Abstract
Importance
Despite a large rural US population, there are potential differences between rural and urban regions in the processes and outcomes following trauma.
Objectives
To describe and evaluate rural vs urban processes of care, injury severity, and mortality among injured patients served by 9-1-1 emergency medical services (EMS).
Design, Setting, and Participants
This was a preplanned secondary analysis of a prospective cohort enrolled from January 1 through December 31, 2011, and followed up through hospitalization. The study included 44 EMS agencies transporting to 28 hospitals in 2 rural and 5 urban counties in Oregon and Washington. A population-based, consecutive sample of 67047 injured children and adults served by EMS (1971 rural and 65 076 urban) was enrolled. Among the 53 487 patients transported by EMS, a stratified probability sample of 17 633 patients (1438 rural and 16 195 urban) was created to track hospital outcomes (78.9% with in-hospital follow-up). Data analysis was performed from June 12, 2015, to May 20, 2016.
Exposures
Rural was defined at the county level by 60 minutes or more driving proximity to the nearest level I or II trauma center and/or rural designation in the Centers for Medicare & Medicaid Services ambulance fee schedule by zip code.
Main outcomes and Measures
Mortality (out-of-hospital and in-hospital), need for early critical resources, and transfer rates.
Results
Of the 53 487 injured patients transported by EMS (17 633 patients in the probability sample), 27 535 were women (51.5%); mean (SD) age was 51.6 (26.1) years. Rural vs urban sensitivity of field triage for identifying patients requiring early critical resources was 65.2% vs 80.5%, and only 29.4% of rural patients needing critical resources were initially transported to major trauma centers vs 88.7% of urban patients. After accounting for transfers, 39.8% of rural patients requiring critical resources were cared for in major trauma centers vs 88.7% of urban patients. Overall mortality did not differ between rural and urban regions (1.44% vs 0.89%; P = .09); however, 89.6% of rural deaths occurred within 24 hours compared with 64% of urban deaths. Rural regions had higher transfer rates (3.2% vs 2.7%) and longer transfer distances (median, 97.4 km; interquartile range [IQR], 51.7-394.5 km; range, 47.8-398.6 km vs 22.5 km; IQR, 11.6-24.6 km; range, 3.5-97.4 km).
Conclusions and Relevance
Most high-risk trauma patients injured in rural areas were cared for outside of major trauma centers and most rural trauma deaths occurred early, although overall mortality did not differ between regions. There are opportunities for improved timeliness and access to major trauma care among patients injured in rural regions.
Multiple studies1-5 have demonstrated higher mortality rates and a greater proportion of deaths following injury in rural compared with urban areas, although 1 study6 found no difference. Even after implementation of a statewide trauma system that reduced mortality in urban areas,7,8 improved the concentration of seriously injured patients in major trauma centers,7,9 and enhanced the processes of rural trauma care,10 mortality from trauma in rural regions did not change.11 Differences in emergency medical services (EMS) systems, injury severity, access to major trauma care, and delays in care have all been cited1-4,11-13 as potential factors explaining this discrepancy in outcomes. Other studies14,15 have demonstrated major differences in geospatial proximity to major trauma centers in the United States. However, prospective research addressing disparities in the process and outcome of patients injured in rural areas remains sparse, and much of the existing literature is based on data obtained more than 20 years ago.
A prospective validation study16 of the national field triage guidelines that included patients injured in urban and rural settings was recently published. This study demonstrated that, although field triage sensitivity for identifying patients with serious injuries (Injury Severity Score17 [ISS] ≥16; range, 0-75, with higher numbers indicating greater injury severity) appeared to be better in rural vs urban regions (81% vs 65.8%), only 12.5% of seriously injured rural patients were initially transported to major trauma centers and only 39.3% were ultimately cared for in major trauma centers.16 However, the primary results of this study did not allow a detailed assessment of rural vs urban differences in trauma care.
We conducted a preplanned secondary analysis of the prospective injury cohort of that study16 to detail rural vs urban differences in field triage, processes of trauma care, injury severity, and mortality. We sought to use these data as an opportunity to address ongoing questions about differences in process and outcomes between urban and rural trauma patients.
Methods
Study Design
This was a preplanned secondary analysis of a prospective, consecutive patient cohort in 7 counties in Oregon and Washington. The study, as well as the secondary analysis, was reviewed and approved by institutional review boards in all study sites (eAppendix in the Supplement) with waiver of informed consent.
Study Setting
The study included 44 EMS agencies transporting to 28 hospitals in 2 rural and 5 urban counties in Oregon and Washington from January 1 through December 31, 2011. Rural vs urban status was determined at the county level, with rural counties defined using the following EMS and trauma system factors: 60 minutes or more driving proximity to the nearest level I or II trauma center and/or rural designation in the Centers for Medicare & Medicaid Services Ambulance Fee Schedule by zip code.18 The additional 5 counties included urban and suburban areas within a 30-minute driving proximity to a level I or II trauma center and were considered urban for the purposes of this analysis. The methods of the parent study have been described in detail elsewhere.16 In Table 1, we report and characterize the counties, EMS structures, population served, and driving proximity to surrounding hospitals.
