Abstract
Background:
Patients undergoing coronary artery bypass graft (CABG) procedures have higher incidence of difficult laryngoscopy and intubation than general surgery population. Accurate prediction of difficult laryngoscopy in CABG patients is desirable to reduce the hemodynamic response and myocardial oxygen requirements. Recently, thyromental height test (TMHT) has been proposed as one of the highly sensitive and specific bedside tests to predict difficult airway. We, in our prospective observational study, evaluated the accuracy of the TMHT in predicting difficult laryngoscopy.
Methodology:
A total of 345 patients undergoing CABG of either sex, in the age group of 35–80 years, American Society of Anesthesiologists 111, undergoing CABG, were studied. Airway assessment was performed with modified Mallampati test with the addition of thyromental distance, sternomental distance, and TMHT. Intraoperatively, direct laryngoscopy was done in accordance with Cormack and Lehane grade of laryngoscopy. The preoperative data and laryngoscopic findings were used together to evaluate the accuracy of TMHT. The sensitivity, specificity, positive and negative predictive values of other three tests were calculated according to standard formula.
Results:
A total of 345 patients were in the group with mean age of study population at 56.7 (standard deviation 9.1) years (35–80 years). This study showed that almost all tests had good specificity, but sensitivity was poor. However, sensitivity of TMHT was 75% with accuracy of 95%. Receiver operating characteristic curve analysis of TMHT-derived cutoff was 52.17 which increased sensitivity to 81.25% and specificity to 92.3%.
Conclusion:
TMHT had a higher sensitivity compared to other tests along with good positive and negative predictive value and a very high specificity.
Keywords: Airway, Cormack–Lehane, laryngoscopy, thyromental height
Introduction
Patients undergoing coronary artery bypass graft (CABG) procedures require general anesthesia with endotracheal intubation. They have higher incidence of difficult laryngoscopy than other patients because of the associated risk factors such as older age, dental problems, limited neck movements,[1] obesity, hypertension, and diabetes.[2] The incidence of difficult laryngoscopy in CABG patients is estimated to be 10%.[1]
Direct laryngoscopy and endotracheal intubation result in sympathetic stimulation that can lead to tachycardia and hypertension. Among many bedside available tests, there is a need for a test with high sensitivity, specificity, and positive predictive value to predict difficult airway.
Recently, thyromental height test (TMHT) has been proposed as a surrogate for frequently cited anthropometric measures. We, in our prospective, observational study, tried to evaluate the accuracy of the TMHT in predicting difficult laryngoscopy in CABG patients.
Methodology
A prospective, observational study was conducted with the approval of hospital's ethics committee. A total of 345 patients, in between July 2015 and November 2015, were included in the study. Informed written consent was obtained from all the patients. Inclusion criteria were patients scheduled for coronary artery bypass surgery under general anesthesia aged between 35 and 80 years of either sex. Patients with known abnormalities or obvious malformations of the airway, pregnant patients, and patients for emergency surgeries were excluded from the study.
Preoperative evaluation
After taking a detailed history, a thorough physical and systemic examination was carried out.
Airway assessment included mouth opening, assessment of receding mandible or protruding upper teeth, and subjective assessment of head and neck extension.
The following four predictive test measurements were obtained and recorded:
Modified Mallampati Classification: Mallampati classification was modified by Samson and Young[3] with patient in the sitting position, mouth maximally opened, and tongue protruded, while the observer looking from the patient's eye level will inspect the pharyngeal structures with a pen torch, without the patient phonating. The oropharyngeal view is graded as Class I where soft palate, fauces, uvula, pillars visible; Class II where soft palate, fauces, uvula visible; Class III where soft palate, base of uvula visible; and Class IV where soft palate not visible at all. Class III and IV are classified as difficult intubation[4]
Thyromental distance (TMD) was measured as straight distance between the thyroid notch and the lower border of mental prominence, with the head fully extended and the mouth closed, using a rigid ruler. A measurement of ≤6.5 cm was considered to be a predictor of difficult intubation[5]
Sternomental distance (SMD): It is the distance in centimeters as straight distance between the superior border of the manubrium sterni and the bony point of the mentum, with the head in full extension and the mouth closed using a rigid ruler. An SMD ≤13.5 cm was considered predictive of difficult laryngoscopy[5,6,7]
The TMHT was performed as follows: The height between the anterior border of the thyroid cartilage (on the thyroid notch just between the two thyroid laminae) and the anterior border of the mentum (on the mental protuberance of the mandible) was measured, with the patient lying supine using a pillow with her/his mouth closed [Figures 1 and 2]. This height was measured with a digital depth gauge (INSIZE® Electronic Depth Gage, INSIZE Co Ltd., Suzhou New District, China).
