOP; 12 studies; n = 3407), agoraphobia without panic disorder (AwP; 8 studies; n = 1209), obsessive-compulsive disorder (OCD; 11 studies; n = 866), posttraumatic stress disorder (PTSD; 12 studies; n = 1459), panic disorder (PD; 11 studies; n = 3240), generalized anxiety disorder (GAD; 15 studies; n = 4422), and anxiety disorders in general (ANX; 14 studies; n = 7443). I 2 = 93.6%–99.7% (all P < 0.0001).
As evidenced by the nonoverlapping confidence intervals of their estimates, SAD, SP, and SOP have a significantly earlier AOO than other anxiety disorders, and GAD has a significantly later AOO than SAD, SP, SOP, AwP, and OCD.
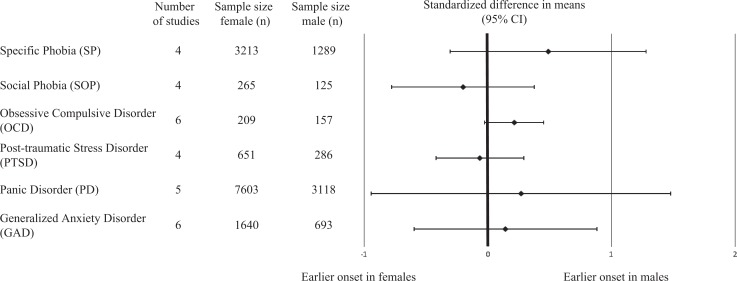
Gender differences in AOO
Because only 2 studies reported gender-specific estimates for SAD, AwP, and ANX, these AOO outcomes could not be analyzed. A total of 31 estimates of 8 separate studies were included in this meta-analysis with a total sample size of 3256 males and 7766 females.
Publication bias could not be assessed because there were not enough estimates for each anxiety disorder subtype. Moreover, combining all different anxiety disorder subtypes in one funnel plot could result in a noninformative conclusion of publication bias.
Figure 3 shows the combined, abbreviated forest plot with the weighted effect size and 95% CI for 6 anxiety disorder subtypes. No significant difference in the AOO of anxiety disorders was found between males and females. The weighted mean difference (WMD) between genders in the AOO varied between –0.20 (95% CI –0.78 to 0.38, I 2 = 82.2%, P < 0.001) for SOP to 0.49 (95% CI –0.31 to 1.28, I 2 = 97.7%, P < 0.001) for SP. Both I 2 measures indicate that there is a significant amount of heterogeneity between studies, which supports our choice of a random-effects model. A nonsignificant trend was found for an earlier onset of OCD in males (WMD = 0.21, 95% CI –0.03 to 0.45, P = 0.08; I 2 = 6.4%, P = 0.376).
Figure 3.
Combined forest plot for gender difference in age of onset (years) for anxiety disorders.
Meta-regressions
Meta-regression outcomes of the impact of study design, number of anxiety disorders covered by ANX, and HDI on the AOO of anxiety disorders are shown in Table 1.
Table 1.
Meta-regression on the effect of study characteristics on AOO of anxiety disorders.