Table 1. Description of Urban and Rural Counties.
| County, State | 2010 Population, No.a | Persons per Square Kilometer, No. | EMS System | Level I Hospitalb | Level II Hospitalb | Any Acute Care Hospitalb | |||
|---|---|---|---|---|---|---|---|---|---|
| Distance, km | Driving Time Without/With Traffic, min | Distance, km | Driving Time Without/With Traffic, min | Distance, km | Driving Time Without/With Traffic, min | ||||
| Urban | |||||||||
| Multnomah, Oregon | 735 334 | 655 | Dual ALS response | 9.2 | 16/26 | NAc | NAc | 2.7 | 7/9 |
| Washington, Oregon | 529 710 | 281 | Dual ALS response | 17.2 | 24/45 | NAc | NAc | 10.0 | 14/22 |
| Clackamas, Oregon | 375 992 | 77 | Dual ALS response | 24.3 | 26/40 | NAc | NAc | 2.6 | 4/4 |
| King, Washington | 1 931 249 | 351 | Tiered BLS-ALS response | 14.2 | 18/26 | NAc | NAc | 13.5 | 16/26 |
| Clark, Washington | 425 363 | 260 | Dual ALS response | 24.3 | 24/40 | 7.9 | 12/16 | 7.9d | 12/16d |
| Rural | |||||||||
| Josephine, Oregon | 82 713 | 19 | Dual response: BLS/ALS | 398.8 | 230/270 | 230.6 | 140/170 | 5.1 | 6/6 |
| Skamania, Washington | 11 066 | 3 | Single-agency ALS response | 76.4 | 55/70 | 66.3 | 55/55 | 38.3 | 35/35 |
Abbreviations: ALS, advanced life support; BLS, basic life support; EMS, emergency medical services; NA, not applicable.
Population and geographic values based on 2010 US Census19 data for these regions.
Transport driving distances calculated for ground transport from the county-based centroid (geographic center based on population density using ArcGIS geospatial mapping) to each level of hospital; all distances rechecked using Google Maps from the same coordinates. Driving times were estimated using Google Maps for travel during typical times with light (11:30 pm) and with heavy (5 pm) traffic based on the ArcGIS coordinates.
Level I trauma center closer than the nearest level II trauma center.
Closest hospital is the level II trauma center.
Participating hospitals differed in type and resource capability and included 5 level I trauma hospitals (including 2 children's hospitals), 2 level II trauma hospitals, 5 level III trauma hospitals, 5 level IV trauma hospitals, and 11 nontrauma hospitals. Trauma centers in these regions are designated by state authorities or verified by the American College of Surgeons Committee on Trauma.20 We defined major trauma centers as all level I and II trauma hospitals. The 44 EMS agencies work under close medical direction, use standardized field trauma triage protocols, and retrain on field triage when there are revisions to the triage algorithm. During the study period, field triage protocols in all counties were based on the 2006 national field triage guidelines.21 For patients with closer proximity to a level III or IV hospital, state trauma guidelines allow EMS transport to such hospitals for initial evaluation and stabilization before potential inter hospital transfer to a higher-level trauma center.
Patient Population and Selection
We included all injured children and adults for whom the 9-1-1 EMS system was activated within the 7 counties. This sampling design provided a population-based, out-of-hospital injury cohort defined through the lens of the EMS provider, representing the full denominator of injured patients served by EMS. To create a representative primary sample feasible for medical record abstraction at the 28 hospitals, we used a probability sampling design based on the following strata: geographic region, triage status, age group, and type of receiving hospital (eFigure 1 in the Supplement).16
Variables and Outcomes
Out-of-hospital variables were collected directly from EMS electronic patient care reports and mapped to standardized National Emergency Medical Services Information System definitions.22 These variables included field triage status, individual triage criteria used by EMS, patient demographics, out-of-hospital time intervals, initial out-of-hospital physiologic status (Glasgow Coma Scale,23 systolic blood pressure, respiratory rate, and heart rate), procedures, mechanism of injury, transport mode, initial receiving hospital, and reason for selecting the hospital destination. We triangulated EMS records, trauma registry records, and base hospital telephone records to minimize misclassification bias for field triage status24,25 and matched EMS records from multiple agencies at the patient level to provide complete field-based information. The electronic EMS data collection processes used for this study have previously been validated.26
Among patients sampled for hospital record abstraction, we collected emergency department (ED) and hospital variables using trained data abstractors (including one of us, S.S.) and a standardized data collection form. Variables included airway management, mechanical ventilation, surgical procedures, blood product transfusion, intensive care unit stay, complications, interhospital transfer, Abbreviated Injury Scale scores (0-6 for separate body regions, with 0 indicating no injury and 6 representing a nonsurvivable injury),27 ISS,17 and in-hospital mortality. For patients transferred between hospitals, records at both facilities were abstracted. To supplement the abstracted hospital data, records from 9 trauma registries were matched to the sample. We double-abstracted a portion of hospital records to ensure reliable and consistent record abstraction.16
We defined early critical resource use as a composite measure of any of the following variables within 24 hours of ED arrival: emergent intubation in the ED, major nonorthopedic surgical intervention [brain, spine, neck, thorax, abdominal-pelvic, or vascular surgery], interventional radiologic procedures, packed red blood cell transfusion of 6 U or more in an adult, or any blood transfusion in a child, or death. This definition was based on previous trauma triage research,28-33 a national consensus study34 defining trauma center need, and a 5-member advisory committee of content experts (including two of us, J.R.H. and N.C.M.) used for the parent study.16
Statistical Analysis
The sample size for the parent study (n = 17 633) was determined based on the desired precision around estimates for overall triage sensitivity.16 To maximize the use of available information for the present study, we used the full EMS sample (n = 67047, including 53 487 patients transported by EMS to acute care hospitals) to characterize out-of-hospital care and the probability sample (n = 17633, weighted to represent the 53487 patients transported by EMS)to describe ED and in-hospital care. The in-hospital follow-up rate of the probability sample was 78.9%. We incorporated sampling strata and probability weights in all analyses involving the probability sample to account for sampling design.
