Abstract
Despite the prevalence of viral infections in the American population, we still have a limited understanding of how they affect pregnancy and fetal development. Viruses can gain access to the decidua and placenta by ascending from the lower reproductive tract or via hematogenous transmission. Viral tropism for the decidua and placenta is then dependent on viral entry receptor expression in these tissues as well as on the maternal immune response to the virus. These factors vary by cell type and gestational age and can be affected by changes to the in utero environment and maternal immunity. Some viruses can directly infect the fetus at specific times during gestation, while some only infect the placenta. Both scenarios can result in severe birth defects or pregnancy loss. Systemic maternal viral infections can also affect the pregnancy, and these can be especially dangerous, because pregnant women suffer higher virus-associated morbidity and mortality than do nonpregnant counterparts. In this Review, we discuss the potential contributions of maternal, placental, and fetal viral infection to pregnancy outcome, fetal development, and maternal well-being.
Introduction
Viral infections during pregnancy have been associated with adverse pregnancy outcomes and birth defects in the offspring; unfortunately, we have limited therapeutic or preventative tools to protect the mother and the fetus during pandemics. Viruses rarely cross the placental barrier, but when the virus does reach the fetus, it can result in severe birth defects such as microcephaly or even fetal death. It has been well established that viral infection of the cells at the maternal-fetal interface can affect placental function, which may result in pregnancy complications such as miscarriage, intrauterine growth restriction (IUGR), or preterm birth (PTB). Furthermore, a growing body of evidence suggests that viral infection of the decidua and/or placenta may result in the production of soluble immune factors that could reach the fetus and might affect fetal development.
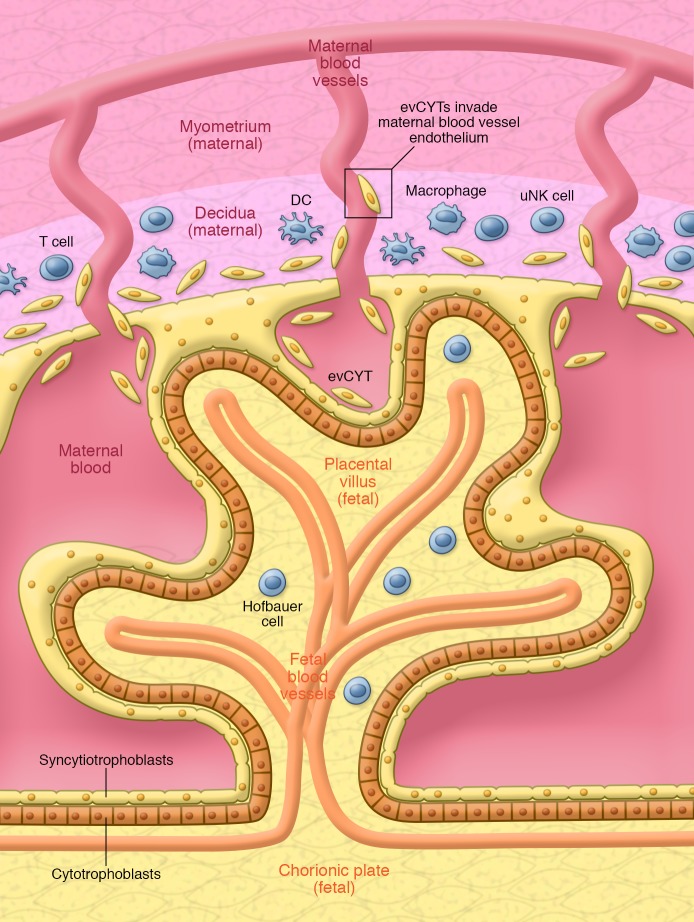
The maternal-fetal interface includes multiple cell types that contribute to the development of the fetus, regulation of the maternal immune system, and protection against microorganisms. The maternal side is made from the stroma of the uterus, or decidual cells, and a wide range of immune cells including NK cells, macrophages, DCs, and Tregs. The fetal side consists of the placental villus, which contains fetal blood vessels surrounded by fibroblasts and fetal macrophages (known as Hofbauer cells), cytotrophoblasts, and, finally, the multinucleated syncytiotrophoblast, an epithelial covering that is in direct contact with maternal blood (Figure 1). In addition, the extravillous trophoblast is in direct contact with cells from the decidua, including maternal immune cells, endothelial cells, and microorganisms present in the uterus.
