Abstract
Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The ACR considers adherence to these guidelines and recommendations to be voluntary, with the ultimate determination regarding their application to be made by the physician in light of each patient's individual circumstances. Guidelines and recommendations are intended to promote beneficial or desirable outcomes but cannot guarantee any specific outcome. Guidelines and recommendations developed or endorsed by the ACR are subject to periodic revision as warranted by the evolution of medical knowledge, technology, and practice.
The American College of Rheumatology is an independent, professional, medical and scientific society which does not guarantee, warrant, or endorse any commercial product or service.
Introduction
The American College of Rheumatology (ACR) published treatment recommendations for juvenile idiopathic arthritis (JIA) in 2011 (1). These recommendations represented the first such effort by the ACR that focused entirely on the treatment of a pediatric rheumatic disease, and included recommendations for the initial and subsequent treatment of patients with synovitis and systemic manifestations and recommendations for medication safety monitoring. Also included in the recommendations was a statement regarding potential areas for a subsequent update. Based on the progress made understanding the pathophysiology of systemic JIA and a rapid increase in data regarding the treatment of systemic JIA and how it differs from other categories of JIA, the ACR determined that the treatment of systemic JIA should be the focus of the first update.
Systemic JIA accounts for approximately 4–15% of JIA and is defined as arthritis in ≥1 joint for at least 6 weeks' duration in a child age <16 years with or preceded by fever of at least 2 weeks' duration that is documented to be daily (“quotidian”) for at least 3 days and accompanied by one or more of the following: evanescent erythematous rash, generalized lymphadenopathy, hepatomegaly or splenomegaly, and serositis (2). The goal of therapy for systemic JIA is similar to that of the other categories of JIA, and focuses on the prompt control of active inflammation and symptoms and the prevention of a number of disease-and/or treatment-related morbidities such as growth disturbances, joint damage, and functional limitations. Many children with systemic JIA have a particularly refractory course, with persistent disease associated with a high risk of joint damage and severe growth impairment (3–5). However, the inflammatory process underlying systemic JIA appears to be distinct from other categories of JIA, with a central role for both interleukin-1 (IL-1) and IL-6 (6,7). Treatments specifically targeting both of these cytokines are now available, and recently there has been a significant increase in the amount of published data regarding their efficacy. Furthermore, approximately 10% of children with systemic JIA develop overt clinical features of macrophage activation syndrome (MAS), a life-threatening condition characterized by fever, organomegaly, cytopenias, hyperferritinemia, hypertriglyceridemia, hypofibrinogenemia, and coagulopathy, among other findings (7–9). The mortality rate for children hospitalized with systemic JIA and MAS is estimated to be as high as 6%, but may even be higher based on estimates from case series (10,11). Systemic JIA is therefore the focus of this update, providing the opportunity to address the treatment of this unique inflammatory process and associated MAS features.
In addition, in response to public comment, this update also includes recommendations for repeat tuberculosis (TB) screening for all categories of JIA patients receiving biologic agents, in order to address questions about followup screening for children receiving these medications for longer durations and the risk of false-positive results associated with annual TB screening performed without regard for risk factors.
As with the previously published ACR recommendations and as specified by the RAND/University of California, Los Angeles (UCLA) Appropriateness Method, cost implications were not considered in assembling these recommendations. The use of combination therapy with a biologic agent was also not considered, due to safety concerns and lack of data. Furthermore, as with the original 2011 ACR JIA treatment recommendations, the results of this project should be considered “recommendations,” and are meant to serve as a reference for health care providers caring for children with JIA. These recommendations are not intended to take the place of physician judgment and shared decision making with patients and are not intended to limit the coverage of medications used in the treatment of JIA. Likewise, these recommendations are intended to offer guidance for providers caring for children with the most common phenotypes associated with systemic JIA, rather than exceptional cases with unusual disease manifestations or refractory disease.
A document containing the 2011 ACR JIA treatment recommendations and the 2013 updated recommendations is provided in Supplementary Appendix A (available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22087/abstract).
Materials and Methods
The ACR reviews its recommendations approximately annually to determine whether a partial update or full revision is warranted, based on changes in supporting evidence and available therapies. In early 2012, the ACR decided that an update to its 2011 JIA recommendations was necessary, specifically in the area of systemic JIA. The ACR leadership subsequently approached the team of investigators who had developed the 2011 JIA guidelines and, through discussions with this group and additional pediatric rheumatologists, assembled a new team to develop the 2013 JIA update.
This project complied with ACR guideline development policies related to disclosure and conflicts of interest. All participants disclosed their relationships at several different points during the process. Disclosures were specifically shared with other participants (e.g., in writing and verbally during meetings), posted online as part of the protocol released for public comment, disclosed during manuscript review, and disclosed in the final manuscript. Per ACR policy, no more than 49% of the Core Expert Panel (CEP) and Task Force Panel (TFP) members had conflicts of interest at any time during this project, and the principal investigators (PIs; SR and PFW) maintained their unconflicted status throughout the project.
The recommendations were developed using the RAND/ UCLA Appropriateness Method, which was also used in the development of the 2011 ACR JIA treatment recommendations (1,12). A CEP, consisting of 11 pediatric rheumatologists experienced in the management of JIA and actively involved in JIA research, assisted with refining the scope of this update, developing the literature search strategy and Evidence Report, and finalizing the clinical scenarios. A TFP, consisting of 12 experts in the field of JIA, including participants from Europe and Canada, participated in 2 rounds of voting on the clinical scenarios. Effort was made to include participants from different geographic locations, with variable time since completion of training and different practice focuses. Thirteen of the CEP and TFP participants also had been involved in the development of the 2011 ACR JIA treatment recommendations.
During the voting rounds, members of the TFP rated the appropriateness of each scenario using a 1–9 ordinal scale, as recommended by the RAND/UCLA method (12). Prior to voting, members of the TFP received a Voter's Handbook that included detailed descriptions of the clinical scenarios and voting instructions, and an Evidence Report summarizing results of the systematic review described below. In the first round, the TFP members cast their votes independently by e-mail. At the subsequent face-to-face meeting, TFP members received a summary of the group's anonymous responses for each scenario, with their own individual responses and the group median responses clearly indicated. Discussions at the face-to-face meeting focused primarily on scenarios where there was disagreement among the TFP members, with the goal of the discussion being not to force consensus, but to ensure that all panel members understood and interpreted the scenario and the available evidence in a similar way. A general pediatrician and evidence-based medicine expert and a parent of a child with systemic JIA also participated in the face-to-face meeting discussion to provide additional perspective and input, but did not vote.
Scope of the recommendations
The overarching objective of this project was to update the 2011 ACR recommendations for the use of nonbiologic disease-modifying anti-rheumatic drugs (DMARDs) and biologic DMARDs in the treatment of systemic JIA. The specific aims of the project were to 1) update the 2011 ACR recommendations regarding indications for starting nonbiologic DMARDs and biologic DMARDs for systemic JIA and indications for switching between nonbiologic DMARDs and biologic DMARDs for systemic JIA; 2) incorporate the use of anti–IL-1 and anti–IL-6 therapies into the ACR recommendations for the treatment of systemic JIA; and 3) develop treatment recommendations for patients with the following 3 general systemic JIA phenotypes: significant systemic features and varying degrees of synovitis, significant arthritis and no significant systemic features, and features concerning for MAS. The aims were specified in the project protocol that was posted online for public comment by the ACR from June to July 2012. In response to public comment, an additional aim was added to the scope to provide recommendations for repeat annual TB screening among children with all categories of JIA who had a negative baseline TB evaluation.
Development of the Evidence Report
Systematic literature review
The literature search strategy was developed by the project's PIs (SR and PFW), a medical research librarian, and the CEP. The search strategy underwent peer review by an additional medical librarian using Peer Review of Electronic Search Strategies (13). The search strategies are included in Supplementary Appendix B (available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22087/abstract).
The following electronic databases were searched: Ovid MEDLINE, Embase, PubMed, and Cochrane Library (Wiley). For medications included in the 2011 ACR JIA treatment recommendations, these databases were searched from October 6, 2009 (the end date of the literature search for the 2011 ACR JIA treatment recommendations) through July 25, 2012 (Table 1). For medications not included in the 2011 recommendations, the databases were searched from their beginning through July 25, 2012. In addition, each database was searched in its entirety for the treatment of MAS in systemic JIA. The same databases were searched for TB screening and JIA from October 6, 2009 through September 5, 2012.
