Abstract
Sensory perceptual processing deficits, such as impaired visual object identification and perceptual closure, have been reported in schizophrenia. These perceptual impairments may be associated with neural deficits in visual association areas, including lateral occipital cortex and inferior temporal areas. However, it remains unknown if such deficits can be found in the intrinsic architecture of the visual system.
In the current study, we measured perceptual closure performance and resting-state functional connectivity using functional magnetic resonance imaging (FMRI) in 16 schizophrenia patients and 16 matched healthy controls. We estimated intrinsic functional connectivity using self-organized grouping spatial ICA, which clusters component maps in the subject space according to spatial similarity. Patients performed worse than controls in the perceptual closure task. This impaired closure performance of patients was correlated with increased severity of psychotic symptoms. We also found that intrinsic connectivity of the visual processing system was diminished in patients compared to controls. Lower perceptual closure performance was correlated to lower visual cortical intrinsic connectivity overall.
We suggest that schizophrenia is associated with impaired intrinsic connectivity of the visual system, and that it is a potential mechanism leading to impaired visual object perception. These findings contribute to increasing evidence for impairments of higher visual functions in schizophrenia.
Keywords: Schizophrenia, Visual processing, FMRI, Resting state, Perceptual closure
Highlights
-
•
We found reduced visual resting-state network connectivity in schizophrenia.
-
•
Reduced connectivity correlated with impaired perceptual closure performance
-
•
Schizophrenia is associated with impaired intrinsic connectivity of the visual system.
1. Introduction
Although schizophrenia has traditionally been conceptualized as a disorder of fronto-limbic-striatal (Meyer-Lindenberg and Weinberger, 2006) or fronto-thalamo-cerebellar (Andreasen, 1999) circuitry, recent research has also zoomed in on dysfunctions of sensory processing systems. Particularly, there is substantial evidence for impaired visual processing in schizophrenia patients. Studies over the recent years have demonstrated deficits in early visual processing pathways in schizophrenia, including dysfunctions in (subcortical) magnocellular pathways and orientation-specificity (Butler et al., 2007, Butler et al., 2005, Martinez et al., 2008, Yoon et al., 2009). Patients also show impaired performance on a number of tasks of visual object recognition, such as visual illusions, Gestalt images and perceptual closure (Doniger et al., 2001, Sack et al., 2005, Uhlhaas et al., 2006a). These findings may point to a particular dysfunction in visual perception, as it has been suggested that the magnocellular pathway may play an important role in the top-down modulation of object-based visual perception (Bar, 2003).
Impairments in visual object processing may be related to core pathological mechanisms in schizophrenia. Many visual tasks on which patients with schizophrenia perform poorly contain elements of contextual processing of sensory information (Javitt, 2009, Silverstein and Keane, 2011). Patients with schizophrenia show impaired performance when contextual information is noisy (Uhlhaas et al., 2006b, Yoon et al., 2009) or incomplete (Doniger et al., 2000, Sack et al., 2005), which indicates that these patients have difficulty integrating top-down contextual processing with bottom-up sensory information. Impaired visual processing has also been observed in sub-clinical at-risk populations (Kim et al., 2010, Oertel et al., 2009), which could indicate that visual impairments share a genetic commonality with other pathogenic mechanisms in schizophrenia. Finally, one study showed improved performance on visual processing tasks after three weeks of clinical treatment, together with alleviation of symptoms (Uhlhaas et al., 2005). Thus, impairments in visual processing may be a core feature in the pathology of schizophrenia.
Impairments in visual object perception can be investigated using perceptual closure tasks. Perceptual closure is the ability to recognize visual objects or shapes from incomplete or obstructed visual information (Snodgrass and Feenan, 1990). In perceptual closure tasks, participants must identify visual items that are partially obstructed or that miss visual details. Previous neuroimaging studies showed that performance in such tasks is associated with activity in object-related processing areas, including the lateral occipital cortex and inferior temporal areas (Doniger et al., 2000, Ploran et al., 2007, Sehatpour et al., 2006). Schizophrenia patients have shown impaired perceptual closure performance in a number of tasks (Doniger et al., 2001, Oertel et al., 2009, Sack et al., 2005). For example, in one study (Sack et al., 2005), schizophrenia patients and healthy participants had to identify partially occluded visual objects and written words within a pre-fixed time interval. Patients identified significantly fewer visual items than did healthy controls. In another study, Doniger et al. (2001) used a perceptual closure task in which the occluded visual object was revealed in a step-wise fashion, such that the image appeared more completed with each step. This process stopped when the participant correctly identified the image or when the image was completely revealed. In their task, schizophrenia patients required significantly more visual information to recognize the objects than did healthy controls. An event-related potential (ERP) study further showed that patients' impaired perceptual closure performance was associated with a diminished closure-related negativity, of which the neural source has been attributed to visual association areas (Doniger et al., 2002).
However, to date it remains unknown whether impaired perceptual closure is associated to impaired connectivity of the visual system in schizophrenia patients. One approach to address this issue is to compare intrinsic brain activity in patients and controls to perceptual closure performance. There is growing evidence that the intrinsic functional architecture, which is commonly measured using resting-state paradigms, is disrupted in schizophrenia (Alderson-Day et al., 2016, Bassett and Bullmore, 2009, Menon, 2011, van de Ven, 2012). Many of these studies have focused on higher-order brain networks that are associated with executive functioning and cognitive control. There is very little known about intrinsic abnormalities of visual cortical processing in schizophrenia patients. One resting state study (Liang et al., 2006) found widespread decreases and increases in intrinsic functional connectivity in patients, compared to controls, which included connections between visual and non-visual brain areas. However, no details about altered connectivity within visual cortex were reported. A second study (Hoptman et al., 2010) analyzed differences in low frequency amplitude (< 0.1 Hz) of resting state activity in patients and healthy controls, which strongly contributes to the functional magnetic resonance (FMRI) resting state signal (Cordes et al., 2001, Fox and Raichle, 2007, van de Ven et al., 2004) and may have a neural underpinning (Leopold et al., 2003, Shmuel and Leopold, 2008). Hoptman et al. (2010) found decreased amplitude of low frequency oscillations in visual cortex in patients, compared to controls, which could indicate impaired visual cortex functioning in patients. However, analysis of functional connectivity within visual RSN was not performed.
In addition, several FMRI resting-state studies have also shown that individual differences in connectivity strength within and between RSNs may be associated to individual behavioral performance on a number of tasks. For example, intrinsic connectivity strength of executive and cognitive control RSNs have been found to correlate with behavioral or self-report measures of attentional or executive abilities (Reineberg et al., 2015, Seeley et al., 2007). Other studies have demonstrated that larger improvements after learning a sensory (Lewis et al., 2009, Urner et al., 2013) or motor skill (Albert et al., 2009, Taubert et al., 2011, Zhang et al., 2014) are associated with larger increases in intrinsic connectivity within and between sensory, motor and higher-order RSNs after learning. Thus, it is possible that alterations in intrinsic visual cortical connectivity may be associated with corresponding changes in perceptual closure performance. However, it remains unknown whether schizophrenia patients show impaired intrinsic connectivity of visual areas and if it is behaviorally relevant for higher-order visual processing.
