Abstract
There is a growing body of evidence demonstrating an association between smoking and DNA methylation. Accordingly, DNA methylation is now considered a promising biomarker of smoking exposure. We evaluated the relationship between methylation markers (AHRR and F2RL3) and urine cotinine as well as self-reported smoking status. DNA methylation levels of AHRR and F2RL3 in blood as well as urine cotinine were measured in 330 adults (46 to 87 years of age). Pyrosequencing was performed to measure DNA methylation of AHRR and F2RL3 associated with smoking exposure. The lung cancer risk associated with DNA methylation and urine cotinine was analyzed using logistic regression analysis. The AHRR and F2RL3 genes were significantly hypomethylated in current smokers compared to in individuals who have never smoked. An inverse relationship was observed between urine cotinine and methylation levels. Methylation of AHRR and F2RL3 distinguished current smokers from never-smokers with high accuracy. Logistic multivariate analysis showed that AHRR methylation is significantly associated with the risk of lung cancer (OR = 0.96, P = 0.011). Our study validated the smoking-associated DNA methylation markers reported in a Korean population-based cohort. In conclusion, DNA methylation of AHRR and F2RL3 provided accurate measures for smoking exposure. Methylation markers reflecting the long-term effect of smoking on the risk of lung cancer showed better performance in distinguishing former smokers from never-smokers.
Introduction
Self-reported exposure to smoke has been widely used to assess the health effects of smoking. Self-reporting, however, can be inaccurate and the amount of smoke products actually inhaled and absorbed depends on the manner of smoking [1, 2]. Serum cotinine is a better measure of smoking exposure than self-reporting methods [3]. However, it only reflects short-term exposure (half-life of cotinine in plasma has been estimated to be about 15–20 hr)[4]. Estimation of long-term smoking exposure is useful for assessing health risks accumulated through tobacco smoking[5].
Recently, long-term smoking exposure may have effects on DNA methylation patterns, which could lead to changes in gene expression and may occur in a broader context to the development or progression of various diseases [6, 7]. A recent study of multi-prospective cohorts demonstrated that hypomethylation of smoking-related genes was associated with lung cancer risk [8].
An epigenome-wide association study from the European Prospective Investigation into Cancer and Nutrition (EPIC-Turin) identified several loci including coagulation factor II (thrombin) receptor-like 3 (F2RL3) and aryl hydrocarbon receptor repressor (AHRR) that are hypomethylated in smokers compared to in non-smokers [9]. Several epigenome-wide studies have consistently shown that the methylation levels of AHRR and F2RL3 were the top-ranked signals associated with tobacco smoking [7, 10] and smoking-related health risks such as lung cancer[11, 12] or cardiovascular disease[13]. Therefore, in the present study, we aimed to validate the previously identified association of the methylation levels of those genes with smoking. In addition, we evaluated the association of methylation with lung cancer risk in a Korean prospective cohort.
We quantified both urine cotinine and blood DNA methylation in a population-based cohort of older adults, and investigated the relationships between DNA methylation and smoke exposure. Furthermore, we assessed the association of both cotinine and DNA methylation biomarkers for risk of lung cancer in a Korean population-based cohort.
Materials and methods
Study population
A total of 110 lung cancer cases and 220 healthy controls matched with age, gender, and area of residence were randomly selected from the Korean National Cancer Center Community Cohort (KNCCC). The KNCCC is a community-based prospective cohort study designed to investigate the relationships in Korea between the risk of cancer and various environmental, lifestyle, and host factors [14]. Baseline information on age, gender, smoking status, and pack year of smokers was included in the present study. Blood and urine samples for each study participant were collected at baseline prior to development of cases and stored at −70°C or below and −20°C, respectively. These samples were used for genetic analysis and cotinine measurement. The cohort was followed from 1993 until 31 December 2012, with an average of 10.1 years of follow-up, through linkage with the Korea National Cancer Incidence Database of the Korean Central Cancer Registry and Cause of Death Database of Statistics Korea. The study participants with a cancer history before cohort enrollment were excluded in the analysis.
The study protocol was approved by the National Cancer Center Institutional Review Boards (IRB number: NCCNHS02-007; NCCNHS03-081-1; NCCNCS-07-080). Participants were provided their written informed consent to participate in this study and the IRB also approved this consent procedure.
Urinary cotinine was measured using liquid chromatography-tandem mass spectrometry (Applied Biosystems/MDS Sciex, Concord, Canada), according to a previous report [15, 16].
Bisulfite treatment and DNA extraction
DNA samples were extracted from buffy coats using the QIAsymphony DNA Midi Kit (Qiagen, Crawley, UK). Bisulfite treatment of 2 mg of each sample was performed using the EZ DNA Methylation Kit (Zymo Research, Orange, CA, USA). The converted DNA was eluted in 50 ml of 0.1X TE buffer and pyrosequenced as previously described [17].
