Abstract
Background
Lyme disease is caused by a tick-borne spirochaete of the Borrelia species. It is associated with facial palsy, is increasingly common in England, and may be misdiagnosed as Bell’s palsy.
Aim
To produce an accurate map of Lyme disease diagnosis in England and to identify patients at risk of developing associated facial nerve palsy, to enable prevention, early diagnosis, and effective treatment.
Design and setting
Hospital episode statistics (HES) data in England from the Health and Social Care Information Centre were interrogated from April 2011 to March 2015 for International Classification of Diseases 10th revision (ICD-10) codes A69.2 (Lyme disease) and G51.0 (Bell’s palsy) in isolation, and as a combination.
Method
Patients’ age, sex, postcode, month of diagnosis, and socioeconomic groups as defined according to the English Indices of Deprivation (2004) were also collected.
Results
Lyme disease hospital diagnosis increased by 42% per year from 2011 to 2015 in England. Higher incidence areas, largely rural, were mapped. A trend towards socioeconomic privilege and the months of July to September was observed. Facial palsy in combination with Lyme disease is also increasing, particularly in younger patients, with a mean age of 41.7 years, compared with 59.6 years for Bell’s palsy and 45.9 years for Lyme disease (P = 0.05, analysis of variance [ANOVA]).
Conclusion
Healthcare practitioners should have a high index of suspicion for Lyme disease following travel in the areas shown, particularly in the summer months. The authors suggest that patients presenting with facial palsy should be tested for Lyme disease.
Keywords: diagnosis, facial palsy, general practice, Lyme disease, Lyme borreliosis
INTRODUCTION
Lyme disease is caused by a tick-borne spirochaete of the Borrelia species, and is increasingly common in the UK.1,2 Different strains cause different patterns of disease.3 The European version is particularly associated with neurological manifestations, including facial nerve palsy.1 Because Lyme disease symptoms are non-specific, it may be misdiagnosed as Bell’s palsy, thwarting the opportunity for it to be medically cured.2 In recognition of the severity of Lyme disease, current advice states that ‘if bitten in a Lyme disease endemic area, consult your GP to discuss antibiotic prophylaxis’.4 However, the endemic areas in the UK have not been defined.2,4
This study primarily aims to produce an accurate map of Lyme disease diagnosis in England. Its secondary aim is to identify those patients at risk of developing associated facial nerve palsy, to help in prevention, early diagnosis, and treatment.
METHOD
Hospital episode statistics (HES) data in England from the Health and Social Care Information Centre were interrogated from April 2011 to March 2015 for International Classification of Diseases 10th revision (ICD-10) codes A69.2 (Lyme disease) and G51.0 (Bell’s palsy) in isolation, and as a combination. There is no ICD-10 code for facial palsy. Demographic details recorded were age, sex, home postcode, and socioeconomic group as defined by the English Indices of Deprivation (2004).5 The incidences of Bell’s palsy, Lyme disease, and the combination of the two were reported, and demographic details compared between the three groups. Statistical analysis was performed using the analysis of variance (ANOVA) test on GraphPad Prism (version 6).
RESULTS
Hospital diagnoses of Bell’s palsy and Lyme disease increased between 2011 and 2015 in England. The number of finished consultant (hospital) episodes (FCE) associated with Bell’s palsy increased from 2011 to 2014, and then decreased by 4% to 2015. Lyme disease diagnoses increased from 2011 to 2015, with a dip between 2013 and 2014 of 6%. The two diagnoses occurring together increased from five in 2012 up to 11 in 2014–2015 (Table 1).
Table 1.
Finished hospital consultant episodes associated with Bell’s palsy, Lyme disease, and a combination of the two diagnoses in the population of England from 2011 to 2015
| Year | UK population, million (% increase/year) | Bell’s palsy total FCE activity (% increase/year) | Lyme disease total FCE activity (% increase/year) | Bell’s palsy and Lyme disease (% increase/year) |
|---|---|---|---|---|
| 2011–2012 | 63.3 | 13 114 | 260 | 20 |
| 2012–2013 | 63.7 (0.63) | 13 151 (0.28) | 336 (29.23) | 5 (−75.0) |
| 2013–2014 | 64.1 (0.63) | 14 011 (6.54) | 316 (−5.95) | 11 (120.0) |
| 2014–2015 | 64.5 (0.62) | 13 463 (−3.91) | 370 (17.09) | 11 (0) |
FCE = finished consultant (hospital) episode.