In the current study, we compared functional connectivity of the visual RSN in schizophrenia patients and healthy controls to perceptual closure performance obtained outside of the scanner environment. We expected to replicate previous findings of impaired perceptual closure performance in schizophrenia patients, compared to healthy controls. Further, we hypothesized that patients show reduced functional connectivity within striate and extrastriate cortex, compared to healthy controls, and that reduced intrinsic visual cortical connectivity is associated with impaired perceptual closure performance.
2. Methods
2.1. Participants
The study included sixteen right-handed schizophrenia patients of the Department of Psychiatry of the University Hospital of Goethe University, Frankfurt, Germany and sixteen control participants matched for handedness, age, gender and parental years of education. The fMRI data have been described in a previous study (Rotarska-Jagiela et al., 2010). Because of the rationale of this previous study, patients were included if they met diagnostic criteria for paranoid schizophrenia according to the DSM IV and had a history of auditory hallucinations. Table 1 lists demographic and clinical data of the participants. Participants with a history of other psychiatric or neurological disorders or drug abuse were excluded. The diagnosis of schizophrenia was confirmed with Structured Clinical Interview for DSM IV (Wittchen et al., 1997). Current psychopathology in the patient group was assessed using PANSS (Fiszbein et al., 1987). The local ethics committee of the University Hospital approved the study. Written informed consent was obtained from all participants.
Table 1.
Demographic variables, symptom ratings and behavioral measures. Numbers in rounded brackets are standard deviations (SD).
| Patients | Controls | Comparison P | |
|---|---|---|---|
| Demographics | |||
| Gender (M/F) | 8/8 | 8/8 | n.s. |
| Age in years | 36.1 (7.9) | 37.0 (7.8) | n.s. |
| Parental years of education | 12.2 (2.0) | 13.1 (3.0) | n.s. |
| Years of education | 13.8 (3.5) | 17.0 (1.8) | < 0.01 |
| Symptoms (PANSS) | |||
| Positive | 14.7 (5.6) | ||
| Negative | 15.9 (4.9) | ||
| General | 29.9 (10.8) | ||
| Behavioral tests | |||
| Mean perceptual closure (OPC and VPC) | 19.3 (5.8) | 23.4 (3.2) | 0.023 |
| Psychomotor Speed in sec | 47.8 (33.6) | 30.1 (13.4) | n.s. |
| Semantic knowledge (items correct) | 29.1 (5.1) | 28.1 (4.3) | n.s. |
2.2. Assessment of visual perceptual closure
To assess visual perceptual closure, we assessed objective performance on two speed-of-closure tests, which we have used in previous studies (Oertel et al., 2009, Sack et al., 2005). The perceptual closure tests are part of a larger general intelligence test battery (Horn, 1983) that comprises high retest reliability (rtt = 0.95). We assessed object-based perceptual closure speed (OPC, retest reliability, rtt = 0.71) and verbal-based perceptual closure speed (VPC, rtt = 0.88). The OPC consists of 40 sketches of common objects (e.g. car, apple, house), in which some pictorial parts are erased, and participants are required to recognize and name the respective objects. The VPC consists of 40 visually degraded words, in which each word contains one false letter, which has to be identified and crossed out. Performance for each of the tests is limited to a time constraint of 1 min. Perceptual closure performance is scored as the number of correctly identified items within the restricted time. Because performance on the two speed-of-closure tests are commonly highly correlated, as was the case in our study (r = 0.65, P < 0.001), the scores were averaged between the two tests to obtain a single measure of perceptual closure.
The perceptual closure tests contain elements of psychomotor speed and semantic knowledge. To control for possible group effects in these cognitive domains, we also assessed the German equivalent (Gaussmann et al., 1978, Oswald, 1986) of the Trail Making Test A (TMT-A (Reitan, 1958)) and the German equivalent (Gaussmann et al., 1978) of the Spot-the-Word-Test (SWT (Baddeley et al., 1993)). In the TMT-A, the material comprises two matrices of numbers that are arranged in random order and participants must connect the numbers in ascending order. Psychomotor speed performance is scored as the mean speed in seconds to complete the matrices. In the SWT, participants must identify a word amongst nonsense-word distractors. Semantic knowledge is scored as the number of correctly identified words. Both psychometric tests possess high test-retest reliability (TMTA: rtt = 0.95; SWT: rtt = 0.87). All tests were completed within seven days prior to scanning.
2.3. Image acquisition
MRI measurements were performed on a 3 Tesla Siemens Allegra. T1-weighted anatomical data were obtained using 3D Modified Driven Equilibrium Fourier Transform (MDEFT) sequence (Deichmann et al., 2004, Lee et al., 1995) with 176 slices and 1 × 1 × 1 mm3 voxel size. Functional T2*-weighted resting-state images were acquired using an EPI sequence (TR/TE 1000/30 ms, flip angle 60°, 16 slices, 400 volumes, 3.1 × 3.1 × 5 mm3). Participants were instructed to lie still during image acquisition with their eyes open and fixate a white cross presented in the center of the visual field.
2.4. Data preprocessing and analysis
The data were analyzed using BrainVoyager QX (Goebel et al., 2006) and in-house software that used functionalities of the NeuroElf toolbox (www.neuroelf.net) implemented in Matlab (The MathWorks, Natick, MA, U.S.A.). Functional data were preprocessed using slice scan time correction, spatial smoothing with a 6 mm FWHM Gaussian kernel, linear trend removal and high pass filtering of 0.0025 Hz per functional run. The data were aligned to anatomical images and resampled to 3 × 3 × 3 mm3 in a standardized 3D Talairach space. Anatomical images were averaged across participants, and an average brain volume mask was created.
2.5. Functional connectivity analysis
Analysis of resting-state functional connectivity was conducted using self-organized grouping sICA (sogICA) (Esposito et al., 2005, van de Ven et al., 2008) to decompose individual time series into 45 spatial components and temporal profiles (using Infomax algorithm (Bell and Sejnowski, 1995)) and cluster the results in the subject space to obtain group representations of the spatial modes. Spatial components and associated temporal profiles were Z-normalized (McKeown et al., 1998). Component clustering in the subject space was performed using hierarchical clustering with spatial similarity as input to the clustering algorithm to obtain 45 clusters of 32 spatial maps. Each participant contributed one spatial map to a cluster. For each cluster, a representative cluster spatial map was obtained by calculating one-sample t-tests of the component values for each voxel (i.e., ignoring group member ship of the cluster members). We then selected by visual inspection the spatial cluster map that best represented early visual cortex, referred to here as the visual RSN, for further analysis. Importantly, this selection was made at the end of the sogICA clustering procedure in order to minimize subjective selection of individual components (Esposito et al., 2005, van de Ven et al., 2008).
