Abstract
Infectious diseases are a major threat to humanity, and it is imperative that we develop imaging tools that aid in their study, facilitate diagnosis, and guide treatment. The alarming rise of highly virulent and multi-drug-resistant pathogens, their rapid spread leading to frequent global pandemics, fears of bioterrorism, and continued life-threatening nosocomial infections in hospitals remain as major challenges to health care in the USA and worldwide. Early diagnosis and rapid monitoring are essential for appropriate management and control of infections. Tomographic molecular imaging enables rapid, noninvasive visualization, localization, and monitoring of molecular processes deep within the body and offers several advantages over traditional tools used for the study of infectious diseases. Noninvasive, longitudinal assessments could streamline animal studies, allow unique insights into disease pathogenesis, and expedite clinical translation of new therapeutics. Since molecular imaging is already in common use in the clinic, it could also become a valuable tool for clinical studies, for patient care, for public health, and for enabling precision medicine for infectious diseases.
Key words: Bacteria, PET, Influenza, TB, Optical imaging, Microbiome
Introduction
Humans in the modern era are increasingly prone to virulent infections. Selection and dissemination of “super bugs” by overuse (misuse) of antimicrobials, global travel and the rapid spread of infections, and the increasing use of medical procedures—implants, catheters, immunosuppressive/cancer therapies—are leading to life-threatening infections that are a growing threat to humanity [1–4]. In 2011, about 722,000 Americans developed hospital-acquired infections, resulting in 75,000 deaths in the USA. Bacteria, notably from the Enterobacteriaceae family (26.8 %), Clostridium difficile (12.1 %), Staphylococcus aureus (10.7 %), and Pseudomonas aeruginosa (7.1 %), accounted for the majority of these infections [5, 6]. Similarly, viral infections such as influenza cause millions of new cases and several thousand deaths annually in the USA [7]. The burden of hospital-acquired and other infections is substantially higher globally. For example, Mycobacterium tuberculosis, the causative agent for tuberculosis (TB), was responsible for 10.4 and 1.8 million new cases and deaths in 2015 alone [8]. The alarming rise of multi-drug-resistant (MDR) and extensively drug-resistant (XDR) strains, as well as HIV co-infection, continues to fuel this epidemic [8–10]. Global travel and rapid spread of infections—swine flu, SARS-CoV, Ebola, and Zika virus—have led to several recent global pandemics [11, 12]. Finally, several infectious pathogens, e.g., Yersinia pestis (causes plague) from the Enterobacteriaceae family, are also recognized as biothreat agents [13].
Imaging of Infection Interest Group
Developing a better understanding of the pathogenic mechanism(s) of disease and new tools that could visualize these processes in vivo is a key to controlling infections. Therefore, the World Molecular Imaging Society has made a commitment for advancing imaging tools for infectious diseases and inflammation by creating the Imaging of Infection Interest Group (IOI-IG). This interest group is tasked with the mission to globally advance the development of new imaging technologies for infectious diseases and the translation of effective imaging tools to provide unique insights into disease mechanisms, enable drug and vaccine development, guide treatments, and benefit patients (Fig. 1). As part of these efforts, the IOI-IG organized several sessions at the 2016 World Molecular Imaging Congress (WMIC). This included a 1-day workshop focused on imaging of infection and inflammation, which brought together individuals from multiple scientific disciplines and highlighted the latest developments in the field. In addition, the workshop also had a panel discussion on the challenges in funding research, with panelists from the US National Institutes of Health. A similar workshop is planned at the 2017 WMIC (Philadelphia, PA) and will focus on leveraging current resources, promoting collaborations, clinical translation, and finding strategies to overcome the challenges in funding research in this emerging field.
Fig. 1.
Imaging of Infection Interest Group. The Imaging of Infection (IOI) Interest Group was formed as part of the World Molecular Imaging Society to advance the field of infectious disease imaging.
The Clinical Problem
Rapid and accurate diagnosis and localization of infections are essential for effective early interventions and appropriate management. However, traditional diagnostic tools, namely microscopy, microbiology, and molecular techniques, are dependent upon sampling suspected sites of infection, often blindly, and then performing assays that can be time consuming. While major advances are being made in the application of molecular techniques such as nucleic acid amplification (NAA), deep sequencing, and matrix-assisted laser desorption/ionization, they are all dependent on the availability of a relevant clinical sample. Easily obtained clinical samples such as blood or urine may lack relevance and not contribute to a specific diagnosis, especially with deep-seated infections, and invasive biopsies are often required. Biopsies can be costly, risky (anesthesia, dangers of surgery), and prone to incorrect sampling (limited to the tip of the biopsy needle) as well as lead to the introduction of artifacts or contamination. Molecular imaging techniques detect crucial biological and biochemical changes at the sites of infection, often at the earliest phase of the disease, thereby allowing the clinician to promptly identify not only the infective or inflammatory focus but also the class of the causative pathogen and establish the best therapeutic approach for patients.
