Abstract
The authors present the case of a 46-year-old woman who was admitted to their institution after suffering acute intratumoral hemorrhage. There was no history and evidence of neoplasms, trauma, seizures and coagulopathy in the patient. Surgery was performed for evacuation of the hematoma and tumor excision after brain CT scan. Post operative results her neurologic function recovered completely. The pathology reports revealed angioblastic meningioma. The key to make an early and accurate diagnosis is good radiological examination, and definitive surgery can bring a more favorable outcome, lowering the morbidity and mortality rate.
Keywords: Hemorrhage, intratumoral, meningioma
Introduction
Spontaneous hemorrhage associated with intracranial neoplasms is rare, and only occurs in approximately 1.4-10% from all intracranial neoplasm. These hemorrhages are mostly associated with malignancy such as glioblastomas, oligodendrogliomas, and metastatic brain tumors.[1,2,3] Meningiomas is slow growing, usually benign, and extra-axial tumor arising from arachnoid cap cell.
Meningiomas associated with intratumoral hemorrhage is very rare, and the pathophysiology mechanisms of the bleeding are currently not well understood.[1,2,3,4] The incidence of hemorrhage associated with meningiomas is between 0.5-2.4% with a mortality rate of 28-50% in the last three decades.[4,5,6,7] Niiro et al.[4] described only six cases (2%) with hemorrhagic onset in a series of 298 patients with intracranial meningioma.
Hemorrhage associated with meningiomas may remain confined within the tumor itself (intratumoral), within the surrounding brain parenchyma (intracerebral), or extend into the subarachnoid spaces.[3,8] We have experienced one case of convexity meningioma manifesting spontaneous intratumoral hemorrhage.
Case Report
History and presentation
A 46-year-old woman with a history of controlled hypertension for 1 year was admitted to our hospital with sudden episode of unconsciousness and left-sided hemiparesis. She had severe headache, hemiparesis, severe vomiting one day before admission. There was no history symptoms of neoplasm, trauma, seizures, and coagulopathy in the patient. The patient was treated by neurologic division in emergency room and consulted to our department.
Examination
On admission, she was comatose, blood pressure 180/90 mmHg, pupil unequal with right dilated pupil, and left-sided hemiparesis. Blood laboratory values, chest x-ray and electrocardiography were within normal limit. Brain CT scan without contrast showed a right temporoparietal hyperdense lesion [Figure 1a]. Due to the patient's history, neurologic examination, and brain CT scan results, we decided to perform craniotomy evacuation of hematoma immediately.
Figure 1.
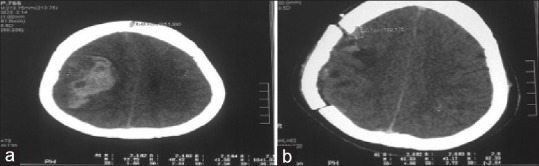
(a) Preoperative brain CT scan without contrast; (b) Postoperative brain CT scan without contrast
Operative and pathological examination
Emergency right temporoparietal craniotomy was performed and a soft mass, extra axial tumor was found with a large hematoma cavity within the mass itself [Figure 2]. All the mass and hematoma were removed completely. Histopathology examination revealed angioblastic meningioma with necrosis and hemorrhagic centers inside the tumor [Figure 3].
Figure 2.
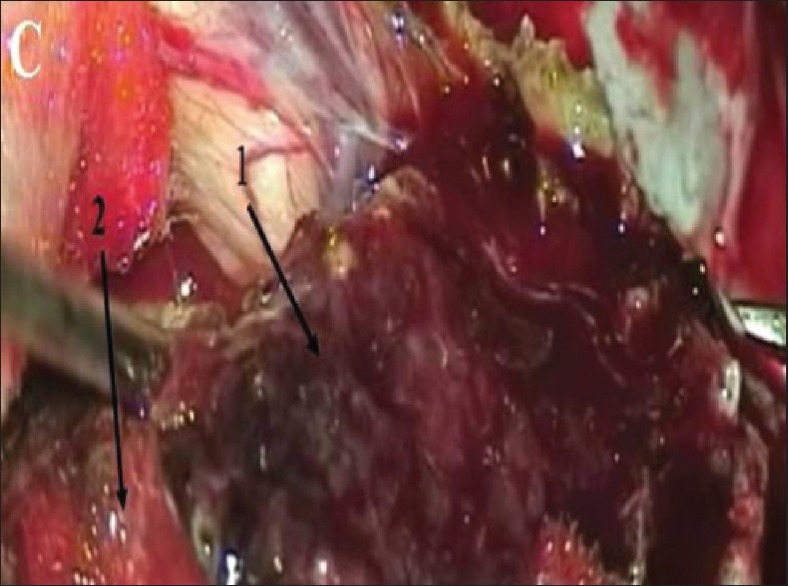
Intraoperative picture. Arrow no. 1 – Hematoma; 2 – Mass
Figure 3.
