Abstract
Context
Obesity in men is associated with low serum testosterone and both are associated with several diseases and increased mortality.
Objectives
Examine the direction and causality of the relationship between body mass index (BMI) and serum testosterone.
Design
Bi-directional Mendelian randomization (MR) analysis on prospective cohorts.
Setting
Five cohorts from Denmark, Germany and Sweden (Inter99, SHIP, SHIP Trend, GOOD and MrOS Sweden).
Participants
7446 Caucasian men, genotyped for 97 BMI-associated SNPs and three testosterone-associated SNPs.
Main outcome measures
BMI and serum testosterone adjusted for age, smoking, time of blood sampling and site.
Results
1 SD genetically instrumented increase in BMI was associated with a 0.25 SD decrease in serum testosterone (IV ratio: -0.25, 95% CI: -0.42–-0.09, p = 2.8*10−3). For a body weight reduction altering the BMI from 30 to 25 kg/m2, the effect would equal a 13% increase in serum testosterone. No association was seen for genetically instrumented testosterone with BMI, a finding that was confirmed using large-scale data from the GIANT consortium (n = 104349).
Conclusions
Our results suggest that there is a causal effect of BMI on serum testosterone in men. Population level interventions to reduce BMI are expected to increase serum testosterone in men.
Introduction
Observational studies demonstrate that obesity is associated with low serum testosterone (T) [1], but the direction and causality of this relationship is unclear. Most randomized, placebo-controlled trials have indicated that T treatment increases lean mass and reduces fat mass in men with low serum T [2–7], but the overall effect on body weight and BMI in men with different T-status is inconsistent. One possible explanation for the conflicting results regarding the effects of T treatment on body weight and BMI might be that the observational association between low T and high BMI is subject to reverse causation [8–10]. Based on the inverse association between T and obesity-related diseases [11–13], it has been hypothesized that T supplementation could be used as a means to reduce the risk of developing obesity-associated cardio-metabolic diseases in men with low serum T. However, safety concerns have been raised, since some studies have reported an increase in cardiovascular events after T supplementation [14, 15] and randomized controlled trials are still needed [16].
A Mendelian randomization (MR) approach uses genetic variants that index the exposure of interest to test for a causal relationship between exposure and outcome. Since genes can be thought of as randomized and fixed at conception, confounding factors will be equally distributed among different genotypes. As a consequence, MR analyses will be less prone to confounding than the directly observed association. Furthermore, it will be free of reverse causation since a phenotypic trait cannot cause genetic variation.
The most recent and largest genome wide association study (GWAS) on BMI identified 97 independent genetic variants associated with BMI while the largest GWAS on serum T identified three independent genetic variants associated with serum T in men [17, 18].
As the prescription of T to men has increased substantially [19] and its impact on obesity and obesity-related diseases is unclear, we believe it is important to determine the direction and causality of the relatively strong observational relationship between BMI and serum T. The aim of the present study was to identify a possible causative relationship, and its direction of effect, between BMI and serum T using genetic variants as instruments in bi-directional MR analyses.
Methods
Participants
This study included participants from five different cohorts of Caucasian men (Inter99, SHIP, SHIP Trend, GOOD and MrOS Sweden) from Denmark, Germany and Sweden. A total of 7446 participants with available genotype and phenotype data were included (Table 1).
Table 1. Characteristics of the cohorts.
| GOOD | MrOS Sweden | SHIP | SHIP Trend | INTER99 | |
|---|---|---|---|---|---|
| Characteristics | (n = 929) | (n = 1682) | (n = 1912) | (n = 427) | (n = 2496) |
| Outcomes | |||||
| Testosterone—ng/ml | 4.7 (1.5) | 4.5 (1.7) | 4.8 (1.7) | 4.0 (1.3) | 4.4 (1.6) |
| BMI—kg/m2 | 22.4 (3.2) | 26.3 (3.6) | 27.7 (4.0) | 27.8 (3.7) | 26.8 (4.0) |
| SHBG—nmol/l | 20.4 (7.2) | 46.0 (22.9) | 51.3 (25.6) | 38.3 (14.2) | 31.8 (13.1) |
| Covariates | |||||
| Age—years | 18.9 (0.6) | 75.4 (3.2) | 50.8 (16.4) | 50.1 (14.2) | 46.7 (7.9) |
| Smoking—percent | 9% | 9% | 34% | 22% | 36% |
| Genetic Risk scores | |||||
| wGRSBMI | 88.8 (6.3) | 89.0 (6.3) | 89.1 (6.2) | 88.8 (6.2) | 87.6 (6.1)* |
| uwGRSBMI | 91.4 (6.4) | 91.7 (6.3) | 91.6 (6.1) | 91.5 (6.2) | 90.6 (6.0)* |
| wGRST | 1.4 (0.6) | 1.4 (0.6) | 1.4 (0.5) | 1.4 (0.5) | 1.3 (0.5) |
| uwGRST | 2.3 (0.7) | 2.4 (0.8) | 2.3 (0.7) | 2.3 (0.7) | 2.3 (0.8) |
Values are given as mean with standard deviation within brackets.
wGRSBMI = Weighted genetic risk score based on 97 BMI-associated SNPs.
uwGRSBMI = Un-weighted genetic risk score based on 97 BMI-associated SNPs.
wGRSTestosterone = Weighted genetic risk score based on 3 SNPs associated with serum testosterone.
uwGRST = Un-weighted genetic risk score based on 3 SNPs associated with serum testosterone.
*) Based on 96 instead of 97 SNPs.
Subjects known to use medications affecting sex hormones (testosterone, 5-alpha reductase inhibitors and antiandrogens) and/or who were surgically or chemically castrated, were excluded when this information was available. A more detailed description of the cohorts is available in the supplemental methods. All participants provided written, informed consent, and ethical permission was granted by the local research ethics committees for all participating studies (GOOD: local ethics committee at University of Gothenburg; MrOS Sweden: local ethics committees at Gothenburg University and Lund University; SHIP and SHIP Trend: local ethics committee of the University of Greifswald; Inter99: local ethics committee of Copenhagen County).