Table 1. Medications evaluated for the treatment of systemic juvenile idiopathic arthritis*.
| 2011 recommendations |
2013 recommendations |
|
|---|---|---|
| NSAIDs† | X | X |
| Glucocorticoids | X | X |
| Methotrexate | X | X |
| Leflunomide | X | X |
| IVIG | X | X |
| Calcineurin inhibitors‡ | X | X |
| TNFα inhibitors§ | X | X |
| Abatacept | X | X |
| Rituximab | X | X |
| Anakinra | X | X |
| Canakinumab | X | |
| Rilonacept | X | |
| Tocilizumab | X |
NSAIDs = nonsteroidal antiinflammatory drugs; IVIG = intravenous immunoglobulin; TNFα = tumor necrosis factor α.
Includes all NSAIDs commonly used in clinical practice in the US, including selective cyclooxygenase 2 inhibitors.
Cyclosporine and tacrolimus.
Adalimumab, etanercept, and infliximab.
Conference abstracts were searched for preliminary reports of randomized clinical trials for which the final results were not yet published. Embase was searched for conference abstracts relating to all of the medications included in this update between January 1, 2010 and July 27, 2012. ClinicalTrials.gov was also searched to identify any additional studies with potentially relevant results that were not yet published. Two articles were in submission at the time of the first TFP votes and were included in the Evidence Report, with permission from the authors, to provide the TFP with the most current evidence (14,15). Both articles were in press by the time of the face-to-face meeting, and have subsequently been published.
An updated search was performed for all sources through January 14, 2013 in order to ensure that more recently published articles were also available for citation. An evaluation of the literature search results was performed by the PIs (SR and PFW) to determine whether any of the newly identified articles would change the recommendations, but none were deemed contradictory to the recommendations made by the TFP, and therefore it was determined that additional consideration of these articles by the TFP was not necessary.
Criteria for study inclusion/exclusion
Studies were included in the Evidence Report if they comprised children (defined as participants ages <18 years) with systemic JIA and if they specifically addressed the treatment of systemic JIA and/or the safety of medications used in this context.
Studies in languages other than English were excluded, as were non-systematic review articles, commentaries, and consensus statements. Articles that reported mechanistic aspects of therapy and did not describe the clinical characteristics of patients or their outcomes were excluded. Studies that assessed only costs were also excluded, as specified by the guideline scope and the RAND/UCLA method.
Development of the Evidence Report
The titles and abstracts of the 2,200 articles identified by the initial search were screened by a panel of volunteers consisting of a medical student, fellows, and junior faculty in pediatric rheumatology (see Acknowledgments), and articles not fulfilling the inclusion criteria were removed. If it was unclear whether an article should be included, it was kept on the list of potentially eligible articles. The full text of each potentially eligible article then underwent additional screening by a volunteer, who gave the article a final determination regarding inclusion/exclusion and extracted relevant data for the Evidence Report. If the reviewer was uncertain about the article's eligibility, the article underwent additional review by one of the PIs (SR), who also reviewed each article's final determination.
A total of 125 articles were included in the final Evidence Report. Three articles were subsequently included from the updated literature search. The data abstracted from each article for the Evidence Report included study design, participants (number and diagnosis), medication (including dose), concurrent medications, inclusion criteria, exclusion criteria, baseline disease measures, primary and secondary outcomes, adverse events, and limitations. If children with different categories of JIA were included in a study, reviewers were asked to document the results for systemic JIA patients separately, whenever possible. The abstracted data were reviewed for clarity and completeness by one of the PIs (SR), and additional data abstraction was performed when needed. Summaries of specific articles from the 2011 Evidence Report were also included in the new report, when relevant. The entire Evidence Report used for the development of the 2011 ACR JIA recommendations was also made available to the TFP members for review, upon request.
Development of the clinical scenarios
Clinical scenarios were developed by the PIs (SR and PFW) with input from the CEP based on the 3 primary phenotypes (see below). The features of poor prognosis and levels of disease activity specified in the 2011 ACR JIA recommendations were not applied to the scenarios in this update based on input from the CEP that these characteristics were of unclear relevance to decision making at the point of care for patients with systemic JIA. The consensus opinion of the CEP was that certain features of poor prognosis (i.e., joint erosions) are often not known or pertinent in new-onset cases. The choice of disease activity variables and their decision thresholds was made using an iterative process via e-mail and teleconferences with repeated revision until they were accepted by all CEP members. For each scenario, there was consensus among CEP members that the disease activity variables included provided a meaningful clinical threshold relevant for treatment decisions. The decision thresholds of active joint count (AJC; ≤4 or >4) and physician global assessment (MD global; <5 or ≥5) were chosen by CEP consensus. Disease activity descriptors were also limited to restrict the number of scenarios in order to avoid voter fatigue (12). Medication monitoring was not specifically addressed in these scenarios because it was determined that monitoring recommendations for the medications included in this project would not be expected to differ from those of the 2011 ACR JIA recommendations and/or the publicly available recommendations included in the package inserts for each of these medications. Three primary clinical phenotypes were developed. In each case, it was specified that the participants had met the International League of Associations for Rheumatology criteria for systemic JIA at disease onset (2).
For the first phenotype, systemic JIA with active systemic features and varying degrees of synovitis, active systemic features were defined as the presence of any combination of the following disease features: fever, evanescent rash, lymphadenopathy, hepatomegaly, splenomegaly, or serositis. Rather than considering specific combinations of these manifestations, the TFP was asked to consider the treatments among patients with an MD global of <5 or ≥5 on a 10-point numerical rating scale and by AJC (0 joints, 1–4 joints, or >4 joints).
For the second phenotype, systemic JIA without active systemic features but with active synovitis, TFP members were asked to rate the appropriateness of medical therapies based on the total number of active joints (≤4 joints or >4 joints).
For the third phenotype, systemic JIA with features concerning for MAS, features concerning for MAS were defined as any combination of the following disease manifestations: persistent (rather than quotidian) fever, cytopenias or falling cell line counts (particularly platelets), falling erythrocyte sedimentation rate, hypertriglyceridemia, hypofibrinogenemia, hemophagocytosis, transaminitis, coagulopathy, organomegaly, low or absent natural killer cell activity, hyperferritinemia, or central nervous system dysfunction. This definition was left intentionally broad given the lack of validated classification criteria for MAS. The scenarios specifically excluded critically ill patients requiring intensive care unit admission.
A separate scenario was developed to address repeat TB screening among all categories of JIA patients receiving biologic agents. The TFP was asked to consider the appropriateness of different screening approaches for TB, including annual screening and risk-based approaches. The TFP did not consider the method of screening (e.g., interferon-γ–release assay versus tuberculin skin test).
Medications, duration of therapy, and doses used in clinical scenarios
The medications addressed in the guideline scenarios are shown in Table 1. For each scenario, it was assumed that prior medications were given for a minimum of 3 months, with the exceptions of 1) anakinra, for which the duration was defined as ≥1 month; 2) nonsteroidal antiinflammatory drug (NSAID) monotherapy, for which the maximum duration was defined as 1 month; and 3) systemic glucocorticoid (GC) monotherapy, for which the maximum duration was defined as 2 weeks. The duration of anakinra was discussed with the CEP at large prior to the TFP voting, and 4 weeks was the timeframe agreed upon for an expected response. The duration of NSAID monotherapy and systemic GC monotherapy was voted on by the TFP.
There was no consideration of combination therapy with a biologic agent. When biologic agents were evaluated as sequential therapy, it was indicated that prior biologic agents were discontinued before initiation of a new one. For the scenarios that addressed the sequential therapy of patients with active systemic features, the TFP voting panel was instructed that these patients could be assumed to be receiving concurrent systemic GC therapy (with the exception of the scenario used to determine the duration of NSAID monotherapy, in which adjunct systemic GCs were specifically excluded) and that they should rate the appropriateness of initiating the medication under consideration either with or without concurrent initiation or increase of GC therapy (whichever approach was considered more appropriate by the voter). Receipt of concurrent GC therapy was not assumed for those scenarios that addressed the treatment of patients without active systemic features but with active synovitis. Tumor necrosis factor α (TNFα) inhibitors were considered together as a single group rather than as individual medications. Different IL-1 inhibitors were considered separately for the scenarios that addressed initiation of the medication because it was determined by the CEP that currently available data could inform this choice. For scenarios that considered IL-1 inhibitors as sequential therapy, these medications were considered as a group rather than separate medications, both to restrict the number of scenarios and because it was determined there would be sparse data to inform the use of a specific IL-1 inhibitor in this situation. For all recommendations, it was also assumed that patients received the typical maximum dose of each medication. Although higher doses of these medications may be appropriate in certain clinical situations, these situations were not specifically considered by the TFP.
In order to limit the number of clinical scenarios on which the TFP would vote, the issue of whether a nonbiologic DMARD and a biologic agent could be combined or whether they would only be used sequentially was left to the provider's discretion.
