Abstract
The use of smartphones in clinical practice is steadily increasing with the availability of low cost/freely available "apps" that could be used to assess human gait. The primary aim of this manuscript is to test the concurrent validity of kinematic measures recorded by a smartphone application in comparison to a 3D motion capture system in the sagittal plane. The secondary aim was to develop a protocol for clinicians on the set up of the smartphone camera for video movement analysis.
The sagittal plane knee angle was measured during heel strike and toe off events using the smart phone app and a 3D motion-capture system in 32 healthy subjects. Three trials were performed at near (2-m) and far (4-m) smartphone camera distances. The order of the distances was randomized. Regression analysis was performed to estimate the height of the camera based on either the subject's height or leg length.
Absolute measurement errors were least during toe off (3.12 ± 5.44 degrees) compared to heel strike (5.81 ± 5.26 degrees). There were significant (p < 0.05) but moderate agreements between the application and 3D motion capture measures of knee angles. There were also no significant (p > 0.05) differences between the absolute measurement errors between the two camera positions. The measurement errors averaged between 3 - 5 degrees during toe off and heel strike events of the gait cycle.
The use of smartphone apps can be a useful tool in the clinic for performing gait or human movement analysis. Further studies are needed to establish the accuracy in measuring movements of the upper extremity and trunk.
Keywords: Medicine, Issue 121, smartphones, gait analysis, video movement analysis, sagittal plane measurements, knee goniometric measurements, physical therapy, kinematics
Introduction
Assessment of human gait is a key component of the physical therapy evaluation and clinical decision-making process.1 Gait assessment is a frequently used clinical tool to assess gait deficits in patients with neurological and musculoskeletal deficits. Reassessment of gait can then provide the clinician with information about the efficacy of an intervention in achieving the goals they had set at their initial evaluation. There is a nationally recognized need in the United States for physical therapists to utilize standardized outcome measurements when evaluating patients.2 This need stems from the rapidly changing landscape of insurance reimbursement policies, as well as an emphasized shift for physical therapists to rely more heavily on evidence based practices.3 There are numerous outcome measures to assess different aspects of gait, which can be observed in a number of ways including: visual observation by a clinician, functional assessments, video recorded measures, electronic walkways, three-dimensional motion analysis software, etc. In clinical settings, observational (visual) gait analysis is commonly performed, as it requires minimal equipment and time.
While observational gait analysis is commonly used within the clinic, it still remains a subjective assessment.4 Therefore, factors such as therapist experience, visual acuity, distance from the subject (camera distance), measurement tools, and any other such factors can introduce variability and error in the assessment. The potential for such variability presents a critical need for a more reliable means of measurement, which can ultimately be overcome by the use of valid instrumentation.5
Since its inception, videography and related technology has been used to examine various functional limitations resulting from impaired movement capability as well as a form of visual feedback. This is acutely true in regards to gait assessment. Stuberg et al. found that "videography equipment is commonly available in the clinic…and provides the clinician with additional objective information on posture and joint position during the gait cycle."4 As technology has continued to improve, so have the capabilities of video analysis. These capabilities provide the physical therapist with greater ability to clinically assess the various parameters of gait.
The two key parameters that physical therapists focus on include kinematic and spatiotemporal parameters. As the name implies, spatiotemporal measures involve elements of distance and time. Specific to a gait cycle, spatiotemporal measures would include, but not be limited to, stride length, step length, cadence, and velocity.6 Kinematic measures on the other hand focus on the joint movements/rotations of the lower extremities observed during each gait cycle.
A number of peer-reviewed articles have been published that have cited the use of video motion analysis as an outcome measure, specifically 2D camera systems, to assess kinematic, spatiotemporal, or a combination of both types of parameters. These articles have evaluated various clinical populations including individuals with a history of a stroke (CVA), traumatic brain injuries (TBI), spinal cord injuries (SCI), Parkinson's disease (PD), cerebral palsy (CP), and healthy individuals. The schematic presented below (Figure 1) provides the framework that was adopted to identify relevant peer-reviewed literature that has been published on this topic.
