Abstract
Objectives
The most recent reports of nationally representative health-related quality of life (HRQoL) values for the United States use data that were collected over a decade ago. We update these values using data from 2011, stratified by age and sex.
Methods
This study uses data from 2 sources—the 2011 Medical Expenditures Panel Survey (MEPS) and the 2011 National Health Interview Survey (NHIS). Both are nationally representative surveys of the US non-institutionalized civilian population. The MEPS was used to calculate four HRQoL scores: categorical self-rated health, mental and physical component summaries from the SF-12, and the SF-6D. We also estimated Quality of Well-being scale scores from the NHIS. We report means and quartiles for all continuous scores, stratified by decade-of-age and sex.
Results
There were 23,906 eligible subjects in the 2011 MEPS and 32,242 eligible subjects in the 2011 NHIS. All age and sex categories had instrument completion rates above 84%. Females reported lower mean scores than males across all ages and instruments. In general, those in older age groups reported lower scores than younger age groups, with the exception of the mental component summary from the SF-12. When compared to prior reports, these new values were generally lower than prior reports but rarely reached minimally important difference criteria.
Conclusions
This report updates US nationally representative age- and sex-stratified estimates for five HRQoL scores using data from 2011. These values are important for use in both generalized comparisons of health status and in cost-effectiveness analyses.
Keywords: Health status, quality of life, surveys and questionnaires, United States
Introduction
Standardized health-related quality of life (HRQoL) measures are used to describe health status and measure health changes over time in both individuals and groups. Standardization ensures comparability across different studies, and generic HRQoL measures are important for comparisons across different diseases and health conditions. Generic HRQoL measures with algorithms that yield utility scores are appropriate for constructing quality-adjusted life years to inform decision making, as well as for cost-effectiveness analyses.1 Several reports by the Institute of Medicine have called for the use of standardized measures of population health to track the wellness of the populations over time2. However, we still do not have a standardized population health metric for the US population.
Some generic HRQoL measures have been included in US nationally representative datasets3. As a step towards quantifying US population health, we previously published a catalog of values representative of the US non-institutionalized civilian population using data collected in 2001 in the Medical Expenditures Panel Survey (MEPS) and the National Health Interview Survey (NHIS).3–5 The data collected in 2011 were recently released, so we report 10-year updates for five of the HRQoL measures included in the prior catalog: categorical self-rated health, mental and physical component summaries from the SF-12,6 an estimated Quality of Well-being (QWB) score,7 and the SF-6D.8
Methods
Subjects
This study uses data from 2 sources—the 2011 MEPS and the 2011 NHIS. Both are nationally representative surveys of the US non-institutionalized civilian population. The NHIS is an interviewer-administered, cross-sectional household survey, which gathers information on all household members with detailed information about one adult and one child per household. The detailed information includes health status information used in this analysis. The NHIS sampling and interviewing are continuous throughout each year (see http://www.cdc.gov/nchs/nhis.htm).
The sampling frame of the Household Component of the Medical Expenditure Panel Survey (MEPS-HC) is drawn from respondents to the National Health Interview Survey. The MEPS-HC collects data from a nationally representative sample of households through an overlapping panel design. The two years of data for each panel are collected in five rounds of interviews. This provides continuous and current estimates of health care expenditures at both the person and household level for two panels for each calendar year. In 2011, the Self-Administered Questionnaire given to all adults aged 18 years or older in MEPS included the SF-12 v2™ and categorical self-rated health9.
Measures
Mental Component Summary (MCS) and Physical Component Summary (PCS)—Self-Administered
Data were obtained using the Medical Outcomes Study 12 item Short Form (SF-12 v2™)6 The 12 multiple-choice items of the SF-12 relate to eight health dimensions: physical functioning, physical role limitations, emotional role limitations, pain, general health, vitality, social functioning, and mental health. The MCS and PCS were developed from reducing the eight dimensions to two dimensions using factor analysis. The factor scores were normalized so that both the MCS and PCS have averages of 50 and standard deviations of 10, with respect to the proprietary US national dataset held by QualityMetric, Inc. (Lincoln, RI)10. We included imputed scores that were calculated using a proprietary algorithm of QualityMetric, Inc. and in the MEPS dataset.
The SF-12 also includes the categorical self-rated health item, “In general, would you say your health is: Excellent, Very good, Good, Fair, or Poor?”.