PCR primer design and pyrosequencing methylation analysis
We investigated the methylation status of the AHRR (cg5575921) and F2LR3 (cg03636183) promoters. PCR was performed with FastStart Taq polymerase (Roche Applied Science, IN, USA) using 2 ml of bisulfite modified DNA and 3 mM MgCl2, 50 mM dNTPs, and 0.2 mM primer mixture. Pyrosequencing was performed using a PSQ96MA system (Biotage, Uppsala, Sweden) according to the manufacturer’s protocol. PCR primer sequences and pyrosequencing primers are shown in (Table 1). For sequencing, the assay was validated using an internal control (non-CpG cytosine in targeted methylation sequence region). AHRR and F2RL3 methylation for each sample was calculated as the average value of eight CpGs (mC/total C x 100 (%)) of the promoter CpG islands examined.
Table 1. PCR and pyrosequeincing primers for AHRR and F2RL3.
| Gene | Forward | Reverse | Product size |
|---|---|---|---|
| AHRR | 5′- AGGGGTTGTTTAGGTTATAGATT-3′ | 5′biotin- CCTACCAAAACCACTCCCAAA-3′ | 180 |
| Pyrosequencing primer | 5′- TTTTGAGAGGGTAGT–3′ | ||
| F2RL3 | 5′- GGGTTGGGTGTTTATTAGGT-3′ | 5′biotin-CAACAACAACACTAAACCATACATATA-3′ | 286 |
| Pyrosequencing primer | 5′- GGGGTTGTAGGTTAATGG-3′ |
Statistical analysis
The Kruskal-Wallis ANOVA test was used to compare data. Pearson tests were performed to assess any correlation between methylation values. The logistic regression model was constructed to evaluate the risk of lung cancer with methylation, urine cotinine, age, and sex. The sensitivity and specificity were calculated using receiver operative curve (ROC) analyses. Area under the curve (AUC) values were calculated for AHRR CG site (cg21161138) and F2RL3 (cg03636183), and compared to those for cotinine for differentiating between never- and current smokers. All statistical analyses were performed in NCSS (NCSS, Kaysville, UT, USA).
Results
The characteristics of the study population were described in Table 2. In this study, 320 participants were analyzed after 10 participants with no DNA samples were excluded. The median age was 65 (range 46–87) years for males (n = 223) and 65 (range 39–81) years for female (n = 97).
Table 2. Characteristics of the study population.
| Characteristics | Case | Control | |
|---|---|---|---|
| N (%) 110 (33.3) | N (%) 220 (66.7) | ||
| Gender | |||
| Men | 76 (69.1) | 156 (70.9) | |
| Women | 34 (30.9) | 64 (29.1) | |
| Age (year) | |||
| < 60 | 18 (16.4) | 49 (22.3) | |
| 60–69 | 55 (50.0) | 107 (48.6) | |
| ≥ 70 | 37 (33.6) | 64 (29.1) | |
| Smoking status | |||
| Never smokers | 28 (25.5) | 81 (36.8) | |
| Former smokers | 18 (16.4) | 69 (31.4) | |
| Current smokers | 64 (58.2) | 70 (31.8) | |
| BMI (kg/m2) | |||
| Normal (< 23) | 60 (54.6) | 109 (49.6) | |
| Overweight ( ) 23 and <25) | 23 (20.9) | 43 (19.6) | |
| Obesity ( ( ) 2 | 23 (20.9) | 63 (28.6) | |
| Unknown | 4 (3.6) | 5 (2.3) | |
| Education level | |||
| Uneducated | 43 (39.1) | 48 (21.8) | |
| Elementary school or middle school | 54 (49.1) | 127 (57.7) | |
| High school or more | 5 (4.6) | 32 (14.6) | |
| Unknown | 8 (7.3) | 13 (5.9) | |
| Cotinine (ng/ml) (GM ± GSD)a | 55.5 ± 53.9 | 19.5 ± 23.2 | |
| Pack year among smokers (mean ± SD)b | 37.3 ± 23.3 | 37.3 ± 30.2 | |
| Year follow up (mean ± SD) | 5.3 ± 4.1 | 9.6 ± 4.0 | |
| AHRR methylation% (mean ± SD)c | 55.0 ± 15.5 | 62.4 ± 14.6 | |
| F2RL3 methylation% (mean ± SD)c,d | 72.4 ± 8.8 | 75.8 ± 9.0 | |
Abbreviations: SD, standard deviation; GM, geometric mean; GSD, geometric standard deviation
a Data missing for 14, 11 and 16 participants in never, former and current smokers, respectively.
b Data missing for 8 and 5 participants in former and current smokers
c No DNA samples for 10 participants
d Data failure for 5 participants in F2RL3 methylation analysis
Smoking intensity and urine cotinine levels of the study population
Smoking intensity, estimated by the self-reported smoking measured in pack-years[Median (interquartile)] among former- and current smokers was 30 (0.3–141) and 30.8 (0.9–180), respectively. The median (interquartile) cotinine concentration for current smokers was 1230.0 (645.0–1895.0) ng/ml and the median concentration of cotinine for former- and non-smokers was 2.2 (0.9–5.3) and 2.3 (0.8–4.2) ng/ml, respectively.