Serum testosterone
GOOD and MrOS Sweden used a validated gas chromatography/mass spectroscopy (intra-assay CV, 2.9%; inter-assay CV, 3.4%) to measure serum T [20]. SHIP and Inter99 used immunoassays (intra-assay CV 8.9–13.3%, inter-assay CV 2.3%) [21] to measure serum T. A liquid chromatography-tandem mass spectrometry was used to measure serum T (intra-assay and inter-assay CVs<10%) in SHIP Trend [22].
Serum SHBG
GOOD and MrOS Sweden used an immunoradiometric assay to measure serum SHBG (sex hormone-binding globuline; GOOD: intra-assay CV 3%, inter-assay CV 7%; MrOS Sweden: intra-assay CV <5.5%, inter-assay CV < 6.9%) [23]. SHIP used a competitive chemiluminescent enzyme immunoassays (inter-assay CV 6.6–7.7%) to measure serum SHBG [24]. Inter99 used a time-resolved immunofluorometric assay to measure serum SHBG (inter- and intra-assay CVs < 8%)[25].
Genotyping and genetic risk scores
All cohorts except Inter99 used imputed genotype dosage SNP data (HapMap CEU r22) for the analyses. Inter99 had directly genotyped data (BeadChip) available for the BMI-associated SNPs and used KASPar from KBioscience for the three testosterone-associated SNPs. For details, please see supplemental methods.
The 97 BMI-associated SNPs identified in a recent large-scale GWAS on BMI were used to construct a weighted genetic risk score, wGRSBMI, where weights were based on each SNP´s effect size with BMI in the meta-analysis by Locke et al [17]. For the primary analyses, the wGRSBMI was used.
For T, a weighted T-decreasing genetic risk score (wGRST) was developed based on three SNPs (rs6258, rs12150660, rs5934505) with weights identified in a recent large-scale GWAS on T [18].
Due to a partial overlap between the cohorts used by the original GWA studies identifying the SNPs and the present study an unweighted BMI-increasing genetic risk score (uwGRSBMI) and an unweighted T-decreasing genetic risk score (uwGRST) were also developed. Please see supplemental methods for further details.
Statistical analysis
The BMI data distribution was positively skewed and was therefore natural log transformed (Shapiro-Wilk test, p-value < 2.2e-16). Standardized residuals of ln BMI, serum SHBG and serum T (Z-scores) were calculated. An additive genetic model was used. Furthermore, although covariates are expected to be randomly distributed with respect to genotype, the associations between genotype and known confounders (age and smoking) were examined as this is a key assumption in MR analyses. In addition, due to the close connection between T and SHBG, the association between genotypes and SHBG were analyzed. Models with BMI as an outcome were adjusted for age, smoking and site, whereas models with serum T as an outcome were additionally adjusted for time of sampling. When evaluating a possible interaction effect between covariates and the genetic risk scores, an interaction term was added to the regression models.
The strength of the genetic risk scores as instruments was determined using the F statistic which was calculated as [F-stat = (n-2)*R2/(1-R2)], where R2 refers to the proportion of variance explained [26]. Two independent instrumental variables were used for each phenotype to assess pleiotropy. Linearity was assessed by adding a quadratic term to the regression analyses. The IV ratio method, using a two-stage least squares regression, was used to estimate the unconfounded causal effect of BMI on serum T and vice versa [27]. In addition, we also determined the causal effect of BMI on serum T after adjustment for serum SHBG as well as the causal effect of BMI on serum SHBG after adjustment for serum T.
In order to confirm the validity of our data, we also performed the combined analyses by pooling the samples. The effect on T as a result of a decline in BMI from 30 kg/m2 to 25 kg/m2 was estimated using pooled data and the obtained causal effect (the IV ratio) adjusted for age, smoking, cohort, site and blood sampling time. Since the IV ratio was calculated as standard deviations of T (SD(T)) per standard deviation of natural log transformed BMI (SD(log BMI)), the IV ratio was multiplied with SD(T) divided by SD(log BMI) to obtain the IV ratio in terms of T units per unit of log BMI. This was then multiplied with the difference between log 25 and log 30 to arrive at the difference in T levels given the decline in BMI from 30 kg/m2 to 25 kg/m2. In order to obtain the percentage change in T levels, the difference in T levels was then divided by the predicted T levels given a BMI of 30 kg/m2. In order to confirm our lack of evidence of a causal effect of T on BMI, we used summary statistics from the GIANT consortium (please see supplemental methods for details) [17, 28].
Power calculations for IV regression were based on a previously published analytical approach, using sample size, the observed association between phenotypes and the association between each phenotype and their genetic proxies [29]. To evaluate the ability to detect weaker effects on BMI using the wGRST and on serum T using wGRSBMI, power was also calculated based on half the observed association effect between BMI and serum T (1/2β).
Please see supplemental methods for further details on the statistical analysis.
Results
Phenotypic association between BMI and serum T: Observational estimates
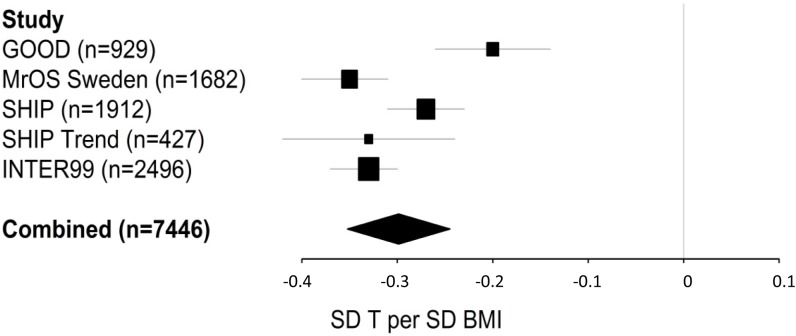
The observational association between BMI and serum T was significant in all cohorts after adjustment for age, smoking, site and blood sampling time, but slightly more pronounced in the MrOS cohort including the oldest men (mean age 75.4 years; -0.35 SD T per SD ln BMI) compared to the GOOD cohort including the youngest men (mean age 18.9 years; -0.20 SD T per SD ln BMI; Fig 1). In the meta-analysis of the five cohorts, we found evidence of heterogeneity (I-squared = 82%, p = 0.0005) among cohorts and therefore performed a random effect inverse-variance meta-analysis, demonstrating that a 1 SD increase in ln-transformed BMI was associated with a 0.30 SD decrease in serum T (95% CI -0.35–-0.24; Fig 1). A similar observational estimate was found in a pooled analysis of the five participating cohorts, revealing that 1 SD increase in ln-transformed BMI was associated with 0.30 SD decrease in serum T (95% CI: -0.33–-0.28).