Rating of the clinical scenarios by the TFP
The TFP members were asked to rate the appropriateness of the interventions in each of the clinical scenario permutations using the Evidence Report, as well as their best clinical judgment. “Appropriateness” was defined as “the health benefits exceed the health risks by a sufficiently wide margin that the intervention is worth doing” (12). The decision to recommend or not recommend initiation of a medication for a particular scenario included the risk of not initiating an alternative therapy (e.g., the risk of initiating drug A includes the risk of not initiating drug B). Each scenario was scored on a numerical rating scale from 1–9, where 1–3 = “inappropriate,” 4–6 = “uncertain,” and 7–9 = “appropriate.” An uncertain score indicated that either the risks or benefits were approximately equal or there was not enough information available for the TFP to make a meaningful evaluation.
Developing recommendations from the TFP votes
The second round of votes from the face-to-face meeting was used to create the final recommendations. Therapies are listed as “recommended” if they met the RAND/UCLA appropriateness definition that includes a median score of 7–9 and no disagreement. Therapies listed as “inappropriate” had a median in the range of 1–3 and no disagreement. Disagreement was defined as at least 3 panelists rating the indication between 1 and 3 and at least 3 panelists rating the indication between 7 and 9. “Uncertain” indications had a median in the range of 4–6 or disagreement regardless of the median score.
Rating of the evidence supporting the final ACR recommendations
Following the development of recommendations, a level of evidence was assigned to each recommendation using the system proposed by the Oxford Centre for Evidence-Based Medicine (16). This is the same rating system used for the 2011 ACR JIA treatment recommendations. Briefly, this rating system creates the following 4 categories for rating evidence: A = randomized controlled trials; B = nonrandomized studies, including retrospective cohort studies; C = uncontrolled studies, including case series; and D = expert opinion. Level B was also assigned to any recommendation for which there was extrapolation from randomized controlled trials. Level C was also assigned to any recommendation for which there was extrapolation from a nonrandomized study or more complex extrapolation from a randomized controlled trial. The level of evidence assigned reflects the highest rating achieved for each recommendation (i.e., if studies in support of a recommendation have a level of evidence ranging from B-D, the overall level of evidence is reported as B). In order to provide the most comprehensive reference list, all relevant articles from the Evidence Report are cited, even if they did not provide the highest level of evidence.
Results
The recommendations for initiation of various therapeutic agents are listed separately for the following clinical phenotypes of systemic JIA: 1) active systemic features and varying degrees of synovitis, 2) no active systemic features and varying degrees of active synovitis, and 3) features concerning for MAS. Recommended initial therapeutic options are listed first, in alphabetical order. Therapeutic options for continued disease activity after initial therapy are listed next, in alphabetical order. Medications that were considered by the TFP but were determined to be inappropriate or uncertain (and were not recommended for any of the related scenarios) are listed at the end of each section, in alphabetical order. The assigned level of evidence and corresponding publication citations follow each treatment recommendation. If a recommendation is noted to be irrespective of the AJC or MD global, the recommendation was for children with an AJC ≥0 or an MD global >0, respectively. Continued disease activity, as used in the recommendations below, was defined as an AJC >0 and/or an MD global >0. In some cases, children may qualify for more than one pathway, in which case it is left to the provider's discretion to choose the path they feel is most appropriate based upon specific patient characteristics and/or patient and family preferences.
Systemic JIA with active systemic features and varying degrees of synovitis
The treatment recommendations for this group of patients are shown in Figure 1. The TFP was asked to consider the treatments among patients with an MD global of <5 or ≥5 on a 10-point numerical rating scale and by AJC (0 joints, 1–4 joints, or >4 joints). The TFP voting panel was informed that these patients could be assumed to be receiving concurrent systemic GC therapy and that they should rate the appropriateness of initiating the medication under consideration either with or without concurrent initiation or increase of GC therapy (whichever approach was considered more appropriate by the voter). The recommendations in this section are for patients with active systemic features. If the systemic features (but not the arthritis) respond to therapy, then subsequent treatment decisions should be based upon recommendations in the next section, “Systemic JIA without active systemic features and with varying degrees of active synovitis.”
Figure 1.
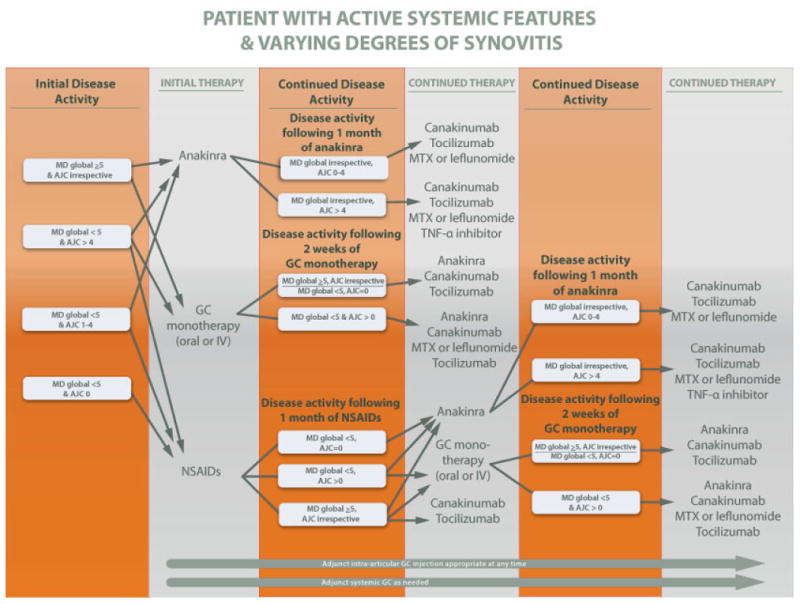
Treatment pathways for patients with active systemic features and varying degrees of synovitis. The Task Force Panel was asked to consider the treatments among patients with active systemic features and a physician global assessment (MD global) of <5 or ≥5 on a 10-point numerical rating scale (0–10 visual analog scale, where 0 = no disease activity and 10 = the most severe) and by active joint count (AJC; 0 joints, 1–4 joints, or >4 joints). If a recommendation is noted to be irrespective of the AJC or MD global, the recommendation was for children with an AJC ≥0 or an MD global >0, respectively. Adjunct systemic glucocorticoids (GCs) and/or intraarticular GCs may be added at any point. Children may qualify for >1 pathway, in which case it is left to the provider's discretion to choose the path they feel is most appropriate based upon specific patient characteristics and/or patient and family preferences. Steps in the progression of therapy can be additive or sequential, except that therapies with a biologic agent are sequential (combination therapy with a biologic agent is not endorsed). The recommendations in this figure are for patients with active systemic features. If the systemic features (but not the arthritis) respond to therapy, then subsequent treatment decisions should be based upon the recommendations in Figure 2. NSAIDs = nonsteroidal antiinflammatory drugs; IV = intravenous; MTX = methotrexate; TNF-α = tumor necrosis factor α.
Initial therapeutic options (listed alphabetically)
Anakinra was recommended as one initial therapeutic option for patients with an MD global ≥5 irrespective of the AJC, or an MD global <5 and an AJC >0 (level C) (17–19).
Systemic GC monotherapy (administered by oral or intravenous route) was recommended for a maximum period of 2 weeks as a therapeutic option for patients with an MD global <5 and an AJC >4 and for all patients with an MD global ≥5 irrespective of the AJC (level C) (20,21). Continuing GCs as monotherapy for ≥1 month for patients with continued disease activity was inappropriate (level D). The minimum duration of GC monotherapy and specific tapering regimens for GCs were not specifically addressed by the TFP.
Initiating NSAID monotherapy in a patient without prior treatment was recommended as one approach for patients with an MD global <5 irrespective of the AJC (level D). NSAID monotherapy was inappropriate for patients with an MD global ≥5 and an AJC >0 (level D). Continuing NSAID monotherapy for longer than 1 month for patients with continued disease activity was inappropriate (level D). The minimum duration of a trial of NSAIDs was not specifically addressed by the TFP.
Therapeutic options for continued disease activity (listed alphabetically)
Use of abatacept was recommended only for patients with an MD global ≥5 and an AJC >4 after a trial of both an IL-1 inhibitor and tocilizumab (sequentially) (level D). Use of abatacept for patients with an AJC of 0 irrespective of the MD global was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially), in which case it was uncertain. Use of abatacept for patients with an MD global <5 and an AJC >0 or an MD global ≥5 and an AJC <4 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or a DMARD plus either an IL-1 inhibitor or tocilizumab, in which case it was uncertain. Use of abatacept for patients with an MD global ≥5 and an AJC >4 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially), in which case it was appropriate (level D), or patients who had tried a DMARD plus either an IL-1 inhibitor or tocilizumab, in which case it was uncertain.