The Solution
Tomographic imaging can evaluate disease processes deep within the body, noninvasively and rapidly. Moreover, the ability of imaging to conduct noninvasive, longitudinal assessments in the same individual is a fundamental advantage over current traditional tools. Other major advantages of imaging are its ability to provide a holistic, three-dimensional assessment of the whole organ or body, less likely to be limited by sampling errors and co-relating well with the overall disease process (Table 1). Selected recent examples highlighting the unique role of imaging in infectious diseases are briefly described in this overview.
Table 1.
Role of imaging in infectious diseases
| Advantages of tomographic imaging over traditional techniques used for infections | ||
| Evaluate disease processes deep within the body, noninvasively, and relatively rapidly | ||
| Longitudinal assessments in the same individual—fundamental advantage over traditional tools | ||
| Provide holistic, three-dimensional assessment of the whole organ or body representative of the overall disease (versus tip of a biopsy needle) and therefore less prone to sampling error | ||
| Imaging in infectious diseases | ||
| Role | Setting | Overall goal(s) |
| Pathogenesis | Preclinical |
Unique insights into disease pathogenesis, e.g., assessing hideouts of infections, defining the diversity of the microbial populations (microbiome) Studying multi-compartment antimicrobial pharmacokinetics Expedite bench-to-bedside translation of new therapeutics, e.g., surrogate end points to assess antimicrobial or vaccine efficacy or predict stable cure |
| Clinical trials |
Unique insights into disease pathogenesis—noninvasive visualization of processes deep inside the body Phase 0 studies to determine compartment-specific antimicrobial penetration/binding (sites of infection, necrotic/fibrotic lesions, privileged sites—CNS) to inform appropriate dosing of novel drugs; determine accumulation at non-target sites to assess potential toxicities; current US Food and Drug Administration (FDA) guidelines require tissue drug distribution studies at the infected sites |
|
| Patient settings | Enabling precision medicine by providing unique insights into disease pathogenesis, antimicrobial pharmacokinetics, etc. | |
| Diagnosis | Clinical trials and patient settings |
Rapidly and specifically distinguish an infectious process from other diseases (malignancy, sterile inflammatory processes, etc.) Determine the site (e.g., extension/metastasis to other organs or privileged sites) and extent of disease Provide information on the class of the infectious pathogen, which could help in targeted empiric antimicrobial treatments |
| Monitoring and prognostication | Preclinical | Noninvasive longitudinal assessments, especially in studies utilizing larger, more expensive animal species; serial assessments in the same animal could significantly reduce sample size, inter-animal variability (outbreed animals), and therefore cost of the studies |
| Clinical trials |
Early end points for treatment trials to assess activity of treatments and to predict stable cure Assessing host-directed treatments for infections Enable adaptive designs |
|
| Patient settings |
Rapidly detect treatment failures due to drug-resistant organisms or other reasons Rapidly monitor treatment responses in patients with drug-resistant organisms and individualize treatments Early end points for duration of treatment and predict stable cure enabling precision medicine |
|
| Public health |
Rapid determination of the infectious risk of a patient to the population based on response to treatment and extent and location of disease Rapid diagnosis and monitoring of biothreat agents |
|
Pathogenesis
Optical imaging methods have been used extensively to study disease pathogenesis, largely in small laboratory animals. For example, real-time analysis of Mycobacterium marinum infection in the transparent zebrafish has provided new insights into the temporal kinetics of host-pathogen interactions [14]. Similarly, immune responses to central nervous system (CNS) viral infections were visualized in real time using intravital two-photon laser scanning microscopy [15]. While highly sensitive, optical imaging is limited by the depth of the signal and is therefore well suited for the study of laboratory animal models but has limited clinical utility. The limited depth of penetration of signal is not a problem using nuclear medicine tools. For example, 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) positron emission tomography (PET) and computed tomography (CT) were used to monitor the spatial evolution of individual pulmonary lesions in a cohort of infected mice that develops TB lesions akin to humans [16–18] and study the temporal evolution of reactivation pulmonary TB (relapse) [19]. It was noted that the fate of individual pulmonary lesions in the same animal varied substantially. More interestingly, several lesions also arose de novo within regions with no prior lesions suggesting that dormant bacteria may also reside outside TB lesions. Similar variability of TB lesion within the same host was also reported in non-human primates [20]. Molecular imaging can therefore provide unique insights into disease pathogenesis that are not possible with traditional tools. Other applications include assessing hideouts of infections, defining the diversity of the microbial populations (microbiome), and providing end points to assess antimicrobial or vaccine efficacy or predict stable cure.