Quality of Well-being (QWB) Scale (Estimated)—Interviewer Administered
The QWB Scale categorizes a respondent with respect to mobility, physical activity, social activity, and symptom/problem. Preference weights for each function level were derived from 867 raters, and a scoring algorithm was developed to yield scores between 0 and 1.11 A QWB estimation (QWBx1) procedure has been developed from NHIS data recorded from 1979 to 19967. NHIS data since 1997 contained questions on functional limitations that more closely match with the QWB social activity and physical activity subscales and the estimate algorithm was modified to reflect these changes. The modified algorithm can be accessed at http://www.pitt.edu/~jzh23/.
SF-6D—Self-Administered
The SF-6D scoring algorithm uses seven questions from the SF-12. These questions were used to construct health scenarios that were evaluated using the standard-gamble technique in a representative sample of the UK population8. Regression analysis was then used to model the preferences assigned to each health status. A utility-based score can be assigned to each health status using the resulting scoring algorithm with scores between 0 and 1.
Analyses
Data were analyzed using SAS 9.3 (Cary, NC) to allow adjustment for the complex sampling design of the MEPS and the NHIS. The reported results incorporate the sampling and post-stratification weights, yielding nationally representative estimates for non-institutionalized adults.
For categorical self-rated health, we report the full distribution of responses. For each continuous scale, we report the estimated mean value, 95% confidence interval around the mean estimate, and quartile-point estimates. All analyses were stratified by sex and decade of age.
Results
There were 23,906 eligible subjects in the 2011 MEPS and 32,242 eligible subjects in the 2011 NHIS. Supplemental Table 1 shows the number of respondents in each sample for each HRQoL measure stratified by age and sex. In general, instrument completion rates were very high, and all completion rates were above 84%. Imputation of the QWBx1 was completed for all respondents in NHIS.
Supplemental Table 2 presents the full distribution of categorical self-rated health responses stratified by age and sex. Females were less likely than males to report “excellent” self-rated health in all age groups. As age increased, the proportion of those who reported “excellent” and “very good” health decreased, while the proportion of those who reported “fair” and “poor” health increased in both females and males.
When categorical self-rated health results were compared to the results from 2001 data, there was an increase in “excellent” reports from 20- to 29-year-old females and males. Results from those aged 30–39, 40–49, and 50–59 were similar to results from 2001, though there was a small but consistent decrease in the proportion of males who reported “excellent” or “very good” health in these age groups. There was an increase in “excellent” and “very good” health responses in females and males aged 60–69, 70–79, and 80–89. For example, the proportion of 60–69-year-old females who reported “excellent” health was 9.0% in 2001 and 11.2% in 2011.
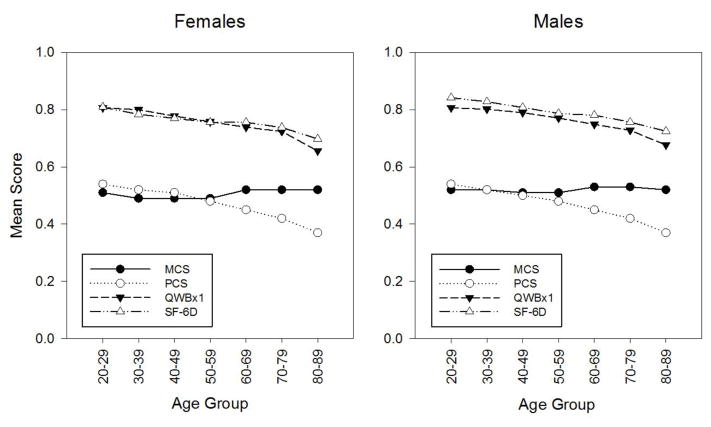
Results from the continuous HRQoL measures illustrate age- and sex-stratified mean scores (Table 1, Supplemental Table 3, and Figure 1). All scores are lower for females than for males. Older age groups reported lower PCS, SF-6D, and QWBx1 scores but higher MCS scores.
Table 1.