Fig 1. Observational estimates.
An increased BMI is associated with a decreased serum testosterone (T). Linear regression models were used adjusting for age, smoking, site and time of day for blood sample, when applicable. The combined effect was calculated with random effect meta-analysis (I-squared = 82%, p = 0.0005) using all cohorts (n = 7446). Effect sizes are given in standard deviations (SD) of T per SD ln-transformed BMI. Horizontal bars represent 95% confidence intervals.
Validation of the instruments
Although both BMI and serum T were associated with age and smoking (p<0.05), the different GRSs evaluated in the present study (wGRSBMI, uwGRSBMI, wGRST and uwGRST) were not associated with these two potential confounders (p>0.05; S1 Fig). This illustrates that these GRSs can be used as largely un-confounded instruments to assess the causality of the inverse association between BMI and serum T.
BMI SNPs
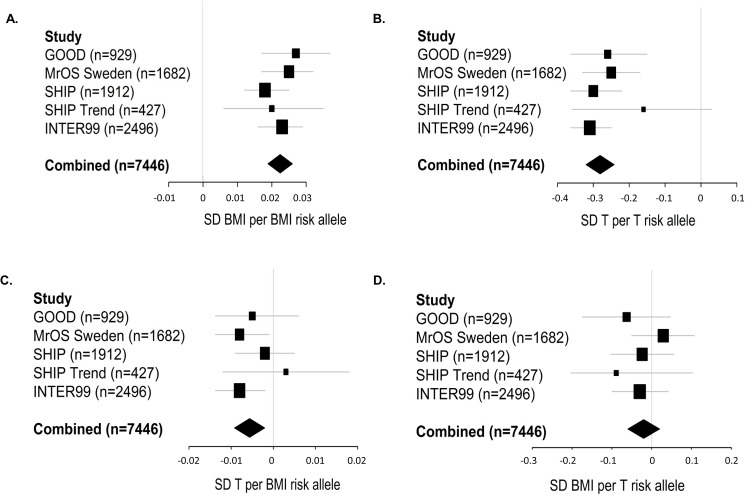
Both wGRSBMI and uwGRSBMI were highly significantly associated with ln-transformed BMI in all cohorts individually and when combined in a meta-analytic approach (wGRSBMI p = 4.2*10−35, R2 = 1.9%; uwGRSBMI p = 5.0*10−27, R2 = 1.5%; Fig 2A, S1 Table). There was no evidence of heterogeneity in these analyses. The F-statistics, reflecting the strength of the instruments, were 147 and 111 for wGRSBMI and uwGRSBMI, respectively (S1 Table). Similar significant associations were observed using pooling instead of a meta-analytic approach (S1 Table). The wGRSBMI and uwGRSBMI associations with BMI did not vary by age, smoking or serum T (p > 0.05 for all interaction terms in pooled analyses). No evidence of non-linearity was found for wGRSBMI or uwGRSBMI. When the 97 SNPs included in the wGRSBMI were evaluated separately, 16 SNPs were nominally (p<0.05) significantly associated with BMI. Three of these SNPs were still, after a conservative Bonferroni adjustment (p<0.05/97), significantly associated with BMI (S2 Table).
Fig 2. The genetic risk scores’ association with BMI and serum T.
A) High weighted genetic risk score on BMI (wGRSBMI) is associated with high BMI. B) The weighted genetic risk score on serum testosterone (T; wGRST) is inversely associated with serum T. C) The weighted genetic risk score on BMI (wGRSBMI) is inversely associated with serum testosterone (T). D) The weighted genetic risk score on serum T (wGRST) is not associated with BMI. Linear regression models were used adjusting for age, smoking, site and time of day for blood sample, when applicable. The combined effect was calculated with fixed-effect meta-analysis (A: I-squared = 0%, p = 0.63; B: I-squared = 0%, p = 0.49; C: I-squared = 0%, p = 0.51; D: I-squared = 0%, p = 0.62) using all cohorts (n = 7446). Effect sizes are given in standard deviations (SD) of ln-transformed BMI per weighted BMI risk allele in A, SD of T per weighted T risk allele in B, SD of T per weighted BMI risk allele in C and SD of ln-transformed BMI per weighted T risk allele in D. Horizontal bars represent 95% confidence intervals.
Testosterone SNPs
Both wGRST and uwGRST were highly significantly associated with serum T in the meta-analyzed combined data set (wGRST p = 4.7*10−45, R2 = 2.5%; uwGRST p = 3.9*10−38, R2 = 2.1%; Fig 2B, S3 Table). There was no evidence of heterogeneity in these analyses (Fig 2B). The F-statistics were 188 and 156 for wGRST and uwGRST, respectively (S3 Table). Similar significant associations were observed using pooling instead of a meta-analytic approach (S3 Table). The wGRST and uwGRST associations with T did not vary by age, smoking or BMI (p values > 0.05 for all interaction terms in pooled analyses). No evidence of non-linearity was found for wGRST or uwGRST. All three SNPs included in the wGRST were individually associated with serum T (p<0.05/3; S4 Table).
Power analysis
The present study was adequately powered to detect a causal association between BMI and T if the strength of this association was equal to the observed association between serum BMI and T. In theory, we had approximately similar power to detect an association between BMI and T using the wGRSBMI (95%) compared with an equal sized effect in the other direction using the wGRST (98%, n = 7446 subjects; S2 Fig).