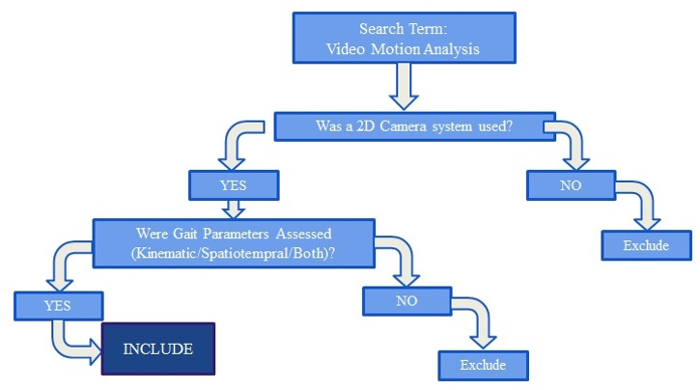 Figure 1. Schematic for Article Selection Criteria. The schematic outlines the steps used in choosing peer-reviewed articles to ascertain the type of variables that were reported in gait analysis. Please click here to view a larger version of this figure.
Figure 1. Schematic for Article Selection Criteria. The schematic outlines the steps used in choosing peer-reviewed articles to ascertain the type of variables that were reported in gait analysis. Please click here to view a larger version of this figure.
The majority of the research studies that have used video motion analysis for recording gait parameters were validation studies. Kinematic validation studies can be further broken down into one of three categories: assessing abnormal motion resulting from a specific diagnosis/pathology,7 examining joint angles during specific functional motions,8,9 and evaluating the effectiveness of treatment via comparison of pre-intervention motion and post-intervention motion.10,11 Similarly, research studies assessing spatiotemporal parameters can also be broken down into three categories: assessment of abnormal motion resulting from a specific pathology,12,13,14 examination of a platform during a specific functional activity,15,16 and determination of the effect of a specific intervention.17 The research studies that evaluated both kinematic and spatiotemporal parameters were primarily aimed at determining the effectiveness of specific treatment interventions such as orthoses17 or body weight/partial body weight supported treadmill training.18,19 A preliminary descriptive analysis of these articles determined that 52.1% of the studies (the sum of those looking solely at kinematics (30.4%) and those that examined a combination of parameters (21.7%)) researched kinematic parameters with a 2D camera system. This is in comparison to the 69.5% of the articles (sum of articles that researched spatiotemporal parameters (47.8%) and a combination of parameters (21.7%)) that assessed spatiotemporal parameters.
The methodological differences in recording and assessing kinematic and spatiotemporal gait parameters are also seen in clinical practice in terms of the type of observational gait analysis being used. Spatiotemporal parameters are assessed with much greater frequency as indicated by the research. There are three generally agreed upon reasons for this trend: low cost, ease of use, and the existence of a standard protocol to measure such parameters. Observational kinematic measurements have been shown to have very low intra-rater (60%) and inter-rater reliability (40% - 94%) in clinical settings.4 This wide range is understood to be due to the variation in the placement of markers on bony landmarks and the specific tools used to assess joint angles. Minute differences in location placement of the markers can significantly alter the resultant angles. Spatiotemporal measurements have much higher reliability (ranging 69% - 97%), especially when using the paper, pencil and stop clock method to assess gait.20
The technological advances in the last few decades have significantly changed the way healthcare is practiced. With the recent emergence of smartphones, access to the Internet, online research articles, and other electronic resources are now more readily available to clinicians at any time. Martin et al. reported that "general use of smartphones is increasing in clinical practice, medical education and research."21 In this study, more than 50% of medical doctors under the age of 35 responded that they have implemented using a smartphone in clinical practice. This trend increased in 2009 when 64% of physicians in the United States were found to be using smartphones in their clinical practice. The Manhattan Review study further predicted that this growth would continue to climb to 81% of physicians and healthcare clinicians implementing smartphone usage in clinical practice by 2012.22 While further research has not been conducted to determine if this upward trend has indeed continued to climb, it is reasonable to assume, with the known implementation of technology in healthcare, that the use of smartphone platforms in clinical practice will become more commonplace.
The current use of smartphone applications in physical therapy practice has not been established. There have been no studies evaluating the use of smartphone video analysis applications by a physical therapist to date. However, various smartphone applications have been used by individual physical therapists as a breakthrough assistive tool in outpatient orthopedic settings for use in both rehabilitating and training athletes of various disciplines. Smartphone apps are also available that can measure joint angles, some of which have been validated.23,24 Individual therapists have begun using various analysis applications on smartphones for visual feedback for the patient and for easier breakdown of various components that may be lacking in a patient's gait cycle, based on anecdotal evidence. However, the validity of these measures remains unknown. The limited research that does exist regarding these smartphone video analysis applications has focused on the validation of kinematic gait parameters, specifically ankle, knee and hip angles, in the frontal plane,25 and inter-rater reliability of the device.26 There are no studies to date that have validated the use of smartphone video analysis applications to record kinematics of gait in the sagittal plane, which is most commonly performed in clinical gait analysis.