Figure 1.

Measurement of thyromental height; while the patient lies supine with her/his mouth closed, the line
Figure 2.

Measurement of thyromental height using a depth gauge
All the patients were premedicated, the night before surgery, with tablet pantoprazole 40 mg and tablet diazepam 5 mg. Patients were kept nil oral overnight before the surgery.
Induction of anesthesia
After securing the IV line and arterial line, baseline values of invasive arterial blood pressure, heart rate, electrocardiogram, and oxygen saturation were recorded. After preoxygenation, general anesthesia was induced with titrated doses of fentanyl (2–3 mcg/kg) and midazolam (0.1 mg/kg) and propofol, and before administering muscle relaxant, mask ventilation was checked. Pancuronium bromide (0.1 mg/kg) was used for neuromuscular blockade. Patients were ventilated manually with isoflurane (1% end tidal) in oxygen using facemask, and laryngoscopy was done at the end of 3 min. The laryngoscopy was performed in sniffing position, using Macintosh blade size 3 or 4 by a conventionally trained anesthesiologist. If no laryngeal view was achieved, an external backward, upward, and rightward laryngeal pressure 46 was applied, and the view was classified as per Cormack–Lehane's (CL) scale as follows.
Cormack and Lehane classification
Grade I - full view of the glottis; Grade II - glottis partially exposed, posterior commissure not seen; Grade III - only epiglottis seen; Grade IV - epiglottis not seen.
Difficult visualization was described as Grade III and IV classification. 11 Easy visualization was described as Grade I and II classification.
The preoperative assessment data and laryngoscopy findings were used together to evaluate the accuracy of TMHT in predicting difficult laryngoscopy.
Statistical analysis was done using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA; version 22.0 for Windows) software. Yate's and Fisher's Chi-square tests were used to test the significance of difference for qualitative variables. P < 0.05 was taken to denote significant difference. Usefulness of various tests for identifying difficult intubation was evaluated by Bayesian method in terms of sensitivity, specificity, accuracy, positive predictive value, and negative predictive value. A high sensitivity is desirable as it will identify most patients in whom intubation will truly be difficult. Specificity indicates the number of patients in whom intubations will be correctly predicted as easy. Positive predictive value identifies the number of patients predicted to have difficult intubation and a negative predictive value signifies the number of patients correctly predicted not to have difficult intubation.
Results
Data from 345 patients revealed that 90.7% patients had easy intubation while 9.3% had difficult airway management.
Demographic data
Mean age of the chosen patients was 56.7 years; mean height and weight being 162 and 65.3 cm, respectively, with mean BMI of 24.72 kg/m2. Sensitivity, specificity, accuracy, positive predictive value Refer to Table 1, and negative predictive value were calculated for all the tests individually.
Table 1.
Height/weight/body mass index
| Variable | Range | Mean | SD |
|---|---|---|---|
| Height (cm) | 136-180 | 162.6 | 7.9 |
| Weight (kg) | 43-88 | 65.3 | 7.3 |
| BMI (kg/m2) | 16.97-35.03 | 24.72 | 2.74 |
SD: Standard deviation, BMI: Body mass index
It shows that almost all tests have a good specificity and negative predictive value.
However, the sensitivity is poor.
Sensitivity of TMHT has shown the best result of 75%.
Accuracy of modified Mallampati test (MMT) has come as only 79% whereas TMHT was most accurate with an accuracy of 95%.