Evaluation of causal association using MR approach
BMI has a causal effect on serum testosterone
Both wGRSBMI (p = 2.0*10−3) and uwGRSBMI (p = 1.7*10−3) were significantly and inversely associated with serum T in the meta-analyzed combined cohort (Fig 2C; S1 Table). Similar significant associations were observed using pooling instead of a meta-analytic approach (S1 Table). After adjustment for BMI, none of these associations were still significant. The wGRSBMI and uwGRSBMI associations with T did not vary by age or smoking (p > 0.05 for interaction terms in pooled analyses). Interestingly, the two BMI SNPs that were most robustly associated with BMI were also significantly associated with serum T, but in the opposite direction (rs1558902 in the FTO locus, p = 4.0*10−2 and rs6567160 in the M4CR locus, p = 3.0*10−3; S2 Table). However, none of the SNPs were still significant after adjustment for BMI. IV analyses used to establish the direction and causality of the BMI-T association, revealed that 1 SD increase in ln-transformed BMI lead to a 0.25 (using wGRSBMI, p = 2.8*10−3) to 0.29 (using uwGRSBMI, p = 2.5*10−3) SD decrease in serum T (Table 2, S1 Table). There was no significant difference between β-coefficients from observational and IV analysis (wGRSBMI: p value 0.44, uwGRSBMI: p value 0.82).
Table 2. Summary of the coefficients used for IV ratio analyses.
| IV | Risk Score with the Intermediate Trait | Risk score with the Outcome | IV Ratio | |
|---|---|---|---|---|
| Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | P value | |
| wGRSBMI | 0.022 (0.019–0.026) | -0.006 (-0.009–-0.002) | -0.25 (-0.42–-0.09) | 0.003 |
| uwGRSBMI | 0.020 (0.016–0.023) | -0.006 (-0.009–-0.002) | -0.29 (-0.48–-0.10) | 0.003 |
| wGRST | -0.281 (-0.320–-0.242) | -0.020 (-0.060–0.020) | 0.07 (-0.56–0.70) | 0.214 |
| uwGRST | -0.191 (-0.220–-0.162) | -0.004 (-0.034–0.025) | 0.02 (-0.13–0.18) | 0.777 |
IV ratio was calculated as the ratio between the genetic risk score's association with the outcome and intermediate trait (n = 7446).
Coefficients for intermediate trait and outcome are given as SD per unit in genetic risk score.
wGRSBMI = Weighted genetic risk score on BMI.
uwGRSBMI = Un-weighted genetic risk score on BMI
wGRST = Weighted genetic risk score on serum testosterone.
uwGRSTT = Un-weighted genetic risk score on serum testosterone.
IV ratio is expressed in SD testosterone per SD ln-transformed BMI for wGRSBMI and uwGRSBMI, while it is expressed in SD ln-transformed BMI per SD testosterone for wGRST and uwGRST.
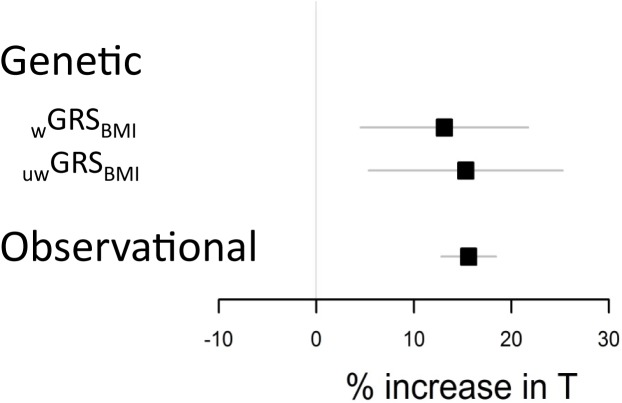
Notably, for a body weight reduction altering the BMI from 30 (cut off for obesity) to 25 (cut off for overweight) kg/m2, the effect would equal a 13% (using IV ratio from wGRSBMI) to 15% (using IV ratio from uwGRSBMI) increase in serum T while a corresponding observational effect would equal a 16% increase in serum T (Fig 3). To reduce the risk of pleiotropy, we next evaluated two separate independent genetic instruments (rs1558902 from the FTO locus and a weighted risk score based on the remaining 96 SNPs). These two independent genetic instruments had similar point estimates of the causal effect of BMI on serum T (S5 Table).
Fig 3. Genetic and observational estimates of the influence of altering BMI on serum testosterone (T).
Effect sizes are given in percent change in serum T based on a decrease in BMI from 30 (cut off for obesity) to 25 (cut off for overweight) kg/m2 (n = 7446). wGRSBMI = weighted genetic risk score on BMI. uwGRSBMI = un-weighted genetic risk score on BMI. Horizontal bars represent 95% confidence intervals.
No evidence of a causal effect of serum testosterone on BMI
Neither the wGRST nor the uwGRST was associated with BMI (Fig 2D, S3 Table). Furthermore, the IV ratio analyses provided no evidence for a causal effect of serum T on BMI (Table 2, S3 Table). For the two autosomal SNPs it was possible to use the GIANT consortium, including up to 104349 men, to evaluate the causal effect of serum T on BMI in a larger setting. However, no significant evidence was found supporting that any of these T SNPs were associated with BMI individually, or when combined as a genetic risk score (S6 Table).
Due to the complexity of the T synthesis and bio-availability we also performed sub-analyses using two separate GRSs based on SNPs located within, or outside, the SHBG locus. Although both these two separate T GRSs were robustly associated with serum T, no evidence of significant associations between these two separate T GRSs and BMI was observed (S7 Table).
Genetic risk scores for BMI and serum T in relation to serum SHBG
Since serum SHBG is a known major determinant of serum total T, we also tested the association between serum SHBG and the weighted genetic risk scores for BMI (wGRSBMI) and serum T (wGRST). wGRSBMI was inversely associated with serum SHBG in the pooled combined cohort (S3 Fig). However, after adjustment for serum T wGRSBMI was not significantly associated with SHBG (combined cohort: p = 0.59). wGRST was robustly associated with serum SHBG (combined cohort: p = 2.7*10−49, S3 Fig). Interestingly, the association between wGRSBMI and serum T remained significant (p = 0.02) after adjustment for serum SHBG in the pooled combined cohort.