Drug Development
Current antimicrobial dosing regimens are based on achievable serum concentrations. However, a growing number of studies support the importance of monitoring drug concentration in infected tissues, rather than serum alone. Inadequate drug concentrations in target tissues can lead to treatment failure and selection of drug-resistant organisms. Additionally, altered metabolism in diseased states may lead to organ toxicities. Vancomycin, a widely used antimicrobial to treat drug-resistant, Gram-positive bacteria, highlights these limitations. Studies performed in response to treatment failures noted in patients with standard doses of vancomycin revealed that it penetrates poorly into infected tissues, with levels only one sixth of plasma [21]. Conversely, high levels of vancomycin can cause nephrotoxicity. Based on these data, new recommendations have been developed for vancomycin [22], which, unfortunately, had been inappropriately under-dosed for decades.
Noninvasive bioimaging can be used to assess the distribution of drugs into multiple compartments of interest, simultaneously. For example, given the importance of rifampin for successful cure, potential for shortening the duration of TB treatments, and the limited availability of in situ data [23], dynamic PET imaging was performed over 60 min after injection of 11C-rifampin in live, M. tuberculosis-infected mice [24]. 11C-rifampin rapidly distributed and quickly localized to the liver. Areas under the concentration-time curve for the first 60 min (AUC0–60) in infected and uninfected mice were uniformly low in the brain (10 to 20 % of blood values). However, lower concentrations were noted in necrotic lung tissues of infected mice than in healthy lungs, demonstrating the need for higher dosing than those determined by serum levels alone.
Specific Diagnosis
An ideal imaging agent for diagnosing infections needs to be both sensitive and specific. While current, noninvasive techniques, such as CT, magnetic resonance imaging (MRI), and ultrasound, can rapidly detect anatomic pathology, they are non-specific and cannot reliably differentiate infectious lesions from non-infectious processes such as cancer or autoimmune diseases. Similarly, highly sensitive, current nuclear imaging tools such as [111In]oxine-tagged white blood cell, single-photon emission computed tomography (SPECT), and [18F]FDG PET, which are increasingly being used for infections, are non-specific [25]. Finally, all these imaging tools are dependent upon host responses, which could be altered in immunosuppressed states (e.g., cancer, AIDS).
Radiolabeled antibiotics or antimicrobial peptides have been previously tested as pathogen-specific imaging tracers [26, 27]. However, radiolabeled antibiotics have demonstrated variable specificity and an inability to reliably differentiate infection from sterile inflammation [28]. Radiolabeled peptides lack mechanistic binding or uptake, but recent PET tracers may show promise [29]. Tracers targeting pathogen-specific metabolic processes have also been evaluated in preclinical studies [30, 31]. [124I]FIAU, a nucleoside analog substrate for thymidine kinase, was developed as a γ-herpesvirus and bacteria-specific tracer [32] but was later found to lack specificity, presumably due to host mitochondrial metabolism [33]. Ning et al. and Gowrishankar et al. have demonstrated the feasibility of F-18-labeled maltohexaose and [18F]fluoromaltose to specifically image bacteria in vivo [34, 35]. These tracers target the maltodextrin transporter present in a wide range of Gram-negative and Gram-positive bacteria. Enterobacteriaceae are an important class of Gram-negative bacteria that cause serious infections in humans and include Escherichia coli, Klebsiella spp., Enterobacter spp., Citrobacter spp., Serratia spp., and Yersinia spp. Weinstein and Ordonez et al. demonstrated that 2-deoxy-2-[18F]fluorosorbitol ([18F]FDS) PET could specifically detect Enterobacteriaceae in vivo in various different sites including the brain, and the PET signal was not affected by immunosuppressive cancer treatments [36]. F-18 analogs of trehalose have also been developed as potential imaging agents for mycobacteria [37], while Aspergillus fumigatus has been imaged in vivo using Ga-68-radiolabeled siderophores [38]. Investigators have also utilized radiolabeled antibodies to image A. fumigatus and Yersinia in murine models [39, 40]. Similarly, Santangelo et al. developed a technique to image simian immunodeficiency virus (SIV) replication using a Cu-64-labeled SIV Gp120-specific antibody and were able to detect virus-specific PET signals in treated and untreated monkeys [41]. Other approaches have utilized Tc-99m-labeled oligomers to specifically target the ribosomal RNA in the pathogen [42, 43]. Finally, using endogenous CEST contrast, Liu et al. were able to image bacteria-specific MRI signals from C. novyi-NT-infected tumors in mice [44].