We used descriptive statistics to characterize processes of care, injury severity, and injury patterns between patients injured in rural and urban regions. To address potential mortality differences, unadjusted and adjusted analyses were used. For unadjusted analyses, mortality estimates were combined across the out-of-hospital, ED, and in-hospital phases of care. For adjusted analyses, we developed a multivariable logistic regression model based on common predictors and confounders used in risk-adjustment models for trauma. The role of time was tested using survival analysis and hazard ratios (HRs) in a Cox proportional hazards regression model. For all comparisons, rural vs urban designation was based on the region in which the patient was initially served by EMS.
To minimize bias and preserve study power, we used multiple imputation to handle missing values,35,36 the validity and rigor of which have been demonstrated for trauma and EMS data.24,37,38 Flexible chains regression models were used for multiple imputation39 with generation of 10 multiply imputed data sets (IVEware, version 0.1; Institute for Social Research, University of Michigan). All estimates and 95% CIs were generated using Rubin's36 rules to appropriately account for variance within and between data sets.
Geospatial analysis (ArcGIS, version 10.2.1; Esri) was used to evaluate hospital proximity and interhospital distances. We first identified each county's population centroid, representing the population-weighted geospatial center of the county and geospatial mean for EMS incident location. Road networks were then created in ArcGIS from street map shape files, and hospital locations were added to calculate driving distances from the county centroid to the nearest hospital and major trauma center, as well as the shortest driving distance between hospitals. Because driving times were not available in public use geospatial files and ArcGIS underestimates drive times,40 we used Google Maps (Google Inc) to estimate typical drive times for time periods with heavy (5 pm) and light (11:30 pm) traffic. All data-base management and statistical models were conducted using SAS, version 9.3 (SAS Institute Inc). Data analysis was performed from June 12, 2015, to May 20, 2016.
Results
Among the 67047 injured patients evaluated by EMS during the 12-month study period, 1971 patients (2.9%) were injured in rural counties and 65 076 individuals (97.1%) were injured in urban counties. Characteristics for patients in both regions are demonstrated in Table 2. Among the 53 487 patients (79.8%) transported by EMS, 27535 were women (51.5%); mean (SD) age was 51.6 (26.1) years. Those injured in rural counties tended to be older, female, and injured by falls, but had physiological status similar to that of patients injured in urban counties. The EMS response and transport intervals were longer in rural counties, but the on-scene interval was similar to that of urban counties. Most patients in rural areas were initially transported to non–level I or II hospitals, with hospital proximity cited as the most common reason for hospital selection by EMS. The use of individual triage criteria also differed by region (eFigure 2 in the Supplement).
Table 2. Characteristics of 67 047 Injured Patients Evaluated by Emergency Medical Services in Rural vs Urban Counties.
| Characteristic | No. (%) | P Value | |
|---|---|---|---|
| Rural | Urban | ||
| All patients evaluated by EMS | 1971 | 65 076 | |
| Death in the field | 15 (0.8) | 143 (0.2) | <.001 |
| Not transported | 507 (25.7) | 12 312 (18.9) | |
| Transported by ground | 1412 (71.6) | 51 970 (79.9) | |
| Transported by air | 26 (1.3) | 79 (0.1) | |
| Transported to nonhospital setting | 0 | 354 (0.5) | |
| Taken into police custody | 11 (0.6) | 218 (0.3) | |
| Patients transported by EMS to acute care hospitalsa | 1438 | 52 049 | |
| Age, y | |||
| 0-14 | 73 (5.1) | 3427 (6.6) | <.001 |
| 15-54 | 518 (36) | 25 222 (48.5) | |
| ≥55 | 847 (58.9) | 23 401 (45) | |
| Women | 803 (55.8) | 26 732 (51.4) | <.001 |