Discussion
Obesity is associated with low serum T in men, but the direction of the association and the potentially causal effect is still debated. Herein, we presented evidence that higher BMI leads to lower serum T. Conversely, our analyses provided no evidence for a causal role of serum T on BMI. These results suggest that although increases in T status are not likely to help with weight regulation in the general male population, low serum T could contribute to the adverse health effects associated with obesity in men. Our study highlights the importance of considering obesity as a risk factor for low serum T in men with implications on the possible targeting of relevant health promotion strategies.
We evaluated the relationship between BMI and serum T using a bi-directional MR analysis which is free of reverse causation. Our genetic instruments in these analyses were derived from the most recent large-scale GWAS-meta-analyses on serum T and BMI [17, 18]. Three key assumptions underlie the MR randomization approach: the genotypes are randomized; the genetic variants considered as instruments affect the outcome only by modifying the biomarker—that is, these variants have no pleiotropic effects on the outcome; and the genotype is independent of confounders [27, 30, 31]. We did not detect any violations of the assumptions underlying MR as far as they could be tested. For instance, although both BMI and T were associated with age and smoking, the different GRSs used in the present study were not associated with these two potential confounders. It could be argued that as the biological functions for some of the used BMI-associated SNPs are yet to be established [17, 28], there could be alternative biological pathways explaining their association with BMI. However, using as many as 97 recently reported independent SNPs to index BMI, we were able to minimize the risk of shared pleiotropy and linkage-disequilibrium-induced confounding pleiotropic effects [32, 33]. Moreover, the use of two separate independent genetic instruments with similar point estimates of the causal effect of BMI on serum T further reduced the risk of pleiotropy [32, 33].
In the present study, there was a small overlap (less than 2%), between the cohorts used in the present study and the study by Locke et al that identified the BMI-associated SNPs[17]. As a consequence, there is a chance that the causal estimate calculated using the wGRSBMI could be biased. It is, however, highly unlikely that this has had a major impact on the results for two reasons. Firstly, very similar results were obtained using an unweighted genetic risk score that avoids the potential bias from the use of internal weights. Secondly, similar results were also obtained using a genetic risk score based solely on the SNP in the FTO gene, which is a gene that has been found to be associated with BMI in numerous studies, where none of the cohorts used in the present study were included [34–36]. The validity of our findings was strengthened by the fact that very similar results were obtained for both weighted and un-weighted genetic risk scores and when combined estimates were calculated using pooling and a meta-analytic approach. Also, as we included participants at random and consecutively from the general population, the potential for selection bias is minimal.
Cross-sectional data from the large European Male Aging Study (EMAS) revealed that BMI was the strongest determinant of serum T and obese men (BMI > 30 kg/m2) had as much as 1.47 ng/ml lower serum T compared with normal weight subjects (BMI < 25 kg/m2; [1]). The main finding in the present study is our results supporting a causal effect of BMI on serum T. The magnitude of this effect is similar to the observational association. Each SD genetically instrumented increase in BMI was associated with a 0.25 SD decrease in serum T. For a body weight reduction altering the BMI from 30 to 25 kg/m2, the effect would equal a 13–15% increase in serum T. This evidence of a causative effect of BMI on serum T is supported by a recent meta-analysis of the impact of body weight reduction on serum T, revealing that body weight reductions as a result of both low-calorie diet and bariatric surgery are associated with significantly increased serum T [37]. Notably, this meta-analysis demonstrated that the degree of body weight loss is a robust determinant of the increase in serum T. The mean percent body weight loss at endpoint was 10% in low-calorie diet studies and 32% in bariatric surgery studies and the corresponding increases in serum T levels were 0.83 ng/ml and 2.54 ng/ml, respectively. It was even proposed that normalization of T levels is a possible mechanism contributing to the beneficial health effect of bariatric surgery in morbid obesity [37].
Although the present study provides compelling evidence that obesity reduces serum T levels, it cannot determine the mechanism for this causal effect which may occur at several levels of the hypothalamus-pituitary-gonadal axis. Obese subjects often have reduced gonadotropin concentrations indicating that the primary effect is mediated at the hypothalamus-pituitary level rather than at the testicular level [38]. Not only serum T but also the gonadotropins FSH and LH were increased by body weight reduction, suggesting that body weight loss reverses obesity-associated hypogonadotropic hypogonadism [37]. It is well known that in morbidly obese men, LH levels and pulse amplitude are attenuated when compared with normal-weight controls [39, 40]. Thus high BMI seems to repress serum T mainly via central inhibitory effects on gonadotropin secretion [38, 41]. The exact mechanism for this inhibitory effect of high BMI/obesity on gonadotropin secretion is unclear but might include insulin resistance, inflammatory mediators, leptin, hypothalamic kisspeptin affecting gonadotropin -releasing hormone (GnRH) secretion and/or increased aromatase activity resulting in elevated estradiol levels which in turn augment negative feed-back regulation [7, 37, 38, 42–44].
Notably, the two SNPs most robustly associated with BMI in the present study are also significantly associated with serum T but in the opposite direction. The underlying loci of these two SNPs, FTO and MC4R, are well established obesity-related loci [35, 36, 45]. The FTO locus has previously been reported to be associated with affected androgen levels, polycystic ovary syndrome susceptibility and age at menarche in females while its impact on serum T and T-related diseases in men is unknown and warrants further investigations [46, 47].
Our study highlights the importance of considering obesity as a risk factor for low testosterone concentrations in men with implications for its possible targeting in relevant health promotion strategies. Our finding supports the notions that male hypogonadism can be considered as one of the many adverse consequences of overweight and obesity and that body weight loss and lifestyle interventions should be the first approach offered to obese men with low serum T [48]. Based on the described significant secular trends of reduced serum T and increased BMI in men [25, 49] and the present evidence of a causative effect of BMI on T, we propose that successful population level interventions reverting the obesity epidemic might also lead to a reversal of the secular trend of reduction in serum T.
