Abstract
Dermoid cyst is a congenital lesion that arises due to embryogenic impairment. It accounts for less than 0.3% of all intracranial masses. Herein we report a 30-year-old male who presented with a short history of headache and behavioral disorder. Physical and radiological examination diagnosed it to be a lipoma/epidermoid arising from corpus callosum. The lesion was removed endoscopically and histopathologic examination was performed which confirmed it to be a dermoid cyst. Rarity of the lesion and difficulty in pre-operative diagnosis prompted us to bring forward this case report.
Keywords: Corpus callosum, dermoid cyst, histopathologic
Introduction
Dermoid cyst, a congenital lesion, is classified under the category of “inclusion tumors,” which also includes more prevalent tumors like epidermoids and hamartomas. Dermoid cyst is the least common in this group. Several studies report its prevalence as 0.3%. It arises usually in midline in posterior fossa and with a lesser frequency in thirrd ventricle.[1]
The content of cyst is a greasy grumous material with dermal appendages like sebaceous glands, sweat glands, and hair follicles, which distinguishes it from epidermoid cyst.[1] The symptoms are related to dislocation and compression of brain parenchyma.
Herein, we report a case of intracerebral dermoid cyst arising from the corpus callosum; which was difficult to diagnose without histopathologic examination.
Case Report
A 30-year-old male presented with a low-intensity, poorly localized headache for several months. The family members noticed disorganized behavior for a week prior to his hospitalization without any associated history of neurological deficit or seizures.
Non-contrast computed tomography (CT) scan showed a large fat density mass of size 54 × 47 mm, with a few eccentric calcific foci in the frontal region involving the anterior part of corpus callosum, causing effacement of frontal horns of lateral ventricles and suggesting a diagnosis of corpus callosum lipoma.
Magnetic resonance imaging (MRI) revealed a lesion which was hypointense on T1-weighted (T1W) images and hyperintense on T2-weighted (T2W) images without any contrast enhancement, suggesting the probable diagnosis of epidermoid cyst. Neurosurgeons performed endoscopy-guided procedure and the tissue was removed and sent for histological examination [Figure 1].
Figure 1.

(a and b) Non-contrast computed tomographic scan showing a large fat density mass with few eccentric calcific foci. (c) T1W and (d) T2W images showing a hyperintense lesion in the corpus callosum
Gross examination showed multiple gray-brown soft tissue pieces measuring 40 × 30 × 10 mm.
Microscopic examination revealed mature stratified squamous epithelium along with adnexal structures (hair shaft and sebaceous glands) and keratinous material, confirming the diagnosis of dermoid cyst [Figure 2]. Postoperative course of the patient was unremarkable and he was discharged without any neurological deficit.
Figure 2.
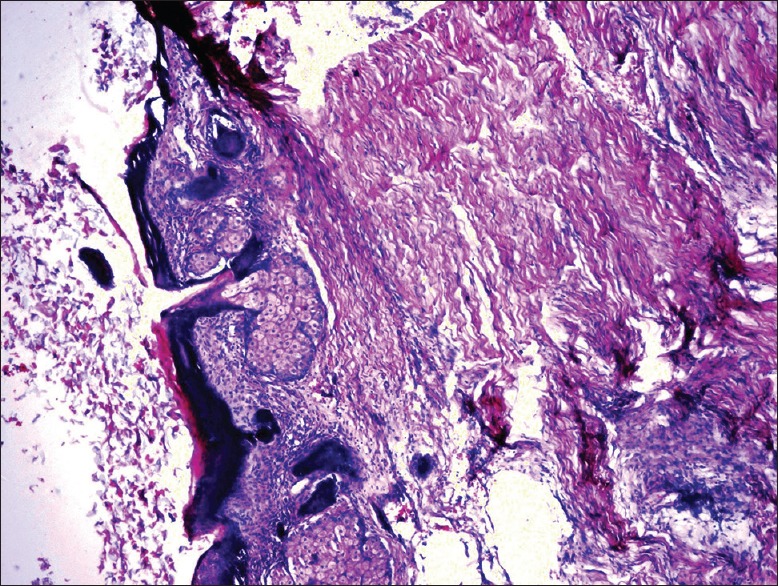
Photomicrograph showing keratinous material along with stratified squamous epithelium, adnexal structures, and glial tissue (H and E; ×200)
Discussion
Intracranial dermoid cyst is a congenital dysembryogenic lesion that develops from inclusion of ectodermal elements during neural tube closure, which explains its propensity for midline.[2]
It is a benign, ectopic, squamous epithelial cyst containing dermal elements, including hair follicles, sebaceous and sweat glands. The lesion is four to nine times less common than epidermoid cyst. Usually it occurs between 2nd and 3rd decades of life, with a male predilection. When the entrapment of embryonic ectoderm tissue into the neural tube occurs between the 5th and 6th weeks of fetal life, the lesion is usually localized in the midline; if the entrapment occurs later, during the formation of secondary cerebral vesicles, it is paramedial.