The purpose of this study was to test the concurrent validity of kinematic measures recorded by the smartphone application and compare them to measures recorded by a 3D motion capture system in the sagittal plane. We predict that there will be no significant differences between the measures recorded by the smartphone application when compared to the measures recorded by the 3D motion capture system. The secondary purpose is to test if two distinct placements of the smartphone camera from the subject (near distance of 2-m; far distance of 4 -nt difference in measures between the two distinct placements of the smartphone camera. The final purpose of the study is to draft a protocol for clinical video gait analysis using a smartphone application.
Protocol
This protocol was approved by the Institutional Review Board of Wayne State University.
1. Experimental Preparation
- Position cameras to capture the entire 6-m walkway. Use a total of 4 3D motion captures cameras to capture walking over a 6-m walkway.
- Place each of the cameras at the 4 corners of the 6 m walkway. Orient each of the cameras at the diagonal ends of the walkway to face each other.
- Collect height, weight and leg length measures of each participant.
- Measure mass in kilograms.
- Measure leg length (in meters) from greater trochanter to medial malleoli of both legs with a measuring tape.
- Measure the height (in meters), by having the participant stand barefoot next to a measuring tape attached to the wall. Place a ruler on top of the participant's head to read the measurement from the measuring tape attached to the wall.
Mount the smartphone on a tripod with a tripod adapter for a smart phone holder clip. Place the tripod at 2-m or 4-m, perpendicular to the center of the walkway. Randomize the order of this placement if performing a validation study.
- Place clusters of 3 smart markers on the participant on bilateral anterior superior iliac crests (ASIS), upper 1/3 of thigh, upper 1/3 of calf and dorsum of foot. Place a single smart marker in midline between the right and left posterior superior iliac crests.
- Secure the smart markers with Velcro straps/double sided sticky tape. Secure thigh and calf markers in the frontal plane.
Place stickers indicating bony landmarks over bilateral medial and lateral femoral condyles, medial and lateral malleoli and the webspace between first and second toes for calibration of the 3D motion capture system. NOTE: The calibration procedure is specific to each laboratory, and 3D motion capture equipment and software.
For the calibration procedure, refer to the instructional manual provided by the manufacturer of the 3D motion capture equipment and/or software that is used to analyze the data. The process used here involves using an instrumented "Wand" with smart markers, to register the 3D location of the stickers that were placed.
2. Experiment
Adjust the smart phone camera lens height to capture either the participant's lower body only (ASIS as superior border) or upper and lower body (acromion as superior border). Measure the height from the floor to the camera lens in meters.
Give participants a practice trial. Have one investigator operate the smart phone, and the other operate the computer that controls the 3D motion capture system. Use numbered paper to indicate trial number on the smart phone recording.
Open the smart phone application. Press the red "record" button on the bottom, center of the screen to begin recording (when in vertical orientation). NOTE: If the smartphone has already been placed on the tripod, the button appears at the middle, right side of the phone, near the home button of the smartphone.
- Instruct the participant to walk at their normal pace, focused on a marker placed on opposite wall to assist them in walking a straight line. Place the smartphone parallel to the walkway to capture a side profile of the participant. Have the participant cross the first two 3D motion capture cameras placed at the beginning of the walkway on either side, and walk towards another two 3D motion capture cameras placed at the other end of the walkway on either side.
- For each trial, give each participant a countdown to start (3, 2, 1, GO) and end the trial (3, 2, 1, STOP).
After the subject finishes walking 6-m distance, select the red "record" button once more to finish recording this walking trial.
Check all markers for position after each trial. If a marker position was altered, return to step 1.6 to recalibrate the 3D motion capture system to the new marker placements.
Have participants perform 3 trials at each camera distance in step 2.1.
Move the tripod with the smart phone to the second distance. Return the participant to stand on the mid-point of the walk way. Follow instructions in protocol steps 2.2 - 2.5.