Receiver operating characteristic curve analysis of the thyromental height was drawn for predicting difficult laryngoscopy which derived a cutoff of 52.17. If we use this, sensitivity is increased to 81.25% though specificity becomes 92.33%. Although true negative will decrease by this, true positive will also increase which is more appropriate as we are concerned with difficult laryngoscopy more than identifying an easy laryngoscopy.
Discussion
Unanticipated difficult airway is a major concern for an anesthesiologist.[14] The need to predict potentially difficult tracheal intubation with an accurate marker, even before laryngoscopy, has received more importance but with limited success. It has been observed that predictors such as weight, head and neck movement, jaw movement, receding mandible, buck teeth, modified Mallampati classification, TMD, SMD, mouth opening, and Wilson risk score are not (refer to Figure 3, also refer to Table 2) foolproof to predict a difficult intubation.[8] Hence, there is a need for a test, which is (a) quick and easy to perform; (b) is highly sensitive (so that majority of difficult cases can be identified); and (c) highly specific (so that false-positive rate will be low when the test is used routinely). Any test devised should be easy to perform and interpret at the bedside. Etezadi et al.[9] validated the use of TMHT. We have used similar protocol, but our study population was patients with coronary artery disease undergoing CABG. In our study, we decided to assess the efficacy of this test in the patients undergoing CABG along with other standard airway assessments so that we can have an additional tool to predict difficult laryngoscopy in these patients. Incidence of difficult laryngoscopy in CABG surgery is 10%.[1] In our study, out of 345 patients, 32 (9.3%) had difficult airway management.
Figure 3.
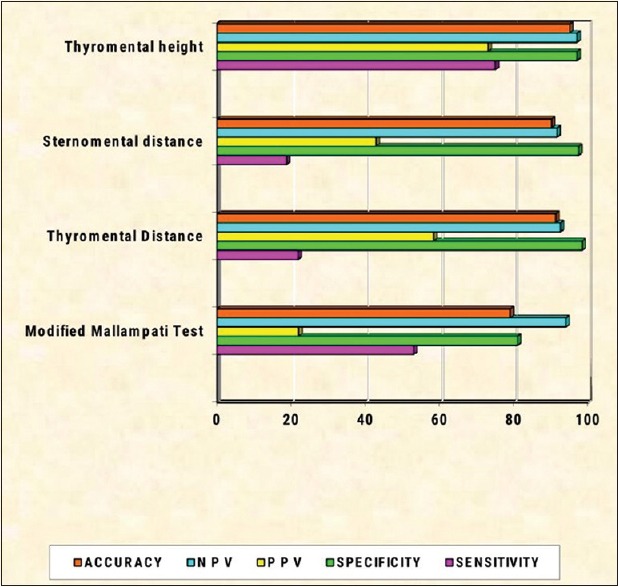
All the parameters are compared as obtained by the various tests
Table 2.
Efficacy of different tests as per the ease of laryngoscopy
| Cormack-Lehane grade | Significance | ||
|---|---|---|---|
| Difficult (%) | Easy (%) | ||
| MMT | |||
| Difficult (76) | 17 (22.4) | 59 (77.6) | P<0.0001 (S) |
| Easy (269) | 15 (56) | 254 (94.4) | |
| TMD | |||
| Difficult (12) | 7 (58.33) | 5 (41.66) | P<0.0001 (S) |
| Easy (333) | 25 (7.5) | 308 (92.49) | |
| SMD | |||
| Difficult | 6 (42.85) | 8 (57.14) | P<0.0007 (S) |
| Easy | 26 (7.85) | 305 (92.14) | |
| TMHT | |||
| Difficult (33) | 24 (72.7) | 9 (27.3) | P<0.0001 (S) |
| Easy (312) | 8 (2.6) | 304 (97.4) | |
S: Significant, MMT: Modified Mallampati test, TMD: Thyromental distance, SMD: Sternomental distance, TMHT: Thyromental height test
In our study, the prediction of difficult laryngoscopy was done by MMT, TMD, SMD, and thyromental height during preoperative assessment and correlating it to CL laryngoscopy grading at intubation. MMT Class III and IV, TMD ≤6.5 cm, SMD ≤13.5 cm, and CL Grade III and IV were considered as predictors of difficult intubation. Among these, CL grading was considered as gold standard, other tests were compared with this.