| Anxiety disorder subtype | Slope (standard error) | 95% CI | R 2 value |
|---|---|---|---|
| Separation anxiety disorder | |||
| Study design | n.s. | ||
| HDI | –90.45 (9.10)a | –108.29 to –72.61 | 0.94 |
| Specific phobia | |||
| Study design | n.s. | ||
| HDI | n.s. | ||
| Social phobia | |||
| Study design | –3.12 (1.21)b | –5.49 to –0.74 | —c |
| HDI | –17.38 (4.20)a | –25.61 to –9.14 | 0.44 |
| Agoraphobia without panic disorder | |||
| Study design | –8.25 (2.64)b | –13.43 to –3.08 | 0.65 |
| HDI | n.s. | ||
| Obsessive-compulsive disorder | |||
| Study design | –13.16 (4.78)a | –22.54 to –3.79 | 0.31 |
| HDI | –88.21 (19.42)a | –126.27 to –50.15 | 0.62 |
| Posttraumatic stress disorder | |||
| Study design | –16.60 (3.33)a | –23.12 to –10.07 | 0.51 |
| HDI | n.s. | ||
| Panic disorder | |||
| Study design | –15.21 (2.76)a | –20.62 to –9.80 | 0.69 |
| HDI | n.s. | ||
| Generalized anxiety disorder | |||
| Study design | –18.19 (3.62)a | –25.29 to –11.09 | 0.51 |
| HDI | –83.75 (20.55)a | –124.03 to –43.47 | 0.45 |
| Anxiety disorders in general | |||
| Study design | –12.36 (4.87)b | –21.91 to –2.81 | —c |
| Number of subtypes covered | –6.34 (1.31)a | –8.90 to –3.78 | 0.32 |
| HDI | n.s. | ||
Study design represents a dummy variable (0 = retrospective, 1 = prospective). AOO = age of onset; HDI = Human Developmental Index; n.s. = not significant.
a P < 0.001.
b P < 0.01.
cExplained variance could not be calculated because the between-study variance was higher after entering the covariate.
First, we investigated the impact of a prospective design versus a retrospective design on the AOO. Ninety-eight estimates were included in 9 separate meta-regressions. The results showed an earlier AOO of AwP, OCD, PTSD, PD, and GAD for studies with a prospective design, explaining 30.93% to 75.57% of the variance in the AOO between studies.
Second, we determined whether the AOO of ANX was associated with the number of anxiety disorder subtypes covered by ANX in the different studies. Fourteen estimates were included in this analysis. The results showed that an earlier AOO of ANX was found when ANX was covered by more anxiety disorder subtypes (β = –6.34 [1.31], 95% CI –8.90 to 3.78, R 2 = 0.32, P < 0.001).
Third, we related the HDI of the study country to the AOO of anxiety disorders. A total of 98 estimates were included in this analysis. Differences in the AOO between different levels of the HDI were found. An earlier onset of SAD, SOP, OCD, and GAD was reported for countries with a higher HDI. Explained variances varied between anxiety disorder subtypes, with 4.46% for GAD up to 94.45% for SAD.
Discussion
This meta-analysis aimed to estimate the AOO of anxiety disorders and examine gender differences in the AOO and the effect of study characteristics on the AOO. Twenty-four studies with a general population sample were included in the present study. ANX had an estimated mean AOO of 21.3 years. Significant differences in the AOO were found between anxiety disorder subtypes. SAD, SP, and SOP had their onset in childhood and early adolescence, whereas AwP, OCD, PTSD, PD, and GAD had their onset in young adulthood. Gender was not related to the AOO of anxiety disorders. An earlier AOO was found for ANX when it comprised more anxiety disorder subtypes. For certain specific anxiety disorder subtypes, study design and developmental level of the study were associated with the AOO.
A strength of the current meta-analysis is that we were able to use previous empirical studies in the general population to estimate the AOO for each anxiety disorder subtype. The 2 previous reviews of Kessler et al19 and McGorry et al20 did not specify AOOs for each anxiety disorder. Moreover, the AOO reported by McGorry et al20 was younger probably because their review was limited to studies of adolescents.
The current meta-analysis shows differences in the onset of anxiety disorder subtypes, ranging from early adolescence to young adulthood. This sequence validates the current taxonomy of anxiety disorders,50 as social and cognitive development has been shown to affect the timing of anxiety disorder subtypes,51,52 in addition to environmental and genetic risk factors.53 The later onset of AwP, PD, and GAD, for instance, is in line with research that separates these disorders from SP based on genetic predisposition.54,55 SOP, which was found to emerge in adolescence, has a shared genetic susceptibility with AwP, PD, and GAD.