| Met ≥1 field triage criteria | 306 (21.3) | 6943 (13.3) | <.001 |
| Mechanism of injury | |||
| Gunshot wound | 9 (0.6) | 321 (0.6) | .002 |
| Stabbing | 17 (1.2) | 1447 (2.8) | |
| Assault | 42 (2.9) | 2998 (5.8) | |
| Fall | 796 (55.3) | 26 298 (50.5) | |
| Motor vehicle crash | 258 (17.9) | 11 257 (21.6) | |
| Motor vehicle vs pedestrian | 12 (0.9) | 642 (1.2) | |
| Other | 305 (21.2) | 9086 (17.5) | |
| Out-of-hospital time interval, min | |||
| Response interval, mean (SD) | 10.1 (8.1) | 6.3 (5.3) | <.001 |
| 90th Percentile response interval | 20 | 11 | |
| On-scene interval, mean (SD) | 19.3 (11.5) | 19.4 (12.6) | .90 |
| 90th Percentile on-scene interval | 31 | 31 | |
| Transport interval, mean (SD) | 16.8 (15.1) | 15.3 (11) | <.001 |
| 90th Percentile transport interval | 37.1 | 27.6 | |
| Out-of-hospital physiological status | |||
| SBP <90mmHg | 19 (1.3) | 744 (1.4) | .71 |
| GCS ≤8 | 13 (0.9) | 525 (1) | .83 |
| GCS 9-12 | 39 (2.7) | 1284 (2.5) | |
| GCS 13-15 | 1386 (96.4) | 50 240 (96.5) | |
| Respiratory rate <10 or >29 breaths/min | 29 (2) | 1167 (2.2) | .63 |
| Heart rate <60 or >110 beats/min | 151 (10.5) | 6927 (13.3) | .002 |
| Out-of-hospital procedures | |||
| Assisted ventilation, bag-valve mask ventilation, intubation, supraglottic airway placement, cricothyrotomy | 13 (0.9) | 622 (1.2) | .31 |
| Intravenous or intraosseus line placement | 656 (45.6) | 10 340 (19.9) | <.001 |
| Out-of-hospital transport patterns | |||
| Level I | 20 (1.4) | 12 607 (24.2) | <.001 |
| Level II | 76 (5.3) | 3724 (7.2) | |
| Nontrauma centerb | 1342 (93.3) | 35 718 (68.6) | |
| EMS reason for selecting hospital destination | |||
| Specialty center | 22 (1.5) | 4405 (8.5) | <.001 |
| Proximity | 1173 (81.6) | 6320 (12.1) | |
| Ambulance diversion | 8 (0.6) | 839 (1.6) | |
| Patient/family request | 174 (12.1) | 34 952 (67.2) | |
| Other | 60 (4.2) | 5533 (10.6) | |
Abbreviations: EMS, emergency medical services;GCS, Glasgow Coma Scale; SBP, systolic blood pressure.
For consistency and clarity, all values below this row in the table are based on the denominator of patients transported by EMS to an acute care hospital (ie, nontransported patients do not have many of the time and transport measures presented).
Nontrauma centers included level III and IV trauma hospitals.
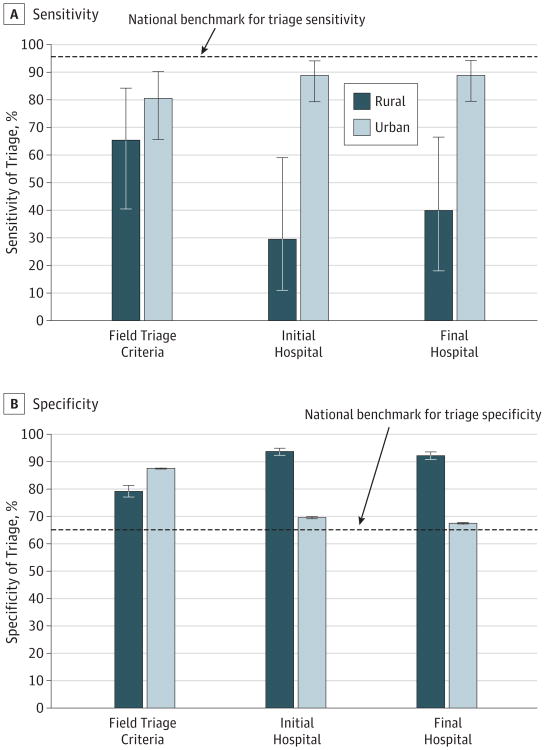
We calculated the sensitivity and specificity of triage for identifying patients requiring early critical resources across 3 phases (field identification, initial hospital selection, and final hospital destination) separated by rural vs urban location (Figure 1). The sensitivity of identifying trauma patients by EMS at the scene of injury who ultimately required early critical resources was 65.2% vs 80.5% for rural and urban regions, respectively. However, few of these high-risk patients in rural regions were transported directly to major trauma centers (29.4% vs 88.7%). Even after accounting for subsequent interhospital transfers, most rural trauma patients requiring early resources were cared for outside of major trauma centers (39.8% vs 88.7%).
Figure 1. Diagnostic Accuracy of the Triage Process (Field Identification, Initial Hospital Selection, Final Hospital Destination) for Identifying Trauma Patients Requiring Early Critical Resources in Rural (n = 1438) vs Urban (n =16195) Regions, Sensitivity (A) and specificity (B) results shown.
Triage sensitivity estimates for patients with an Injury Severity Score of 16 or higher (indicating serious injuries; range, 0-75, with higher numbers indicating greater injury severity) injured in rural regions were included in the parent study publication.16 Early critical resource need was defined as any of the following within 24 hours of arrival at the emergency department: emergent intubation in the emergency department, major nonorthopedic surgery (brain, spine, neck, thorax, abdominal-pelvic, or vascular surgery), interventional radiologic procedures, packed red blood cell transfusion of 6 U or more or any transfusion in a child, or death. Error bars indicate 95% CI.
