Abstract
Primary extranodal Hodgkin lymphoma (HL) is very rare. We report the first case of primary renal Hodgkin lymphoma and with the absence of supra- and sub-diaphragmatic adenopathy.
Keywords: Hodgkin lymphoma, Kidney, Lymphoma, Renal pelvis
Abbreviations: HL, Hodgkin lymphoma; CT, computed tomography; MR, magnetic resonance; DWI, diffusion weighted image; PET, positron emission tomography
Introduction
Hodgkin lymphoma (HL) is a malignant neoplasm of lymphoid tissues. Cervical lymphadenopathy is the most common head and neck presentation for HL.
Presentation with extranodal disease is quite unusual, although HL is known to occasionally involve extranodal sites. However, no well-documented cases of renal pelvic HL have been described. We report the case of an 85-year-old man who presented with incidentally found as right renal pelvic mass.
Case presentation
An 85-year-old male present with incidentally found as incidental right renal pelvic mass in follow-up computed tomography (CT) post cholecystectomy due to gallbladder cancer 5 month previously.
Physical examination was normal. Hematological and biochemical investigations, including a liver function profile and renal function tests, were normal. Routine urinalysis was unremarkable and urine cytology showed class III. There was no lymphadenopathy or any other mass palpated.
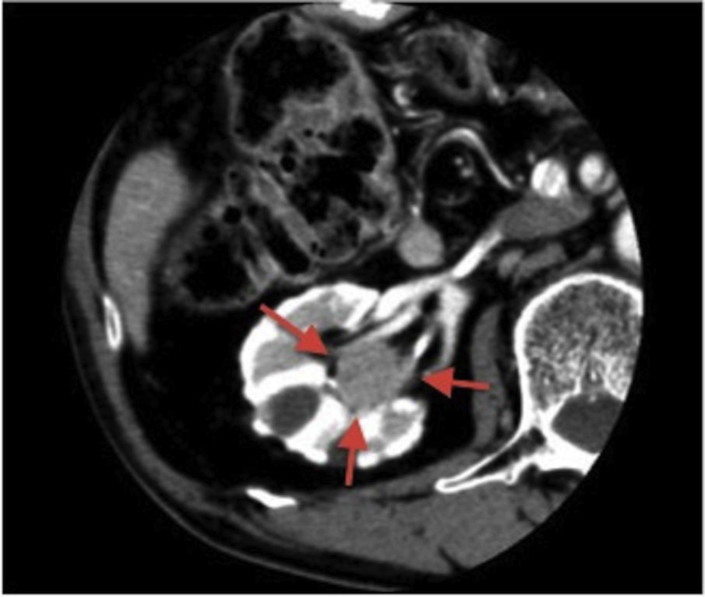
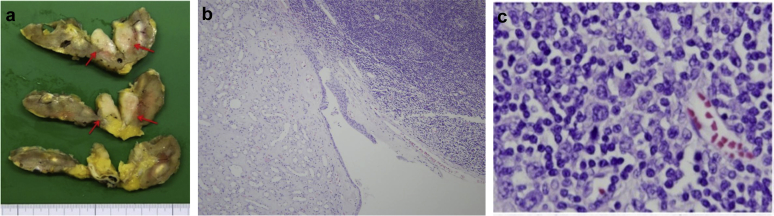
Axial contrast-enhanced CT scan obtained a homogenous 30 × 33 mm poor enhanced mass (arrow) in the right renal pelvis (Fig. 1). Coronal T2-weighted magnetic resonance (MR) image shows the low signal-intensity filling defect mass in the right renal pelvis. Diffusion weighted image (DWI) exhibits high signal intensity. According to these examinations, we diagnosed this case as right renal pelvic tumor. A right nephroureterectomy was accomplished. The specimen consisted of kidney with its an ureter and bladder cuff. The kidney measured 9.0 × 5.0 × 5.0 cm. In the renal pelvis 2.5 × 2.2 cm yellowish-white mass was included (Fig. 2a). But on microscopic examination, the mass was located just under submucosal area of renal pelvis and did not infiltrate the renal parenchyma (Fig. 2b). And the tumor was composed of a polymorphic population of cells including many eosinophils and atypical mononuclear cells. Reed-Sternberg cells were also seen at places (Fig. 2c). Histopathology study revealed HL of renal pelvis. Immunostaining showed that the large atypical cells were positive for CD30 (ki-1) while CD3, CD5, CD10, and CD20 were negative. These features were consistent with the diagnosis of HL of mixed cellular variety.