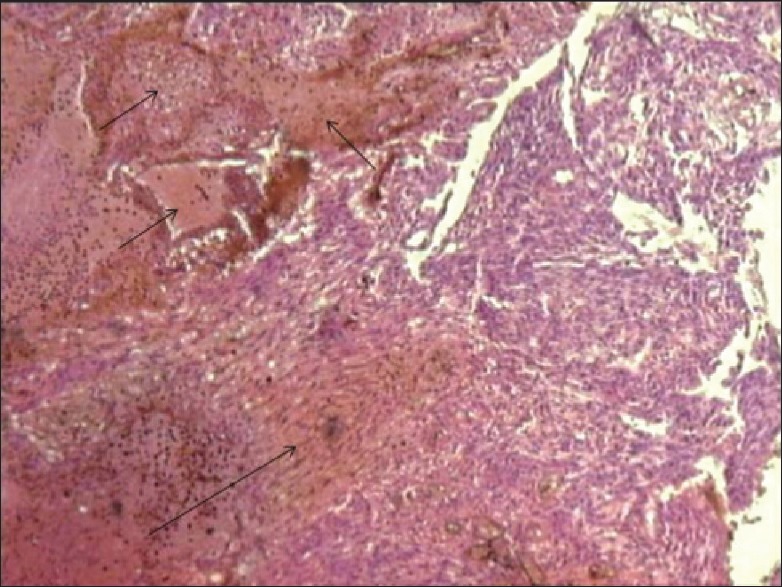
Angiomatous meningioma – A meningioma in which many large and small vascular channels predominate, with small intervening nests of meningotheliomatous or fibrous meningioma (three small arrows), hematoma on stroma (long arrow)
Postoperative course
Control brain CT Scans confirmed complete removal of the lesion as shown in Figure 1b, and the patient was discharged from hospital on the 7th postoperative day. All her neurological function recovered completely.
Discussion
The apoplexy form was found in our patient who experienced stroke-like symptoms. Angioblastic meningiomas characteristically are composed by abnormal blood vessels, and this abnormal vascularity could be related with tumor-associated hemorrhage. Helle and Conley[9] calculated the “relative bleeding tendency” of meningiomas, and found that the angioblastic and malignant varieties tended to bleed more frequently than the others. These increased bleeding tendency also reconfirmed by Bosnjak et al.,[5] in their large series of meningiomas review. There was a trend that convexity location and angioblastic or fibrous histologic type has tendency to increased of spontaneous bleeding.[5,9] This trend was also found in our case, located convexity and angioblastic type.
Actually subarachnoid hemorrhage is the most common location followed by intracerebral location, while subdural and intratumoral hemorrhage are less common.[1,3,8] Intratumoral hemorrhage is quite rare and is usually associated with anticoagulation consumption or following preoperative tumor embolization.[10,11,12] Some authors reported that subdural hemorrhage may arise from intratumoral hemorrhage that secondarily diffused into subdural space.[3]
The mortality and morbidity rates differ significantly in the group of conscious, permanently unconscious, or patient with clinical deterioration. This mortality and morbidity rate also influenced by the type of hemorrhage that occurred.[5,9] In our case, her uneventful recovery with no neurologicaldeficit relates to the type of intratumoral hemorrhage only, and early hematoma evacuation with tumor removal.
Hypothesis of intratumoral bleeding
The pathophysiological mechanisms of underlying spontaneous meningioma bleeding are not well understood, but several hypotheses have been proposed lately.
Rupture of the abnormal vascular network of the tumor. This hypothesis is based on the histological findings, such as thin-walled vessels or direct peritumoral erosion by the tumor[1,3,4,8,9,13]
Intratumoral infarct and necrosis caused by rapid growth of the tumor or by venous thrombosis.[1,4,6,9,13] Kim et al.[1] reported extensive intratumoral infarct and no abnormal blood vessels were encountered on histological examination from all three cases of spontaneous peritumoral hemorrhage from meningioma. As the infarct progress, the intratumoral pressure increased and rupture of the peritumoral vessel eventually occurs. Intratumoral infarct is not the cause of hemorrhage, but the result
Enlarged feeding arteries become tortuous, less resistant to blood pressure changes and finally susceptible to rupture under stressful conditions[1,9,13]
Stretching of the subdural bridging veins caused by the expansion and tumor growth may cause the veins to rupture.[1,3,4,6,8,13] Martinez-Lage et al.[6] reported that 10 out of 57 cases of meningioma with hemorrhage presented with subdural hemorrhage. But this mechanisms cannot explain the acute and devastating subdural hematoma associated with small meningiomas[3]
Disruption of blood vessels by direct vascular invasion by the tumor cells[4,6,8]
Vaso-active substances released by the meningioma.[3,8] Mast cells are usually present in the leptomeninges. They may be seen in small numbers in meningiomas, primarily syncytial-type meningiomas. Mast cell granules contain many substances such as histamine, heparin, tryptase, superoxide dismutase, beta-hexosaminidase, leukotrienes, eosinophil, and neutrophil chemotactic factors. These intratumoral vaso-active substances such as histamine could induce vasodilatation and tumoral hemorrhage. Intratumoral hemorrhage is most frequently associated with syncytial meningiomas.[3]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Dr. Titien Suseri, SpPA (Dept of pathology) for preparation of the microphotographs.