Our analyses provided no evidence for a causal role of serum T on BMI. It could be argued that if a possible effect of serum T on BMI would be substantially less pronounced than the observational association between T and BMI, then our study would not be adequately powered. However, the use of the GIANT consortium to test the association between T-related autosomal SNPs and BMI in a much larger sample including 104349 men also failed to identify a causal role of T on BMI. While the MR approach enables the approximation of life-long differences in average concentrations, genetic markers do not examine the influences arising from the extremes of non-linear distributions [28, 50]. Consequently, we cannot discount a possible causative effect of severe T-deficiency on BMI. Due to the complexity of the T synthesis and bio-availability we performed sub-analyses using two separate GRSs based on SNPs located within, or outside, the SHBG locus. SHBG is the dominant high-affinity binding protein for serum T and its primary function is to bind and transport steroids in the blood to access target tissues and to determine the bioavailable fraction. Although both these two separate T GRSs were robustly associated with serum T, no evidence of significant associations between these two separate T GRSs and BMI was observed.
Serum SHBG is a major well-known determinant of total serum T. In fact, in the cohorts included in this study SHBG explained about 26% of the total variance in serum T. This close connection between serum T and SHBG makes it difficult to discriminate between an effect directly on serum T and an effect mediated via SHBG. In the present study, we found evidence of a causal effect of BMI on serum T, but the BMI-based genetic risk score was also associated with serum SHBG. When serum T was added as a covariate to the analysis, the association between the BMI-based genetic risk scores and SHBG was no longer significant. However, in the opposite analysis where serum T was the outcome and SHBG the covariate, wGRSBMI was significantly associated with serum T, supporting a SHBG-independent effect of BMI on serum T. Two of the three SNPs constituting the genetic risk score for BMI reside in the SHBG locus and have previously been reported to associate with SHBG (18). In line with this, both wGRST and uwGRST were significantly associated with SHBG in the present study.
The participant data used in the present study were unrelated men with European ancestry, limiting the generalizability of the observed findings to other ethnic groups. However, this also means that a major influence from population stratification is unlikely.
In conclusion, our results suggest that there is a causal effect of BMI on serum T in men. Population level interventions to reduce BMI are expected to increase serum T in men.
Supporting information
(TIF)
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
The raw data underlying this study are restricted to protect participant privacy, as required by data protection acts in Denmark, Germany and Sweden. Data will be made available upon request to researchers who qualify for access to confidential data by contacting the following (Inter99: The Research Centre for Prevention and Health, the Capital Region of Denmark, E-mail: fcfs@regionh.dk; GOOD: Regionala Etikprövningsnämnden i Göteborg, Box 401, 405 30 Göteborg, Sweden; MrOS Sweden: Regionala Etikprövningsnämnden i Göteborg, Box 401, 405 30 Göteborg, Sweden and Regionala etikprövningsnämnden i Lund, Box 133, 221 00 Lund, Sweden; SHIP and SHIP Trend: Ethikkommission an der Medizinischen Fakultät, Ernst-Moritz-Arndt-Universität Greifswald, Institut für Pharmakologie, Felix-Hausdorff-Str. 3, 17487 Greifswald, Germany).
Funding Statement
This study was supported by the Swedish Research Council and by grants from the Swedish government (under the Avtal om Läkarutbildning och Medicinsk Forskning [Agreement for Medical Education and Research]), the Lundberg Foundation, the Torsten Söderberg Foundation, the Novo Nordisk Foundation and the Knut and Alice Wallenberg Foundation. Data collection in the Inter99 Study was supported economically by The Danish Medical Research Council, The Danish Centre for Evaluation and Health Technology Assessment, Novo Nordisk, Copenhagen County, The Danish Heart Foundation, The Danish Pharmaceutical Association, Augustinus foundation, Ib Henriksen foundation and Becket foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. The Journal of clinical endocrinology and metabolism. 2008;93(7):2737–45. doi: 10.1210/jc.2007-1972 [DOI] [PubMed] [Google Scholar]
- 2.Blackman MR, Sorkin JD, Munzer T, Bellantoni MF, Busby-Whitehead J, Stevens TE, et al. Growth hormone and sex steroid administration in healthy aged women and men: a randomized controlled trial. Jama. 2002;288(18):2282–92. [DOI] [PubMed] [Google Scholar]
- 3.Kenny AM, Prestwood KM, Gruman CA, Marcello KM, Raisz LG. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels. J Gerontol A Biol Sci Med Sci. 2001;56(5):M266–72. [DOI] [PubMed] [Google Scholar]
- 4.Page ST, Amory JK, Bowman FD, Anawalt BD, Matsumoto AM, Bremner WJ, et al. Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. The Journal of clinical endocrinology and metabolism. 2005;90(3):1502–10. doi: 10.1210/jc.2004-1933 [DOI] [PubMed] [Google Scholar]
- 5.Snyder PJ, Peachey H, Hannoush P, Berlin JA, Loh L, Lenrow DA, et al. Effect of testosterone treatment on body composition and muscle strength in men over 65 years of age. The Journal of clinical endocrinology and metabolism. 1999;84(8):2647–53. doi: 10.1210/jcem.84.8.5885 [DOI] [PubMed] [Google Scholar]
- 6.Srinivas-Shankar U, Roberts SA, Connolly MJ, O'Connell MD, Adams JE, Oldham JA, et al. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. The Journal of clinical endocrinology and metabolism. 2010;95(2):639–50. doi: 10.1210/jc.2009-1251 [DOI] [PubMed] [Google Scholar]