Save and verify the 3D motion capture recordings and smartphone recordings before removal of smart markers.
3. Data Analysis
Follow software/manufacturer's instructions to compute the knee angle. Manually record the knee angle that is displayed on the screen at heel strike and toe off phase of the gait cycle.
Complete the analysis of smart phone recordings for heel strike and toe off events captured by a team of two investigators, who have to agree on the moment of heel strike and toe off events and angle measurement land marks. Use a stylus for increased accuracy of landmark placement for knee angle measurements. The steps below are done jointly by the two investigators.
To view the trial that was just recorded, select the video square in the bottom left corner of the screen (in vertical orientation).
Using the scroll bar at the base of the screen, select the frame in which the subject is closest to heel strike or toe off (whichever is the preferred variable) in the center of the screen.
To drop in the angle, tap on the white, outlined pencil icon on the upper right side of the screen.
Select the angle option, the second option in the drop down menu.
Choose a preferred color and the angle maker. Please note that only one angle can be measured at one time. The angle measured in this protocol purely consisted of the knee angle in the sagittal plane.
Slide or tap the stylus anywhere on the screen to drop in the angle.
Place the center of the angle on the knee joint (lateral condyle), with the vectors reaching upwards along the femur and downwards towards the lateral malleoli.
If needed, "zoom in" by placing two fingers close together in the center of the screen and slowly drawing them apart from one another. NOTE: Once satisfied with the placement of the angle, the tool automatically calculates the knee angle at that given frame.
To identify the knee angle at other phases of toe off or heel strike, repeat steps 3.4 - 3.10.
4. Clinical Protocol
Measure and mark off a 6-m walkway using a measuring tape and marker/sticky tape.
Place the smartphone on a tripod parallel and close to the center of the 6-meter walkway.
Place the tripod 2 m away from the center of the walkway to capture the lower extremity, or 4 m away to capture the trunk and lower extremity. All camera positions allow only capture of sagittal plane kinematics.
Calculate the height of the smartphone camera lens height from the floor using the following formulae: Near camera configuration (2 m) for only lower extremity capture Camera lens height = (0.87xPatient's reference leg length in meters)- 0.12 Far camera configuration (4 meters) for both lower extremity and trunk capture Camera lens height = Patient's reference leg length in meters - 0.23
Repeat sections 2 - 3 to record and analyze data using the smart phone app.
Representative Results
All 32 subjects completed the 6 walking trials; however, data from 6 of the participants were not included in the data analysis due to technical problems resulting in poor marker visibility. The absolute measurement errors of knee angles were least during toe off events (3.12 ± 5.44 degrees) compared to heel strike (5.81 ± 5.26 degrees) (Table 1b). There were no statistically significant agreements (P > 0.05) between the smartphone application and 3D motion capture measures of knee angles. There were also no significant differences (P> 0.05) between the absolute measurement errors between the two camera positions (2.0 m and 4.0 m). The participants' leg length accounted for 40.4% variance of the height at which the smartphone camera was placed in the far distance (4.0 m, P < 0.0001), and 50% variance in the near distance (2.0 m, P < 0.0001).
Intraclass correlation (ICC) (2, k) analysis showed that the smartphone application measures showed low to moderate agreement especially during the Toe Off phase, when compared to those of the 3D capture system (Table 1a). At events Toe Off 1, Heel Strike 1 and Toe Off 2, for both near and far distances, the smartphone application showed moderate agreement. Improved agreement was observed at Toe Off 2, both in the near and far distances, with improved ICC values observed (Toe Off 2 Near ICC = 0.447, P < 0.05; Toe Off 2 Far ICC = 0.454, P < 0.05).
| Camera Position | Gait Phase | Mean Errors | Std. Deviation |
| Near | Heel Strike 1 | 5.74 | 8.49 |
| Heel Strike 2 | 6.36 | 4.14 | |
| Toe Off 1 | 3.93 | 5 | |
| Toe Off 2 | 2.49* | 4.99 | |
| Far | Heel Strike 1 | 4.97 | 5.58 |
| Heel Strike 2 | 5.47 | 3.6 | |
| Toe Off 1 | 2.71 | 5.64 | |
| Toe Off 2 | 2.54* | 4.69 |
Table 1: Intraclass Correlation Analysis with Significance Values (p-value). * indicates p < 0.05.