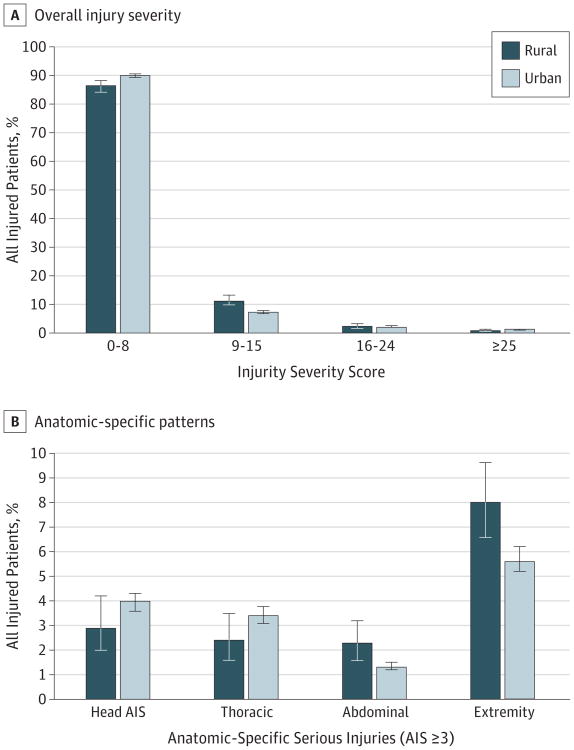
Figure 2 illustrates injury severity between rural and urban patients. Rural patients had fewer minor injuries (ISS 0-8: 86.3% vs 89.9%) and more moderate injuries (ISS 9-15: 11.0% vs 7.1%), yet the distribution of patients with more severe injuries was similar. The proportion of patients with serious head and thoracic injuries was similar, but serious abdominal (2.3% vs1.3%) and extremity (8.0% vs5.6%) injuries were more common in rural areas.
Figure 2. Injury Patterns Among Patients Transported by Emergency Medical Services From Rural (n = 1438) vs Urban (n = 16195) Regions.
A, Overall injury severity by Injury Severity Score. B, Anatomic-specific injury patterns by Abbreviated Injury Scale (AIS) score. Error bars indicate 95% CI.
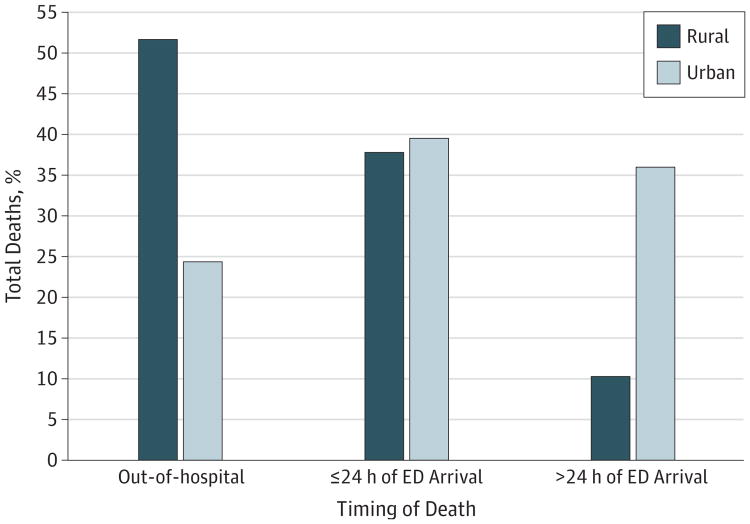
We evaluated mortality and resource utilization across multiple time points following initial contact with 9-1-1 EMS. Overall mortality, combined across the out-of-hospital, ED, and in-hospital phases of care, did not differ between rural and urban regions (1.44% vs 0.89%; P = .09). However, a greater proportion of rural deaths occurred shortly after injury, with 90% of rural deaths occurring within 24 hours compared with 64% of urban deaths (Figure 3). Among the 29 deaths in rural regions, there were 15 out-of-hospital (51.7%), 11 within 24 hours or less (37.9%), and 3 after 24 hours (10.3%). Among the 583 deaths in urban regions, 143 (24.5%) occurred out-of-hospital, 230 (39.5%) were within 24 hours or less, and 210 (36%) more than 24 hours (absolute numbers of deaths reflect entire sample of 67 047 injured patients evaluated by EMS). Among patients transported to a hospital, mortality was higher among rural patients in the first 24 hours (rural, 0.65%; 95% CI, 0.17%-1.13% vs urban, 0.13%; 95% CI, 0.09%-0.16%), yet this difference disappeared when calculated across the entire hospital stay (rural, 0.74%; 95% CI, 0.23%-1.26% vs urban, 0.74%; 95% CI, 0.60%-0.89%). There were no rural vs urban mortality differences in survival analyses (HR, 0.83; 95% CI, 0.65%-2.21%) and after accounting for important con-founders (adjusted odds ratio, 0.65; 95% CI, 0.25-1.64) (eTable 1 in the Supplement). Rural and urban comparison of resource utilization suggested that rates for certain procedures (eg, thoracotomy, abdominal surgery, and craniotomy) were less among rural patients, but 95% CIs were wide and most comparisons did not reach statistical separation (eTable 2 in the Supplement). For example, use of craniotomy or ventriculostomy within the first 24 hours by rural vs urban region was 0.09% (95% CI, 0%-0.28%) vs 0.18% (95% CI, 0.14%-0.22%). Composite early critical resource use was similar at 24 hours (1.40% vs 1.98%) and across hospitalization (3.16% vs 3.35%) (eTable 2 in the Supplement). Rates of do-not-resuscitate order use did not differ substantively by rural (0.21%; 95% CI, 0.03%-1.14%) vs urban (0.80%; 95% CI, 0.44%-1.43%) location.
Figure 3. Decedent Analysis Comparing the Timing of Rural Deaths vs Urban Deaths Among Injured Patients Served by Emergency Medical Services (EMS).