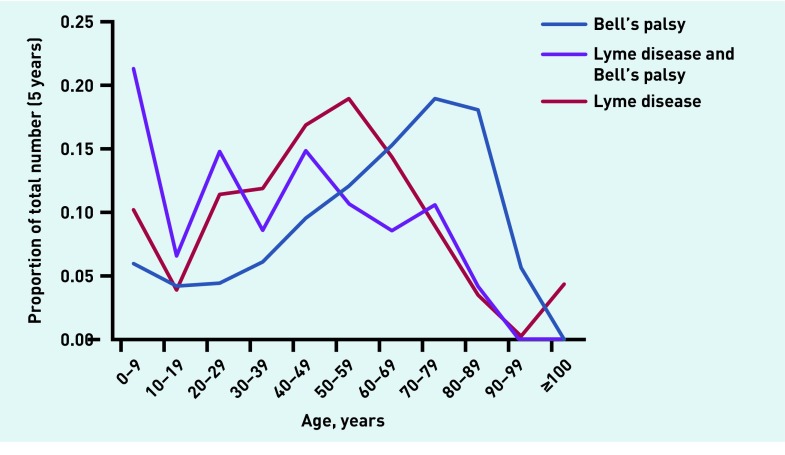
The groups showed similar results regarding patients’ sex. Patients with Lyme disease and facial palsy were a younger group than either the Bell’s palsy or Lyme disease group (41.7 years, compared with 59.6 years for Bell’s palsy and 45.9 years for Lyme disease, ANOVA, P = 0.05, Table 2). Figure 1 demonstrates the trends in age distribution for the three diagnoses.
Table 2.
A comparison of age distribution and sex, from 2011 to 2015
| Bell’s palsy | Lyme disease | Bell’s palsy and Lyme disease combined | P-value (ANOVA) | |
|---|---|---|---|---|
| Mean age, years | 59.6 | 45.9 | 41.7 | 0.05 |
| Female sex, % | 53.5 | 54.3 | 40.4 | >0.99 |
ANOVA = analysis of variance.
Figure 1.
Diagnoses of Bell’s palsy, Lyme disease, and a combination of the two as a proportion of the total found, in 10-year age bands.
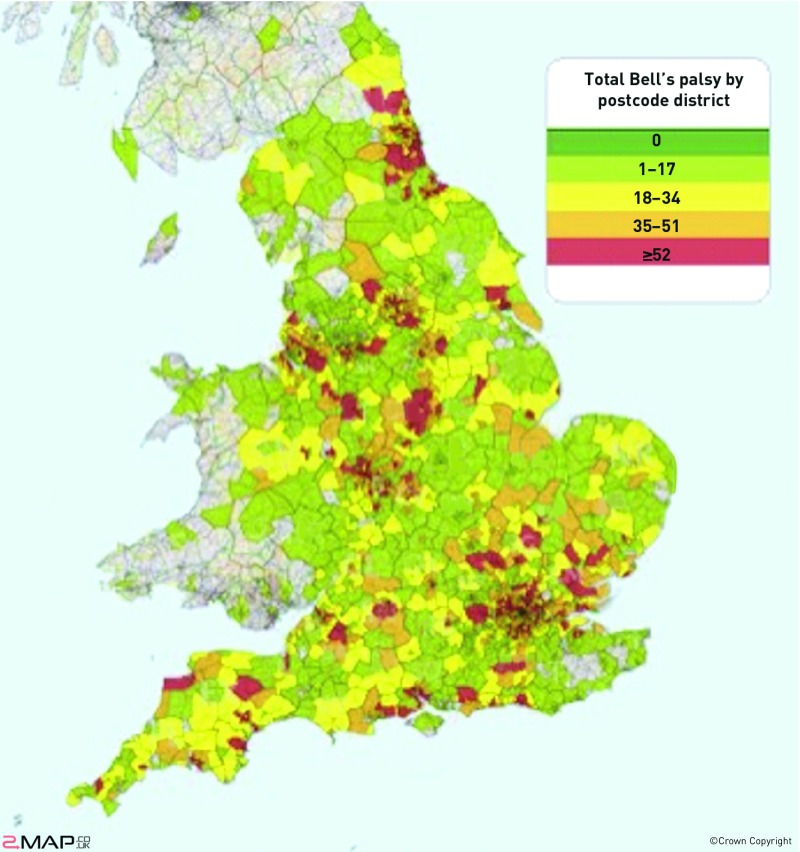
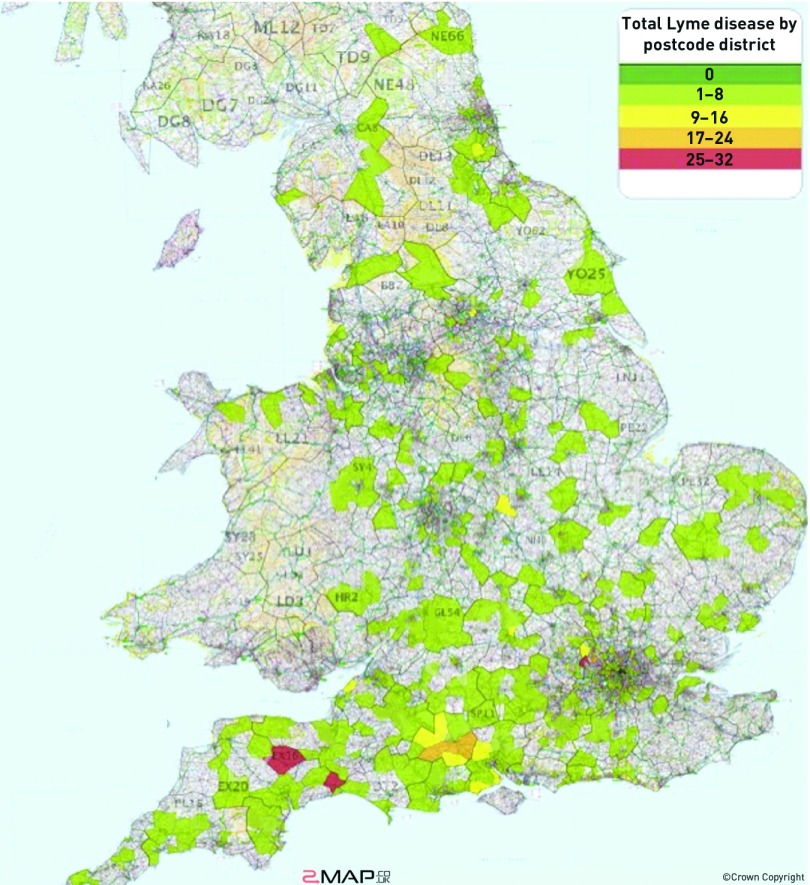