| Camera Position | Gait Phase | Intraclass Correlation | Significance |
| Near | Heel Strike 1 | 0.168 | 0.368 |
| Toe Off 1 | 0.324 | 0.126 | |
| Heel Strike 2 | 0.335 | 0.07 | |
| Toe Off 2 | 0.447 | .018* | |
| Far | Heel Strike 1 | 0.157 | 0.327 |
| Toe Off 1 | 0.284 | 0.084 | |
| Heel Strike 2 | 0.248 | 0.119 | |
| Toe Off 2 | 0.454 | .046* |
Table 2:Knee Angle Measurement Errors. Bland-Altman plots generated from the difference in measures between the application and motion capture systems offer visual evidence that suggests that differences are of a random nature, without any proportional errors being observed (Figures 2a & 2b). The plots for 2.0 m and 4.0 m distances display data that are more scattered around the mean difference line in the center. This indicates that the camera position did not contribute to the errors in measurements.
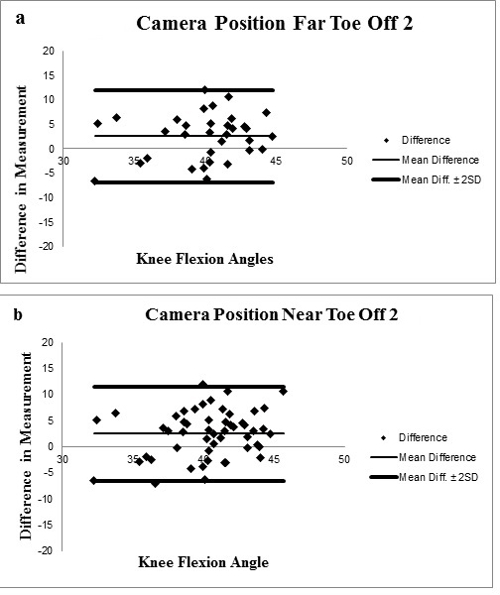 Figure 2.Bland and Altman Plots Showing the Difference between Measures Recorded by the App and 3D Motion Capture System During Toe off at Far and Near Camera Positions. a) Camera Position Far Toe Off 2. b) Camera Position Near Toe Off 2.
Figure 2.Bland and Altman Plots Showing the Difference between Measures Recorded by the App and 3D Motion Capture System During Toe off at Far and Near Camera Positions. a) Camera Position Far Toe Off 2. b) Camera Position Near Toe Off 2.
Discussion
The purpose of this validation study was to determine the validity of a freely available smartphone application in order to be clinically used as an objective and cost effective means of using smartphone technology for kinematic gait analysis in the clinical setting. Existing validation studies that examined kinematic measures with a smartphone application are limited and have not assessed dynamic kinematic measures recorded during gait in the sagittal plane. This validation study is the first to have examined kinematic knee measures in the sagittal plane with a smartphone. Additionally, this validation study is the first known to develop a protocol for kinematic gait analysis in the sagittal plane using a smartphone application for replication in the clinical setting.
Based on the results, there was a significant difference between knee angle measurements by the 3D motion capture system and smartphone application, which was to be expected. There is limited precision of measurements obtained by the smartphone in comparison to the capacity of the 3D motion capture system. The limited precision of the smartphone is based on the technological parameters that were available on the specific device when the study was performed. As technology continues to advance, the smartphone platforms may present with improved capture rates. The ability to slow video for analysis and capture still images within a moving frame may also improve the precision of kinematic analysis on available smartphone platforms. Incorporation of features such as high definition video recording, slow motion capture, quality of zoom and focus capacities may greatly improve the analysis of the extremity without distortion of the desired gait moment. Even though the precision of measurement influenced the knee measure obtained, no significant difference in measurement error was detected between the two camera distances. There was moderate agreement of the knee angle measurements during the toe off phase, indicating the increased agreement of knee flexion measure in comparison to agreement of knee extension or hyperextension measurement during heel strike.