We then regressed the temporal profile of the individual components of the visual RSN in a multiple regression analysis for each participant's resting-state time series. Visual RSN regressors were supplemented with FMRI covariates that included time series sampled from the ventricles and from white matter, global signal and six head-volume rotation and translation parameters for each participant (Birn et al., 2006, Fox et al., 2005). The regression fits of the visual RSN were interpreted as linear fits of functional connectivity. Analysis of the absolute values of the six head movement parameters revealed no systematic differences between the two groups (P > 0.6).
A multi-subject representation of the visual RSN was calculated by a one-sample t-test of functional connectivity maps. The statistical summary map was thresholded for visualization at a false-discovery rate (FDR (Genovese et al., 2002)) of q = 0.01 and a minimum region-size threshold of 270 mm3 (arbitrarily chosen to minimize isolated voxels and bias results towards contiguous clusters surviving the FDR correction). This map also served as a statistical voxel map to empirically restrict voxel-based analysis of functional connectivity to visual RSN areas.
2.5.1. Global and local connectivity
Group differences of connectivity were assessed at the global (that is, map-based) and local level (that is, voxel-based). For the global-level analysis, we calculated a spatial goodness-of-fit (SGI) index (Esposito et al., 2008, Greicius et al., 2004) as the spatial correlation of an individual's visual RSN to a leave-one-out template of the multi-subject visual RSN (Esposito et al., 2008). In the leave-one-out procedure, the template was calculated as the mean of the visual RSNs of all participants with the exception of the one to which the template is compared to. The ensuing correlation values were normalized using Fisher's Z transformation and then used as a dependent variable in subsequent analyses with Group as independent factor.
For the local-level analysis, the distributions of voxel-based connectivity values were analyzed with Group as independent factor in a voxel-by-voxel manner. Only voxels that were tagged by the thresholded multi-subject map were investigated, which amounted to < 15% of all brain voxels. The resulting statistical map was thresholded at q(FDR) = 0.05.
To simplify the ROI analysis, we pooled voxel clusters according to early vs. higher-level visual areas, which largely coincides with the psychophysical results of visual perceptual deficits in schizophrenia (e.g., (Silverstein and Keane, 2011)). Voxel clusters at or near the calcarine fissure were pooled into an early visual ROI. Voxel clusters in extrastriate and inferotemporal areas were pooled into a higher-visual ROI.
2.5.2. Associations with perceptual closure
We analyzed associations between visual RSN and perceptual closure using correlation analysis at the global and local level. Within the patient group, we also correlated symptom ratings with the perceptual closure scores.
2.5.3. Associations with psychopathology
Finally, we analyzed whether psychopathology was associated with visual RSN connectivity in patients by correlating the symptom ratings for positive, negative and general symptoms to functional connectivity coefficients at the global and local level. This analysis was conducted as an exploratory analysis, following up on previously reported correlations between intrinsic connectivity and psychopathology ratings (e.g., (Oertel-Knöchel et al., 2014, Shinn et al., 2013, Whitfield-Gabrieli et al., 2009)).
3. Results
3.1. Behavioral test performance
Behavioral test scores of one control participant were not logged correctly, and were therefore excluded from analysis. Table 1 provides an overview of the demographic values and behavioral performance on the perceptual closure, psychomotor speed and semantic knowledge tests. Patients did not significantly differ from the control group on age, gender, handedness and parental years of education. However, patients had lower years of education than controls (P = 0.004).
Patient performance on perceptual closure was worse (mean [SD] = 19.3 [5.8]) compared to control participants (23.4 [3.2]), and this difference was significant (T[29] = 2.4, P = 0.023). Perceptual closure scores did not correlate with years of education (P > 0.4). Further, patients performed slower on the psychomotor speed test (mean [SD] = 47.8 [33.6]) compared to controls (30.1 [13.4]), but this difference did not reach significance (P = 0.068). Finally, performance on the semantic knowledge test was not significantly different (P = 0.59).
Because of the significant difference in years of education and the close-to-significant effect on psychomotor speed, we removed the covariance of these measures from the subsequent functional connectivity analyses by means of least squares regression.
3.2. Visual RSN
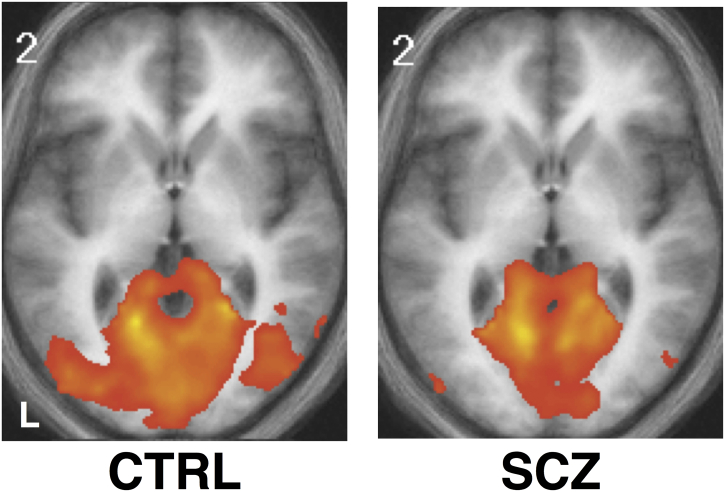
A multi-subject map of the visual RSN of patients (one-sample t-test, thresholded at q = 0.05 and minimum region-size threshold of 270 mm3) showed significant functional connectivity in bilateral striate and extrastriate visual cortex, including medial and lateral occipital gyri, inferior temporal areas and parahippocampal gyri (see Fig. 1). This map was very similar to the multi-subject map of the control participants, as indicated by the high spatial correlation between the two maps (r = 0.70). We used the one-sample t-test map of all participants combined as a voxel mask for subsequent analyses.
Fig. 1.
Visual RSN group maps. Shown are the thresholded (q(FDR) = 0.05) one-sample t-test maps of the visual RSNs for healthy control participants (A) and schizophrenia patients (B) superimposed on the average anatomical image of all participants. White number at left-top of each panel indicates Talairach Z coordinate. Left hemisphere is depicted on the left of each image.
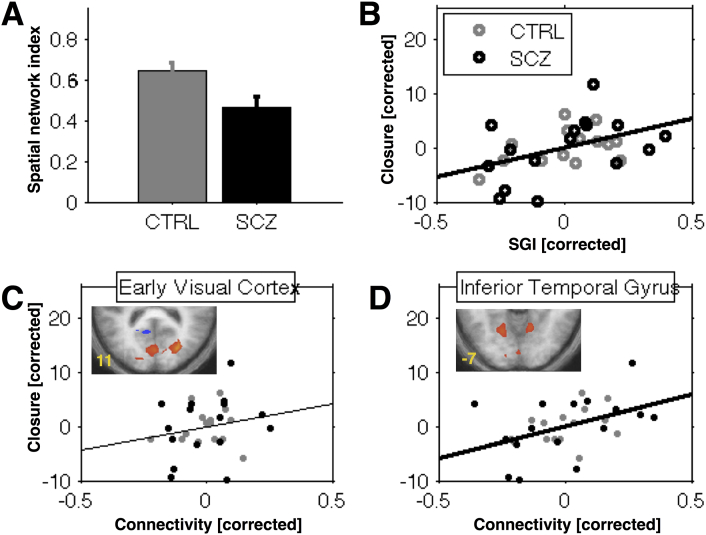
We assessed between-group effects on a global and local level. For the global level, the spatial goodness-of-fit index (SGI) was significantly (T[29] = 2.5, P = 0.017) lower for patients (mean [SD] = 0.47 [0.22]) compared to controls (0.65 [0.17]) (see Fig. 2A). This result indicated that within the visual RSN the degree of network-wide functional connectivity in patients was less strong or consistent than in controls.