- 7.Saad F, Aversa A, Isidori AM, Gooren LJ. Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: a review. Curr Diabetes Rev. 2012;8(2):131–43. PubMed Central PMCID: PMCPMC3296126. doi: 10.2174/157339912799424573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haring R, Ittermann T, Volzke H, Krebs A, Zygmunt M, Felix SB, et al. Prevalence, incidence and risk factors of testosterone deficiency in a population-based cohort of men: results from the study of health in Pomerania. The aging male: the official journal of the International Society for the Study of the Aging Male. 2010;13(4):247–57. [DOI] [PubMed] [Google Scholar]
- 9.Laaksonen DE, Niskanen L, Punnonen K, Nyyssonen K, Tuomainen TP, Valkonen VP, et al. The metabolic syndrome and smoking in relation to hypogonadism in middle-aged men: a prospective cohort study. The Journal of clinical endocrinology and metabolism. 2005;90(2):712–9. doi: 10.1210/jc.2004-0970 [DOI] [PubMed] [Google Scholar]
- 10.Travison TG, Araujo AB, Kupelian V, O'Donnell AB, McKinlay JB. The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. The Journal of clinical endocrinology and metabolism. 2007;92(2):549–55. doi: 10.1210/jc.2006-1859 [DOI] [PubMed] [Google Scholar]
- 11.Haffner SM, Shaten J, Stern MP, Smith GD, Kuller L. Low levels of sex hormone-binding globulin and testosterone predict the development of non-insulin-dependent diabetes mellitus in men. MRFIT Research Group. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996;143(9):889–97. [DOI] [PubMed] [Google Scholar]
- 12.English KM, Mandour O, Steeds RP, Diver MJ, Jones TH, Channer KS. Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J. 2000;21(11):890–4. doi: 10.1053/euhj.1999.1873 [DOI] [PubMed] [Google Scholar]
- 13.Ohlsson C, Barrett-Connor E, Bhasin S, Orwoll E, Labrie F, Karlsson MK, et al. High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol. 2011;58(16):1674–81. doi: 10.1016/j.jacc.2011.07.019 [DOI] [PubMed] [Google Scholar]
- 14.Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, et al. Adverse events associated with testosterone administration. The New England journal of medicine. 2010;363(2):109–22. PubMed Central PMCID: PMC3440621. doi: 10.1056/NEJMoa1000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vigen R, O'Donnell CI, Baron AE, Grunwald GK, Maddox TM, Bradley SM, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. Jama. 2013;310(17):1829–36. doi: 10.1001/jama.2013.280386 [DOI] [PubMed] [Google Scholar]
- 16.Nguyen CP, Hirsch MS, Moeny D, Kaul S, Mohamoud M, Joffe HV. Testosterone and "Age-Related Hypogonadism"—FDA Concerns. The New England journal of medicine. 2015;373(8):689–91. doi: 10.1056/NEJMp1506632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206. PubMed Central PMCID: PMCPMC4382211. doi: 10.1038/nature14177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohlsson C, Wallaschofski H, Lunetta KL, Stolk L, Perry JR, Koster A, et al. Genetic determinants of serum testosterone concentrations in men. PLoS genetics. 2011;7(10):e1002313 PubMed Central PMCID: PMC3188559. doi: 10.1371/journal.pgen.1002313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Handelsman DJ. Global trends in testosterone prescribing, 2000–2011: expanding the spectrum of prescription drug misuse. Med J Aust. 2013;199(8):548–51. [DOI] [PubMed] [Google Scholar]
- 20.Vandenput L, Labrie F, Mellstrom D, Swanson C, Knutsson T, Peeker R, et al. Serum levels of specific glucuronidated androgen metabolites predict BMD and prostate volume in elderly men. J Bone Miner Res. 2007;22(2):220–7. doi: 10.1359/jbmr.061018 [DOI] [PubMed] [Google Scholar]
- 21.Friedrich N, Volzke H, Rosskopf D, Steveling A, Krebs A, Nauck M, et al. Reference ranges for serum dehydroepiandrosterone sulfate and testosterone in adult men. J Androl. 2008;29(6):610–7. doi: 10.2164/jandrol.108.005561 [DOI] [PubMed] [Google Scholar]
- 22.Thienpont LM, Van Uytfanghe K, Blincko S, Ramsay CS, Xie H, Doss RC, et al. State-of-the-art of serum testosterone measurement by isotope dilution-liquid chromatography-tandem mass spectrometry. Clin Chem. 2008;54(8):1290–7. doi: 10.1373/clinchem.2008.105841 [DOI] [PubMed] [Google Scholar]
- 23.Lorentzon M, Swanson C, Andersson N, Mellstrom D, Ohlsson C. Free testosterone is a positive, whereas free estradiol is a negative, predictor of cortical bone size in young Swedish men: the GOOD study. J Bone Miner Res. 2005;20(8):1334–41. doi: 10.1359/JBMR.050404 [DOI] [PubMed] [Google Scholar]
- 24.Haring R, Volzke H, Spielhagen C, Nauck M, Wallaschofski H. The role of sex hormone-binding globulin and testosterone in the risk of incident metabolic syndrome. Eur J Prev Cardiol. 2013;20(6):1061–8. doi: 10.1177/2047487312452965 [DOI] [PubMed] [Google Scholar]
- 25.Andersson AM, Jensen TK, Juul A, Petersen JH, Jorgensen T, Skakkebaek NE. Secular decline in male testosterone and sex hormone binding globulin serum levels in Danish population surveys. The Journal of clinical endocrinology and metabolism. 2007;92(12):4696–705. doi: 10.1210/jc.2006-2633 [DOI] [PubMed] [Google Scholar]
- 26.Rice J. Expected Values In: Mathematical Statistics and Data Analysis. 2nd edition ed: Duxbury Press; 1995. [Google Scholar]
- 27.Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Statistics in medicine. 2008;27(8):1133–63. doi: 10.1002/sim.3034 [DOI] [PubMed] [Google Scholar]
- 28.Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, et al. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS medicine. 2013;10(2):e1001383 PubMed Central PMCID: PMC3564800. doi: 10.1371/journal.pmed.1001383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freeman G, Cowling BJ, Schooling CM. Power and sample size calculations for Mendelian randomization studies using one genetic instrument. International journal of epidemiology. 2013;42(4):1157–63. doi: 10.1093/ije/dyt110 [DOI] [PubMed] [Google Scholar]