We found that GAD had the latest AOO at around 35 years. This high estimation of the AOO of GAD might be biased due to the large diagnostic overlap with major depressive disorders56,57 in combination with the relatively later onset of mood disorders.1 SAD was found to have the earliest AOO. This early onset is probably due to the requirement in ICD-10, DSM-III-R, and DSM-IV that the onset of SAD is before the age of 18 years. As DSM-5 allows for the onset of SAD in adulthood,58 AOO estimates for SAD will probably be higher in future studies.
Although it is well known that anxiety disorders are more common among women (for an overview, see Somers et al59), and that women comprised two-thirds of the individuals in our study, we did not find gender differences in the AOO of anxiety disorders. No gender difference in AOOs was found in a large study by McLean et al.60 This finding suggests that the period of greatest vulnerability for developing an anxiety disorder is the same for men and women.
An earlier AOO was estimated for SAD, SOC, GAD, and OCD in countries with a higher HDI. This suggests that some anxiety disorder subtypes have an earlier onset in countries that provide better life expectancy, education, and income. However, other factors can explain these findings as well. First, most studies had a retrospective design. Retrospective studies on AOOs rely heavily on the recall of the first onset of symptoms. More public awareness of and less prejudice against mental health problems in developed countries than in developing countries61 might result in the earlier recognition and recall of anxiety problems in people from developed countries. Additionally, families in developing countries might have more pressing concerns, which could result in delayed recall of the onset of anxiety disorders when asked retrospectively. Second, most of the prospective studies were carried out in developed countries. Prospective studies likely have a more accurate estimate of the AOO of mental disorders compared to retrospective studies. This could be an explanation of why earlier AOOs were found for developed countries. Third, half of the studies in countries with a low HDI did not cover SAD and OCD. Therefore, AOO estimates of SAD and OCD for developing countries are not very robust.
Limitations
Because of the large diversity in study characteristics and statistics reported by the studies included in this meta-analysis, the following limitations should be taken into account. First, many studies could not be included in the present meta-analysis because they did not report sufficient statistical summary measures. Second, we were not able to control for the age of the samples as no study provided mean age statistics. Presumably, an older sample will be associated with later AOOs due to recall bias and a longer period of being at risk of developing the disorder. Third, we found that prospective studies reported lower AOOs of anxiety disorders. As most studies that were included in this meta-analysis had a retrospective design, this could have led to higher estimates of the AOO due to recall bias. Fourth, we had to transform reported medians to means, while skewness of the data favours using median instead of mean scores. This may also have led to a later estimated AOO. Using prevalence rates to determine the sample size of individuals who reported on the AOO of anxiety disorders probably overestimated the weight of these studies in the meta-analysis, as not all individuals are able to report on their AOO.
Implications
There are several important implications from the results of this meta-analysis. The estimated AOOs identified risk periods for the development of different anxiety disorders. This information could guide prevention programs to target factors contributing to the emergence of anxiety disorders in key vulnerability periods. Because primary prevention programs have generally been provided at schools, the later onset of AwP, OCD, PTSD, PD, and GAD highlights the need for prevention beyond the education system. As to future research, when studying AOOs in either general community or clinical samples, more uniform reporting would help in the interpretation of study results. Based on the diversity found in the reporting of AOOs and the results of the current study, we propose for reporting both the mean or median and the variation of this measure. In addition, more prospective studies with frequent screening would further guide our understanding of the AOO of anxiety disorders.
Conclusions
The current meta-analysis indicates that ANX has an onset around 21 years and that anxiety disorder subtypes differ in the mean AOO. No gender differences in the AOO of anxiety disorders were found. Moreover, a prospective study design and higher development status of a country were associated with an earlier onset of anxiety disorders. The identified intervals of AOOs for different anxiety disorders indicate windows of risk in which to implement tailored preventive strategies.
Supplementary Material
Acknowledgments
The authors thank biomedical information specialist W.M. Bramer for his assistence in executing the systematic literature search, next to the corresponding authors of the studies who provided additional information, which contributed to the realization of this study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: The online supplement is available at http://journals.sagepub.com/doi/suppl/10.1177/0706743716640757.