Anakinra was recommended for patients with continued disease activity after treatment with GC monotherapy (level A) (17,18,22–30) or NSAID monotherapy (level C) (17,18,22,28).
Use of a calcineurin inhibitor was recommended only for patients with an MD global ≥5 and an AJC of 0 after a trial of both an IL-1 inhibitor and tocilizumab (sequentially) (level C) (31–36). Use of a calcineurin inhibitor for patients with an MD global <5 and an AJC of 0 was inappropriate (level D), with the exception of patients who received either an IL-1 inhibitor or tocilizumab, in which case it was uncertain. Use of a calcineurin inhibitor for patients with an MD global ≥5 and an AJC of 0 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially), in which case it was appropriate (level C) (31–36), or patients who had tried an IL-1 inhibitor or tocilizumab, in which case it was uncertain. Use of a calcineurin inhibitor for patients with an AJC >0 irrespective of the MD global was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or an alternate DMARD plus either an IL-1 inhibitor or tocilizumab, in which case it was uncertain.
Canakinumab was recommended for patients with continued disease activity after treatment with GC monotherapy (level A) (14,37), methotrexate (MTX) or leflunomide (level A) (14,37), anakinra (level B) (14,37), or tocilizumab (level C) (14,37) irrespective of the MD global and AJC. Canakinumab was also recommended for patients with an MD global ≥5 irrespective of the AJC, despite prior NSAID monotherapy (level C) (14,37).
GC monotherapy was recommended as an option following failed treatment with NSAID monotherapy for patients with an MD global <5 and an AJC >0 and for patients with an MD global ≥5 irrespective of the AJC (level C) (20,21). Adjunct GC therapy at any point was appropriate to consider (level D).
Intraarticular GC injection was recommended as adjunct therapy at any time (level C) (38,39).
MTX or leflunomide was recommended for patients with an MD global <5 and an AJC >0 after treatment with GC monotherapy (level C) (40), an IL-1 inhibitor (level D), or tocilizumab (level D). MTX or leflunomide was recommended for patients with an MD global ≥5 and an AJC >0, only after a trial of an IL-1 inhibitor or tocilizumab (level C) (40). Initiation of MTX or leflunomide was inappropriate for patients with an AJC of 0 irrespective of the MD global (level D).
Initiation of a TNFα inhibitor was recommended for patients with an AJC >4 irrespective of the MD global after a trial of an IL-1 inhibitor or tocilizumab (level C) (41,42). Initiation of a TNFα inhibitor was recommended for patients with an AJC >0 irrespective of the MD global after a trial of both an IL-1 inhibitor and tocilizumab (sequentially) (level C) (41,42). Use of a TNFα inhibitor for patients with an MD global <5 and an AJC of 0 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or a DMARD plus either an IL-1 inhibitor or tocilizumab, in which case it was uncertain. Use of a TNFα inhibitor for patients with an MD global ≥5 and an AJC of 0 was inappropriate (level D), with the exception of patients who had tried an IL-1 inhibitor or tocilizumab, in which case it was uncertain.
Tocilizumab was recommended as a therapeutic option for patients with continued disease activity following GC monotherapy (level A) (15,43–49), MTX or leflunomide (level B) (15,43–49), or anakinra (level B) (15) irrespective of the MD global and AJC. Tocilizumab was also recommended for patients with an MD global ≥5 irrespective of the AJC despite prior NSAID monotherapy (level C) (15,43–49).
Uncertain or inappropriate options for continued disease activity (listed alphabetically)
Use of IVIG was inappropriate irrespective of the AJC and MD global (level D).
Use of nonbiologic DMARD combination therapy (MTX plus leflunomide and/or a calcineurin inhibitor) was uncertain irrespective of the AJC and MD global.
Use of rilonacept was inappropriate as initial therapy irrespective of the MD global and AJC (level D). Use of rilonacept was uncertain for continued disease activity after a trial of other therapeutic options irrespective of the AJC and MD global.
Use of rituximab was inappropriate for patients with an AJC of 0 irrespective of the MD global. Use of rituximab for patients with an MD global <5 and an AJC <4 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially), in which case it was uncertain. Use of rituximab for patients with an MD global <5 and an AJC >4 or an MD global ≥5 and an AJC >0 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or a DMARD plus either an IL-1 inhibitor or tocilizumab, in which case it was uncertain.
Systemic JIA without active systemic features and with varying degrees of active synovitis
The treatment recommendations for this group of patients are shown in Figure 2. The TFP was asked to rate the appropriateness of therapies based on the total number of active joints (≤4 joints or >4 joints). Each of the recommendations below is irrespective of the MD global.
Figure 2.
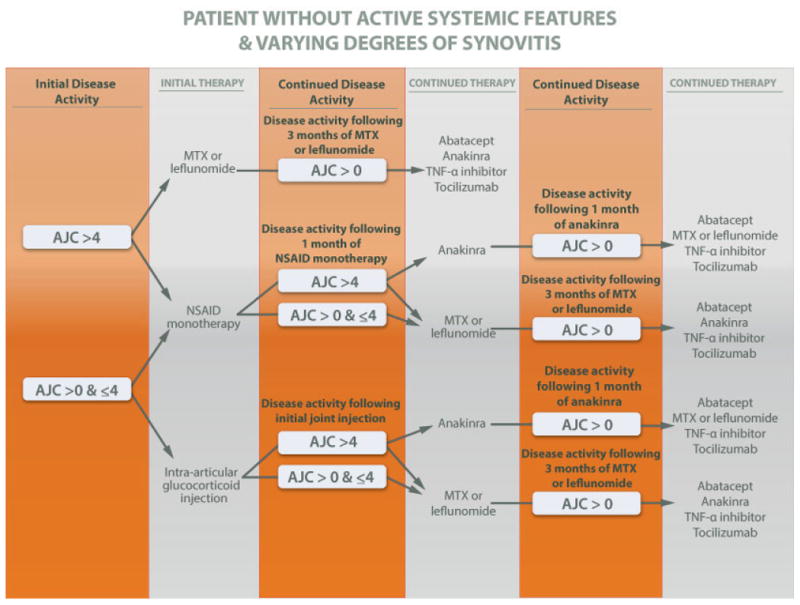
Treatment pathways for patients without active systemic features and with varying degrees of synovitis. The Task Force Panel was asked to rate the appropriateness of therapies based on the total number of active joints (≤4 or >4). Children may qualify for >1 pathway, in which case it is left to the provider's discretion to choose the path they feel is most appropriate based upon specific patient characteristics and/or patient and family preferences. Steps in the progression of therapy can be additive or sequential, except that therapies with a biologic agent are sequential (combination therapy with a biologic agent is not endorsed). AJC = active joint count; MTX = methotrexate; NSAID = nonsteroidal antiinflammatory drug; IV = intravenous; TNF-α = tumor necrosis factor α.
Initial therapeutic options (listed alphabetically)
Intraarticular GC injection was recommended as an initial treatment option for patients with an AJC ≤4 (level C) (38,39). Intraarticular GC injection as the only therapeutic intervention was uncertain for patients with an AJC >4. The utility of repeating intraarticular injection as the only intervention was uncertain in a joint or joints currently affected.
Initiation of MTX or leflunomide was recommended for patients with an AJC >4 (level C) (40,50–53).
Initiation of NSAID monotherapy in a patient without prior treatment for a maximum period of 1 month was recommended as one treatment approach for patients with an AJC >0 (level D). Continuing NSAID monotherapy for longer than 2 months for patients with continued disease activity was inappropriate (level D). The minimum duration of a trial of NSAIDs was not specifically addressed by the TFP.
Therapeutic options for continued disease activity (listed alphabetically)
Use of abatacept was recommended for patients with an AJC >0 after treatment with MTX or leflunomide (level B) (54–57), anakinra (level D), or tocilizumab (level D).
Anakinra was recommended as a therapeutic option for patients with an AJC >4 following failed intraarticular injection or NSAID monotherapy (level B) (29,58). Use of anakinra was also recommended for patients with an AJC >0 following treatment with MTX or leflunomide (level B) (22,29,30,58).
Initiation of canakinumab was recommended for patients with an AJC >4 only after a trial of a DMARD plus anakinra or tocilizumab (level B) (14,37), a DMARD plus a TNFα inhibitor (level B) (14,37), or abatacept (level C) (14,37).
Use of MTX or leflunomide was recommended as an option for an AJC >0 following treatment with intraarticular injection (level C) (51,52), NSAID monotherapy (level C) (51,52), an IL-1 inhibitor (level D), or tocilizumab (level D).
Initiation of a TNFα inhibitor was recommended for patients with an AJC >0 after treatment with MTX or leflunomide (level C) (59–61), anakinra (level D), or tocilizumab (level D).