Monitoring
Noninvasive imaging, including non-specific agents, can be used to monitor disease, and serial imaging has been used to assess antimicrobial treatments in animals and humans [9, 45–47]. For example, phase III TB trials entail treating hundreds of patients ≥6 months and monitoring for ≥1 year thereafter for relapse [48]. As M. tuberculosis can infect any part of the lung (or extra-pulmonary sites), traditional tools such as sputum culture or NAA (e.g., Xpert® MTB/RIF) do not always correlate with the overall disease burden. Recently, Chen et al. reported that [18F]FDG PET and CT imaging were superior to traditional (sputum) microbiology for monitoring response to treatments in adults with MDR-TB [49]. In this study, quantitative changes in lesion volumes on CT imaging were predictive of treatment responses. Moreover, quantitative changes in [18F]FDG PET not only correlated with treatment responses but were also predictive of long-term treatment outcomes. In another more recent study, given the absence of clinical or microbiological markers of disease, low-radiation exposure pulmonary CT imaging was successfully used to monitor treatment response in a 2-year-old child with XDR-TB and guide an individualized drug regimen [9]. Imaging agents with higher specificity for TB-associated inflammation have been shown to be promising in animal models [45]. Pathogen-specific imaging could be an even better predictor of treatment responses [36]. For example, both 18F-labeled maltohexaose and [18F]FDS PET could rapidly identify therapeutic failures associated with drug-resistant infections [34, 36].
Public Health
Given that several infectious agents are easily transmissible (e.g., via aerosol), imaging could also help with rapid determination of the infectious risk of a patient to the population. This could be especially relevant for highly drug-resistant organisms or biothreat agents, where rapid diagnosis and therapeutic monitoring would be critical to prevent spread to others in the community.
Biocontainment
A large majority of infectious pathogens can be handled using standard precautions. However, animals infected with pathogens designated as biosafety level 3/4 (BSL-3/4) require appropriate containment. In addition, work with biothreat pathogens requires regulatory approvals, as well as highly trained personnel [50]. To achieve containment, several groups have installed imaging equipment inside the BSL-3/4 barrier (e.g., NIAID, University of Pittsburg). While advantageous, maintaining expensive equipment within these barriers can be complicated. Therefore, other groups have utilized animal isolation approaches achieved by isolating infected-animals inside sealed, biocontainment devices that can be transported to the imaging equipment housed in standard environments [46, 51, 52] or polycarbonate plastic tubes extending from the biocontainment space to the imaging equipment [53]. A tail vein catheter system was also used for on-table drug delivery to infected animals while sealed inside the biocontainment device [24, 54]. Animal containment allows for easier maintenance of the equipment, which can also be shared with other investigators that do not work within the BSL-3/4 barrier.
Clinical Translation
Unlike traditional microbiological or molecular techniques, imaging can provide key spatial information to dictate treatment, enabling detection and therapeutic monitoring of infections in patients with deep-seated infections for whom traditional clinical samples (e.g., blood, urine) would be insensitive and high risk/impractical (e.g., biopsy for brain infection) or where rapid assessment of therapeutic effect is needed. In fact, in our clinical practice at Johns Hopkins Hospital, oncology patients with fever and neutropenia or patients with fever of unknown origin (FUO) routinely undergo whole body imaging to look for foci of infection. However, current imaging modalities are not specific, and biopsies are often non-diagnostic, leading to uncertainty and overuse (or misuse) of broad-spectrum antimicrobials.
CT and other nuclear medicine techniques are often perceived to deliver high levels of radiation. However, recent technological developments have significantly lowered radiation exposure and also allowed rapid scans that avoids the need for sedation in children. For example, the effective dose for each chest CT in the child treated for XDR-TB was 0.4–0.7 mSv [9]. This is equivalent to 3 months of natural background radiation, a single screening mammography, or four trans-Atlantic airplane round trips [55–57]. Moreover, no sedation was required for this child as scan times were short (3 s). We calculated the risks related to infections, with TB as an example, and compared them to the various imaging techniques used currently (Fig. 2). The risk of mortality for patients with MDR- and XDR-TB on treatment is similar to that due to cancers [8, 52, 58]. Moreover, even patients with drug-susceptible TB on treatment have several orders of magnitude higher risk of mortality than the theoretical risk due to radiation-induced cancers [59, 60]. Development of nuclear imaging tracers with short half-life isotopes and rapid elimination from the body could further limit radiation exposure. While no studies should be performed without an excellent rationale and clinical indication, we need to be pragmatic about the (minimal) risks of imaging, especially when dealing with infections due to MDR organisms.
Fig. 2.