MMT is one of the most commonly performed predictive tests. In our study, out of 345 patients, 269 patients’ MMT class was observed to be I and II, and in 76 patients, it was observed to be III and IV. Specificity was found to be 81%, sensitivity was 53%, negative predictive value was 94%, but positive predictive value was only 22%. We found that MMT has a sensitivity of 53% and positive predictive value of 22% in modified Mallampati classification of all the patients.
Etezadi et al.[9] found sensitivity of 21%, specificity of 80.41%, and positive predictive value of only 8%. Oates et al.[10] and Iohom et al.[7] also found the sensitivity of Mallampati test to be 42% and 43%, respectively. We could not comment on interobserver variation as only one observer determined the modified Mallampati classification of all the patients. Hence, we conclude that MMT has a good specificity but low sensitivity and poor predictive value which correlates with many of the studies.
In our study of TMD, we found sensitivity of 22%, specificity of 98%, positive predictive value of 58%, and negative predictive value of 92.5%. Etezadi et al.[9] found its specificity as 80% and sensitivity as 26% which is comparable with our study. This was comparatively lesser as seen in other studies.[11,12,13]
In our study, SMD specificity was found to be 97.5%, sensitivity was 19%, positive predictive value was 43%, and negative predictive value was 92%. Etezadi et al.[9] found its positive predictive value lesser (10.71%). The poor sensitivity of this test was also seen in other studies. SMD has high specificity but a very poor sensitivity and positive predictive value.
In our study, mean of TMHT was 57.82 mm. In our study, we had a cutoff value of 50 mm as used by Etezadi et al.[9] We found 33 patients having TMHT <50 mm. In 345 patients studied, true positive, false positive, true negative, and false negative results were found in 24, 9, 304, and 8, respectively. And also, sensitivity was 75%, specificity was 97%, positive predictive value was 73%, negative predictive value was 97%, and accuracy was 95% [See Figure 4]. Etezadi et al.[9] found sensitivity of 82.6%, specificity of 99.31%, positive predictive value of 90.47%, negative predictive value of 98.63%, and accuracy of 98.08% of the TMHT.
Figure 4.
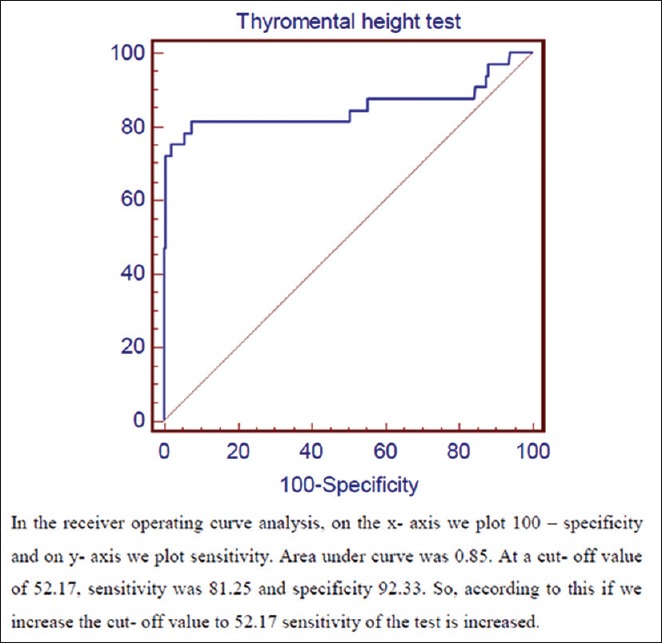
Receiver operating characteristic curve
TMHT thus has a good sensitivity and specificity in comparison to other tests. In our study, we found accuracy of TMHT as 95% which is higher than the other tests [Refer to Table 3].
Table 3.