AHRR gene and F2RL3 gene methylation and smoking
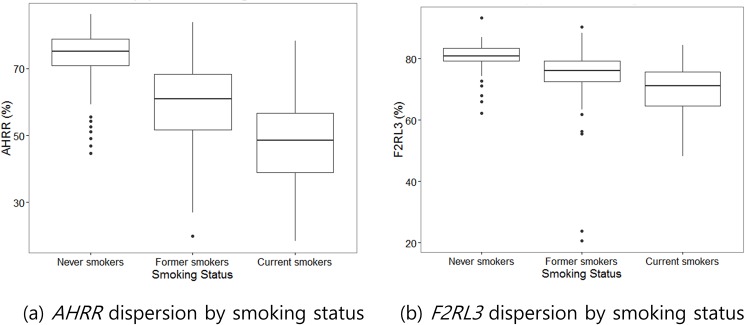
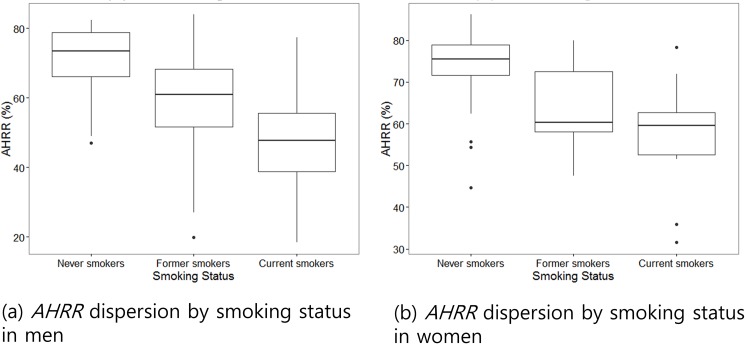
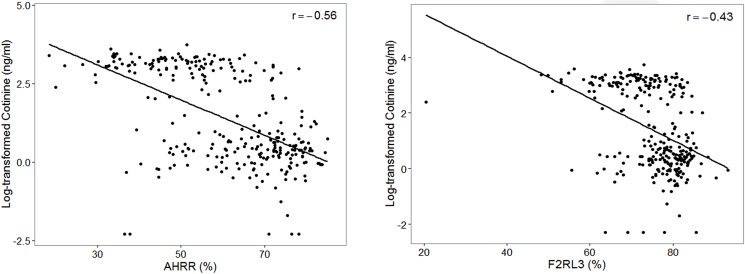
The methylation levels of AHRR and F2RL3 genes were compared according to smoking status (Fig 1). Methylation of the AHRR promoter in current smokers (49.1 ± 12.5%) was significantly lower than in former-smokers (59.4 ± 12.2%, P < 0.001) and never-smokers (73.6 ± 7.9%, P < 0.001, Table 3, S1 Table). F2RL3 was also significantly hypomethylated in current smokers (70.1 ± 8.3%) compared to former- and never-smokers (74.0 ± 10.3 and 80.8 ± 4.2%, respectively, Table 3). Hypomethylation of AHRR (Fig 2) and F2RL3 according to smoking status were still observed even after separating male and female study participants. An inverse relationship was demonstrated between urine cotinine and methylation of AHRR and F2RL3 (r = -0.56, r = -0.43, respectively, P < 0.05, Fig 3).
Fig 1.
Box plots of distribution showing methylation of AHRR (a) and F2RL3 (b) genes in never-, former- and current smokers.
Table 3. Methylation levels for AHRR and F2RL3 genes as differentially methylated in current smokers vs. former- and non-smokers.
| Methylation % (mean+/- SD) | ||||
|---|---|---|---|---|
| Current smoker (n = 130) | Former-smoker (n = 83) | Never-smoker (n = 107) | P | |
| AHRR | 49.1 ± 12.5 | 59.4 ± 12.2 | 73.6 ± 7.9 | <0.001 |
| Male | 48.2 ± 12.2 | 59.1 ± 12.2 | 70.7 ± 10.1 | <0.001 |
| Female | 57.3 ± 12.9 | 63.7 ± 12.2 | 74.6 ± 6.8 | <0.001 |
| F2RL3 | 70.1 ± 8.3 | 74.0 ± 10.3 | 80.8 ± 4.2 | <0.001 |
| Male | 69.8 ± 8.2 | 73.8 ± 10.6 | 79.5 ± 5.7 | <0.001 |
| Female | 72.5 ± 8.7 | 76.5 ± 6.7 | 81.3 ± 3.5 | <0.001 |
Kruskal-Wallis ANOVA test
Fig 2. Box plots of distribution showing methylation of AHRR gene in never-, former- and current smokers according to gender.