Age- and Sex-Stratified Mean and 95% Confidence Interval (CI) for Each Continuous Health-Related Quality-of-Life Summary Score
| Females | Males | ||||||
|---|---|---|---|---|---|---|---|
| Measure | Age Group | Lower 95% CI | Mean | Upper 95% CI | Lower 95% CI | Mean | Upper 95% CI |
| MCS (SF-12) | 20–29 | 50.0 | 50.5 | 51.1 | 51.7 | 52.3 | 52.8 |
| 30–39 | 48.7 | 49.2 | 49.7 | 51.2 | 51.6 | 52.1 | |
| 40–49 | 48.3 | 48.9 | 49.4 | 50.6 | 51.2 | 51.8 | |
| 50–59 | 49.2 | 49.8 | 50.4 | 50.6 | 51.1 | 51.6 | |
| 60–69 | 50.9 | 51.5 | 52.0 | 52.2 | 52.7 | 53.2 | |
| 70–79 | 51.1 | 52.0 | 52.9 | 51.8 | 52.6 | 53.4 | |
| 80–89 | 50.7 | 51.7 | 52.8 | 50.5 | 51.7 | 52.9 | |
| PCS (SF-12) | 20–29 | 53.1 | 53.5 | 53.9 | 54.1 | 54.5 | 54.9 |
| 30–39 | 51.5 | 52.0 | 52.4 | 52.6 | 53.1 | 53.5 | |
| 40–49 | 49.5 | 50.1 | 50.6 | 50.6 | 51.1 | 51.7 | |
| 50–59 | 47.0 | 47.6 | 48.2 | 48.2 | 48.8 | 49.4 | |
| 60–69 | 44.0 | 44.9 | 45.7 | 45.7 | 46.5 | 47.3 | |
| 70–79 | 40.8 | 41.7 | 42.6 | 42.2 | 43.2 | 44.1 | |
| 80–89 | 36.0 | 37.3 | 38.5 | 37.0 | 38.5 | 39.9 | |
| QWBx1 | 20–29 | 0.807 | 0.807 | 0.807 | 0.807 | 0.807 | 0.807 |
| 30–39 | 0.800 | 0.800 | 0.800 | 0.802 | 0.802 | 0.802 | |
| 40–49 | 0.778 | 0.778 | 0.778 | 0.790 | 0.790 | 0.790 | |
| 50–59 | 0.758 | 0.758 | 0.758 | 0.771 | 0.771 | 0.771 | |
| 60–69 | 0.739 | 0.739 | 0.739 | 0.749 | 0.749 | 0.749 | |
| 70–79 | 0.724 | 0.724 | 0.724 | 0.728 | 0.728 | 0.728 | |
| 80–89 | 0.656 | 0.656 | 0.656 | 0.677 | 0.677 | 0.677 | |
| SF-6D | 20–29 | 0.802 | 0.809 | 0.817 | 0.834 | 0.842 | 0.849 |
| 30–39 | 0.777 | 0.784 | 0.791 | 0.821 | 0.828 | 0.835 | |
| 40–49 | 0.762 | 0.770 | 0.777 | 0.799 | 0.808 | 0.817 | |
| 50–59 | 0.747 | 0.756 | 0.765 | 0.778 | 0.787 | 0.796 | |
| 60–69 | 0.746 | 0.756 | 0.766 | 0.770 | 0.781 | 0.791 | |
| 70–79 | 0.724 | 0.738 | 0.752 | 0.744 | 0.757 | 0.769 | |
| 80–89 | 0.680 | 0.698 | 0.715 | 0.706 | 0.725 | 0.745 | |
Note: MCS, mental component summary from the SF-12; PCS, physical component summary from the SF-12; QWB, Quality of Well-being Scale. Sampling weights are taken into account.
Figure 1. Age- and sex-stratified mean scores for the MCS, PCS, QWBx1, and SF-6D scores.
MCS is the mental component summary score and PCS is the physical component summary score for the SF-12; these scores have been rescaled from 0–100 to 0–1.0 for illustration purposes. QWBx1 is the estimated Quality of Well-being scale and SF-6D is the Short form-6D from the SF-12.
When comparing 2001 to 2011 results, mean scores for the QWBx1 were lower in 2011 than 2001 in all age groups under age 70 and slightly higher in the oldest age group, though none reached an MID of 0.0312. Mean scores for the SF-6D were lower in all age- and sex-stratified groups, with an MID of 0.0313 reached in females aged 30–39, 40–49, and 50–59 and males aged 50–59. There were small differences in mean MCS and PCS though none reached a minimally important difference (MID) of 5 points10. Comparing results from 2001 to 2011 for SF-12 derived scores is somewhat problematic because 2001 used the SF-12 version 1, while 2011 used SF-12 version 2™. The first use of version 2 in MEPS was in 2003. When comparing 2003 to 2011 results, neither MCS nor PCS scores showed changes that reached MID.