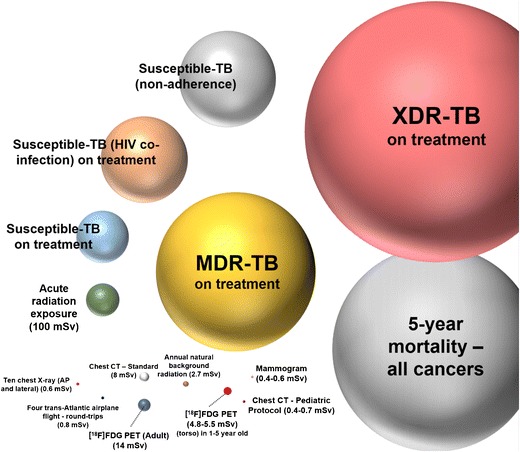
Relative risk of infections with treatment- and radiation-induced cancer. The risk of mortality due to infections (TB as an example) compared to the risk of radiation-induced cancer due to commonly used imaging techniques. The risk of mortality for MDR- and XDR-TB patients on treatment is similar to that due to cancers. Even drug-susceptible TB patients on treatment have significantly higher risk of mortality than radiation-induced cancers with optimized imaging. The risk of radiation-induced cancer and mortality has been theoretically estimated based on acute radiation exposure (100 mSv), and actual risks are likely to be much lower for smaller amounts of radiation.
Given sub-pharmacological dosing, there are several approaches for translating PET tracers to humans [61], allowing more rapid translation of new imaging tools to the clinic. Some PET tracers discussed above are currently being tested in humans. Recently, a study in healthy volunteers demonstrated that 18F-FDS was safe, well tolerated, and rapidly cleared, following a single, intravenous dose [62], suggesting significant potential for use in humans.
Imaging in the Developing World
During the past decade, developing countries, especially the BRICS nations (Brazil, Russia, India, China, South Africa), have witnessed significant increases in the installation and use of advanced imaging. For example, New Delhi (India) alone has >100 clinical MRI scanners (several with 3 T strength) [63, 64]. Moreover, CT, MRI, and PET/CT costs are substantially lower, ~$50–$100 for CT and MRI and $300 for PET per scan at private (for-profit centers) in developing nations such as India than in the USA [53]. Mobile PET scanners and 68Ga PET agents that can be generated without the need of a cyclotron hold great promise for use in remote areas [29]. China has already overtaken the USA to become the largest economy in purchasing power parity, with India expected to become the second largest economy in purchasing power parity by 2050 [65]. Infections are rampant in the developing world, and given the considerable number of people living in big cities, advanced imaging has the potential to become a powerful routine clinical tool for the early diagnosis and monitoring of infectious diseases in developing countries.
Acknowledgements
I would like to thank M. Mahesh (Chief Physicist—Johns Hopkins Hospital) for reviewing the data on the radiation risks related to imaging techniques.
Compliance with Ethical Standards
Funding
This review was funded by the National Institutes of Health (NIH) Director’s Transformative Research Award R01-EB020539 (S.K.J.) and the R01-HL131829 (S.K.J.) as well as NIH Director’s New Innovator Award DP2-OD006492 (S.K.J.). The funders had no role in review design, decision to publish, or preparation of the manuscript.
Conflict of Interest
The author declares that he has no conflict of interest.
References
- 1.McKenna M. Antibiotic resistance: the last resort. Nature. 2013;499:394–396. doi: 10.1038/499394a. [DOI] [PubMed] [Google Scholar]
- 2.Melzer M, Petersen I. Mortality following bacteraemic infection caused by extended spectrum beta-lactamase (ESBL) producing E. coli compared to non-ESBL producing E. coli. J Infect. 2007;55:254–259. doi: 10.1016/j.jinf.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 3.McGann P, Snesrud E, Maybank R, et al. Escherichia coli Harboring mcr-1 and blaCTX-M on a novel IncF plasmid: first report of mcr-1 in the United States. Antimicrob Agents Chemother. 2016;60:4420–4421. doi: 10.1128/AAC.01103-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 5.Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198–1208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC HAI Data and Statistics. https://www.cdc.gov/hai/surveillance/. Accessed 29 Dec 2016
- 7.CDC Seasonal Influenza-Associated Hospitalizations in the United States. https://www.cdc.gov/flu/about/qa/hospital.htm. Accessed 27 Dec 2016
- 8.WHO Global tuberculosis report (2016) http://www.who.int/tb/publications/global_report/gtbr2016_executive_summary.pdf?ua=1. Accessed 29 Dec 2016
- 9.Salazar-Austin N, Ordonez AA, Hsu AJ, et al. Extensively drug-resistant tuberculosis in a young child after travel to India. Lancet Infect Dis. 2015;15:1485–1491. doi: 10.1016/S1473-3099(15)00356-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gandhi NR, Nunn P, Dheda K, et al. Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet. 2010;375:1830–1843. doi: 10.1016/S0140-6736(10)60410-2. [DOI] [PubMed] [Google Scholar]