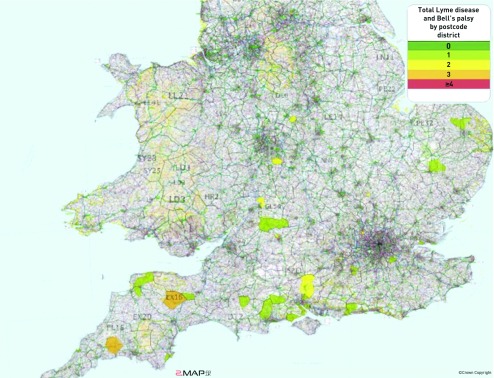
The diagnoses of Bell’s palsy largely centred on urban areas (Figure 2), whereas the majority of diagnoses of Lyme disease were in rural areas (Figure 3). The majority of combined diagnoses were made in the south of England, with clustering around Exmoor and the New Forest (Figure 4).
Figure 2.
The postcode distribution of diagnoses of Bell’s palsy. The map was generated using Hospital Episode Statistics data from the Health and Social Care Information Centre. Grey or green shading is equivalent to 0 cases.
Figure 3.
The postcode distribution of diagnoses of Lyme disease. The map was generated using Hospital Episode Statistics data from the Health and Social Care Information Centre. Grey or green shading is equivalent to 0 cases.
Figure 4.
The postcode distribution of diagnoses of a combination of Bell’s palsy and Lyme disease. Grey or green shading is equivalent to 0 cases.