Fig 3. The correlation between methylation and urine continine concentration (ng/ml).
The methylation (x-axis) of AHRR (left) and F2RL3 (right) inversely correlated with urine cotinine concentration (y-axis).
Discrimination of current and former smokers vs. never- smokers by cotinine and methylation levels
a. Distinguishing current smokers from non-smokers
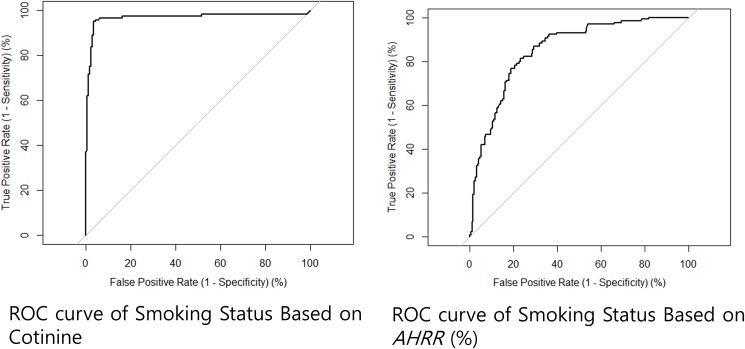
Table 4 indicates the AUC values based on methylation values for each genomic locus in predicting current smoker from never-smoker status, in addition to cotinine. The AUC for AHRR (AUC = 0.942) and F2RL3 (AUC = 0.891) demonstrated similar ability to distinguish former from non-smokers with cotinine levels (AUC = 0.974). With a methylation cut-off of >60.2% for AHRR, the sensitivity was 84.0% and the specificity was 95.4% (Fig 4, Table 4). Discrimination of the performance of urine cotinine between current smokers and never-smokers (>201.0 ng/ml) showed a sensitivity of 89.5% and 100.0% specificity.
Table 4. The AUCs based on methylation (AHRR and F2RL3) and urine cotinine in predicting current smoker from never-smoker status.
| Biomarkers (cut-off) | Sensitivity | Specificity | AUC current vs. never |
|---|---|---|---|
| AHRR (60.2%) | 84.0 | 95.4 | 0.942 |
| F2RL3 (77.6%) | 80.5 | 86.5 | 0.891 |
| Urine Cotinine (>201.0 ng/ml) | 89.5 | 100 | 0.974 |
Fig 4. ROC analysis for predicting current smoking status.
Cotinine levels above the cutoff of 201.0 ng/ml were associated with current smoking status, with high predictive value for current smokers compared to never-smokers (left, AUC = 0.974). Using a cut-off level for AHRR gene methylation of 60.2%, AHRR gene methylation also showed high performance for predicting current smokers (right, AUC = 0.942) with a sensitivity of 84.0% and specificity of 95.4%.
b. Ability to distinguish current and former-smokers from non-smokers
Table 5 indicates the AUC values based on methylation values for each genomic locus in predicting current and former-smoker from never-smoker status. The AUCs for AHRR (AUC = 0.907) and F2RL3 (AUC = 0.859) demonstrated an ability of these parameters to distinguish former from non-smokers. The sensitivity and specificity at the optimal cut-off (AHRR = 68.1%) were 85.4% and 86%, respectively (Table 5).
Table 5. The AUCs based on methylation (AHRR and F2RL3) in predicting current and former smoker from never-smoker status.
| Biomarkers (cut-off) | Sensitivity | Specificity | AUC current & former vs. never |
|---|---|---|---|
| AHRR (68.1%) | 85.4 | 86.0 | 0.907 |
| F2RL3 (78.8%) | 80.6 | 79.8 | 0.859 |
Logistic regression of methylation
Lung cancer patients had significantly more hypomethylated AHRR and F2RL3 compared to controls (Table 2). Urine cotinine levels significantly increased in patients with lung cancer (Table 2).
The logistic multivariate analysis demonstrated that AHRR methylation was significantly associated with the risk of lung cancer (OR = 0.960, 95% CI = 0.930–0.990, P = 0.011). In contrast, the urine cotinine failed to show any association with the risk of lung cancer (OR = 1.019, 95% CI = 0.990–1.050, P = 0.2056, Table 6). Age and sex were also independent factors related to the risk of lung cancer.