- 11.Rota PA, Oberste MS, Monroe SS, et al. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 12.WHO Zika virus. http://www.who.int/mediacentre/factsheets/zika/en/. Accessed 29 Dec 2016
- 13.Donnenberg MS. Enterobacteriaceae. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. Philadelphia: Elsevier Inc; 2010. pp. 2815–2833. [Google Scholar]
- 14.Clay H, Volkman HE, Ramakrishnan L. Tumor necrosis factor signaling mediates resistance to mycobacteria by inhibiting bacterial growth and macrophage death. Immunity. 2008;29:283–294. doi: 10.1016/j.immuni.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGavern DB, Kang SS. Illuminating viral infections in the nervous system. Nat Rev Immunol. 2011;11:318–329. doi: 10.1038/nri2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pan H, Yan BS, Rojas M, et al. Ipr1 gene mediates innate immunity to tuberculosis. Nature. 2005;434:767–772. doi: 10.1038/nature03419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harper J, Skerry C, Davis SL, et al. Mouse model of necrotic tuberculosis granulomas develops hypoxic lesions. J Infect Dis. 2012;205:595–602. doi: 10.1093/infdis/jir786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ordonez AA, Tasneen R, Pokkali S, et al. Mouse model of pulmonary cavitary tuberculosis and expression of matrix metalloproteinase-9. Disease Models and Mechanisms. 2016;9:779–788. doi: 10.1242/dmm.025643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murawski AM, Gurbani S, Harper JS, et al. Imaging the evolution of reactivation pulmonary tuberculosis in mice using 18F-FDG PET. J Nucl Med. 2014;55:1726–1729. doi: 10.2967/jnumed.114.144634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin PL, Ford CB, Coleman MT, et al. Sterilization of granulomas is common in active and latent tuberculosis despite within-host variability in bacterial killing. Nat Med. 2014;20:75–79. doi: 10.1038/nm.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scheetz MH, Wunderink RG, Postelnick MJ, Noskin GA. Potential impact of vancomycin pulmonary distribution on treatment outcomes in patients with methicillin-resistant Staphylococcus aureus pneumonia. Pharmacotherapy. 2006;26:539–550. doi: 10.1592/phco.26.4.539. [DOI] [PubMed] [Google Scholar]
- 22.Stein GE, Wells EM. The importance of tissue penetration in achieving successful antimicrobial treatment of nosocomial pneumonia and complicated skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus: vancomycin and linezolid. Curr Med Res Opin. 2010;26:571–588. doi: 10.1185/03007990903512057. [DOI] [PubMed] [Google Scholar]
- 23.van Ingen J, Aarnoutse RE, Donald PR, et al. Why do we use 600 mg of rifampicin in tuberculosis treatment? Clin Infect Dis. 2011;52:e194–e199. doi: 10.1093/cid/cir184. [DOI] [PubMed] [Google Scholar]
- 24.DeMarco VP, Ordonez AA, Klunk M, et al. Determination of [11C]rifampin pharmacokinetics within Mycobacterium tuberculosis-infected mice by using dynamic positron emission tomography bioimaging. Antimicrob Agents Chemother. 2015;59:5768–5774. doi: 10.1128/AAC.01146-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meller J, Sahlmann CO, Scheel AK. 18F-FDG PET and PET/CT in fever of unknown origin. J Nucl Med. 2007;48:35–45. [PubMed] [Google Scholar]
- 26.van Oosten M, Hahn M, Crane LM, et al. Targeted imaging of bacterial infections: advances, hurdles and hopes. FEMS Microbiol Rev. 2015;39:892–916. doi: 10.1093/femsre/fuv029. [DOI] [PubMed] [Google Scholar]
- 27.Auletta S, Galli F, Lauri C, Martinelli D, Santino I, Signore A. Imaging bacteria with radiolabelled quinolones, cephalosporins and siderophores for imaging infection: a systematic review. Clin Transl Imaging. 2016;4:229–252. doi: 10.1007/s40336-016-0185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Love C, Marwin SE, Palestro CJ. Nuclear medicine and the infected joint replacement. Semin Nucl Med. 2009;39:66–78. doi: 10.1053/j.semnuclmed.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Ebenhan T, Zeevaart JR, Venter JD, et al. Preclinical evaluation of 68Ga-labeled 1,4,7-triazacyclononane-1,4,7-triacetic acid-ubiquicidin as a radioligand for PET infection imaging. J Nucl Med. 2014;55:308–314. doi: 10.2967/jnumed.113.128397. [DOI] [PubMed] [Google Scholar]