Proportions were calculated based on the denominator of total deaths in each region (eg, all rural proportions add to 100%). The absolute number of deaths was calculated based on the full sample of injured patients served by EMS in these regions during the study period (n = 67 047). Among patients injured in rural regions, there were 29 deaths (15 [51.7%] out-of-hospital, 11 [37.9%] at ≤24 hours, and 3 [10.3%] at >24 hours). Among patients injured in urban regions, there were 583 deaths (143 [24.5%] out-of-hospital, 230 [39.5%] at ≤24 hours, and 210 [36%] at >24 hours). The overall mortality comparison demonstrated rural mortality of 1.44% (95% CI, 0.96-2.15) vs urban mortality of 0.89% (95% CI, 0.68-1.17; P = .09 for comparison). ED indicates emergency department.
Of the 53 487 patients transported by EMS, 2.7% (weighted n = 1447) patients were transferred between hospitals following EMS transport, including 3.2% of rural patients (weighted n = 46 of 1438 transported patients) and 2.7% of urban patients (weighted n = 1401 of 52 049 transported patients). Among the 28 hospitals, there were 67 different unique hospital combinations used for interhospital transfers. All transfers from rural regions involved higher-level facilities (38.1% to level I hospitals, 14.3% to level II hospitals, and 47.6% to level III hospitals). Among urban transfers, 82.4% were for higher-level care, 8.0% were lateral transfers, and 9.6% were lower-level transfers. The median transfer distance for rural patients was 97.4 km (IQR, 51.7-394.5 km; range, 47.8-398.6 km), compared with 22.5 km (IQR, 11.6-24.6 km; range, 3.5-97.4 km) for urban patients.
Discussion
In this study, we compared trauma processes and outcomes for injured patients servedby9-1-1 EMS in rural and urban regions. Our study differs from previous research by using a prospective cohort served by EMS and evaluating patients across multiple phases of care to address lingering questions about rural trauma care. Although overall mortality did not differ between regions, the timing of death was different, with most rural deaths occurring shortly after injury. Also, most high-risk patients injured in rural regions were cared for outside of major trauma centers. Our findings have important public health, operational, and health policy implications.
Similar to previous research,2,4,12,13 we demonstrate that most rural trauma deaths occur early after an injury event, often outside the hospital, which differs from urban areas. However, the overall mortality rate did not differ between regions, a finding that contrasts with those of several prior studies.1,3,5 The lack of a statistically significant difference in mortality may reflect a rural sample size that was underpowered to detect such a difference or inherent characteristics of the rural counties included in our sample. It is also possible that the efficiency and resources available in urban areas delay the inevitable outcome of patients with nonsurvivable injuries. Our data do not provide a definitive answer to these possibilities. Previous studies1,2,12 have attributed a higher mortality rate in rural areas to prolonged discovery times, delays in out-of-hospital care, more severe injuries, limited access to major trauma centers, and delays in the receipt of definitive care. Of these possibilities, our data confirm longer EMS response intervals and notably less access to major trauma care. Injury severity between regions was not substantively different. Although serious abdominal and extremity injuries were more common in rural counties, out-of-hospital physiological status was similar and early resuscitation practices did not markedly differ between rural and urban regions. Because time of injury was unavailable, we could not evaluate discovery time, which remains a potentially important determinant in early rural mortality.
Regarding access to major trauma care, most high-risk patients injured in rural regions were cared for outside of major trauma centers. Although the field identification step was similar between regions, there were major differences in where high-risk trauma patients received care. Most high-risk rural patients were initially transported to non–level I or II hospitals, regardless of triage status, reflecting hospital proximity. Even after accounting for interhospital transfers, most high-risk patients remained outside of major trauma centers. The high rate of unnecessary interhospital transfers in rural trauma systems suggested in previous research41 was not supported by our data. Rather, rural hospitals in our sample tended not to transfer patients who were most likely to benefit from care in major trauma centers, suggesting that secondary triage (hospital-based) and transfer processes are being underused. Improved trauma transfer practices offer the opportunity to reduce variability in transfer processes41-43 and potentially enhance early survival among patients injured in rural settings.44
There were limitations in this study. We used an EMS-based definition for rural applied at the county level. However, a national reference45 defines rural based on different factors, categorizing the 2 rural counties in the present study as small metropolitan and largefringe metropolitan. It is possible that these counties may not have been remote enough to demonstrate the mortality differences shown in previous research. In addition, these rural regions provide advanced life support care by EMS agencies and function as part of mature inclusive trauma systems. Therefore, these areas may not be generalizable to other rural regions.
Our sample was based on injured patients accessing 9-1-1 EMS. Although most patients with serious injuries use such services, patients presenting to hospitals outside of the 9-1-1 system and deaths in the field without an EMS response were not captured in our sample. In addition, the rural sample size and total number of rural deaths were modest, which reduced our ability to make definitive statistical comparisons and to evaluate important subgroups of patients (eg, those with serious injuries [ISS ≥16] and/or traumatic brain injury). The study was not designed to detect mortality differences between regions; it is possible that a larger sample size would have demonstrated statistically significant differences in mortality between regions. Finally, in our stratified probability sampling, we assumed that patient characteristics and outcomes at participating and nonparticipating hospitals were similar.