Table 6. Odds ratios of lung cancer risk for AHRR and F2RL3 methylation in multivariate analysis.
| Variables | HR | 95%CI | P |
|---|---|---|---|
| Age | 1.047 | 1.007–1.088 | 0.021 |
| Sex (male vs. female) | 2.583 | 1.256–5.314 | 0.010 |
| AHRR methylation | 0.960 | 0.930–0.990 | 0.011 |
| F2RL3 methylation | 1.000 | 0.954–1.049 | 0.978 |
| Urine cotinine/creatinine (ng/mg) | 1.019 | 0.990–1.050 | 0.206 |
Discussion
In this study, we validated studies showing that methylation of AHRR and F2RL3 showed inverse relationships with self-reported smoking status. We also identified an inverse relationship between urine cotinine and methylation markers (AHRR and F2RL3).
In this study, methylation of AHRR and F2RL3 could distinguish current from never-smokers, similar to urine cotinine. Interestingly, only methylation markers were independently associated with the risk of lung cancer. In recent epigenome-wide studies of DNA methylation patterns, it has been found that there is a difference in the DNA methylation of several genes depending on the smoking status[7, 9, 10]. Fasanelli et al. showed that hypomethylation of AHRR and F2RL3 genes is associated with the risk of lung cancer in 4 cohorts [8]. Our study confirmed the previous studies showing that hypomethylation of these AHRR and F2RL3 genes with respect to tobacco smoking was significantly associated with lung cancer risk in a Korean prospective cohort. Logistic multivariate analysis showed that AHRR methylation was significantly associated with the risk of lung cancer (OR = 0.96), but cotinine was not (OR = 1.02) although univariate analysis showed that cotinine was significantly associated with the risk of lung cancer. This finding reflects the long-term effect of methylation on lung cancer development.
Multiple previous studies have investigated the relationship of cotinine levels to lung cancer and showed the relationship of cotinine levels to lung cancer risk [18–20]. Of the tobacco constituents, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) and its parent compound 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) as well as N′-nitrosonornicotine (NNN) are carcinogenic[21], but continine is a noncarcinogenic constituent. NNAL and methylation because NNAL has the longer half-life (t1/2 = 10 days to 3 weeks). The KNCC community cohort samples used in this study is derived from a population-based cohort in Korea with a wide spectrum of data to investigate other chronic diseases in the Korean population [14].
Experimentally, tobacco smoking induces “cancer-associated” epigenomic alterations in cultured respiratory epithelia [22], including lymphoblasts and pulmonary macrophages [23]. With respect to DNA methylation of peripheral blood leukocytes, the tobacoco smoke constituent metabolites enter the bloodstream and directly alter the epigenetic profile of blood leukocytes [9]. Accordingly, the biological effects of smoking could persist for extended periods following smoking cessation [24]. Thus, smoking-associated epigenetic changes could better reflect the risk of lung cancer development in former smokers than cotinine which has a relatively short half-life and was reported to be not associated with the risk of lung cancer in former smokers in large prospective study[25], although the relationship of cotinine levels to lung cancer were showed in several previous studies[18–20, 26].
A definitive inverse relation between cotinine and methylation level was recently identified [5], and we confirmed the relationship between urine cotinine and methylation markers (AHRR and F2RL3) in this study.
Although clear inverse dose-response relationships with F2RL3 methylation intensity were reported for both current intensity and lifetime pack-years of smoking [27], we could not replicate the association between smoking intensity and biomarkers (urine cotinine and methylation of genes) in this study cohort.
Both cotinine and methylation of AHRR accurately distinguished current from never-smokers. However, the discrimination performance of F2RL3 methylation (AUC < 0.900) on current smokers from non-smokers was relatively lower than that of cotinine and AHRR (AUC = 0.974 and AUC = 0.942, respectively). Methylation markers proved excellent for distinguishing current and former-smokers from non-smokers. Methylation markers may serve as better biomarkers for distinguishing former from never-smokers than urine cotinine because urine cotinine has a relatively short half-life and undetectable within several daysafter quitting smoking[4]. In this study, the AUCs for AHRR (AUC = 0.907) and F2RL3 (AUC = 0.859) demonstrated greater ability of these parameters to distinguish former from non-smokers than cotinine levels (AUC = 0.790).