References
- 1. Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 2. Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry. 2000;157(5):669–682. [DOI] [PubMed] [Google Scholar]
- 3. Stein MB, Roy-Byrne PP, Craske MG, et al. Functional impact and health utility of anxiety disorders in primary care outpatients. Med Care. 2005;43(12):1164–1170. [DOI] [PubMed] [Google Scholar]
- 4. Baxter AJ, Vos T, Scott KM, et al. The global burden of anxiety disorders in 2010. Psychol Med. 2014;22:1–12. [DOI] [PubMed] [Google Scholar]
- 5. Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60(7):427–435. [DOI] [PubMed] [Google Scholar]
- 6. Andlin-Sobocki P, Jonsson B, Wittchen HU, et al. Cost of disorders of the brain in Europe. Eur J Neurol. 2005;12 Suppl 1:1–27. [DOI] [PubMed] [Google Scholar]
- 7. Bittner A, Egger HL, Erkanli A, et al. What do childhood anxiety disorders predict? J Child Psychol Psychiatry. 2007;48(12):1174–1183. [DOI] [PubMed] [Google Scholar]
- 8. Barrett PM, Farrell LJ, Ollendick TH, et al. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: an evaluation of the friends program. J Clin Child Adolesc Psychol. 2006;35(3):403–411. [DOI] [PubMed] [Google Scholar]
- 9. Christensen H, Pallister E, Smale S, et al. Community-based prevention programs for anxiety and depression in youth: a systematic review. J Prim Prev. 2010;31(3):139–170. [DOI] [PubMed] [Google Scholar]
- 10. Benjamin CL, Harrison JP, Settipani CA, et al. Anxiety and related outcomes in young adults 7 to 19 years after receiving treatment for child anxiety. J Consult Clin Psychol. 2013;81(5):865–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kendall PC, Safford S, Flannery-Schroeder E, et al. Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. J Consult Clin Psychol. 2004;72(2):276–287. [DOI] [PubMed] [Google Scholar]
- 12. Saavedra LM, Silverman WK, Morgan-Lopez AA, et al. Cognitive behavioral treatment for childhood anxiety disorders: long-term effects on anxiety and secondary disorders in young adulthood. J Child Psychol Psychiatry. 2010;51(8):924–934. [DOI] [PubMed] [Google Scholar]
- 13. de Girolamo G, Dagani J, Purcell R, et al. Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiol Psychiatr Sci. 2012;21(1):47–57. [DOI] [PubMed] [Google Scholar]
- 14. Anholt GE, Aderka IM, van Balkom AJ, et al. Age of onset in obsessive-compulsive disorder: admixture analysis with a large sample. Psychol Med. 2014;44(1):185–194. [DOI] [PubMed] [Google Scholar]
- 15. Ramsawh HJ, Weisberg RB, Dyck I, et al. Age of onset, clinical characteristics, and 15-year course of anxiety disorders in a prospective, longitudinal, observational study. J Affect Disord. 2011;132(1–2):260–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosellini AJ, Rutter LA, Bourgeois ML, et al. The relevance of age of onset to the psychopathology of social phobia. J Psychopathol Behav Assess. 2013;35(3):356–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lim SW, Ha J, Shin YC, et al. Clinical differences between early- and late-onset social anxiety disorders. Early Interv Psychiatry. 2013;7(1):44–50. [DOI] [PubMed] [Google Scholar]
- 18. Tibi L, van Oppen P, Aderka IM, et al. Examining determinants of early and late age at onset in panic disorder: an admixture analysis. J Psychiatr Res. 2013;47(12):1870–1875. [DOI] [PubMed] [Google Scholar]
- 19. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McGorry PD, Purcell R, Goldstone S, et al. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 2011;24(4):301–306. [DOI] [PubMed] [Google Scholar]
- 21. Wittchen HU, Burke JD, Semler G, et al. Recall and dating of psychiatric symptoms: test-retest reliability of time-related symptom questions in a standardized psychiatric interview. Arch Gen Psychiatry. 1989;46(5):437–443. [DOI] [PubMed] [Google Scholar]