Comparative efficacy of the four tests
| Parameters | Value as per | |||
|---|---|---|---|---|
| MMT (%) | TMD test (%) | SMD test (%) | TMHT (%) | |
| True positive | 17 | 7 | 6 | 24 |
| False positive | 59 | 5 | 8 | 9 |
| True negative | 254 (73) | 308 (89) | 305 (88) | 304 (88) |
| False negative | 15 | 25 | 26 | 8 |
| Sensitivity | 53 | 22 | 19 | 75 |
| Specificity | 81 | 98 | 97 | 97 |
| Positive predictive value | 22 | 58 | 43 | 73 |
| Negative predictive value | 94 | 92 | 92 | 97 |
| Accuracy | 79 | 91 | 90 | 95 |
True positive: A difficult laryngoscopy that had been predicted to be difficult. False positive: An easy laryngoscopy that had been predicted to be difficult. True negative: An easy laryngoscopy that had been predicted to be easy. False negative: A difficult laryngoscopy that had been predicted to be easy. MMT: Modified Mallampati test, TMD: Thyromental distance, SMD: Sternomental distance, TMHT: Thyromental height test
Conclusion
TMHT is a simple yet useful and important test involving the measurement of external anatomic structures in predicting a difficult laryngoscopy preoperatively. It was found to be more accurate than modified Mallampati classification, TMD, and SMD. TMHT was the only test which had a high sensitivity compared to others along with a good positive and negative predictive value and a very high specificity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ezri T, Weisenberg M, Khazin V, Zabeeda D, Sasson L, Shachner A, et al. Difficult laryngoscopy: Incidence and predictors in patients undergoing coronary artery bypass surgery versus general surgery patients. J Cardiothorac Vasc Anesth. 2003;17:321–4. doi: 10.1016/s1053-0770(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 2.Hogan K, Rusy D, Springman SR. Difficult laryngoscopy and diabetes mellitus. Anesth Analg. 1988;67:1162–5. [PubMed] [Google Scholar]
- 3.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 4.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 5.Krishna HM, Agarwal M, Dali JS, Tampal P. Role of ratio of patient's height to thyromental distance for prediction of difficult airway in Indian population. J Clin Pharmacol. 2005;21:257–60. [Google Scholar]
- 6.Prakash S, Kumar A, Bhandari S, Mullick P, Singh R, Gogia AR. Difficult laryngoscopy and intubation in the Indian population: An assessment of anatomical and clinical risk factors. Indian J Anaesth. 2013;57:569–75. doi: 10.4103/0019-5049.123329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iohom G, Ronayne M, Cunningham AJ. Prediction of difficult tracheal intubation. Eur J Anaesthesiol. 2003;20:31–6. doi: 10.1017/s0265021503000061. [DOI] [PubMed] [Google Scholar]
- 8.Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–6. doi: 10.1093/bja/61.2.211. [DOI] [PubMed] [Google Scholar]
- 9.Etezadi F, Ahangari A, Shokri H, Najafi A, Khajavi MR, Daghigh M, et al. Thyromental height: A new clinical test for prediction of difficult laryngoscopy. Anesth Analg. 2013;117:1347–51. doi: 10.1213/ANE.0b013e3182a8c734. [DOI] [PubMed] [Google Scholar]
- 10.Oates JD, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. Br J Anaesth. 1991;66:305–9. doi: 10.1093/bja/66.3.305. [DOI] [PubMed] [Google Scholar]
- 11.Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: A prospective blind study. Anesth Analg. 1995;81:254–8. doi: 10.1097/00000539-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Qudaisat IY, Al-Ghanem SM. Short thyromental distance is a surrogate for inadequate head extension, rather than small submandibular space, when indicating possible difficult direct laryngoscopy. Eur J Anaesthesiol. 2011;28:600–6. doi: 10.1097/EJA.0b013e328347cdd9. [DOI] [PubMed] [Google Scholar]
- 14.Aitkenhead AR. Injuries associated with anaesthesia. A global perspective. Br J Anaesth. 2005;95:95–109. doi: 10.1093/bja/aei132. [DOI] [PubMed] [Google Scholar]