How this fits in
Lyme disease causes distressing symptoms including facial palsy, which is often misdiagnosed as Bell’s palsy. There has been a call for epidemiological data concerning Lyme disease, which is currently lacking. If identified early, >95% of patients with Lyme disease can expect a cure. A heightened awareness of risk may facilitate appropriate prophylaxis, diagnosis, and treatment. This study found Lyme disease is commoner in certain areas and in the summer months, but increasingly, as the climate changes, also in winter. Testing for Lyme disease in younger patients with Bell’s palsy should be considered.
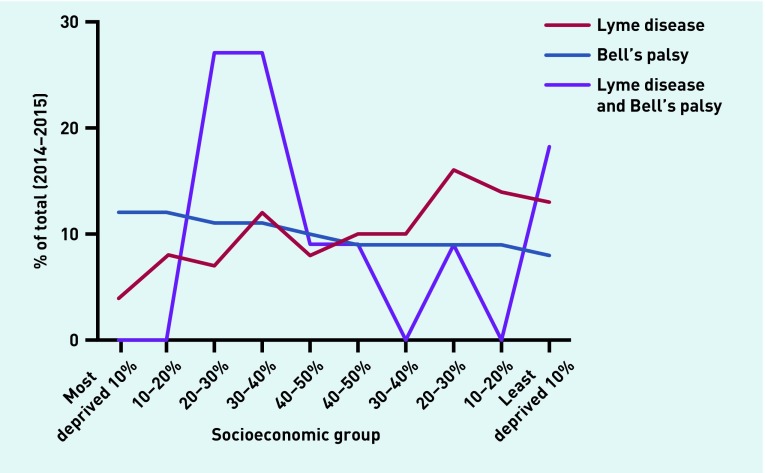
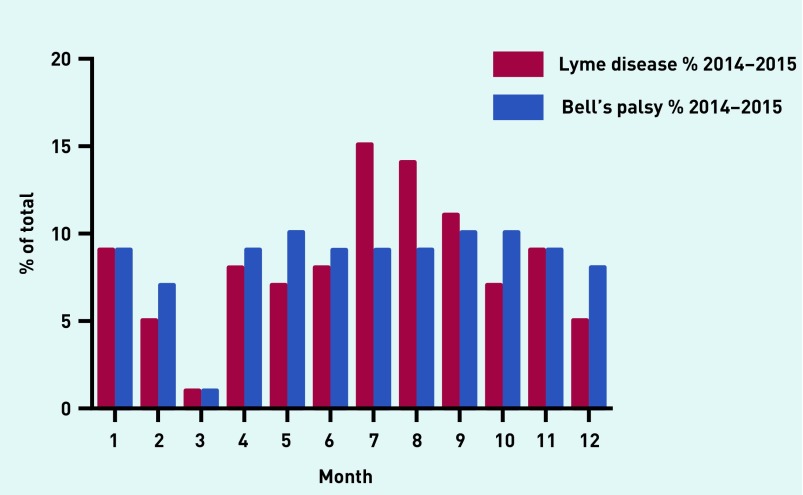
The diagnosis of Lyme disease tended to be in the less deprived half of the population compared with Bell’s palsy (Figure 5). Bell’s palsy diagnoses were spread throughout the year with the exception of March. Lyme disease diagnosis showed a trend towards the summer months (Figure 6).
Figure 5.
A comparison of socioeconomic groups diagnosed with Bell’s palsy and Lyme disease, and a combination of the two (P = 0.97, unpaired t-test).
Figure 6.
Seasonal variation in diagnoses of Bell’s palsy and Lyme disease.
DISCUSSION
Summary
Lyme disease carries significant morbidity, including the potential to develop facial palsy, a potentially devastating condition.6 Although there are areas of the country where Lyme disease is thought to be endemic,7 there is limited knowledge about who gets it, where, and when.2 Awareness of high-risk areas in the UK would allow appropriate preventive and treatment strategies to try to target Lyme disease and associated facial palsy.8 It would also minimise the risk of misdiagnosis and missed opportunities for treatment through inappropriate management as Bell’s palsy.9
Strengths and limitations
HES data provide a national account of FCEs associated with coded diagnoses in England. Whereas previously there was only one primary code per admission, now up to 24 ICD10/20 procedure codes are allowed per FCE. Additionally, patient details, such as age and socioeconomic group (deduced from postcodes), are recorded, which in this context may give clues as to the patient groups most vulnerable to Lyme disease and facial palsy in combination.