- 22. World Health Organization. Cross-national comparisons of the prevalences and correlates of mental disorders: WHO International Consortium in Psychiatric Epidemiology. Bull World Health Organ. 2000;78(4):413–426. [PMC free article] [PubMed] [Google Scholar]
- 23. United Nations Development Programme. Human Development Report. New York: United Nations; 2014. [Google Scholar]
- 24. Borenstein M, Hedges L, Higgens J, et al. Comprehensive Meta-Analysis version 2. Englewood (NJ): Biostat; 2005. [Google Scholar]
- 25. Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alhasnawi S, Sadik S, Rasheed M, et al. The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS). World Psychiatry. 2009;8(2):97–109. [PMC free article] [PubMed] [Google Scholar]
- 27. Angst J, Gamma A, Endrass J, et al. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. Eur Arch Psychiatry Clin Neurosci. 2004;254(3):156–164. [DOI] [PubMed] [Google Scholar]
- 28. Becker ES, Rinck M, Turke V, et al. Epidemiology of specific phobia subtypes: findings from the Dresden Mental Health Study. Eur Psychiatry. 2007;22(2):69–74. [DOI] [PubMed] [Google Scholar]
- 29. Bienvenu OJ, Onyike CU, Stein MB, et al. Agoraphobia in adults: incidence and longitudinal relationship with panic. Br J Psychiatry. 2006;188:432–438. [DOI] [PubMed] [Google Scholar]
- 30. Bonnewyn A, Bruffaerts R, Vilagut G, et al. Lifetime risk and age-of-onset of mental disorders in the Belgian general population. Soc Psychiatry Psychiatr Epidemiol. 2007;42(7):522–529. [DOI] [PubMed] [Google Scholar]
- 31. Caraveo-Anduaga JJ, Colmenares Bermudez E. The epidemiology of obsessive-compulsive disorder in Mexico City. Salud Ment. 2004;27(2):1–6. [Google Scholar]
- 32. Chapman C, Mills K, Slade T, et al. Remission from post-traumatic stress disorder in the general population. Psychological Medicine. 2012;42(8):1695–1703. [DOI] [PubMed] [Google Scholar]
- 33. Chartier MJ, Walker JR, Stein MB. Considering comorbidity in social phobia. Soc Psychiatry Psychiatr Epidemiol. 2003;38(12):728–734. [DOI] [PubMed] [Google Scholar]
- 34. Cho MJ, Chang SM, Hahm BJ, et al. Lifetime risk and age of onset distributions of psychiatric disorders: analysis of national sample survey in South Korea. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):671–681. [DOI] [PubMed] [Google Scholar]
- 35. Falk DE, Yi HY, Hilton ME. Age of onset and temporal sequencing of lifetime DSM-IV alcohol use disorders relative to comorbid mood and anxiety disorders. Drug Alcohol Depend. 2008;94(1–3):234–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gau SSF, Chong MY, Yang P, et al. Psychiatric and psychosocial predictors of substance use disorders among adolescents: longitudinal study. Br J Psychiatry. 2007;190:42–48. [DOI] [PubMed] [Google Scholar]
- 37. Giaconia RM, Reinherz HZ, Silverman AB, et al. Ages of onset of psychiatric disorders in a community population of older adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33(5):706–717. [DOI] [PubMed] [Google Scholar]
- 38. Goncalves DC, Byrne GJ. Sooner or later: age at onset of generalized anxiety disorder in older adults. Depress Anxiety. 2012;29(1):39–46. [DOI] [PubMed] [Google Scholar]
- 39. Gureje O, Uwakwe R, Udofia O, et al. Common psychiatric disorders over a lifetime: age of onset, risk and treatment contact in the Nigerian survey of mental health and wellbeing. Afr J Med Med Sci. 2008;37(3):207–217. [PubMed] [Google Scholar]
- 40. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 41. Knappe S, Beesdo-Baum K, Fehm L, et al. Social fear and social phobia types among community youth: differential clinical features and vulnerability factors. J Psychiatr Res. 2011;45(1):111–120. [DOI] [PubMed] [Google Scholar]