Fig. 2.
Visual RSN and perceptual closure. (A) Spatial Goodness-of-fit index (SGI) of visual RSN was lower for patients (black bar) than for healthy controls (gray bar). (B) SGI values correlated with perceptual closure performance across both groups. SGI and perceptual closure scores were corrected for Group because both showed a significant difference between groups (see main text). (C, D) Regional functional connectivity values in inferior temporal areas (D), but not in early visual areas (C), correlated with perceptual closure performance. Connectivity values and perceptual closure scores were corrected for Group. Error bars indicate 1 SEM. Thick regression line indicates a significant linear association (P < 0.05).
At the local level, the voxel-by-voxel group comparison within the visual RSN revealed several voxel clusters of significant difference in connectivity around the calcarine fissure, the anatomical marker for striate cortex, lateral occipital cortex and inferior temporal gyri, extending into parahippocampal regions. Table 2 lists the coordinates and sizes of the clusters. The regional results reflected widespread changes within the visual RSN, which mostly was in the direction of decreased connectivity in patients compared to controls, thereby corroborating the global connectivity results. That is, visual cortex connectivity in schizophrenia is reduced in strength, rather than increased network heterogeneity. To focus the analysis on key visual sensory processing areas, we pooled areas according to homologue location in the left and right hemisphere for cuneus (region-of-interest for early visual processing) and inferior temporal gyrus (region-of-interest for higher order visual processing), which we used for further analysis.
Table 2.
Visual RSN regional differences. Clusters were obtained from a between-group voxel-by-voxel analysis of the visual RSN (thresholded at q(FDR) = 0.05). Coordinates are in standardized Talairach space. Contrast specifies the direction of the effect.
| ROI | L/R | x y z [mm] | Size [mm] | Contrast |
|---|---|---|---|---|
| Cuneus | L | 6 − 79 22 | 192 | C > P |
| R | − 15 − 85 4 | 99 | C > P | |
| ITG | L | − 18 − 61 − 5 | 27 | C > P |
| R | 12 − 58 − 8 | 10 | C > P | |
| MTG | R | 42 − 70 22 | 46 | C < P |
| PCC | L | − 9 − 43 7 | 34 | C < P |
3.3. Association with perceptual closure
Initial correlation analysis between perceptual closure scores and the global network index showed that higher global connectivity was associated with increased perceptual closure performance across both groups (SGI, r = 0.55, P = 0.002). However, because both measures significantly differed between the two groups, we regressed out the Group factor from both measures. The correlation between the two corrected measures remained significant (r = 0.41, P = 0.011) (see Fig. 2B).
We also correlated the perceptual closure scores with the functional connectivity values of the two bilateral visual RSN regions. A significant correlation was found for bilateral ITG (r = 0.53, P < 0.001) and for bilateral cuneus (r = 0.39, P = 0.014), indicating that higher connectivity was associated with better perceptual closure performance. To rule out the possibility that these correlations were confounded by Group factor, we regressed out Group factor and recalculated the correlations for both regions. We again found a significant correlation corrected for Group in bilateral ITG (r = 0.40, P = 0.014; see Fig. 2D) but not for early visual cortex (Fig. 2C).
Finally, we assessed how perceptual closure performance correlated with symptom ratings. Perceptual closure performance in patients correlated negatively with positive symptom severity (r = − 0.66, P = 0.005), such that higher positive symptom severity was associated with decreased perceptual closure performance. We did not find significant associations between perceptual closure and negative or general symptom ratings (Ps > 0.05). Moreover, perceptual closure performance in patients was not associated with patient age (P > 0.6), illness duration (P > 0.8) or medication (dosage in chlorpromazine equivalent mg/day, mean [SD] = 651.5 [296.3], P > 0.9).
3.4. Association between intrinsic connectivity and psychopathology
We found no significant correlations between positive, negative or general PANSS scores and global or local functional connectivity.
4. Discussion
We compared perceptual closure performance and functional connectivity of the visual RSN in schizophrenia patients to that of matched healthy control participants. We found that patients performed worse on perceptual closure than did healthy controls, independent of psychomotor speed or semantic knowledge. This finding corresponds to previous reports of impaired perceptual closure in schizophrenia (Doniger et al., 2001, Oertel et al., 2009, Sack et al., 2005, Uhlhaas and Mishara, 2007).
Moreover, we found that strength of functional connectivity was diminished throughout the visual RSN in patients compared to controls, including early and higher-level visual areas. These findings correspond to a previous report of reduced low frequency amplitudes during resting state in patients with schizophrenia and schizoaffective disorder compared to healthy controls (Hoptman et al., 2010). Our results expand on these findings by showing that resting state FMRI can identify aberrant functional connectivity beyond moments of task-related visual perception.
Further, our finding of decreased functional connectivity in early as well as higher-order visual areas fits to previous reports of impaired visual sensory processing. Reports of diminished magnocellular pathway responses (Butler et al., 2007, Butler et al., 2005, Martinez et al., 2008), impaired performance in visual contextual tasks (Dakin et al., 2005, Yoon et al., 2009) and visual illusions (Kantrowitz et al., 2009) indicate deficits in neural pathways at the level of primary visual cortex or before, at subcortical levels. At the same time, schizophrenia patients have also shown impairments for stimuli of higher-order perceptual organization, such as in Gestalt perception of faces (Butler et al., 2008, Uhlhaas et al., 2006a) or perceptual closure of objects (Doniger et al., 2001, Oertel et al., 2009, Sack et al., 2005). The functional relevance of visual cortical connectivity is further supported by the observed correlation between perceptual closure scores and functional connectivity strength in higher-level but not in early visual areas. The perceptual closure tests included degraded visual objects and word forms, which are processed in inferior temporal areas rather than in early visual cortex (Grützner et al., 2010, Ploran et al., 2007, Sehatpour et al., 2006). It is conceivable that performance on perceptual organization tasks that tap into subcortical and early visual processes (e.g., (Butler et al., 2007, Martinez et al., 2008)) may show a stronger correlation with intrinsic connectivity in early visual areas, rather than inferior temporal cortical connectivity. Yet, it is also likely that a deficit at one level of the visual hierarchy influences processing at another level. For example, deficits in magnocellular pathways can result in noisy processing at higher levels of visual representation (Demb et al., 1998), while top-down processing such as visual attention can alter processing at primary visual (Kastner and Ungerleider, 2000) and even subcortical levels (O'Connor et al., 2002). Our study did not use other perceptual tasks that may be sensitive to higher or lower levels of visual processing, which precludes further insight into this issue. Future studies are required to test the functional specificity of intrinsic visual cortical connectivity and its role in the pathophysiology of schizophrenia.