- 30.Wang X, Murthy N. Bacterial imaging comes of age. Sci Transl Med. 2014;6:259fs243. doi: 10.1126/scitranslmed.3010746. [DOI] [PubMed] [Google Scholar]
- 31.Ordonez AA, Weinstein EA, Bambarger LE, et al. A systematic approach for developing bacteria-specific imaging tracers. J Nucl Med. 2016;58:144–150. doi: 10.2967/jnumed.116.181792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bettegowda C, Foss CA, Cheong I, et al. Imaging bacterial infections with radiolabeled 1-(2′-deoxy-2′-fluoro-beta-D-arabinofuranosyl)-5-iodouracil. Proc Natl Acad Sci U S A. 2005;102:1145–1150. doi: 10.1073/pnas.0408861102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang XM, Zhang HH, McLeroth P, et al. [124I]FIAU: human dosimetry and infection imaging in patients with suspected prosthetic joint infection. Nucl Med Biol. 2016;43:273–279. doi: 10.1016/j.nucmedbio.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Ning X, Seo W, Lee S, et al. PET imaging of bacterial infections with fluorine-18-labeled maltohexaose. Angew Chem Int Ed Engl. 2014;53:14096–14101. doi: 10.1002/anie.201408533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gowrishankar G, Namavari M, Jouannot EB, et al. Investigation of 6-[18F]-fluoromaltose as a novel PET tracer for imaging bacterial infection. PLoS One. 2014;9:e107951. doi: 10.1371/journal.pone.0107951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinstein EA, Ordonez AA, DeMarco VP, et al. Imaging Enterobacteriaceae infection in vivo with 18F-fluorodeoxysorbitol positron emission tomography. Sci Transl Med. 2014;6:259ra146. doi: 10.1126/scitranslmed.3009815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rundell SR, Wagar ZL, Meints LM, et al. Deoxyfluoro-d-trehalose (FDTre) analogues as potential PET probes for imaging mycobacterial infection. Org Biomol Chem. 2016;14:8598–8609. doi: 10.1039/C6OB01734G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrik M, Haas H, Dobrozemsky G, et al. 68Ga-siderophores for PET imaging of invasive pulmonary aspergillosis: proof of principle. J Nucl Med. 2010;51:639–645. doi: 10.2967/jnumed.109.072462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rolle AM, Hasenberg M, Thornton CR, et al. ImmunoPET/MR imaging allows specific detection of Aspergillus fumigatus lung infection in vivo. Proc Natl Acad Sci U S A. 2016;113:E1026–E1033. doi: 10.1073/pnas.1518836113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wiehr S, Warnke P, Rolle AM, et al. New pathogen-specific immunoPET/MR tracer for molecular imaging of a systemic bacterial infection. Oncotarget. 2016;7:10990–11001. doi: 10.18632/oncotarget.7770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santangelo PJ, Rogers KA, Zurla C, et al. Whole-body immunoPET reveals active SIV dynamics in viremic and antiretroviral therapy-treated macaques. Nat Methods. 2015;12:427–432. doi: 10.1038/nmeth.3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen L, Cheng D, Liu G, et al. Detection of Klebsiella. Pneumoniae infection with an antisense oligomer against its ribosomal RNA. Mol Imaging Biol. 2016;18:527–534. doi: 10.1007/s11307-015-0927-4. [DOI] [PubMed] [Google Scholar]
- 43.Wang Y, Chen L, Liu X, et al. Detection of Aspergillus fumigatus pulmonary fungal infections in mice with 99mTc-labeled MORF oligomers targeting ribosomal RNA. Nucl Med Biol. 2013;40:89–96. doi: 10.1016/j.nucmedbio.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu G, Bettegowda C, Qiao Y, et al. Noninvasive imaging of infection after treatment with tumor-homing bacteria using chemical exchange saturation transfer (CEST) MRI. Magn Reson Med. 2013;70:1690–1698. doi: 10.1002/mrm.24955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ordonez AA, Pokkali S, DeMarco VP, et al. Radioiodinated DPA-713 imaging correlates with bactericidal activity of tuberculosis treatments in mice. Antimicrob Agents Chemother. 2015;59:642–649. doi: 10.1128/AAC.04180-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis SL, Nuermberger EL, Um PK, et al. Noninvasive pulmonary [18F]-2-fluoro-deoxy-D-glucose positron emission tomography correlates with bactericidal activity of tuberculosis drug treatment. Antimicrob Agents Chemother. 2009;53:4879–4884. doi: 10.1128/AAC.00789-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sathekge M, Maes A, Kgomo M, Stoltz A, Van de Wiele C. Use of 18F-FDG PET to predict response to first-line tuberculostatics in HIV-associated tuberculosis. J Nucl Med. 2011;52:880–885. doi: 10.2967/jnumed.110.083709. [DOI] [PubMed] [Google Scholar]