On average, a 2 - 6 degree range of measurement error was detected. The range of error obtained in this study corresponds well with an established, clinically acceptable range of error. For example, multiple goniometric measures taken of an extremity by a single examiner has a range of 4 to 5 degrees.27,28 Further, the mean standard deviation of extremity goniometric measures taken by multiple examiners is 5 to 6 degrees. When compared to a study investigating capture of mechanical lifting in the sagittal plane, measurement error is also reflective of the clinically acceptable measure previously mentioned. In a study performed by Norris et al.5, the standard error of mean measured of the hip, knee and ankle during mechanical lifting was analyzed. There was 6.1 degrees of error for knee measurements. However, the measures obtained by Norris utilized a camcorder to record the measures with analysis on a computer with a smartphone compatible application. The measurement errors cannot be directly compared to the measures obtained in this study because all measures were both captured and analyzed on a smartphone. In order to replicate the results presented in this manuscript, all steps in the protocol must be followed as described. In particular Section 2 is critical to performing this validation technique and also obtaining a valid kinematic measure using the smartphone app. These steps outline the smartphone camera placement method and performing the kinematic measures.
In addition to the validation of smartphone use for kinematic joint measurement, this study has attempted to simplify and standardize the use of smartphone technology for gait analysis of the sagittal plane in the clinic. The investigators developed a protocol for a realistic reproduction of this study within a clinical space, using minimal and readily available equipment. The protocol includes parameters for the space needed, equipment needed, and necessary formulae to calculate patient specific setup for appropriate capture of the desired lower extremity segments. By following the setup outlined below, the investigators are relatively confident that clinicians will obtain valid kinematic measures with ± 5 degrees of error.
Disclosures
No relevant financial relationship exists with Hudl Technique (Ubersense). Adams Physical Therapy Clinic, Novi, MI were our clinical collaborators on this study.
Acknowledgments
The authors wish to thank all the participants who generously gave their time to participate in this study.
References
- Brunnekreef JJ, van Uden CJ, van Moorsel S, Kooloos JG. Reliability of videotaped observational gait analysis in patients with orthopedic impairments. BMC Musculoskelet Disord. 2005;6(17) doi: 10.1186/1471-2474-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89(2):125–135. doi: 10.2522/ptj.20080234. [DOI] [PubMed] [Google Scholar]
- Jette DU, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003;83(9):786–805. [PubMed] [Google Scholar]
- Stuberg WA, Colerick VL, Blanke DJ, Bruce W. Comparison of a Clinical Gait Analysis Method Using Videography and Temporal-Distance Measures with 16-Mm Cinematography. Phys Ther. 1988;68(8):1221–1225. [PubMed] [Google Scholar]
- Norris BS, Olson SL. Concurrent validity and reliability of two-dimensional video analysis of hip and knee joint motion during mechanical lifting. Physiother Theory Pract. 2011;27(7):521–530. doi: 10.3109/09593985.2010.533745. [DOI] [PubMed] [Google Scholar]
- Robinson JL, Smidt GL. Quantitative gait evaluation in the clinic. Phys Ther. 1981;61(3):351–353. doi: 10.1093/ptj/61.3.351. [DOI] [PubMed] [Google Scholar]
- Krystkowiak P, et al. Gait abnormalities induced by acquired bilateral pallidal lesions: a motion analysis study. J Neurol. 2006;253(5):594–600. doi: 10.1007/s00415-006-0066-6. [DOI] [PubMed] [Google Scholar]
- Grunt S, et al. Reproducibility and validity of video screen measurements of gait in children with spastic cerebral palsy. Gait Posture. 2010;31(4):489–494. doi: 10.1016/j.gaitpost.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Womersley L, May S. Sitting posture of subjects with postural backache. J Manipulative Physiol Ther. 2006;29(3):213–218. doi: 10.1016/j.jmpt.2006.01.002. [DOI] [PubMed] [Google Scholar]