Our findings of decreased connectivity in schizophrenia are in line with a growing body of reports that show widespread impairments in intrinsic connectivity in schizophrenia (Alderson-Day et al., 2016, Menon, 2011, Northoff and Qin, 2011). In particular, the default-mode network (DMN), salience network (SN) and the central executive network (CEN) seem to be affected in psychotic patients, compared to healthy controls, and which may be related to symptomatology and higher-order cognitive impairments in patients (Alonso-Solís et al., 2012, Orliac et al., 2013, Palaniyappan et al., 2013, Rotarska-Jagiela et al., 2010, Whitfield-Gabrieli et al., 2009, Woodward et al., 2011). In turn, aberrantly connected networks may impair sensory information processing, thereby playing a role in perceptual impairments as well. For example, one study showed that, in first-episode psychosis patients, the DMN's posterior cingulate cortex was less strongly connected to visual areas, including inferior temporal and cuneus areas, compared to age and gender-matched controls (Alonso-Solís et al., 2012). Yet, aberrant connectivity between visual and other RSNs in schizophrenia is not a common finding. We also did not find aberrant connectivity between the visual and non-visual brain areas in our study. However, we note that differences in patient sample and analytical approaches between the two studies make comparison of results difficult.
It is currently unknown how the association between impaired visual processing and disrupted intrinsic functional connectivity is related to pathogenic factors in schizophrenia. Impairments in perceptual organization are not generally observed in most other mental disorders, such as bipolar disorder (Keri et al., 2005) or non-psychotic disorders (Uhlhaas et al., 2005). Conversely, we and others previously showed impaired perceptual closure performance in clinically unaffected relatives of patients with schizophrenia (Kim et al., 2010, Oertel et al., 2009), suggesting that closure deficits may be associated to the pathogenic mechanism of schizophrenia. Our use of intrinsic connectivity measures may be a useful method in further investigating how perceptual processing impairments are related to schizophrenia. Indeed, several resting-state FMRI studies showed impairments in non-clinical at-risk groups that were similar to those observed in schizophrenia patients (Oertel-Knöchel et al., 2013, Peeters et al., 2015, Whitfield-Gabrieli et al., 2009).
Finally, we found that impaired perceptual closure performance was associated with increased positive symptom severity in patients. It has been suggested that perceptual closure tasks tap into processes that integrate sensory evidence with top-down executive and memory functions (Javitt, 2009, Silverstein and Keane, 2011), which may also play a role in the generation of psychotic symptoms in schizophrenia (Frith, 2000). Our finding appears in line with this postulation. Further support comes from a previous study that used a Gestalt perception task based on inverted faces and reported that decreased Gestalt perception was associated with increased positive symptom ratings, including hallucinations (Uhlhaas et al., 2006a). However, other studies that used comparable tasks reported decreased task performance in association with increased negative (Doniger et al., 2002) or disorganization symptoms (Uhlhaas et al., 2006b), which suggests that the putative link between visual impairments and positive symptoms may not be very specific. A dedicated and high-powered study using one or more perceptual closure tasks and detailed clinical phenotyping in schizophrenia is required to resolve this issue.
We carefully controlled our study for known confounding effects. Our results appear not to be confounded by use of antipsychotic medication in patients, as correlations between medication dosage and perceptual closure performance were not significant. Also, we carefully matched the two participant groups on various demographic variables, and controlled for confounding effects of differences in years of education and psychomotor speed between the groups. Finally, the confounding effects of head motion in resting state analysis has been fiercely debated over recent years (Power et al., 2012, Turner et al., 2015, van Dijk et al., 2012). Particularly, schizophrenia patients may show more frequent and larger head movements compared to healthy controls, which could spuriously amplify differences between groups (Callicott and Weinberger, 1999). In our study, we found no clear indication of systematically larger head movements in patients than in controls. Also, we controlled for individual head movement in all participants in the functional connectivity analysis, following previous recommendations.
In conclusion, we found impaired functional connectivity in visual RSN in schizophrenia, which was associated with impaired perceptual closure performance. The association was strongest in higher-order visual areas, which fits to the visual object-related nature of the closure task that we used. Visual RSN abnormalities may be a causative factor in explaining visual processing deficits in schizophrenia.
Conflict of interest
D.E.J.L. was an associate editor of Neuroimage: Clinical at the time of this manuscript's original submission and took over as co-editor-in-chief when it had already entered the evaluation process. He has taken no part in the editorial evaluation of this manuscript. The other authors declare no conflict of interest in this work.
References
- Albert N.B., Robertson E.M., Miall R.C. The resting human brain and motor learning. Curr. Biol. 2009;19:1023–1027. doi: 10.1016/j.cub.2009.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderson-Day B., Diederen K., Fernyhough C., Ford J.M., Horga G., Margulies D.S., McCarthy-Jones S., Northoff G., Shine J.M., Turner J., van de Ven V., van Lutterveld R., Waters F., Jardri R. Auditory hallucinations and the Brain's resting-state networks: findings and methodological observations. Schizophr. Bull. 2016 doi: 10.1093/schbul/sbw078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso-Solís A., Corripio I., de Castro-Manglano P., Duran-Sindreu S., Garcia-Garcia M., Proal E., Nuñez-Marín F., Soutullo C., Alvarez E., Gómez-Ansón B., Kelly C., Castellanos F.X. Altered default network resting state functional connectivity in patients with a first episode of psychosis. Schizophr. Res. 2012;139:13–18. doi: 10.1016/j.schres.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen N.C. A unitary model of schizophrenia. Arch. Gen. Psychiatry. 1999;56:781–787. doi: 10.1001/archpsyc.56.9.781. [DOI] [PubMed] [Google Scholar]