Conclusions
This study identified major differences in the processes of trauma care and sequence of events following injury in rural vs urban regions. Although the ability to identify high-risk patients by rural EMS providers was similar to urban regions, there were major discrepancies in the location of hospital care. Most rural trauma deaths occurred early after injury, although overall mortality did not differ between regions. Enhancing early rural trauma transfer practices may reduce disparities in access to major trauma care and potentially improve early survival among patients injured in rural areas.
Supplementary Material
Key Points.
Question
What are process and outcome differences among patients injured in rural vs urban areas?
Findings
In this preplanned, secondary analysis of a prospective cohort comparing 1971 rural patients and 65 076 urban patients using 9-1-1 emergency medical services following injury, most rural trauma deaths occurred within 24 hours. In addition, most high-risk rural patients were cared for outside of major trauma centers.
Meaning
Patients injured in rural areas have less access to major trauma care and deaths tend to occur early, suggesting that there are opportunities to optimize rural trauma care.
Acknowledgments
Funding/Support: This project was supported by grant R01CE001837 from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We acknowledge and thank all the participating emergency medical services (EMS) agencies, EMS medical directors, hospitals, trauma centers, and trauma registrars that supported and helped provide data for this project. We also acknowledge the guidance and oversight by study advisory committee members who are not coauthors of this article: Nathan Kuppermann, MD, MPH (University of California, Davis); E. Brooke Lerner, PhD (Medical College of Wisconsin); and Gregory J. Jurkovich, MD (University of Colorado during the study; currently, University of California, Davis). Members of the study advisory committee received financial compensation.
Footnotes
Author Contributions: Drs Newgard and Fu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Newgard, Hedges, Hansen.
Acquisition, analysis, or interpretation of data: Newgard, Fu, Bulger, Hedges, Mann, Wright, Lehrfeld, Shields, Hoskins, Wittwer, Cook, Verkest, Conway, Somerville, Hansen.
Drafting of the manuscript: Newgard, Fu.
Critical revision of the manuscript for important intellectual content: Bulger, Hedges, Mann, Wright, Lehrfeld, Shields, Hoskins, Warden, Wittwer, Cook, Verkest, Conway, Somerville, Hansen.
Statistical analysis: Newgard, Fu, Hansen.
Administrative, technical, or material support: Newgard, Bulger, Hedges, Lehrfeld, Shields, Wittwer.
Study supervision: Newgard, Bulger, Hedges, Hansen.
Conflict of Interest Disclosures: None reported.
References
- 1.Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. Am J Public Health. 2004;94(10):1689–1693. doi: 10.2105/ajph.94.10.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomez D, Berube M, Xiong W, et al. Identifying targets for potential interventions to reduce rural trauma deaths: a population-based analysis. J Trauma. 2010;69(3):633–639. doi: 10.1097/TA.0b013e3181b8ef81. [DOI] [PubMed] [Google Scholar]
- 3.Fatovich DM, Phillips M, Langford SA, Jacobs IG. A comparison of metropolitan vs rural major trauma in Western Australia. Resuscitation. 2011;82(7):886–890. doi: 10.1016/j.resuscitation.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 4.Rogers FB, Shackford SR, Hoyt DB, et al. Trauma deaths in a mature urban vs rural trauma system: a comparison. Arch Surg. 1997;132(4):376–381. doi: 10.1001/archsurg.1997.01430280050007. [DOI] [PubMed] [Google Scholar]
- 5.Leonhard MJ, Wright DA, Fu R, Lehrfeld DP, Carlson KF. Urban/rural disparities in Oregon pediatric traumatic brain injury. Inj Epidemiol. 2015;2:32. doi: 10.1186/s40621-015-0063-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipsky AM, Karsteadt LL, Gausche-Hill M, et al. A comparison of rural versus urban trauma care. J Emerg Trauma Shock. 2014;7(1):41–46. doi: 10.4103/0974-2700.125639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40(4):536–545. doi: 10.1097/00005373-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271(24):1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 9.Mann NC, Hedges JR, Mullins RJ, Helfand M, Worrall W, Zechnich AD. OHSU Rural Trauma Research Group. Rural hospital transfer patterns before and after implementation of a statewide trauma system. Acad Emerg Med. 1997;4(8):764–771. [PubMed] [Google Scholar]
- 10.Olson CJ, Arthur M, Mullins RJ, Rowland D, Hedges JR, Mann NC. Influence of trauma system implementation on process of care delivered to seriously injured patients in rural trauma centers. Surgery. 2001;130(2):273–279. doi: 10.1067/msy.2001.115898. [DOI] [PubMed] [Google Scholar]
- 11.Clay Mann N, Mullins RJ, Hedges JR, Rowland D, Arthur M, Zechnich AD. Mortality among seriously injured patients treated in remote rural trauma centers before and after implementation of a statewide trauma system. Med Care. 2001;39(7):643–653. doi: 10.1097/00005650-200107000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Esposito TJ, Maier RV, Rivara FP, et al. The impact of variation in trauma care times: urban versus rural. Prehosp Disaster Med. 1995;10(3):161–166. doi: 10.1017/s1049023x00041947. [DOI] [PubMed] [Google Scholar]
- 13.Grossman DC, Kim A, Macdonald SC, Klein P, Copass MK, Maier RV. Urban-rural differences in prehospital care of major trauma. J Trauma. 1997;42(4):723–729. doi: 10.1097/00005373-199704000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 15.Nance ML, Carr BG, Branas CC. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med. 2009;163(6):512–518. doi: 10.1001/archpediatrics.2009.65. [DOI] [PubMed] [Google Scholar]
- 16.Newgard CD, Fu R, Zive D, et al. Prospective validation of the National Field Triage Guidelines for Identifying Seriously Injured Persons. J Am Coll Surg. 2016;222(2):146–58.e2. doi: 10.1016/j.jamcollsurg.2015.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Proposed rule for payment under the Ambulance Fee Schedule (AFS) [Accessed November 12, 2015]; https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AmbulanceFeeSchedule/. Published May 26, 2006.