Initiation of tocilizumab was recommended for an AJC >0 following treatment with anakinra (level B) (15) or MTX or leflunomide (level B) (15).
Uncertain or inappropriate options for continued disease activity (listed alphabetically)
Initiation of nonbio-logic DMARD combinations (MTX plus leflunomide and/or a calcineurin inhibitor) was uncertain irrespective of the AJC.
Initiation of rilonacept was uncertain irrespective of the AJC.
Use of rituximab for patients with an AJC ≤4 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or a DMARD in combination with an IL-1 inhibitor or tocilizumab, in which case it was uncertain. Use of rituximab for patients with an AJC >4 was inappropriate (level D), with the exception of patients who had tried both an IL-1 inhibitor and tocilizumab (sequentially) or a DMARD in combination with an IL-1 inhibitor, tocilizumab, a TNFα inhibitor, or abatacept, in which case it was uncertain.
Systemic JIA with features concerning for MAS
The recommendations for treatment of patients with systemic JIA and features concerning for MAS are described below. These treatment options are not meant to be mutually exclusive and there may be certain clinical situations for which the simultaneous initiation of more than one of these medications is appropriate. Combination therapy with anakinra, a calcineurin inhibitor, and systemic GCs was not specifically addressed.
Initial therapeutic options (listed alphabetically)
Use of anakinra was recommended as one therapeutic option for patients with features concerning for MAS (level C) (18,19,28,62–64).
Use of a calcineurin inhibitor was recommended as one therapeutic option for patients with features concerning for MAS (level C) (65–69).
Use of systemic GC monotherapy (administered by oral or intravenous route) was also recommended as a therapeutic option for patients with features concerning for MAS (level C) (70,71). Continuing GC monotherapy for ≥2 weeks in patients with continued features concerning for MAS was inappropriate (level D). Specific tapering strategies for GCs were not specifically addressed by the TFP.
Uncertain or inappropriate options for continued disease (listed alphabetically)
Initiation of abatacept was inappropriate (level D).
Use of canakinumab was uncertain, with the exception of patients with an MD global <5 who had received no prior therapy, GC monotherapy, or calcineurin monotherapy, in which case it was inappropriate (level D).
Use of IVIG was inappropriate (level D), with the exception of patients who had tried a calcineurin inhibitor in combination with anakinra, in which case it was uncertain.
Use of MTX or leflunomide was inappropriate (level D).
Use of rilonacept was uncertain.
Use of rituximab was inappropriate (level D).
Use of a TNFα inhibitor was inappropriate irrespective of the MD global (level D), with the exception of patients who had tried a calcineurin inhibitor in combination with anakinra, in which case it was uncertain.
Use of tocilizumab was uncertain.
Repeat testing for latent TB for children with all categories of JIA
Annual screening of children at low risk of TB with an initial negative TB test was inappropriate (level D). It was recommended that patients with an initial negative TB test prior to starting a biologic agent have TB screening repeated at any point if their risk of TB changed to moderate or high, as determined by regional infectious disease guidelines (level D).
Discussion
These recommendations for the treatment of systemic JIA and secondary TB screening are the culmination of a systematic review and formal evaluation of 1,226 scenarios using the RAND/UCLA methodology by an international panel of experts in the field of JIA and pediatric rheumatology, with input from an expert in evidence-based medicine and from the parent of a child with systemic JIA. This current work represents an update of the 2011 ACR JIA treatment recommendations that included recommendations for systemic JIA with systemic features, but due to limitations of data at the time, did not provide recommendations for specific phenotypes of systemic JIA. Since the publication of these initial recommendations, data from randomized trials of new IL-1 inhibitors and IL-6 inhibitors in children with systemic JIA have been published, supporting the need for updated recommendations including these medications (14,15).
These recommendations should be interpreted in the context of several limitations. First, systemic JIA is a complex disease with heterogeneous manifestations. The phenotypes and scenarios used in the development of these recommendations do not represent all possible patient presentations. The specific influence of disease features such as hip arthritis, rash, and fever was not evaluated; the assumption of the CEP was that fever and other relevant systemic features would be reflected in the MD global. The lack of a standardized disease activity score also limited the development of clinical scenarios, and the categorization of disease severity by the AJC and MD global may also limit the scenarios' representation of the variety of possible patient presentations. The decision thresholds of AJC (≤4 or >4) and MD global (<5 and ≥5) were chosen by CEP consensus. Their validity may be scrutinized in the future by examining their relationship with therapeutic decisions in standard clinical practice and with criteria for enrolling patients in randomized clinical trials.
Several recommendations were assigned level of evidence A because there was at least one well-designed randomized clinical trial to help inform the recommendation. For example, the level A evidence available to support the use of anakinra after treatment with GC monotherapy for children with active systemic features is the ANAJIS trial, which is a randomized trial, but it is a single trial that enrolled only 24 patients, making it necessary to interpret efficacy and safety data with some caution. The conclusions of ANAJIS are borne out from multiple case series that reached the same conclusion. Furthermore, because many of these recommendations are derived from expert opinion (level of evidence D) rather than higher levels of evidence, these recommendations may require revision as new data are generated regarding treatment efficacy, effectiveness, and safety, and as understanding of the underlying disease pathogenesis expands.
Specifying GC dosing, route of administration, and tapering guidelines is an important endeavor, but was beyond the scope of this project and not amenable to the RAND/UCLA methodology. However, a recent study used consensus methodology to develop an algorithm for standardized GC management in systemic JIA (72). Optimal combinations of DMARD therapies with or without therapies with a biologic agent for the scenarios above are not well understood, and it is anticipated that new data may help to clarify these treatment choices as well. Lastly, although the treatment pathways generated by these recommendations have been simplified as much as possible to facilitate their use in the clinical setting, they remain relatively complex. This complexity reflects the level of discussion and decision making by the TFP and it is anticipated that in the future, with more data available, these pathways may be simplified.
Development of treatment recommendations for children with systemic JIA and features of MAS is particularly challenging. First, there are no diagnostic criteria for MAS complicating systemic JIA, although preliminary criteria were proposed in 2005 and there is an international effort underway to develop these criteria based on expert opinion and analysis of existing patient data (73,74). Second, the etiology of MAS complicating systemic JIA is likely heterogeneous. As such, a specified stepwise treatment algorithm will not work for all patients with this disease. As more is learned about the various etiologies and pathophysiology of MAS in this population of patients, we will hopefully be able to use more targeted and efficacious therapies. The recommendation to use anakinra, calcineu-rin inhibitors, and GCs is certainly an important first step. However, it is anticipated that in the near future, with more data regarding treatments and a better understanding of the disease process, these recommendations may be modified.
It should be noted that these recommendations do not address the initial screening for TB prior to prescribing immunosuppressive medication, the necessity of which has been clearly established elsewhere (75). These guidelines also do not assess the method of screening, since this is addressed by the American Academy of Pediatrics (AAP) Red Book and by the Centers for Disease Control and Prevention (75,76). Currently, interferon-γ–release testing is not indicated for children ages <5 years. The AAP Red Book does not recommend repeat routine testing for children who remain at low risk while receiving immunosuppressive medication, consistent with the conclusion of the TFP for this project. If the patient history or local epidemiologic factors suggest a possible exposure, immediate and periodic skin testing or interferon-y–release testing is recommended by the AAP.
These recommendations are distinct from the recently published Childhood Arthritis and Rheumatology Research Alliance (CARRA) systemic JIA consensus treatment plans (CTPs) (77). The CARRA treatment plans reflect the existing diverse treatment practices across North America, are based on nominal group consensus techniques, and were developed for the purpose of conducting observational comparative effectiveness research. In contrast to these guidelines, the CTPs do not address specific disease phenotypes, and are more restricted in the medications assessed. It is anticipated that data from comparative effectiveness research based upon the CARRA CTPs will likely be very informative in future guidelines projects.
These recommendations, representing the culmination of a rigorous systematic literature review and the use of the RAND/UCLA appropriateness methodology, are an important contribution to the care of children with systemic JIA, offering recommendations to providers caring for children with this challenging disease.
Supplementary Material
Acknowledgments
The authors would like to thank Janet Joyce, Amy Miller, and Regina Parker of the ACR for their guidance and administrative support. We would also like to thank the following people for their assistance with screening and abstraction of articles for the development of the Evidence Report: Drs. Abdul Al-Rasheed, Alex Aminoff, Danielle Bennett, Colleen Correll, Lauren Henderson, Patricia Hobday, Ginger Janow, Jennifer Ji Young Lee, Pai-Yue Lu, Melissa Mannion, Theresa Muskardin, Dax Rumsey, Yonit Sterba, Alysha Taxter, and Patricia Vega-Fernandez.