- Baddeley A.D., Emslie H., Nimmo-Smith I. The spot-the-word test: a robust estimate of verbal intelligence based on lexical decision. Br. J. Clin. Psychol. 1993;32:55–65. doi: 10.1111/j.2044-8260.1993.tb01027.x. [DOI] [PubMed] [Google Scholar]
- Bar M. A cortical mechanism for triggering top-down facilitation in visual object recognition. J. Cogn. Neurosci. 2003;15:600–609. doi: 10.1162/089892903321662976. [DOI] [PubMed] [Google Scholar]
- Bassett D.S., Bullmore E.T. Human brain networks in health and disease. Curr. Opin. Neurol. 2009;22:340–347. doi: 10.1097/WCO.0b013e32832d93dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell A.J., Sejnowski T.J. An information-maximization approach to blind separation and blind deconvolution. Neural Comput. 1995;7:1129–1159. doi: 10.1162/neco.1995.7.6.1129. [DOI] [PubMed] [Google Scholar]
- Birn R.M., Diamond J.B., Smith M.A., Bandettini P.A. Separating respiratory-variation-related fluctuations from neuronal-activity-related fluctuations in fMRI. NeuroImage. 2006;31:1536–1548. doi: 10.1016/j.neuroimage.2006.02.048. [DOI] [PubMed] [Google Scholar]
- Butler P.D., Zemon V., Schecter I., Saperstein A.M., Hoptman M.J., Lim K.O., Revheim N., Silipo G., Javitt D.C. Early-stage visual processing and cortical amplification deficits in schizophrenia. Arch. Gen. Psychiatry. 2005;62:495–504. doi: 10.1001/archpsyc.62.5.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler P.D., Martinez A., Foxe J.J., Kim D., Zemon V., Silipo G., Mahoney J., Shpaner M., Jalbrzikowski M., Javitt D.C. Subcortical visual dysfunction in schizophrenia drives secondary cortical impairments. Brain. 2007;130:417–430. doi: 10.1093/brain/awl233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler P.D., Silverstein S.M., Dakin S.C. Visual perception and its impairment in schizophrenia. Biol. Psychiatry. 2008;64:40–47. doi: 10.1016/j.biopsych.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callicott J.H., Weinberger D.R. Neuropsychiatric dynamics: the study of mental illness using functional magnetic resonance imaging. Eur. J. Radiol. 1999;30:95–104. doi: 10.1016/s0720-048x(99)00048-0. [DOI] [PubMed] [Google Scholar]
- Cordes D., Haughton V.M., Arfanakis K., Carew J.D., Turski P.A., Moritz C.H., Quigley M.A., Meyerand M.E. Frequencies contributing to functional connectivity in the cerebral cortex in “resting-state” data. Am. J. Neuroradiol. 2001;22:1326–1333. [PMC free article] [PubMed] [Google Scholar]
- Dakin S., Carlin P., Hemsley D. Weak suppression of visual context in chronic schizophrenia. Curr. Biol. 2005;15:822–824. doi: 10.1016/j.cub.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Deichmann R., Schwarzbauer C., Turner R. Optimisation of the 3D MDEFT sequence for anatomical brain imaging: technical implications at 1.5 and 3 T. NeuroImage. 2004;21:757–767. doi: 10.1016/j.neuroimage.2003.09.062. [DOI] [PubMed] [Google Scholar]
- Demb J.B., Boynton G.M., Best M., Heeger D.J. Psychophysical evidence for a magnocellular pathway deficit in dyslexia. Vis. Res. 1998;38:1555–1559. doi: 10.1016/s0042-6989(98)00075-3. [DOI] [PubMed] [Google Scholar]
- Doniger G.M., Foxe J.J., Murray M.M., Higgins B.A., Snodgrass J.G., Schroeder C.E., Javitt D.C. Activation timecourse of ventral visual stream object-recognition areas: high density electrical mapping of perceptual closure processes. J. Cogn. Neurosci. 2000;12:615–621. doi: 10.1162/089892900562372. [DOI] [PubMed] [Google Scholar]
- Doniger G.M., Silipo G., Rabinowicz E.F., Snodgrass J.G., Javitt D.C. Impaired sensory processing as a basis for object-recognition deficits in schizophrenia. Am. J. Psychiatry. 2001;158:1818–1826. doi: 10.1176/appi.ajp.158.11.1818. [DOI] [PubMed] [Google Scholar]
- Doniger G.M., Foxe J.J., Murray M.M., Higgins B.A., Javitt D.C. Impaired visual object recognition and dorsal/ventral stream interaction in schizophrenia. Arch. Gen. Psychiatry. 2002;59:1011–1020. doi: 10.1001/archpsyc.59.11.1011. [DOI] [PubMed] [Google Scholar]
- Esposito F., Scarabino T., Hyvärinen A., Himberg J., Formisano E., Comani S., Tedeschi G., Goebel R., Seifritz E., Di Salle F. Independent component analysis of fMRI group studies by self-organizing clustering. NeuroImage. 2005;25:193–205. doi: 10.1016/j.neuroimage.2004.10.042. [DOI] [PubMed] [Google Scholar]
- Esposito F., Aragri A., Pesaresi I., Cirillo S., Tedeschi G., Marciano E., Goebel R., Di Salle F. Independent component model of the default-mode brain function: combining individual-level and population-level analyses in resting-state fMRI. Magn. Reson. Imaging. 2008;26:905–913. doi: 10.1016/j.mri.2008.01.045. [DOI] [PubMed] [Google Scholar]
- Fiszbein A., Kay S.R., Opler L.A. The positive and negative syndrome scale for schizophrenia. Schizophr. Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Fox M.D., Raichle M.E. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat. Rev. Neurosci. 2007;8:700–711. doi: 10.1038/nrn2201. [DOI] [PubMed] [Google Scholar]
- Fox M.D., Snyder A.Z., Vincent J.L., Corbetta M., Van Essen D.C., Raichle M.E. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc. Natl. Acad. Sci. U. S. A. 2005;102:9673–9678. doi: 10.1073/pnas.0504136102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frith C. Explaining the symptoms of schizophrenia: abnormalities in the awareness of action. Brain Res. Rev. 2000;31:357–363. doi: 10.1016/s0165-0173(99)00052-1. [DOI] [PubMed] [Google Scholar]
- Gaussmann A., Hochhausen R., Schmidt-Rogge I. Der Mehrfachwahl-Wortschatz-Test (MWT) und der Zahlen-Verbindungs-Test (ZVT) als Masse der Allgemeinen Intelligenz. Diagnostica. 1978;24:50–77. [Google Scholar]
- Genovese C.R., Lazar N.A., Nichols T.E. Thresholding of statistical maps in functional neuroimaging using the false discovery rate. NeuroImage. 2002;15:870–878. doi: 10.1006/nimg.2001.1037. [DOI] [PubMed] [Google Scholar]
- Goebel R., Esposito F., Formisano E. Analysis of functional image analysis contest (FIAC) data with brainvoyager QX: from single-subject to cortically aligned group general linear model analysis and self-organizing group independent component analysis. Hum. Brain Mapp. 2006;27:392–401. doi: 10.1002/hbm.20249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greicius M.D., Srivastava G., Reiss A.L., Menon V. Default-mode network activity distinguishes Alzheimer's disease from healthy aging: evidence from functional MRI. Proc. Natl. Acad. Sci. U. S. A. 2004;101:4637–4642. doi: 10.1073/pnas.0308627101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grützner C., Uhlhaas P.J., Genc E., Kohler A., Singer W., Wibral M. Neuroelectromagnetic correlates of perceptual closure processes. J. Neurosci. 2010;30:8342–8352. doi: 10.1523/JNEUROSCI.5434-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoptman M.J., Zuo X.-N., Butler P.D., Javitt D.C., D'Angelo D., Mauro C.J., Milham M.P. Amplitude of low-frequency oscillations in schizophrenia: a resting state fMRI study. Schizophr. Res. 2010;117:13–20. doi: 10.1016/j.schres.2009.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn W. Hogrefe; Göttingen: 1983. LPS leistungsprüfsystem. [Google Scholar]