- DeForge D, et al. Effect of 4-aminopyridine on gait in ambulatory spinal cord injuries: a double-blind, placebo-controlled, crossover trial. Spinal Cord. 2004;42(12):674–685. doi: 10.1038/sj.sc.3101653. [DOI] [PubMed] [Google Scholar]
- Lucareli PR, et al. Gait analysis following treadmill training with body weight support versus conventional physical therapy: a prospective randomized controlled single blind study. Spinal Cord. 2011;49(9):1001–1007. doi: 10.1038/sc.2011.37. [DOI] [PubMed] [Google Scholar]
- Lucareli PR, et al. [Gait analysis and quality of life evaluation after gait training in patients with spinal cord injury] Rev Neurol. 2008;46(7):406–410. [PubMed] [Google Scholar]
- McFadyen BJ, Swaine B, Dumas D, Durand A. Residual effects of a traumatic brain injury on locomotor capacity: a first study of spatiotemporal patterns during unobstructed and obstructed walking. J Head Trauma Rehabil. 2003;18(6):512–525. doi: 10.1097/00001199-200311000-00005. [DOI] [PubMed] [Google Scholar]
- Shin JC, Yoo JH, Jung TH, Goo HR. Comparison of lower extremity motor score parameters for patients with motor incomplete spinal cord injury using gait parameters. Spinal Cord. 2011;49(4):529–533. doi: 10.1038/sc.2010.158. [DOI] [PubMed] [Google Scholar]
- Reid S, Held JM, Lawrence S. Reliability and Validity of the Shaw Gait Assessment Tool for Temporospatial Gait Assessment in People With Hemiparesis. Arch Phys Med Rehabil. 2011;92(7):1060–1065. doi: 10.1016/j.apmr.2011.02.014. [DOI] [PubMed] [Google Scholar]
- Stokic DS, Horn TS, Ramshur JM, Chow JW. Agreement Between Temporospatial Gait Parameters of an Electronic Walkway and a Motion Capture System in Healthy and Chronic Stroke Populations. Am J Phys Med Rehabil. 2009;88(6):437–444. doi: 10.1097/PHM.0b013e3181a5b1ec. [DOI] [PubMed] [Google Scholar]
- Arazpour M, et al. Evaluation of a novel powered hip orthosis for walking by a spinal cord injury patient: a single case study. J. Prosthet. Orthot. Int. 2012;36(1):105–112. doi: 10.1177/0309364611431482. [DOI] [PubMed] [Google Scholar]
- Prado-Medeiros CL, et al. Effects of the addition of functional electrical stimulation to ground level gait training with body weight support after chronic stroke. Revista Brasileira De Fisioterapia. 2011;15(6):436–444. doi: 10.1590/s1413-35552011005000030. [DOI] [PubMed] [Google Scholar]
- Sousa CO, Barela JA, Prado-Medeiros CL, Salvini TF, Barela AM. Gait training with partial body weight support during overground walking for individuals with chronic stroke: a pilot study. J Neuroeng Rehabil. 2011;8(48) doi: 10.1186/1743-0003-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs DE, Edelstein JE, Fishman S. Reliability of observational kinamatic gait analysis. J Am Phys Ther Assoc. 1995;65:1027–1033. doi: 10.1093/ptj/65.7.1027. [DOI] [PubMed] [Google Scholar]
- Martin S. More than half of MDs under age 35 now using PDAs. Can. Med. Assoc. J. 2003;169(9):952. [PMC free article] [PubMed] [Google Scholar]
- Mosa AM, Yoo I, Sheets L. A Systematic Review of Healthcare Applications for Smartphones. BMC Med Inform Decis Mak. 2012;12 doi: 10.1186/1472-6947-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferriero G, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(2):146–151. doi: 10.1097/MRR.0b013e32835b8269. [DOI] [PubMed] [Google Scholar]
- Vohralik SL, Bowen AR, Burns J, Hiller CE, Nightingale EJ. Reliability and validity of a smartphone app to measure joint range. Am J Phys Med Rehabil. 2015;94(4):325–330. doi: 10.1097/PHM.0000000000000221. [DOI] [PubMed] [Google Scholar]
- Scholtes SS, Gretchen . Combined Sections Meeting. Las Vegas, USA: APTA; 2014. Ability to detect change in single leg squat movement patterns following instruction in females with patellofemoral pain using 2D motion analysis methods. [Google Scholar]
- Eltoukhy MA, Asfour S, Thompson C, Latta L. Evaluation of the performance of digital video analysis of human motion: dartfish tracking system. IJSER. 2012;3(3):1–6. [Google Scholar]
- Boone DC, et al. Reliability of goniometric measurements. Phys Ther. 1978;58(11):1355–1360. doi: 10.1093/ptj/58.11.1355. [DOI] [PubMed] [Google Scholar]
- Bovens AM, van Baak MA, Vrencken JG, Wijnen JA, Verstappen FT, editors. Variability and reliability of joint measurements. Am J Sports Med. 1990;18(1):58–63. doi: 10.1177/036354659001800110. [DOI] [PubMed] [Google Scholar]