Dr. Ringold's work was supported by the Agency for Healthcare Research and Quality for the duration of this project (grant K12HS019482). Dr. Weiss's work was supported by the National Institute of Arthritis and Musculo-skeletal and Skin Diseases, NIH (grant 1-K23-AR059749-01A1).
Dr. Beukelman has received consulting fees (less than $10,000 each) from Genentech and McKesson Health Solutions and (more than $10,000) from Novartis. Dr. Ilowite has received consulting fees, speaking fees, and/or honoraria (less than $10,000 each) from Janssen and Novartis. Dr. Kimura has received consulting fees, speaking fees, and/or honoraria (less than $10,000) from Novartis. Dr. Laxer has received consulting fees, speaking fees, and/or honoraria (less than $10,000) from Novartis and receives royalties from Textbook of Pediatric Rheumatology. Dr. Lovell has received consulting fees, speaking fees, and/or honoraria (less than $10,000 each) from Novartis and Hoffman-La Roche. Dr. Nigrovic has received consulting fees (less than $10,000) from Novartis.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Drs. Ringold and Weiss contributed equally to this work.
Members of the Core Expert Panel: Timothy Beukelman, Esi Morgan DeWitt, Norman T. Ilowite, Yukiko Kimura, Ronald M. Laxer, Daniel J. Lovell, Peter A. Nigrovic, Sarah Ringold, Angela Byun Robinson, Richard K. Vehe, and Pamela F. Weiss.
Members of the Task Force Panel: Mara Becker, Robert A. Colbert, Vincent Delgaizo, Pavla Dolezalova, Polly Ferguson, Chris Feudtner, Sheila Angeles-Han, Alberto Martini, Murray Passo, Sampath Prahalad, Marilynn Punaro, Rayfel Schneider, David D. Sherry, and Carol A. Wallace.
Author Contributions: All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Drs. Ringold and Weiss had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Ringold, Weiss, Beukelman, DeWitt, Ilowite, Kimura, Laxer, Lovell, Nigrovic, Robinson, Vehe.
Acquisition of data. Ringold, Weiss, Beukelman, Laxer, Lovell, Nigrovic.
Analysis and interpretation of data. Ringold, Weiss, Ilowite, Kimura, Laxer, Nigrovic.
This article is published simultaneously in the October 2013 issue of Arthritis & Rheumatism.
References
- 1.Beukelman T, Patkar NM, Saag KG, Tolleson-Rinehart S, Cron RQ, DeWitt EM, et al. 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care Res (Hoboken) 2011;63:465–82. doi: 10.1002/acr.20460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2. [PubMed] [Google Scholar]
- 3.Singh-Grewal D, Schneider R, Bayer N, Feldman BM. Predictors of disease course and remission in systemic juvenile idiopathic arthritis: significance of early clinical and laboratory features. Arthritis Rheum. 2006;54:1595–601. doi: 10.1002/art.21774. [DOI] [PubMed] [Google Scholar]
- 4.Lomater C, Gerloni V, Gattinara M, Mazzotti J, Cimaz R, Fantini F. Systemic onset juvenile idiopathic arthritis: a retrospective study of 80 consecutive patients followed for 10 years. J Rheumatol. 2000;27:491–6. [PubMed] [Google Scholar]
- 5.Spiegel LR, Schneider R, Lang BA, Birdi N, Silverman ED, Laxer RM, et al. Early predictors of poor functional outcome in systemic-onset juvenile rheumatoid arthritis: a multicenter cohort study. Arthritis Rheum. 2000;43:2402–9. doi: 10.1002/1529-0131(200011)43:11<2402::AID-ANR5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 6.Mellins ED, Macaubas C, Grom AA. Pathogenesis of systemic juvenile idiopathic arthritis: some answers, more questions. Nat Rev Rheumatol. 2011;7:416–26. doi: 10.1038/nrrheum.2011.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martini A. Systemic juvenile idiopathic arthritis. Autoimmun Rev. 2012;12:56–9. doi: 10.1016/j.autrev.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 8.Behrens EM, Beukelman T, Paessler M, Cron RQ. Occult mac-rophage activation syndrome in patients with systemic juvenile idiopathic arthritis. J Rheumatol. 2007;34:1133–8. [PubMed] [Google Scholar]
- 9.Behrens EM, Beukelman T, Gallo L, Spangler J, Rosenkranz M, Arkachaisri T, et al. Evaluation of the presentation of systemic onset juvenile rheumatoid arthritis: data from the Pennsylvania Systemic Onset Juvenile Arthritis Registry (PASOJAR) J Rheumatol. 2008;35:343–8. [PubMed] [Google Scholar]
- 10.Bennett TD, Fluchel M, Hersh AO, Hayward KN, Hersh AL, Brogan TV, et al. Macrophage activation syndrome in children with systemic lupus erythematosus and children with juvenile idiopathic arthritis. Arthritis Rheum. 2012;64:4135–42. doi: 10.1002/art.34661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawhney S, Woo P, Murray KJ. Macrophage activation syndrome: a potentially fatal complication of rheumatic disorders. Arch Dis Child. 2001;85:421–6. doi: 10.1136/adc.85.5.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitch K, Bernstein S, Aguilar M, Burnand B, LaCalle J. The RAND/UCLA appropriateness method user's manual. Santa Monica (CA): RAND; 2001. [Google Scholar]
- 13.Sampson M, McGowan J, Lefebvre C, Moher DG. PRESS: peer review of electronic search strategies. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2008. [Google Scholar]
- 14.Ruperto N, Brunner HI, Quartier P, Constantin T, Wulffraat N, Horneff G, et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2396–406. doi: 10.1056/NEJMoa1205099. [DOI] [PubMed] [Google Scholar]
- 15.De Benedetti F, Brunner HI, Ruperto N, Kenwright A, Wright S, Calvo I, et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2385–95. doi: 10.1056/NEJMoa1112802. [DOI] [PubMed] [Google Scholar]
- 16.CEBM, Centre for Evidence-Based Medicine. Oxford Centre for Evidence-Based Medicine: levels of evidence (March 2009) Oxford (UK): Oxford Centre for Evidence-Based Medicine; 2009. URL: http://www.cebm.net/index.aspx?o=1025. [Google Scholar]
- 17.Quartier P, Allantaz F, Cimaz R, Pillet P, Messiaen C, Bardin C, et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial) Ann Rheum Dis. 2011;70:747–54. doi: 10.1136/ard.2010.134254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nigrovic PA, Mannion M, Prince FH, Zeft A, Rabinovich CE, van Rossum MA, et al. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum. 2011;63:545–55. doi: 10.1002/art.30128. [DOI] [PubMed] [Google Scholar]
- 19.Hedrich CM, Bruck N, Fiebig B, Gahr M. Anakinra: a safe and effective first-line treatment in systemic onset juvenile idiopathic arthritis (SoJIA) Rheumatol Int. 2012;32:3525–30. doi: 10.1007/s00296-011-2249-4. [DOI] [PubMed] [Google Scholar]
- 20.Pay S, Turkcapar N, Kalyoncu M, Simsek I, Beyan E, Ertenli I, et al. A multicenter study of patients with adult-onset Still's disease compared with systemic juvenile idiopathic arthritis. Clin Rheumatol. 2006;25:639–44. doi: 10.1007/s10067-005-0138-5. [DOI] [PubMed] [Google Scholar]
- 21.Picco P, Gattorno M, Buoncompagni A, Pistoia V, Borrone C. 6-methylprednisolone ‘mini-pulses’: a new modality of glucocorticoid treatment in systemic onset juvenile chronic arthritis. Scand J Rheumatol. 1996;25:24–7. doi: 10.3109/03009749609082663. [DOI] [PubMed] [Google Scholar]
- 22.Swart JF, Barug D, Mohlmann M, Wulffraat NM. The efficacy and safety of interleukin-1-receptor antagonist anakinra in the treatment of systemic juvenile idiopathic arthritis. Expert Opin Biol Ther. 2010;10:1743–52. doi: 10.1517/14712598.2010.532785. [DOI] [PubMed] [Google Scholar]
- 23.Zeft A, Hollister R, LaFleur B, Sampath P, Soep J, McNally B, et al. Anakinra for systemic juvenile arthritis: the Rocky Mountain experience. J Clin Rheumatol. 2009;15:161–4. doi: 10.1097/RHU.0b013e3181a4f459. [DOI] [PubMed] [Google Scholar]
- 24.Ohlsson V, Baildam E, Foster H, Jandial S, Pain C, Strike H, et al. Anakinra treatment for systemic onset juvenile idiopathic arthritis (SOJIA) [letter] Rheumatology (Oxford) 2008;47:555–6. doi: 10.1093/rheumatology/ken030. [DOI] [PubMed] [Google Scholar]