- Javitt D.C. Sensory processing in schizophrenia: neither simple nor intact. Schizophr. Bull. 2009 doi: 10.1093/schbul/sbp110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantrowitz J.T., Butler P.D., Schecter I., Silipo G., Javitt D.C. Seeing the world dimly: the impact of early visual deficits on visual experience in schizophrenia. Schizophr. Bull. 2009;35:1085–1094. doi: 10.1093/schbul/sbp100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastner S., Ungerleider L.G. Mechanisms of visual attention in the human cortex. Annu. Rev. Neurosci. 2000;23:315–341. doi: 10.1146/annurev.neuro.23.1.315. [DOI] [PubMed] [Google Scholar]
- Keri S., Kelemen O., Benedek G., Janka Z. Lateral interactions in the visual cortex of patients with schizophrenia and bipolar disorder. Psychol. Med. 2005;35:1043–1051. doi: 10.1017/s0033291705004381. [DOI] [PubMed] [Google Scholar]
- Kim H.S., Shin N.Y., Choi J.S., Jung M.H., Jang J.H., Kang D.H., Kwon J.S. Processing of facial configuration in individuals at ultra-high risk for schizophrenia. Schizophr. Res. 2010;118:81–87. doi: 10.1016/j.schres.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Lee J.-H., Garwood M., Menon R.S., Adriany G., Andersen P., Truwit C.L., Ugurbil K. High contrast and fast three-dimensional magnetic resonance imaging at high fields. Magn. Reson. Med. 1995;34:308–312. doi: 10.1002/mrm.1910340305. [DOI] [PubMed] [Google Scholar]
- Leopold D.A., Murayama Y., Logothetis N.K. Very slow activity fluctuations in monkey visual cortex: implications for functional brain imaging. Cereb. Cortex. 2003;13:422–433. doi: 10.1093/cercor/13.4.422. [DOI] [PubMed] [Google Scholar]
- Lewis C.M., Baldassarre A., Committeri G., Romani G.L., Corbetta M. Learning sculpts the spontaneous activity of the resting human brain. Proc. Natl. Acad. Sci. U. S. A. 2009;106:17558–17563. doi: 10.1073/pnas.0902455106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang M., Zhou Y., Jiang T., Liu Z., Tian L., Liu H., Hao Y. Widespread functional disconnectivity in schizophrenia with resting-state functional magnetic resonance imaging. Neuroreport. 2006;17:209–213. doi: 10.1097/01.wnr.0000198434.06518.b8. [DOI] [PubMed] [Google Scholar]
- Martinez A., Hillyard S.A., Dias E.C., Hagler D.J., Butler P.D., Guilfoyle D.N., Jalbrzikowski M., Silipo G., Javitt D.C. Magnocellular pathway impairment in schizophrenia: evidence from functional magnetic resonance imaging. J. Neurosci. 2008;28:7492–7500. doi: 10.1523/JNEUROSCI.1852-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeown M.J., Makeig S., Brown G.G., Jung T.-P., Kindermann S.S., Bell A.J., Sejnowski T.J. Analysis of fMRI data by blind separation into independent spatial components. Hum. Brain Mapp. 1998;6:160–188. doi: 10.1002/(SICI)1097-0193(1998)6:3<160::AID-HBM5>3.0.CO;2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn. Sci. 2011;15:483–506. doi: 10.1016/j.tics.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Meyer-Lindenberg A., Weinberger D.R. Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat. Rev. Neurosci. 2006;7:818–827. doi: 10.1038/nrn1993. [DOI] [PubMed] [Google Scholar]
- Northoff G., Qin P. How can the brain's resting state activity generate hallucinations? A “resting state hypothesis” of auditory verbal hallucinations. Schizophr. Res. 2011;127:202–214. doi: 10.1016/j.schres.2010.11.009. [DOI] [PubMed] [Google Scholar]
- O'Connor D.H., Fukui M.M., Pinsk M.A., Kastner S. Attention modulates responses in the human lateral geniculate nucleus. Nat. Neurosci. 2002;5:1203–1209. doi: 10.1038/nn957. [DOI] [PubMed] [Google Scholar]
- Oertel V., Rotarska-Jagiela A., van de Ven V., Haenschel C., Grube M., Stangier U., Maurer K., Linden D.E.J. Mental imagery vividness as a trait marker across the schizophrenia spectrum. Psychiatry Res. 2009;167:1–11. doi: 10.1016/j.psychres.2007.12.008. [DOI] [PubMed] [Google Scholar]
- Oertel-Knöchel V., Knöchel C., Matura S., Prvulovic D., Linden D.E.J., van de Ven V. Reduced functional connectivity and asymmetry of the planum temporale in patients with schizophrenia and first-degree relatives. Schizophr. Res. 2013 doi: 10.1016/j.schres.2013.04.024. [DOI] [PubMed] [Google Scholar]
- Oertel-Knöchel V., Knöchel C., Matura S., Stäblein M., Prvulovic D., Maurer K., Linden D.E.J., van de Ven V. Association between symptoms of psychosis and reduced functional connectivity of auditory cortex. Schizophr. Res. 2014;160:35–42. doi: 10.1016/j.schres.2014.10.036. [DOI] [PubMed] [Google Scholar]
- Orliac F., Naveau M., Joliot M., Delcroix N., Razafimandimby A., Brazo P., Dollfus S., Delamillieure P. Links among resting-state default-mode network, salience network, and symptomatology in schizophrenia. Schizophr. Res. 2013;148:74–80. doi: 10.1016/j.schres.2013.05.007. [DOI] [PubMed] [Google Scholar]
- Oswald W.D. Aspekte Psychologischer Forschung. Festschrift Zum 60. Geburtstag von Erwin Roth. 1986. Der Zahlen-Verbindungs-Test im höheren Lebensalter; pp. 377–388. [Google Scholar]
- Palaniyappan L., Simmonite M., White T.P., Liddle E.B., Liddle P.F. Neural primacy of the salience processing system in schizophrenia. Neuron. 2013;79:1–23. doi: 10.1016/j.neuron.2013.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters S.C.T., van Bronswijk S., van de Ven V., Gronenschild E.H.B.M., Goebel R., van Os J., Marcelis M. Cognitive correlates of frontoparietal network connectivity “at rest” in individuals with differential risk for psychotic disorder. Eur. Neuropsychopharmacol. 2015 doi: 10.1016/j.euroneuro.2015.08.007. [DOI] [PubMed] [Google Scholar]
- Ploran E.J., Nelson S.M., Velanova K., Donaldson D.I., Petersen S.E., Wheeler M.E. Evidence accumulation and the moment of recognition: dissociating perceptual recognition processes using fMRI. J. Neurosci. 2007;27:11912–11924. doi: 10.1523/JNEUROSCI.3522-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power J.D., Barnes K.A., Snyder A.Z., Schlaggar B.L., Petersen S.E. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage. 2012;59:2142–2154. doi: 10.1016/j.neuroimage.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reineberg A.E., Andrews-Hanna J.R., Depue B.E., Friedman N.P., Banich M.T. Resting-state networks predict individual differences in common and specific aspects of executive function. NeuroImage. 2015;104:69–78. doi: 10.1016/j.neuroimage.2014.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitan R. Validity of the Trail Making Test as an indicator of organic brain damage. Percept. Mot. Skills. 1958;8:271–276. [Google Scholar]