Figure 1.
A computer tomographic scan shows a homogenous 30 × 33 mm poor enhanced mass (arrow) in the right renal pelvis.
Figure 2.
(a) The macroscopic findings of renal pelvic tumor (arrow). (b) Low power view of the tumor shows that the tumor was located just under submucosal area of renal pelvis and did not infiltrate the renal parenchyma. (c) Medium power view of the nodule shows scattered large atypical Reed-Sternberg cells and variants in a background of small lymphocytes, histiocytes, and eosinophils.
Discussion
HL rarely involves genitourinary organ systems at presentation.1, 2 Renal involvement is extremely rare, HL being rather perirenal. Indeed, its radiologic appearance often consists of invasion of the perirenal space by HL without renal parenchymal involvement. CT (versus urography or US) is the diagnostic modality of choice for detecting renal or perirenal masses.3 And ureteral involvement is extremely rare. Only one case of HL with a ureteral origin has been reported.4 Bladder involvement is also extremely rare. The only two reported cases involved a nonspecific filling defect arising from the bladder wall.5
HL is a nodal malignancy that is now largely curable. At presentation, HL is usually supradiaphragmatic, with contiguous spread often occurring predictably from one nodal group to the next along the lymphatic pathways. HL is usually almost entirely confined to the lymphnodes. Extranodal involvement is much less common in HL than in non-HL. Extranodal invasion of adjacent tissue is seen in up to 15% of cases and hematogenous spread in 5–10%.2 Even when dissemination occurs beyond the lymphoreticular system, certain patterns of associated spread are frequently evident. Extranodal involvement (except in the spleen and thymus) indicates stage IV HL. Initial staging is crucial for demonstrating the presence of extranodal involvement, which will affect therapeutic decisions. First contiguous (E-stage) disease, which requires local radiation therapy, must be distinguished from stage IV disease, which is treated with chemotherapy alone or combined with general radiation therapy. Second, the extent of extranodal involvement must be evaluated because it is considered prognostic. The patient was discharged 18 days following surgery. As outpatient examination, positron emission tomography (PET-CT) was accomplished whether other nodal sites of HL exist or not. The PET-CT showed no other metastatic sites. So in this case, the final diagnosis was given as HL of the renal pelvis.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Castellino R.A. Imaging techniques for staging abdominal Hodgkin’s disease. Cancer Treat Rep. 1982;66:697–700. [PubMed] [Google Scholar]
- 2.Guermazi A., Brice P., de Kerviler E.E. Extranodal Hodgkin disease: spectrum of disease. Radiographics. 2001;21:161–179. doi: 10.1148/radiographics.21.1.g01ja02161. [DOI] [PubMed] [Google Scholar]
- 3.Reznek R.H., Mootoosamy I., Webb J.A.W., Richards M.A. CT in renal and perirenal lymphoma: a further look. Clin Radol. 1990;42:233–238. doi: 10.1016/s0009-9260(05)82109-9. [DOI] [PubMed] [Google Scholar]
- 4.Tozzini A., Bulleri A., Orsitto E. Hodgkin’s lymphoma: an isolated case of involvement of the ureter. Eur Radiol. 1999;9:344–346. doi: 10.1007/s003300050677. [DOI] [PubMed] [Google Scholar]
- 5.Jones M.W. Primary Hodgkin’s disease of the urinary bladder. Br J Urol. 1989;63:438. doi: 10.1111/j.1464-410x.1989.tb05236.x. [DOI] [PubMed] [Google Scholar]