- 48.Jain SK, Lamichhane G, Nimmagadda S, Pomper MG, Bishai WR. Antibiotic treatment of tuberculosis: old problems, new solutions. Microbe. 2008;3:285–292. [Google Scholar]
- 49.Chen RY, Dodd LE, Lee M, et al. PET/CT imaging correlates with treatment outcome in patients with multidrug-resistant tuberculosis. Sci Transl Med. 2014;6:265ra166. doi: 10.1126/scitranslmed.3009501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bocan TM, Panchal RG, Bavari S. Applications of in vivo imaging in the evaluation of the pathophysiology of viral and bacterial infections and in development of countermeasures to BSL3/4 pathogens. Mol Imaging Biol. 2015;17:4–17. doi: 10.1007/s11307-014-0759-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davis SL, Be NA, Lamichhane G, et al. Bacterial thymidine kinase as a non-invasive imaging reporter for Mycobacterium tuberculosis in live animals. PLoS One. 2009;4:e6297. doi: 10.1371/journal.pone.0006297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tucker EW, Pokkali S, Zhang Z, et al. Microglia activation in a pediatric rabbit model of tuberculous meningitis. Dis Model Mech. 2016;9:1497–1506. doi: 10.1242/dmm.027326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lackemeyer MG, Kok-Mercado F, Wada J, et al. ABSL-4 aerobiology biosafety and technology at the NIH/NIAID integrated research facility at Fort Detrick. Viruses. 2014;6:137–150. doi: 10.3390/v6010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weinstein EA, Liu L, Ordonez AA, et al. Noninvasive determination of 2-[18F]-fluoroisonicotinic acid hydrazide pharmacokinetics by positron emission tomography in Mycobacterium tuberculosis-infected mice. Antimicrob Agents Chemother. 2012;56:6284–6290. doi: 10.1128/AAC.01644-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hendrick RE. Radiation doses and cancer risks from breast imaging studies. Radiology. 2010;257:246–253. doi: 10.1148/radiol.10100570. [DOI] [PubMed] [Google Scholar]
- 56.Guidance: ionising radiation: dose comparisons. https://www.gov.uk/government/publications/ionising-radiation-dose-comparisons/ionising-radiation-dose-comparisons. Accessed 28 Dec 2016
- 57.Mettler FA, Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 58.Chung-Delgado K, Guillen-Bravo S, Revilla-Montag A, Bernabe-Ortiz A. Mortality among MDR-TB cases: comparison with drug-susceptible tuberculosis and associated factors. PLoS One. 2015;10:e0119332. doi: 10.1371/journal.pone.0119332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nahid P, Jarlsberg LG, Rudoy I, et al. Factors associated with mortality in patients with drug-susceptible pulmonary tuberculosis. BMC Infect Dis. 2011;11:1. doi: 10.1186/1471-2334-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grant FD, Gelfand MJ, Drubach LA, Treves ST, Fahey FH. Radiation doses for pediatric nuclear medicine studies: comparing the North American consensus guidelines and the pediatric dosage card of the European Association of Nuclear Medicine. Pediatr Radiol. 2015;45:706–713. doi: 10.1007/s00247-014-3211-x. [DOI] [PubMed] [Google Scholar]
- 61.Mosessian S, Duarte-Vogel SM, Stout DB, et al. INDs for PET molecular imaging probes-approach by an academic institution. Mol Imaging Biol. 2014;16:441–448. doi: 10.1007/s11307-014-0735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhu W, Yao S, Xing H, et al. Biodistribution and radiation dosimetry of the Enterobacteriaceae-specific imaging probe [18F]fluorodeoxysorbitol determined by PET/CT in healthy human volunteers. Mol Imaging Biol. 2016;18:782–787. doi: 10.1007/s11307-016-0946-9. [DOI] [PubMed] [Google Scholar]
- 63.Jankharia GR. Commentary—radiology in India: the next decade. Indian J Radiol Imaging. 2008;18:189–191. doi: 10.4103/0971-3026.41868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jha S (2015) Radiology in India: trends in medical imaging technology. http://www.auntminnie.com/index.aspx?sec=ser&sub=def&pag=dis&ItemID=110035. Accessed 28 Dec 2016
- 65.The World in 2050. http://www.pwc.com/gx/en/issues/the-economy/assets/world-in-2050-february-2015.pdf. Accessed 29 Dec 2016