There are large differences in the duration of smoking cessation among former smokers after smoking cessation, so there are individual variations in the risk of smoking-related illness. Alterations in smoke-related methylation are largely reversible after smoking cessation within a few years of smoking cessation[28] and were found to be rapidly reversible whereas some smoking-related genes are slowly normalized or remain abnormal decades after smoking cessation[24, 28, 29]. Such slow reversible genes, potentially detectable for decades after cessation, will be useful biomarkers to precisely measure individual risk profiles of smoking-induced chronic disease such as lung cancer [30]. The expression of some genes, including AHRR, is not normalized to previous levels, which indicates long-term gene expression consequences resulting from DNA methylation changes of prior smoking history [9, 28]. However, methylation status of F2RL3 is reversible, and the levels return to those of non-smokers after smoking cessation [9, 24].
F2RL3 has significant roles in platelet activation [31] and cell signaling [32]. Recently, F2RL3 methylation intensity showed clear dose-response relationships with smoking status and lifetime pack-years of smoking [27]. F2RL3 methylation is a strong predictor of lung cancer risk and mortality [11].
A recent genome-wide approach revealed that AHRR had top-ranked signal changes in DNA methylation associated with tobacco smoking [7]. Shenker et al. showed that AHRR methylation is associated with smoking in WBC DNA and lung tissue [9]. The aryl hydrocarbon receptor (AHR) pathway is important to metabolize diverse biological compounds and synthetic environmental pollutants [9]. Benzopyrene and dioxin-like compounds[33] are released during smoking and are metabolized by AhR, thus releasing further carcinogenic metabolites, which may contribute to tobacco-associated inflammation and lung disease [34, 35]. The gene most strongly upregulated by smoking is AHRR [28]. It was demonstrated that the AHR pathway is required for carcinogen-induced cancer in murine models[28].
In conclusion, although there were several limitations including relatively small sample size and limited numbers of smoking-related methylation genes, this prospective study demonstrated that AHRR and F2RL3 methylation levels had inverse relationships with self-reported smoking status and accurately discriminated for both current- and former- smoking. Moreover, methylation markers distinguished former smokers from never-smokers with high accuracy and significantly associated with an increased risk of lung cancer. Further large prospective studies should be performed to confirm these results. Smoking-related DNA methylations will be promising approach for noninvasive lung cancer screening or risk stratification.
Supporting information
(XLSX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by the National Cancer Center Grant- NCC-1210090 and NCC-1510100.
References
- 1.Rebagliato M. Validation of self reported smoking. Journal of epidemiology and community health. 2002;56(3):163–4. Epub 2002/02/21. PubMed Central PMCID: PMCPmc1732087. doi: 10.1136/jech.56.3.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Connor Gorber S, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2009;11(1):12–24. Epub 2009/02/28. [DOI] [PubMed] [Google Scholar]
- 3.Perez-Stable EJ, Benowitz NL, Marin G. Is serum cotinine a better measure of cigarette smoking than self-report? Preventive medicine. 1995;24(2):171–9. Epub 1995/03/01. [DOI] [PubMed] [Google Scholar]
- 4.Benowitz NL, Kuyt F, Jacob P 3rd, Jones RT, Osman AL . Cotinine disposition and effects. Clinical pharmacology and therapeutics. 1983;34(5):604–11. Epub 1983/11/01. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Y, Florath I, Saum KU, Brenner H. Self-reported smoking, serum cotinine, and blood DNA methylation. Environmental research. 2016;146:395–403. Epub 2016/02/02. doi: 10.1016/j.envres.2016.01.026 [DOI] [PubMed] [Google Scholar]