- 30.Afzal S, Brondum-Jacobsen P, Bojesen SE, Nordestgaard BG. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. BMJ. 2014;349:g6330 PubMed Central PMCID: PMCPMC4238742. doi: 10.1136/bmj.g6330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith GD, Ebrahim S. Mendelian randomization: prospects, potentials, and limitations. International journal of epidemiology. 2004;33(1):30–42. doi: 10.1093/ije/dyh132 [DOI] [PubMed] [Google Scholar]
- 32.Davey Smith G. Use of genetic markers and gene-diet interactions for interrogating population-level causal influences of diet on health. Genes Nutr. 2011;6(1):27–43. PubMed Central PMCID: PMCPMC3040803. doi: 10.1007/s12263-010-0181-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor PN, Richmond R, Davies N, Sayers A, Stevenson K, Woltersdorf W, et al. Paradoxical Relationship Between Body Mass Index and Thyroid Hormone Levels: A Study Using Mendelian Randomization. The Journal of clinical endocrinology and metabolism. 2016;101(2):730–8. doi: 10.1210/jc.2015-3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889–94. PubMed Central PMCID: PMCPMC2646098. doi: 10.1126/science.1141634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS genetics. 2007;3(7):e115 PubMed Central PMCID: PMCPMC1934391. doi: 10.1371/journal.pgen.0030115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loos RJ, Lindgren CM, Li S, Wheeler E, Zhao JH, Prokopenko I, et al. Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat Genet. 2008;40(6):768–75. PubMed Central PMCID: PMCPMC2669167. doi: 10.1038/ng.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corona G, Rastrelli G, Monami M, Saad F, Luconi M, Lucchese M, et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. European journal of endocrinology / European Federation of Endocrine Societies. 2013;168(6):829–43. [DOI] [PubMed] [Google Scholar]
- 38.Dandona P, Dhindsa S. Update: Hypogonadotropic hypogonadism in type 2 diabetes and obesity. The Journal of clinical endocrinology and metabolism. 2011;96(9):2643–51. PubMed Central PMCID: PMCPMC3167667. doi: 10.1210/jc.2010-2724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giagulli VA, Kaufman JM, Vermeulen A. Pathogenesis of the decreased androgen levels in obese men. The Journal of clinical endocrinology and metabolism. 1994;79(4):997–1000. doi: 10.1210/jcem.79.4.7962311 [DOI] [PubMed] [Google Scholar]
- 40.Vermeulen A, Kaufman JM, Deslypere JP, Thomas G. Attenuated luteinizing hormone (LH) pulse amplitude but normal LH pulse frequency, and its relation to plasma androgens in hypogonadism of obese men. The Journal of clinical endocrinology and metabolism. 1993;76(5):1140–6. doi: 10.1210/jcem.76.5.8496304 [DOI] [PubMed] [Google Scholar]
- 41.Saad F, Aversa A, Isidori AM, Zafalon L, Zitzmann M, Gooren L. Onset of effects of testosterone treatment and time span until maximum effects are achieved. European journal of endocrinology / European Federation of Endocrine Societies. 2011;165(5):675–85. PubMed Central PMCID: PMCPMC3188848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mah PM, Wittert GA. Obesity and testicular function. Molecular and cellular endocrinology. 2010;316(2):180–6. doi: 10.1016/j.mce.2009.06.007 [DOI] [PubMed] [Google Scholar]
- 43.George JT, Millar RP, Anderson RA. Hypothesis: kisspeptin mediates male hypogonadism in obesity and type 2 diabetes. Neuroendocrinology. 2010;91(4):302–7. doi: 10.1159/000299767 [DOI] [PubMed] [Google Scholar]
- 44.George JT, Veldhuis JD, Tena-Sempere M, Millar RP, Anderson RA. Exploring the pathophysiology of hypogonadism in men with type 2 diabetes: kisspeptin-10 stimulates serum testosterone and LH secretion in men with type 2 diabetes and mild biochemical hypogonadism. Clinical endocrinology. 2013;79(1):100–4. doi: 10.1111/cen.12103 [DOI] [PubMed] [Google Scholar]
- 45.Peng S, Zhu Y, Xu F, Ren X, Li X, Lai M. FTO gene polymorphisms and obesity risk: a meta-analysis. BMC Med. 2011;9:71 PubMed Central PMCID: PMCPMC3118373. doi: 10.1186/1741-7015-9-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elks CE, Perry JR, Sulem P, Chasman DI, Franceschini N, He C, et al. Thirty new loci for age at menarche identified by a meta-analysis of genome-wide association studies. Nat Genet. 2010;42(12):1077–85. PubMed Central PMCID: PMCPMC3140055. doi: 10.1038/ng.714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Song do K, Lee H, Oh JY, Hong YS, Sung YA. FTO Gene Variants Are Associated with PCOS Susceptibility and Hyperandrogenemia in Young Korean Women. Diabetes Metab J. 2014;38(4):302–10. PubMed Central PMCID: PMCPMC4160584. doi: 10.4093/dmj.2014.38.4.302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism. 2010;95(6):2536–59. doi: 10.1210/jc.2009-2354 [DOI] [PubMed] [Google Scholar]
- 49.Berg C, Rosengren A, Aires N, Lappas G, Toren K, Thelle D, et al. Trends in overweight and obesity from 1985 to 2002 in Goteborg, West Sweden. Int J Obes (Lond). 2005;29(8):916–24. [DOI] [PubMed] [Google Scholar]
- 50.Zheng J, Li Y, Abecasis GR, Scheet P. A comparison of approaches to account for uncertainty in analysis of imputed genotypes. Genet Epidemiol. 2011;35(2):102–10. PubMed Central PMCID: PMCPMC3143715. doi: 10.1002/gepi.20552 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
The raw data underlying this study are restricted to protect participant privacy, as required by data protection acts in Denmark, Germany and Sweden. Data will be made available upon request to researchers who qualify for access to confidential data by contacting the following (Inter99: The Research Centre for Prevention and Health, the Capital Region of Denmark, E-mail: fcfs@regionh.dk; GOOD: Regionala Etikprövningsnämnden i Göteborg, Box 401, 405 30 Göteborg, Sweden; MrOS Sweden: Regionala Etikprövningsnämnden i Göteborg, Box 401, 405 30 Göteborg, Sweden and Regionala etikprövningsnämnden i Lund, Box 133, 221 00 Lund, Sweden; SHIP and SHIP Trend: Ethikkommission an der Medizinischen Fakultät, Ernst-Moritz-Arndt-Universität Greifswald, Institut für Pharmakologie, Felix-Hausdorff-Str. 3, 17487 Greifswald, Germany).