- 19.US Census Bureau American Fact Finder. US Department of Commerce. [Accessed February 20, 2016]; https://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml.
- 20.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2014. [Google Scholar]
- 21.Sasser SM, Hunt RC, Sullivent EE, et al. National Expert Panel on Field Triage, Centers for Disease Control and Prevention (CDC) Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009;58(RR-1):1–35. [PubMed] [Google Scholar]
- 22.Dawson DE. National Emergency Medical Services Information System (NEMSIS) Prehosp Emerg Care. 2006;10(3):314–316. doi: 10.1080/10903120600724200. [DOI] [PubMed] [Google Scholar]
- 23.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 24.Newgard C, Malveau S, Staudenmayer K, et al. WESTRN investigators. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19(4):469–480. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newgard CD, Zive D, Holmes JF, et al. WESTRN investigators. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213(6):709–721. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newgard CD, Zive D, Jui J, Weathers C, Daya M. Electronic versus manual data processing: evaluating the use of electronic health records in out-of-hospital clinical research. Acad Emerg Med. 2012;19(2):217–227. doi: 10.1111/j.1553-2712.2011.01275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abbreviated Injury Scale Manual. Barrington, IL: Association for the Advancement of Automotive Medicine; 2005. [Google Scholar]
- 28.Baxt WG, Jones G, Fortlage D. The trauma triage rule: a new, resource-based approach to the prehospital identification of major trauma victims. Ann Emerg Med. 1990;19(12):1401–1406. doi: 10.1016/s0196-0644(05)82608-3. [DOI] [PubMed] [Google Scholar]
- 29.Zechnich AD, Hedges JR, Spackman K, Jui J, Mullins RJ. Applying the trauma triage rule to blunt trauma patients. Acad Emerg Med. 1995;2(12):1043–1052. doi: 10.1111/j.1553-2712.1995.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 30.Engum SA, Mitchell MK, Scherer LR, et al. Prehospital triage in the injured pediatric patient. J Pediatr Surg. 2000;35(1):82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 31.Newgard CD, Hui SH, Griffin A, Wuerstle M, Pratt F, Lewis RJ. Prospective validation of an out-of-hospital decision rule to identify seriously injured children involved in motor vehicle crashes. Acad Emerg Med. 2005;12(8):679–687. doi: 10.1197/j.aem.2005.03.526. [DOI] [PubMed] [Google Scholar]
- 32.Phillips JA, Buchman TG. Optimizing prehospital triage criteria for trauma team alerts. J Trauma. 1993;34(1):127–132. doi: 10.1097/00005373-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 33.Henry MC, Hollander JE, Alicandro JM, Cassara G, O'Malley S, Thode HC., Jr Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3(11):992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 34.Lerner EB, Willenbring BD, Pirrallo RG, et al. A consensus-based criterion standard for trauma center need. J Trauma Acute Care Surg. 2014;76(4):1157–1163. doi: 10.1097/TA.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 35.Little R, Rubin D. Statistical Analysis With Missing Data. 2nd. New York, NY: John Wiley & Sons, Inc; 2002. [Google Scholar]
- 36.Rubin D. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 37.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. Acad Emerg Med. 2006;13(3):314–324. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research—part 2: multiple imputation. Acad Emerg Med. 2007;14(7):669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 39.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27(1):85–95. [Google Scholar]
- 40.Fleischman RJ, Lundquist M, Jui J, Newgard CD, Warden C. Predicting ambulance time of arrival to the emergency department using global positioning system and Google maps. Prehosp Emerg Care. 2013;17(4):458–465. doi: 10.3109/10903127.2013.811562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sorensen MJ, von Recklinghausen FM, Fulton G, Burchard KW. Secondary overtriage: the burden of unnecessary interfacility transfers in a rural trauma system. JAMA Surg. 2013;148(8):763–768. doi: 10.1001/jamasurg.2013.2132. [DOI] [PubMed] [Google Scholar]
- 42.Newgard CD, McConnell KJ, Hedges JR. Variability of trauma transfer practices among non–tertiary care hospital emergency departments. Acad Emerg Med. 2006;13(7):746–754. doi: 10.1197/j.aem.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 43.Delgado MK, Yokell MA, Staudenmayer KL, Spain DA, Hernandez-Boussard T, Wang NE. Factors associated with the disposition of severely injured patients initially seen at non–trauma center emergency departments: disparities by insurance status. JAMA Surg. 2014;149(5):422–430. doi: 10.1001/jamasurg.2013.4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Newgard CD, McConnell KJ, Hedges JR, Mullins RJ. The benefit of higher level of care transfer of injured patients from nontertiary hospital emergency departments. J Trauma. 2007;63(5):965–971. doi: 10.1097/TA.0b013e31803c5665. [DOI] [PubMed] [Google Scholar]
- 45.Ingram DD, Franco SJ. NCHS urban-rural classification scheme for counties. Vital Health Stat. 2013;2014(166):1–73. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.