- 6.Harlid S, Xu Z, Panduri V, Sandler DP, Taylor JA. CpG sites associated with cigarette smoking: analysis of epigenome-wide data from the Sister Study. Environmental health perspectives. 2014;122(7):673–8. Epub 2014/04/08. PubMed Central PMCID: PMCPmc4080519. doi: 10.1289/ehp.1307480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeilinger S, Kuhnel B, Klopp N, Baurecht H, Kleinschmidt A, Gieger C, et al. Tobacco smoking leads to extensive genome-wide changes in DNA methylation. PloS one. 2013;8(5):e63812 Epub 2013/05/22. PubMed Central PMCID: PMCPmc3656907. doi: 10.1371/journal.pone.0063812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fasanelli F, Baglietto L, Ponzi E, Guida F, Campanella G, Johansson M, et al. Hypomethylation of smoking-related genes is associated with future lung cancer in four prospective cohorts. Nature communications. 2015;6:10192 Epub 2015/12/17. PubMed Central PMCID: PMCPmc4682166. doi: 10.1038/ncomms10192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shenker NS, Polidoro S, van Veldhoven K, Sacerdote C, Ricceri F, Birrell MA, et al. Epigenome-wide association study in the European Prospective Investigation into Cancer and Nutrition (EPIC-Turin) identifies novel genetic loci associated with smoking. Human molecular genetics. 2013;22(5):843–51. Epub 2012/11/24. doi: 10.1093/hmg/dds488 [DOI] [PubMed] [Google Scholar]
- 10.Breitling LP, Yang R, Korn B, Burwinkel B, Brenner H. Tobacco-smoking-related differential DNA methylation: 27K discovery and replication. American journal of human genetics. 2011;88(4):450–7. Epub 2011/04/05. PubMed Central PMCID: PMCPmc3071918. doi: 10.1016/j.ajhg.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Schottker B, Ordonez-Mena J, Holleczek B, Yang R, Burwinkel B, et al. F2RL3 methylation, lung cancer incidence and mortality. International journal of cancer. 2015;137(7):1739–48. Epub 2015/03/31. doi: 10.1002/ijc.29537 [DOI] [PubMed] [Google Scholar]
- 12.Baglietto L, Ponzi E, Haycock P, Hodge A, Bianca Assumma M, Jung CH, et al. DNA methylation changes measured in pre-diagnostic peripheral blood samples are associated with smoking and lung cancer risk. International journal of cancer. 2017;140(1):50–61. Epub 2016/09/16. doi: 10.1002/ijc.30431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y, Yang R, Burwinkel B, Breitling LP, Holleczek B, Schottker B, et al. F2RL3 methylation in blood DNA is a strong predictor of mortality. International journal of epidemiology. 2014;43(4):1215–25. Epub 2014/02/11. PubMed Central PMCID: PMCPMC4258765. doi: 10.1093/ije/dyu006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oh JK, Lim MK, Yun EH, Choi MH, Hong ST, Chang SH, et al. Cohort Profile: Community-based prospective cohort from the National Cancer Center, Korea. International journal of epidemiology. 2015. Epub 2015/12/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryu HJ, Seong MW, Nam MH, Kong SY, Lee DH. Simultaneous and sensitive measurement of nicotine and cotinine in small amounts of human hair using liquid chromatography/tandem mass spectrometry. Rapid communications in mass spectrometry: RCM. 2006;20(18):2781–2. Epub 2006/08/22. doi: 10.1002/rcm.2659 [DOI] [PubMed] [Google Scholar]
- 16.Kim J, Kwon HJ, Lee K, Lee DH, Paek Y, Kim SS, et al. Air Quality, Biomarker Levels, and Health Effects on Staff in Korean Restaurants and Pubs Before and After a Smoking Ban. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2015;17(11):1337–46. Epub 2015/02/05. [DOI] [PubMed] [Google Scholar]
- 17.Hwang SH, Kim KU, Kim JE, Kim HH, Lee MK, Lee CH, et al. Detection of HOXA9 gene methylation in tumor tissues and induced sputum samples from primary lung cancer patients. Clinical chemistry and laboratory medicine. 2011;49(4):699–704. Epub 2011/04/13. doi: 10.1515/CCLM.2011.108 [DOI] [PubMed] [Google Scholar]
- 18.Yuan JM, Koh WP, Murphy SE, Fan Y, Wang R, Carmella SG, et al. Urinary levels of tobacco-specific nitrosamine metabolites in relation to lung cancer development in two prospective cohorts of cigarette smokers. Cancer research. 2009;69(7):2990–5. Epub 2009/03/26. PubMed Central PMCID: PMCPMC2664854. doi: 10.1158/0008-5472.CAN-08-4330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yuan JM, Gao YT, Murphy SE, Carmella SG, Wang R, Zhong Y, et al. Urinary levels of cigarette smoke constituent metabolites are prospectively associated with lung cancer development in smokers. Cancer research. 2011;71(21):6749–57. Epub 2011/10/27. PubMed Central PMCID: PMCPMC3392910. doi: 10.1158/0008-5472.CAN-11-0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuan JM, Butler LM, Stepanov I, Hecht SS. Urinary tobacco smoke-constituent biomarkers for assessing risk of lung cancer. Cancer research. 2014;74(2):401–11. Epub 2014/01/11. PubMed Central PMCID: PMCPMC4066207. doi: 10.1158/0008-5472.CAN-13-3178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hecht SS. Biochemistry, biology, and carcinogenicity of tobacco-specific N-nitrosamines. Chemical research in toxicology. 1998;11(6):559–603. Epub 1998/06/24. doi: 10.1021/tx980005y [DOI] [PubMed] [Google Scholar]