Although very helpful, HES data are not designed as a research tool and are therefore limited. It relies on the input of data by non-clinical coders, and the codes themselves have limitations; for example, there is no separate code for facial palsy, only for Bell’s palsy, and the use of this is based on the assumption that borreliosis had not been excluded before it was coded. The geographical data are based on the patient’s postcode rather than their location of disease contraction, and relies on a hospital admission to be eligible. That HES data rely on secondary care episodes may result in patients who do not attend hospital with facial palsy being missed. Finally, patients might be duplicated over the years, because one patient can have several FCEs.
Comparison with existing literature
Cases of Lyme disease have been rising steadily over recent years, as have diagnoses in combination with Bell’s palsy (Table 1). This may be due to better surveillance, increased awareness of the disease, or increasing infection rates caused by travel to endemic areas.1 Classically, Lyme disease is associated with areas of woodland, pasture, and heath, where ticks parasitise small mammals such as field mice and voles, and larger animals such as sheep, deer, and horses.3 The majority of European cases are within the UK, including forested areas such as the New Forest, Exmoor, the South Downs, Thetford Forest in East Anglia, the Lake District, the Yorkshire Moors, and the Scottish Highlands, although there are also cases in the Dordogne and Eastern Europe.1 The maps provided in Figures 2–4 support this finding and add to them (for example, one of the highest areas in England was found in the north west of London in the Chiltern Hills).
Previous studies have shown that approximately 10% of patients with Lyme disease develop facial palsy.6 The authors found that only 3.5% of patients with Lyme disease developed an associated facial palsy from 2011 to 2015, which is less than expected but many more than were seen in the general population. It is possible that some facial palsy diagnoses were not coded if a cause such as Lyme disease was identified, because Bell’s palsy by definition is idiopathic (but there is no separate code for facial palsy). Also, although all of the Bell’s palsies have facial palsy, some of the Bell’s will actually be related to undiagnosed Lyme disease.
Younger patients with Lyme disease were more likely to develop facial palsy in association (P = 0.05, Table 2 and Figure 1), and there was a trend for them to be male: 60% male in this group, compared with 46% for either Lyme disease or Bell’s palsy in isolation. Those diagnosed with Lyme disease tended to be in higher socioeconomic groups, those who developed facial palsy in combination tended to be in lower ones. This younger group developing Bell’s palsy and Lyme disease may represent the typical age of hikers, walkers, and campers. In the context of hospital statistics, it is relevant that the peak age of admission is older than the generally accepted average age of onset of Bell’s palsy (15–40 years),10 probably due to the differential diagnosis of stroke.
In previous reports, tick activity has peaked seasonally, in spring, early summer, and autumn, with a low level of tick activity persisting through winter in areas with a mild climate, such as the New Forest.3 In this study, Figure 6 appears to demonstrate a high level of diagnoses, through winter, which may reflect milder winters with recent climate change.