The most common symptoms are headache (32%) and seizures (30%) and when the cysts are large, symptoms are related to compression of neurovascular structures with eventual development of cerebral hypertension syndrome.
On CT images, the lesion appears as a uniloculated, well-delineated cystic mass with moderate to significant hypodensity (from 0 to −150 HU) and sometimes with capsular calcifications. Generally, it does not show enhancement after contrast administration.
In our patient, the “fat” density or signal seen in the images was probably not due to the presence of adipose tissue but due to lipid content like cholesterol. Heterogeneous aspect depends on a keratinaceous debris, sebaceous and sweat secretions, as well as appendages including hairs.
Epidermoid cysts are classified into two groups: white and black.[3] The former is bright (hyperintense) in both T1 and T2 images, but the latter is hypointense in T1 images and hyperintense in T2 images. MRI of this patient was typically like the images of a black epidermoid cyst.
Conclusion
The distinction between dermoid and epidermoid cysts is prognostically relevant and may have impact on surgical management. In dermoid, the surgical choice is usually subtotal resection as it rarely recurs. In epidermoid, total resection is preferred. Furthermore, the epidermoid cyst has a low incidence of rupture as its growth is not regulated by hormonal factors but only by squamous exfoliation of lining layer, whereas progressive growth of demoid cyst favors its rupture.[4,5] Dissemination of cystic contents into the cortical and cisternal brain space may lead to subsequent meningitis; so its early diagnosis and resection is warranted.[6]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Youmans JR. Youmans Neurological Surgery. 5th ed. Vol. 4. Philadelphia, PA: Saunders; 2004. pp. 1223–4. 3690-2, 4259-60. [Google Scholar]
- 2.Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids and epidermoids of the head and neck. Radiographics. 1995;15:1437–55. doi: 10.1148/radiographics.15.6.8577967. [DOI] [PubMed] [Google Scholar]
- 3.Brown AP, Fogarty B. Radio lucent dermoid cyst: Report of an unusual case. Br J Plast Surg. 2001;54:180. doi: 10.1054/bjps.2000.3508. [DOI] [PubMed] [Google Scholar]
- 4.Ray MJ, Barnett DW, Snipes GJ, Layton KF, Opatowsky MJ. Ruptured intracranial dermoid cyst. Proc (Bayl Univ Med Cent) 2012;25:23–5. doi: 10.1080/08998280.2012.11928775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stendal R, Pietilä TA, Lehmann K, Kurth R, Suess O, Brock M. Ruptured intracranial dermoid cysts. Surg Neurol. 2002;57:391–8. doi: 10.1016/s0090-3019(02)00723-1. [DOI] [PubMed] [Google Scholar]
- 6.Lunardi P, Missori P, Rizzo A, Gagliardi FM. Chemical meningitis in ruptured intracranial dermoid: Case report and review of the literature. Surg Neurol. 1989;32:449–52. doi: 10.1016/0090-3019(89)90010-4. [DOI] [PubMed] [Google Scholar]