- 22.Liu F, Killian JK, Yang M, Walker RL, Hong JA, Zhang M, et al. Epigenomic alterations and gene expression profiles in respiratory epithelia exposed to cigarette smoke condensate. Oncogene. 2010;29(25):3650–64. Epub 2010/05/05. doi: 10.1038/onc.2010.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monick MM, Beach SR, Plume J, Sears R, Gerrard M, Brody GH, et al. Coordinated changes in AHRR methylation in lymphoblasts and pulmonary macrophages from smokers. American journal of medical genetics Part B, Neuropsychiatric genetics: the official publication of the International Society of Psychiatric Genetics. 2012;159b(2):141–51. Epub 2012/01/11. PubMed Central PMCID: PMCPmc3318996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wan ES, Qiu W, Baccarelli A, Carey VJ, Bacherman H, Rennard SI, et al. Cigarette smoking behaviors and time since quitting are associated with differential DNA methylation across the human genome. Human molecular genetics. 2012;21(13):3073–82. Epub 2012/04/12. PubMed Central PMCID: PMCPmc3373248. doi: 10.1093/hmg/dds135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vineis P, Airoldi L, Veglia F, Olgiati L, Pastorelli R, Autrup H, et al. Environmental tobacco smoke and risk of respiratory cancer and chronic obstructive pulmonary disease in former smokers and never smokers in the EPIC prospective study. BMJ (Clinical research ed). 2005;330(7486):277. Epub 2005/02/01. PubMed Central PMCID: PMCPMC548173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan ES, Qiu W, Carey VJ, Morrow J, Bacherman H, Foreman MG, et al. Smoking-Associated Site-Specific Differential Methylation in Buccal Mucosa in the COPDGene Study. American journal of respiratory cell and molecular biology. 2015;53(2):246–54. Epub 2014/12/18. PubMed Central PMCID: PMCPmc4566042. doi: 10.1165/rcmb.2014-0103OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Yang R, Burwinkel B, Breitling LP, Brenner H. F2RL3 methylation as a biomarker of current and lifetime smoking exposures. Environmental health perspectives. 2014;122(2):131–7. Epub 2013/11/26. PubMed Central PMCID: PMCPmc3915264. doi: 10.1289/ehp.1306937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bosse Y, Postma DS, Sin DD, Lamontagne M, Couture C, Gaudreault N, et al. Molecular signature of smoking in human lung tissues. Cancer research. 2012;72(15):3753–63. Epub 2012/06/05. doi: 10.1158/0008-5472.CAN-12-1160 [DOI] [PubMed] [Google Scholar]
- 29.Ambatipudi S, Cuenin C, Hernandez-Vargas H, Ghantous A, Calvez-Kelm FL, Kaaks R, et al. Tobacco smoking-associated genome-wide DNA methylation changes in the EPIC study. Epigenomics. 2016. Epub 2016/02/13. [DOI] [PubMed] [Google Scholar]
- 30.Guida F, Sandanger TM, Castagne R, Campanella G, Polidoro S, Palli D, et al. Dynamics of smoking-induced genome-wide methylation changes with time since smoking cessation. Human molecular genetics. 2015;24(8):2349–59. Epub 2015/01/04. PubMed Central PMCID: PMCPmc4380075. doi: 10.1093/hmg/ddu751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahn ML, Nakanishi-Matsui M, Shapiro MJ, Ishihara H, Coughlin SR. Protease-activated receptors 1 and 4 mediate activation of human platelets by thrombin. The Journal of clinical investigation. 1999;103(6):879–87. Epub 1999/03/17. PubMed Central PMCID: PMCPmc408153. doi: 10.1172/JCI6042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen HT, Tsou HK, Tsai CH, Kuo CC, Chiang YK, Chang CH, et al. Thrombin enhanced migration and MMPs expression of human chondrosarcoma cells involves PAR receptor signaling pathway. Journal of cellular physiology. 2010;223(3):737–45. Epub 2010/02/23. doi: 10.1002/jcp.22083 [DOI] [PubMed] [Google Scholar]
- 33.Van den Berg M, Birnbaum LS, Denison M, De Vito M, Farland W, Feeley M, et al. The 2005 World Health Organization reevaluation of human and Mammalian toxic equivalency factors for dioxins and dioxin-like compounds. Toxicological sciences: an official journal of the Society of Toxicology. 2006;93(2):223–41. Epub 2006/07/11. PubMed Central PMCID: PMCPMC2290740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chiba T, Uchi H, Yasukawa F, Furue M. Role of the arylhydrocarbon receptor in lung disease. International archives of allergy and immunology. 2011;155 Suppl 1:129–34. Epub 2011/06/10. [DOI] [PubMed] [Google Scholar]
- 35.Martey CA, Baglole CJ, Gasiewicz TA, Sime PJ, Phipps RP. The aryl hydrocarbon receptor is a regulator of cigarette smoke induction of the cyclooxygenase and prostaglandin pathways in human lung fibroblasts. American journal of physiology Lung cellular and molecular physiology. 2005;289(3):L391–9. Epub 2005/05/03. doi: 10.1152/ajplung.00062.2005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.