- 42. Lee S, Tsang A, Zhang MY, et al. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med. 2007;37(1):61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Levinson D, Zilber N, Lerner Y. Prevalence of mood and anxiety disorders in the community: results from the Israel National Health Survey. Isr J Psychiatry Relat Sci. 2007;44(2):94–103. [PubMed] [Google Scholar]
- 44. Lewinsohn PM, Lewinsohn M, Gotlib IH, et al. Gender differences in anxiety disorders and anxiety symptoms in adolescents. J Abnorm Psychol. 1998;107(1):109–117. [DOI] [PubMed] [Google Scholar]
- 45. Marquenie LA, Schade A, van Balkom AJLM, et al. Origin of the comorbidity of anxiety disorders and alcohol dependence: findings of a general population study. Eur Addict Res. 2007;13(1):39–49. [DOI] [PubMed] [Google Scholar]
- 46. Ritchie K, Artero S, Beluche I, et al. Prevalence of DSM-IV psychiatric disorder in the French elderly population. Br J Psychiatry. 2004;184:147–152. [DOI] [PubMed] [Google Scholar]
- 47. Stein DJ, Seedat S, Herman A, et al. Lifetime prevalence of psychiatric disorders in South Africa. Br J Psychiatry. 2008;192(2):112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Viana MC, Andrade LH. Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the Sao Paulo metropolitan area, Brazil: results from the Sao Paulo megacity mental health survey. Rev Bras Psiquiatr. 2012;34(3):249–260. [DOI] [PubMed] [Google Scholar]
- 49. Vaingankar JA, Rekhi G, Subramaniam M, et al. Age of onset of life-time mental disorders and treatment contact. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):835–843. [DOI] [PubMed] [Google Scholar]
- 50. Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Broeren S, Muris P. The relation between cognitive development and anxiety phenomena in children. J Child Fam Stud. 2009;18(6):702–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Muris P, Merckelbach H, Luijten M. The connection between cognitive development and specific fears and worries in normal children and children with below-average intellectual abilities: a preliminary study. Behav Res Ther. 2002;40(1):37–56. [DOI] [PubMed] [Google Scholar]
- 53. Martin EI, Ressler KJ, Binder E, et al. The neurobiology of anxiety disorders: brain imaging, genetics, and psychoneuroendocrinology. Psychiatr Clin North Am. 2009;32(3):549–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hettema JM, Prescott CA, Myers JM, et al. The structure of genetic and environmental risk factors for anxiety disorders in men and women. Arch Gen Psychiatry. 2005;62(2):182–189. [DOI] [PubMed] [Google Scholar]
- 55. Kendler KS, Prescott CA, Myers J, et al. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937. [DOI] [PubMed] [Google Scholar]
- 56. Gorwood P. Generalized anxiety disorder and major depressive disorder comorbidity: an example of genetic pleiotropy? Eur Psychiatry. 2004;19(1):27–33. [DOI] [PubMed] [Google Scholar]
- 57. Zbozinek TD, Rose RD, Wolitzky-Taylor KB, et al. Diagnostic overlap of generalized anxiety disorder and major depressive disorder in a primary care sample. Depress Anxiety. 2012;29(12):1065–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Arlington (VA): American Psychiatric Association; 2013. [Google Scholar]
- 59. Somers JM, Goldner EM, Waraich P, et al. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51(2):100–113. [DOI] [PubMed] [Google Scholar]
- 60. McLean CP, Asnaani A, Litz BT, et al. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry. 2007;19(2):157–178. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.