Implications for research and practice
Bilateral lower motor neurone facial weakness and mononeuritis multiplex ring alarm bells for Lyme disease, but unilateral lower motor neurone facial weakness does not necessarily. It is important, therefore, to consider the clues to the different diagnoses. Bell’s palsy typically presents with an acute onset to a maximum within 72 hours.11 About 50% of patients have a mild-to-moderate post-auricular pain (25% before the weakness, 50% contemporaneous with the weakness, and 25% after the weakness), with altered taste in 35%.11 In 30% a dry eye is noticed, and in 20% a dry mouth, due to parasympathetic involvement.11 Patients with Lyme disease with facial palsy may have noticed a tick bite — a hard-bodied tick attachment with or without engorgement is particularly relevant.9 And 90% will experience a transient rash, erythema migrans, 2–40 days after exposure.9 Approximately 7% will feel generally unwell, and arthralgia has also been reported.3,9,12 Although the diagnosis is clinical, serological testing may be useful, particularly paired blood samples taken at a 4-week interval, to allow for seroconversion.9
If identified early, >95% of patients with Lyme disease can expect a cure.9 Lyme disease is an elusive diagnosis, and a heightened awareness of risk may facilitate appropriate prophylaxis, diagnosis, and treatment. Patients may present with isolated facial palsy, and this is commonly misdiagnosed as Bell’s palsy, as a preceding rash may not have occurred, or may have been missed.3 For example, experienced forestry workers in the New Forest, Hampshire, where the disease is endemic, had a seroprevalence of 25% in a survey published in 1992. None was symptomatic at the time of the survey, and only two of 41 recalled a spreading rash or other clinical finding compatible with a diagnosis of Lyme disease.13 It is therefore likely that Lyme disease is even more prevalent than we are aware of and the reported recent increase in cases vastly under-reports the reality.4
Methods of controlling tick populations have been studied, but results so far suggest that they are unlikely to make a substantial impact in Britain.3 Therefore, it is only through recognition of the high-risk areas, public health and healthcare practitioner education about these areas and higher risk groups, and behavioural and antibiotic prophylactic intervention that we could decrease the likelihood of developing Lyme disease and associated facial palsy.8 Clearly, blanket treatment of unilateral facial palsy with treatment for Lyme disease carries risk also, so clinical judgement is required.
Healthcare practitioners should have a high index of suspicion for Lyme disease following travel in the areas mapped in Figures 2–4, particularly in the summer months, but increasingly also in winter as the climate changes. Consider testing for Lyme disease in younger patients with Bell’s palsy. Public health measures to reduce tick bites may further help to prevent the contraction of Lyme disease and the development of facial palsy.
Funding
None.
Ethical approval
Not applicable.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Hobson J, Weatherall M. Lyme neuroborreliosis. BMJ. 2012;344:e3250. doi: 10.1136/bmj.e3250. [DOI] [PubMed] [Google Scholar]
- 2.Pearson S. Doctors need accredited information on Lyme borreliosis. BMJ. 2012;345:e4727. doi: 10.1136/bmj.e4727. [DOI] [PubMed] [Google Scholar]
- 3.O’Connell S. Lyme disease in the United Kingdom. BMJ. 1995;310:303–308. doi: 10.1136/bmj.310.6975.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans R, Mavin S, Holden S, et al. Lack of accurate information on the prevalence of Lyme disease in the UK. BMJ. 2014;348:g2037. doi: 10.1136/bmj.g2037. [DOI] [PubMed] [Google Scholar]
- 5.Office of the Deputy Prime Minister. The English indices of deprivation. London: Queen’s Printer and Controller of Her Majesty’s Stationery Office; 2004. [Google Scholar]
- 6.Masterson L, Vallis M, Quinlivan R, Prinsley P. Assessment and management of facial nerve palsy. BMJ. 2015;351:h3725. doi: 10.1136/bmj.h3725. [DOI] [PubMed] [Google Scholar]
- 7.O’Connell S, Sorouri-Zanjani R, White J, Guy E. Lyme disease: experience in an endemic area. Br J Dermatol. 1992;127(Suppl 40):21. [Google Scholar]
- 8.Due C, Fox W, Medlock J, et al. Tick bite prevention and tick removal. BMJ. 2013;347:f7123. doi: 10.1136/bmj.f7123. [DOI] [PubMed] [Google Scholar]
- 9.Duncan C, Carle G, Seaton R. Tick bite and early Lyme borreliosis. BMJ. 2012;344:e3124. doi: 10.1136/bmj.e3124. [DOI] [PubMed] [Google Scholar]
- 10.Holland N, Bernstein J. Bell’s palsy. Systematic review 1204. BMJ Clin Evid. 2014;2014:1204. [PMC free article] [PubMed] [Google Scholar]
- 11.Fuller G, Morgan C. Bell’s palsy syndrome: mimics and chameleons. Pract Neurol. 2016 doi: 10.1136/practneurol-2016-001383. [DOI] [PubMed] [Google Scholar]
- 12.Holland N, Weiner GM. Recent developments in Bell’s palsy. BMJ. 2004;329:553–557. doi: 10.1136/bmj.329.7465.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guy EC, Martyn CN, Bateman DE, et al. Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers. Lancet. 1989;1(8636):484–486. doi: 10.1016/s0140-6736(89)91377-9. [DOI] [PubMed] [Google Scholar]