References
- 1.Kim DG, Park CK, Paek SH, Choe GY, Gwak HS, Yoo H, et al. Meningioma manifesting intracerebral haemorrhage: A possible mechanism of haemorrage. Acta neurochir (Wien) 2000;142:165–8. doi: 10.1007/s007010050019. [DOI] [PubMed] [Google Scholar]
- 2.Kwon Y, Ahn JS, Jeon SR, Kim JH, Kim CJ, Lee JK, et al. Intratumoral bleeding in meningioma after gamma knife radiosurgery. J Neurosurg. 2002;97:657–62. doi: 10.3171/jns.2002.97.supplement. [DOI] [PubMed] [Google Scholar]
- 3.Lefranc F, Nagy N, Dewitte O, Balériaux D, Brotchi J. Intracranial meningiomas revealed by non-traumatic subdural haematomas: A series of four cases. Acta neurochir (Wien) 2001;143:977–82. doi: 10.1007/s007010170002. [DOI] [PubMed] [Google Scholar]
- 4.Niiro M, Ishimaru K, Hirano H, Yunoue S, Kuratsu J. Clinico-pathological study of meningiomas with haemorrhagic onset. Acta neurochir (Wien) 2003;145:767–72. doi: 10.1007/s00701-003-0089-z. [DOI] [PubMed] [Google Scholar]
- 5.Bosnjak R, Derham C, Ravnik J. Spontaneous intracranial meningioma bleeding: Clinicopathological features and outcome. J Neurosurg. 2005;103:473–84. doi: 10.3171/jns.2005.103.3.0473. [DOI] [PubMed] [Google Scholar]
- 6.Martínez-Lage JF, Poza M, Martínez M, Esteban JA, Antúnez MC, Sola J. Meningiomas with haemorrhagic onset. Acta neurochir (Wien) 1991;110:129–32. doi: 10.1007/BF01400680. [DOI] [PubMed] [Google Scholar]
- 7.Ziyal IM, Bilginer B, Celik O, Ozcan OE, Ozgen T. Tentorial meningioma on follow-up presenting with sudden deterioration due to intra- and peritumoral hemorrhage. Acta neurochir (Wien) 2006;148:1315–6. doi: 10.1007/s00701-006-1045-5. [DOI] [PubMed] [Google Scholar]
- 8.Di Rocco F, Mannino S, Puca A, Lauriola L, Pompucci A. Intracranial meningiomas associated with non-traumatic chronic subdural hematoma. Acta neurochir (Wien) 2006;148:1097–102. doi: 10.1007/s00701-006-0861-y. [DOI] [PubMed] [Google Scholar]
- 9.Helle TL, Conley FK. Haemorrhage associated with meningioma: A case report and review of the literature. J Neurol Neurosurg Psychiatry. 1980;43:725–9. doi: 10.1136/jnnp.43.8.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onesti ST, Zahos PA, Ashkenazi E. Spontaneous haemorrhage into a convexity meningioma. Acta neurochir (Wien) 1996;138:1250–1. doi: 10.1007/BF01809756. [DOI] [PubMed] [Google Scholar]
- 11.Kondziolka D, Bernstein M, Resch L, Tator CH, Fleming JF, Vanderlinden RG, et al. Significance of hemorrhage into brain tumors: Clinopathological study. J Neurosurg. 1987;67:852–7. doi: 10.3171/jns.1987.67.6.0852. [DOI] [PubMed] [Google Scholar]
- 12.Maeda K, Gotoh H, Chikui E, Furusawa T. Intratumoral hemorrhage from a posterior fossa tumor after cardiac valve surgery. Neurol Med Chir (Tokyo) 2001;41:548–50. doi: 10.2176/nmc.41.548. [DOI] [PubMed] [Google Scholar]
- 13.Kashimura H, Ogasawara K, Beppu T, Kurose A, Ogawa A. Lipomatous meningioma with concomitant acute subdural hematoma. Neurol Med Chir (Tokyo) 2008;48:466–9. doi: 10.2176/nmc.48.466. [DOI] [PubMed] [Google Scholar]