Discussion
This report updates US nationally representative age- and sex-stratified estimates for five HRQoL scores using data from 2011. Consistent with prior reports, women generally reported lower HRQoL than men, and older individuals reported lower HRQoL than younger individuals. When compared to the 2001 catalog, younger age groups tended to report lower HRQoL and older age groups tended to report higher HRQoL. While the differences generally did not reach minimally important difference criteria, the change in reported health status may be important on a population level as HRQoL is a meaningful measure which has been shown to have a stronger association with survival than cardiovascular risk factors and other biologic measures14.
Other than MEPS and NHIS, there are few other US nationally representative samples that include HRQoL measures. The National Health Measurement Survey collected data by telephone in 2005–2006 from a representative sample of adults aged 35–89 (including categorical self-rated health, EuroQol-5D-3L, SF-36, Health Utilities Index Mark 2 and 3, QWB Scale)4. The Joint Canada/United States Survey of Health collected data by telephone in 2002–2003 for those aged 18 and older (categorical self-rated health, Health Utilities Index Mark 2 and 3)15. The US Valuation of the EuroQol EQ-5D Health States Survey collected self-administered information from those aged 18 and older in 2002 (categorical self-rated health, EuroQol-5D-3L, Health Utilities Index Mark 2 and 316). Given that HRQoL scores are affected by measure,17 mode of administration,3 and year18, continuing collection is necessary. Continued collection of these measures in large nationally representative datasets could inform researchers and policymakers about the selection of the most appropriate method for a national metric of population health.
Supplementary Material
Acknowledgments
Funding/Support: Financial support for this study was provided in part by a grant from the National Institutes of Health through grant number KL2 TR000146 and by the National Institute on Aging through grant number R03 AG048855.
Role of the Sponsors: The funding organizations had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gold MR, Stevenson D, Fryback DG. HALYS and QALYS and DALYS, Oh My: similarities and differences in summary measures of population Health. Annu Rev Public Health. 2002;23:115–34. doi: 10.1146/annurev.publhealth.23.100901.140513. [DOI] [PubMed] [Google Scholar]
- 2.IOM. For the Public’s Health: Investing in a Healthier Future. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 3.Hanmer J, Hays RD, Fryback DG. Mode of administration is important in US national estimates of health-related quality of life. Medical care. 2007;45(12):1171–9. doi: 10.1097/MLR.0b013e3181354828. [DOI] [PubMed] [Google Scholar]
- 4.Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Med Care. 2007;45(12):1162–70. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanmer J, Lawrence WF, Anderson JP, Kaplan RM, Fryback DG. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Med Decis Making. 2006;26(4):391–400. doi: 10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- 6.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 7.Anderson JP, Kaplan RM, Ake CF. Arthritis impact on US life quality: morbidity and mortality effects from National Health Interview Survey data 1986–1988 and 1994 using QWBX1 estimates of well-being. Social Indicators Research. 2004;69(1):67–91. [Google Scholar]
- 8.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics. 2002;21(2):271–92. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 9.Cohen SB, Cohen JW. The capacity of the Medical Expenditure Panel Survey to inform the Affordable Care Act. Inquiry. 2013;50(2):124–34. doi: 10.1177/0046958013513678. [DOI] [PubMed] [Google Scholar]
- 10.JEW, MK, SDK . How to Score the SF-12® Physical and Mental Health Summary Scales. Lincoln RI: QualityMetric Incorporated; 1998. [Google Scholar]
- 11.Kaplan RM, Bush JW, Berry CC. Health status: types of validity and the index of well-being. Health Serv Res. 1976;11(4):478–507. [PMC free article] [PubMed] [Google Scholar]
- 12.Kaplan RM. The minimally clinically important difference in generic utility-based measures. COPD. 2005;2(1):91–7. doi: 10.1081/copd-200052090. [DOI] [PubMed] [Google Scholar]
- 13.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523–32. doi: 10.1007/s11136-004-7713-0. [DOI] [PubMed] [Google Scholar]
- 14.Schnittker J, Bacak V. The increasing predictive validity of self-rated health. PloS one. 2014;9(1):e84933. doi: 10.1371/journal.pone.0084933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanmartin C, Berthelot JM, Ng E, et al. Comparing health and health care use in Canada and the United States. Health affairs. 2006;25(4):1133–42. doi: 10.1377/hlthaff.25.4.1133. [DOI] [PubMed] [Google Scholar]
- 16.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Medical care. 2005;43(3):203–20. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Medical care. 2007;45(12):1162. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. American journal of epidemiology. 2009;170(3):343–51. doi: 10.1093/aje/kwp144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.