- Rotarska-Jagiela A., van de Ven V., Oertel-Knoechel V., Uhlhaas P.J., Vogeley K., Linden D.E.J. Resting-state functional network correlates of psychotic symptoms in schizophrenia. Schizophr. Res. 2010;117:21–30. doi: 10.1016/j.schres.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Sack A.T., van de Ven V.G., Etschenberg S., Schatz D., Linden D.E.J. Enhanced vividness of mental imagery as a trait marker of schizophrenia? Schizophr. Bull. 2005;31:97–104. doi: 10.1093/schbul/sbi011. [DOI] [PubMed] [Google Scholar]
- Seeley W.W., Menon V., Schatzberg A.F., Keller J., Glover G.H., Kenna H., Reiss A.L., Greicius M.D. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 2007;27:2349–2356. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sehatpour P., Molholm S., Javitt D.C., Foxe J.J. Spatiotemporal dynamics of human object recognition processing: an integrated high-density electrical mapping and functional imaging study of “closure” processes. NeuroImage. 2006;29:605–618. doi: 10.1016/j.neuroimage.2005.07.049. [DOI] [PubMed] [Google Scholar]
- Shinn A.K., Baker J.T., Cohen B.M., Öngür D. Functional connectivity of left Heschl's gyrus in vulnerability to auditory hallucinations in schizophrenia. Schizophr. Res. 2013;143:260–268. doi: 10.1016/j.schres.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmuel A., Leopold D.A. Neuronal correlates of spontaneous fluctuations in fMRI signals in monkey visual cortex: implications for functional connectivity at rest. Hum. Brain Mapp. 2008;29:751–761. doi: 10.1002/hbm.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein S.M., Keane B.P. Perceptual organization impairment in schizophrenia and associated brain mechanisms: review of research from 2005 to 2010. Schizophr. Bull. 2011;37:690–699. doi: 10.1093/schbul/sbr052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snodgrass J.G., Feenan K. Priming effects in picture fragment completion: support for the perceptual closure hypothesis. J. Exp. Psychol. Gen. 1990;119:276–296. doi: 10.1037//0096-3445.119.3.276. [DOI] [PubMed] [Google Scholar]
- Taubert M., Lohmann G., Margulies D.S., Villringer A., Ragert P. Long-term effects of motor training on resting-state networks and underlying brain structure. NeuroImage. 2011;57:1492–1498. doi: 10.1016/j.neuroimage.2011.05.078. [DOI] [PubMed] [Google Scholar]
- Turner B.O., Lopez B., Santander T., Miller M.B. One dataset, many conclusions: BOLD variability's complicated relationships with age and motion artifacts. Brain Imaging Behav. 2015:115–127. doi: 10.1007/s11682-014-9351-7. [DOI] [PubMed] [Google Scholar]
- Uhlhaas P.J., Mishara A.L. Perceptual anomalies in schizophrenia: integrating phenomenology and cognitive neuroscience. Schizophr. Bull. 2007;33:142–156. doi: 10.1093/schbul/sbl047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas P.J., Phillips W.A., Silverstein S.M. The course and clinical correlates of dysfunctions in visual perceptual organization in schizophrenia during the remission of psychotic symptoms. Schizophr. Res. 2005;75:183–192. doi: 10.1016/j.schres.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Uhlhaas P.J., Linden D.E.J., Singer W., Haenschel C., Lindner M., Maurer K., Rodriguez E. Dysfunctional long-range coordination of neural activity during Gestalt perception in schizophrenia. J. Neurosci. 2006;26:8168–8175. doi: 10.1523/JNEUROSCI.2002-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas P.J., Phillips W.A., Mitchell G., Silverstein S.M. Perceptual grouping in disorganized schizophrenia. Psychiatry Res. 2006;145:105–117. doi: 10.1016/j.psychres.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Urner M., Schwarzkopf D.S., Friston K., Rees G. Early visual learning induces long-lasting connectivity changes during rest in the human brain. NeuroImage. 2013;77:148–156. doi: 10.1016/j.neuroimage.2013.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Ven V. Brain functioning when the voices are silent - Aberrant default-mode and disrupted connectivity in auditory verbal hallucinations. In: Jardri R., Cachia A., Thomas P., Pins D., editors. The Neuroscience of Hallucinations. Springer; New York, NY: 2012. pp. 393–415. [Google Scholar]
- van de Ven V.G., Formisano E., Prvulovic D., Roeder C.H., Linden D.E.J. Functional connectivity as revealed by spatial independent component analysis of fMRI measurements during rest. Hum. Brain Mapp. 2004;22:165–178. doi: 10.1002/hbm.20022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Ven V., Bledowski C., Prvulovic D., Goebel R., Formisano E., di Salle F., Linden D.E.J., Esposito F. Visual target modulation of functional connectivity networks revealed by self-organizing group ICA. Hum. Brain Mapp. 2008;29:1450–1461. doi: 10.1002/hbm.20479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijk K.R.A., Sabuncu M.R., Buckner R.L. The influence of head motion on intrinsic functional connectivity MRI. NeuroImage. 2012;59:431–438. doi: 10.1016/j.neuroimage.2011.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield-Gabrieli S., Thermenos H.W., Milanovic S., Tsuang M.T., Faraone S.V., McCarley R.W., Shenton M.E., Green A.I., Nieto-Castanon A., LaViolette P., Wojcik J., Gabrieli J.D.E., Seidman L.J. Hyperactivity and hyperconnectivity of the default network in schizophrenia and in first-degree relatives of persons with schizophrenia. Proc. Natl. Acad. Sci. U. S. A. 2009;106:1279–1284. doi: 10.1073/pnas.0809141106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen H., Zaudig M., Fydrich T. Hogrefe; Göttingen, Germany: 1997. Strukturiertes Klinisches Interview für DSM-IV. [Google Scholar]
- Woodward N.D., Rogers B.P., Heckers S. Functional resting-state networks are differentially affected in schizophrenia. Schizophr. Res. 2011;130:86–93. doi: 10.1016/j.schres.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon J.H., Rokem A.S., Silver M.a., Minzenberg M.J., Ursu S., Ragland J.D., Carter C.S. Diminished orientation-specific surround suppression of visual processing in schizophrenia. Schizophr. Bull. 2009;35:1078–1084. doi: 10.1093/schbul/sbp064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Long Z., Ge R., Xu L., Jin Z., Yao L., Liu Y. Motor imagery learning modulates functional connectivity of multiple brain Systems in Resting State. PLoS One. 2014;9:e85489. doi: 10.1371/journal.pone.0085489. [DOI] [PMC free article] [PubMed] [Google Scholar]