- 25.Pascual V, Allantaz F, Arce E, Punaro M, Banchereau J. Role of interleukin-1 (IL-1) in the pathogenesis of systemic onset juvenile idiopathic arthritis and clinical response to IL-1 blockade. J Exp Med. 2005;201:1479–86. doi: 10.1084/jem.20050473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merlin E, Berthomieu L, Dauphin C, Stephan JL. Cardiac tamponade in a child with systemic-onset juvenile idiopathic arthritis: dramatic improvement after interleukin-1 blockade by anakinra [letter] Pediatr Cardiol. 2011;32:862–3. doi: 10.1007/s00246-011-0009-6. [DOI] [PubMed] [Google Scholar]
- 27.Mirkinson LJ, Nagle D, Kadom N, Jones OY. Anakinra therapy in a child with systemic-onset juvenile rheumatoid arthritis after human herpesvirus 6 encephalitis. J Clin Rheumatol. 2006;12:83–6. doi: 10.1097/01.rhu.0000208650.99508.4e. [DOI] [PubMed] [Google Scholar]
- 28.Verbsky JW, White AJ. Effective use of the recombinant interleukin 1 receptor antagonist anakinra in therapy resistant systemic onset juvenile rheumatoid arthritis. J Rheumatol. 2004;31:2071–5. [PubMed] [Google Scholar]
- 29.Gattorno M, Piccini A, Lasiglie D, Tassi S, Brisca G, Carta S, et al. The pattern of response to anti–interleukin-1 treatment distinguishes two subsets of patients with systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 2008;58:1505–15. doi: 10.1002/art.23437. [DOI] [PubMed] [Google Scholar]
- 30.Lequerre T, Quartier P, Rosellini D, Alaoui F, De Bandt M, Mejjad O, et al. Interleukin-1 receptor antagonist (anakinra) treatment in patients with systemic-onset juvenile idiopathic arthritis or adult onset Still disease: preliminary experience in France. Ann Rheum Dis. 2008;67:302–8. doi: 10.1136/ard.2007.076034. [DOI] [PubMed] [Google Scholar]
- 31.Ruperto N, Ravelli A, Castell E, Gerloni V, Haefner R, Malattia C, et al. Cyclosporine A in juvenile idiopathic arthritis: results of the PRCSG/PRINTO phase IV post marketing surveillance study. Clin Exp Rheumatol. 2006;24:599–605. [PubMed] [Google Scholar]
- 32.Ravelli A, Moretti C, Temporini F, Rossi F, Magni-Manzoni S, Pistorio A, et al. Combination therapy with methotrexate and cyclosporine A in juvenile idiopathic arthritis. Clin Exp Rheumatol. 2002;20:569–72. [PubMed] [Google Scholar]
- 33.Gerloni V, Cimaz R, Gattinara M, Arnoldi C, Pontikaki I, Fantini F. Efficacy and safety profile of cyclosporin A in the treatment of juvenile chronic (idiopathic) arthritis: results of a 10-year prospective study. Rheumatology (Oxford) 2001;40:907–13. doi: 10.1093/rheumatology/40.8.907. [DOI] [PubMed] [Google Scholar]
- 34.Reiff A, Rawlings DJ, Shaham B, Franke E, Richardson L, Szer IS, et al. Preliminary evidence for cyclosporin A as an alternative in the treatment of recalcitrant juvenile rheumatoid arthritis and juvenile dermatomyositis. J Rheumatol. 1997;24:2436–43. [PubMed] [Google Scholar]
- 35.Pistoia V, Buoncompagni A, Scribanis R, Fasce L, Alpigiani G, Cordone G, et al. Cyclosporin A in the treatment of juvenile chronic arthritis and childhood polymyositis-dermatomyositis: results of a preliminary study. Clin Exp Rheumatol. 1993;11:203–8. [PubMed] [Google Scholar]
- 36.Ostensen M, Hoyeraal HM, Kass E. Tolerance of cyclosporine A in children with refractory juvenile rheumatoid arthritis. J Rheumatol. 1988;15:1536–8. [PubMed] [Google Scholar]
- 37.Ruperto N, Quartier P, Wulffraat N, Woo P, Ravelli A, Mouy R, et al. for the Paediatric Rheumatology International Clinical Trials Organisation A phase II, multicenter, open-label study evaluating dosing and preliminary safety and efficacy of canakinumab in systemic juvenile idiopathic arthritis with active systemic features. Arthritis Rheum. 2012;64:557–67. doi: 10.1002/art.33342. [DOI] [PubMed] [Google Scholar]
- 38.Bloom BJ, Alario AJ, Miller LC. Intra-articular corticosteroid therapy for juvenile idiopathic arthritis: report of an experiential cohort and literature review. Rheumatol Int. 2011;31:749–56. doi: 10.1007/s00296-010-1365-x. [DOI] [PubMed] [Google Scholar]
- 39.Lanni S, Bertamino M, Consolaro A, Pistorio A, Magni-Manzoni S, Galasso R, et al. Outcome and predicting factors of single and multiple intra-articular corticosteroid injections in children with juvenile idiopathic arthritis. Rheumatology (Oxford) 2011;50:1627–34. doi: 10.1093/rheumatology/ker165. [DOI] [PubMed] [Google Scholar]
- 40.Woo P, Southwood TR, Prieur AM, Dore CJ, Grainger J, David J, et al. Randomized, placebo-controlled, crossover trial of low-dose oral methotrexate in children with extended oligoarticular or systemic arthritis. Arthritis Rheum. 2000;43:1849–57. doi: 10.1002/1529-0131(200008)43:8<1849::AID-ANR22>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 41.Russo RA, Katsicas MM. Clinical remission in patients with systemic juvenile idiopathic arthritis treated with anti-tumor necrosis factor agents. J Rheumatol. 2009;36:1078–82. doi: 10.3899/jrheum.090952. [DOI] [PubMed] [Google Scholar]
- 42.Kimura Y, Pinho P, Walco G, Higgins G, Hummell D, Szer I, et al. Etanercept treatment in patients with refractory systemic onset juvenile rheumatoid arthritis. J Rheumatol. 2005;32:935–42. [PubMed] [Google Scholar]
- 43.Inaba Y, Ozawa R, Aoki C, Imagawa T, Mori M, Hara R, et al. Radiologic analysis of the effect of tocilizumab on hands and large joints in children with systemic juvenile idiopathic arthritis. Mod Rheumatol. 2012 doi: 10.1007/s10165-012-0711-0. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 44.Yokota S, Miyamae T, Imagawa T, Iwata N, Katakura S, Mori M, et al. Therapeutic efficacy of humanized recombinant anti– interleukin-6 receptor antibody in children with systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 2005;52:818–25. doi: 10.1002/art.20944. [DOI] [PubMed] [Google Scholar]
- 45.Woo P, Wilkinson N, Prieur AM, Southwood T, Leone V, Livermore P, et al. Open label phase II trial of single, ascending doses of MRA in Caucasian children with severe systemic juvenile idiopathic arthritis: proof of principle of the efficacy of IL-6 receptor blockade in this type of arthritis and demonstration of prolonged clinical improvement. Arthritis Res Ther. 2005;7:R1281–8. doi: 10.1186/ar1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Inaba Y, Ozawa R, Imagawa T, Mori M, Hara Y, Miyamae T, et al. Radiographic improvement of damaged large joints in children with systemic juvenile idiopathic arthritis following tocilizumab treatment. Ann Rheum Dis. 2011;70:1693–5. doi: 10.1136/ard.2010.145359. [DOI] [PubMed] [Google Scholar]
- 47.De La Torre M, Arboleya L, Pozo S, Pinto J, Velasco J. Rapid and sustained response to tocilizumab, anti-interleukin-6 receptor antibody, in a patient with nephrotic syndrome secondary to systemic juvenile idiopathic arthritis-related amyloidosis. NDT Plus. 2011;4:178–80. doi: 10.1093/ndtplus/sfr004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yokota S, Imagawa T, Mori M, Miyamae T, Takei S, Iwata N, et al. Long-term treatment of systemic juvenile idiopathic arthritis with tocilizumab: results of an open-label extension study in Japan [letter] Ann Rheum Dis. 2013;72:627–8. doi: 10.1136/annrheumdis-2012-202310. [DOI] [PubMed] [Google Scholar]
- 49.Yokota S, Imagawa T, Mori M, Miyamae T, Aihara Y, Takei S, et al. Efficacy and safety of tocilizumab in patients with systemic-onset juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled, withdrawal phase III trial. Lancet. 2008;371:998–1006. doi: 10.1016/S0140-6736(08)60454-7. [DOI] [PubMed] [Google Scholar]
- 50.Becker ML, Rose CD, Cron RQ, Sherry DD, Bilker WB, Lautenbach E. Effectiveness and toxicity of methotrexate in juvenile idiopathic arthritis: comparison of 2 initial dosing regimens. J Rheumatol. 2010;37:870–5. doi: 10.3899/jrheum.090826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klein A, Kaul I, Foeldvari I, Ganser G, Urban A, Horneff G. Efficacy and safety of oral and parenteral methotrexate therapy in children with juvenile idiopathic arthritis: an observational study with patients from the German Methotrexate Registry. Arthritis Care Res (Hoboken) 2012;64:1349–56. doi: 10.1002/acr.21697. [DOI] [PubMed] [Google Scholar]
- 52.Foeldvari I, Wierk A. Effectiveness of leflunomide in patients with juvenile idiopathic arthritis in clinical practice. J Rheumatol. 2010;37:1763–7. doi: 10.3899/jrheum.090874. [DOI] [PubMed] [Google Scholar]
- 53.Jahan A, Dewan V, Yadav TP. Leflunomide in systemic onset juvenile idiopathic arthritis. Indian Pediatr. 2012;49:750–2. doi: 10.1007/s13312-012-0139-9. [DOI] [PubMed] [Google Scholar]
- 54.Record JL, Beukelman T, Cron RQ. Combination therapy of abatacept and anakinra in children with refractory systemic juvenile idiopathic arthritis: a retrospective case series [letter] J Rheumatol. 2011;38:180–1. doi: 10.3899/jrheum.100726. [DOI] [PubMed] [Google Scholar]
- 55.Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Perez N, Silva CA, et al. for the Paediatric Rheumatology International Trials Organization and the Pediatric Rheumatology Collaborative Study Group Long-term safety and efficacy of abatacept in children with juvenile idiopathic arthritis. Arthritis Rheum. 2010;62:1792–802. doi: 10.1002/art.27431. [DOI] [PubMed] [Google Scholar]
- 56.Ruperto N, Lovell DJ, Li T, Sztajnbok F, Goldenstein-Schainberg C, Scheinberg M, et al. for the Paediatric Rheumatology International Trials Organization (PRINTO) and the Pediatric Rheumatology Collaborative Study Group (PRCGS) Abatacept improves health-related quality of life, pain, sleep quality, and daily participation in subjects with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2010;62:1542–51. doi: 10.1002/acr.20283. [DOI] [PubMed] [Google Scholar]
- 57.Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Perez N, Silva CA, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372:383–91. doi: 10.1016/S0140-6736(08)60998-8. [DOI] [PubMed] [Google Scholar]
- 58.Ilowite N, Porras O, Reiff A, Rudge S, Punaro M, Martin A, et al. Anakinra in the treatment of polyarticular-course juvenile rheumatoid arthritis: safety and preliminary efficacy results of a randomized multicenter study. Clin Rheumatol. 2009;28:129–37. doi: 10.1007/s10067-008-0995-9. [DOI] [PubMed] [Google Scholar]
- 59.Papsdorf V, Horneff G. Complete control of disease activity and remission induced by treatment with etanercept in juvenile idiopathic arthritis. Rheumatology (Oxford) 2011;50:214–21. doi: 10.1093/rheumatology/keq292. [DOI] [PubMed] [Google Scholar]
- 60.Otten MH, Prince FH, Armbrust W, ten Cate R, Hoppenreijs EP, Twilt M, et al. Factors associated with treatment response to etanercept in juvenile idiopathic arthritis. JAMA. 2011;306:2340–7. doi: 10.1001/jama.2011.1671. [DOI] [PubMed] [Google Scholar]
- 61.Zuber Z, Rutkowska-Sak L, Postepski J, Dobrzyniecka B, Opoka-Winiarska V, Kobusinska K, et al. Etanercept treatment in juvenile idiopathic arthritis: the Polish registry. Med Sci Monit. 2011;17:SR35–42. doi: 10.12659/MSM.882109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miettunen PM, Narendran A, Jayanthan A, Behrens EM, Cron RQ. Successful treatment of severe paediatric rheumatic disease-associated macrophage activation syndrome with interleukin-1 inhibition following conventional immunosuppressive therapy: case series with 12 patients. Rheumatology (Oxford) 2011;50:417–9. doi: 10.1093/rheumatology/keq218. [DOI] [PubMed] [Google Scholar]
- 63.Bruck N, Suttorp M, Kabus M, Heubner G, Gahr M, Pessler F. Rapid and sustained remission of systemic juvenile idiopathic arthritis-associated macrophage activation syndrome through treatment with anakinra and corticosteroids. J Clin Rheumatol. 2011;17:23–7. doi: 10.1097/RHU.0b013e318205092d. [DOI] [PubMed] [Google Scholar]
- 64.Kelly A, Ramanan AV. A case of macrophage activation syndrome successfully treated with anakinra. Nat Clin Pract Rheumatol. 2008;4:615–20. doi: 10.1038/ncprheum0919. [DOI] [PubMed] [Google Scholar]
- 65.Mouy R, Stephan JL, Pillet P, Haddad E, Hubert P, Prieur AM. Efficacy of cyclosporine A in the treatment of macrophage activation syndrome in juvenile arthritis: report of five cases. J Pediatr. 1996;129:750–4. doi: 10.1016/s0022-3476(96)70160-9. [DOI] [PubMed] [Google Scholar]
- 66.Mizrahi M, Ben-Chetrit E. Relapsing macrophage activating syndrome in a 15-year-old girl with Still's disease: a case report. J Med Case Rep. 2009;3:138. doi: 10.1186/1752-1947-3-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hur M, Kim YC, Lee KM, Kim KN. Macrophage activation syndrome in a child with systemic juvenile rheumatoid arthritis. J Korean Med Sci. 2005;20:695–8. doi: 10.3346/jkms.2005.20.4.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ravelli A, De Benedetti F, Viola S, Martini A. Macrophage activation syndrome in systemic juvenile rheumatoid arthritis successfully treated with cyclosporine. J Pediatr. 1996;128:275–8. doi: 10.1016/s0022-3476(96)70408-0. [DOI] [PubMed] [Google Scholar]
- 69.Cortis E, Insalaco A. Macrophage activation syndrome in juvenile idiopathic arthritis. Acta Paediatr Suppl. 2006;95:38–41. doi: 10.1111/j.1651-2227.2006.tb02414.x. [DOI] [PubMed] [Google Scholar]
- 70.Cuende E, Vesga JC, Perez LB, Ardanaz MT, Guinea J. Macrophage activation syndrome as the initial manifestation of systemic onset juvenile idiopathic arthritis [letter] Clin Exp Rheumatol. 2001;19:764–5. [PubMed] [Google Scholar]
- 71.Hadchouel M, Prieur AM, Griscelli C. Acute hemorrhagic, hepatic, and neurologic manifestations in juvenile rheumatoid arthritis: possible relationship to drugs or infection. J Pediatr. 1985;106:561–6. doi: 10.1016/s0022-3476(85)80072-x. [DOI] [PubMed] [Google Scholar]
- 72.Ilowite NT, Sandborg CI, Feldman BM, Grom A, Schanberg LE, Giannini EH, et al. Algorithm development for corticosteroid management in systemic juvenile idiopathic arthritis trial using consensus methodology. Pediatr Rheumatol Online J. 2012;10:31. doi: 10.1186/1546-0096-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ravelli A, Magni-Manzoni S, Pistorio A, Besana C, Foti T, Ruperto N, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005;146:598–604. doi: 10.1016/j.jpeds.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 74.Davi S, Consolaro A, Guseinova D, Pistorio A, Ruperto N, Martini A, et al. An international consensus survey of diagnostic criteria for macrophage activation syndrome in systemic juvenile idiopathic arthritis. J Rheumatol. 2011;38:764–8. doi: 10.3899/jrheum.100996. [DOI] [PubMed] [Google Scholar]
- 75.Red Book: 2009 report of the Committee on Infectious Diseases. 28. Elk Grove Village (IL): American Academy of Pediatrics; 2009. [Google Scholar]
- 76.Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K. Updated guidelines for using interferon γ release assays to detect Mycobacterium tuberculosis infection: United States, 2010. MMWR Recomm Rep. 2010;59:1–25. [PubMed] [Google Scholar]
- 77.DeWitt EM, Kimura Y, Beukelman T, Nigrovic PA, Onel K, Prahalad S, et al. on behalf of the Juvenile Idiopathic Arthritis Disease-Specific Research Committee of the Childhood Arthritis and Rheumatology Research Alliance Consensus treatment plans for new-onset systemic juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2012;64:1001–10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