Figure 1. Cell types at the maternal-fetal interface.
Maternal and fetal cells make up the maternal-fetal interface. The maternal decidua consists of pregnancy-specific differentiated stromal cells that house the maternal blood vessels and maternal immune cells including T cells, uterine NK (uNK) cells, macrophages, and DCs. Extravillous cytotrophoblasts (evCYTs) invade the decidua and reach the maternal spiral arteries, establishing nutrient circulation between the embryo and the mother. The placental villus is in direct contact with the maternal blood and thus facilitates gas, nutrient, and communication exchange between the mother and developing fetus. It is formed by a double cell layer consisting of syncytiotrophoblasts and cytotrophoblasts. The villus contains the fetal blood vessels that are surrounded by fibroblasts and fetal macrophages (termed Hofbauer cells).
Many factors can influence the incidence, longevity, and severity of viral infection at the maternal-fetal interface. Viruses gain access to the cells within the decidua and placenta by ascending from the lower reproductive tract or via hematogenous transmission (1, 2). Following access to the upper reproductive tract, viral tropism for the decidua and/or placenta is then dependent on both viral entry receptor expression by the cellular component of these tissues and the specific maternal immune response to the virus. These factors vary by cell type and gestational age and can be affected by changes to the in utero environment and maternal immunity. Therefore, the virus-host interaction during pregnancy is complex and highly variable (Figure 1).
Innate immune cells, including NK cells, DCs, and macrophages, and the maternal humoral response play a critical role in regulating and controlling the infection and, consequently, determining its severity. Innate cells phagocytize virus complexes and can kill infected cells, while antibodies facilitate viral clearance. Contrary to nonpregnant women, during pregnancy, the function of the innate immune system is influenced and regulated by the fetal/placenta unit. In summary, the route of viral transmission, abundance of permissive cell types (which changes with gestational age), and maternal immune function all influence viral infections at the maternal-fetal interface.
Viral infection at the maternal-fetal interface
The most common virus identified to date at the maternal-fetal interface is CMV, a member of the Herpesviridae family. CMV interacts with ubiquitously expressed heparin sulfate on the cell surface and then penetrates cells via interactions with integrin subunits (3, 4). Roles for other receptors, such as EGFR and PDGFR-α, have also been reported, but those findings have been contradicted, and the role of these receptors in CMV infection remains disputed (5, 6). The known receptors for CMV entry are expressed by multiple cell types, including epithelial cells, endothelial cells, muscle cells, fibroblasts, trophoblasts, and monocytes/macrophages; therefore, these cells can all be permissive to CMV infection. At the maternal-fetal interface, specifically, CMV is more likely to be detected in the maternal decidua, where it infects and replicates in endothelial cells, invasive cytotrophoblast, fibroblasts, and the glandular epithelium (7, 8), than in the placenta. Decidual infection can occur in the first, second, or third trimester and is affected by variations in local maternal innate immune cells. For example, in pregnant women, higher levels of local DCs and macrophages containing phagocytosed viral proteins in the decidua are associated with milder infection, potentially because of the robust innate response to infection in these individuals (7, 8).
Interestingly, placental CMV infection is less common than decidual infection. This is because the syncytiotrophoblast does not express the receptors for CMV entry, and the virus must traverse this layer to infect the susceptible cytotrophoblast localized underneath the syncytiotrophoblast layer. Because of this tissue organization, the severity of infection is dependent on maternal factors such as humoral immunity and microbial coinfections of the placenta (7–9) that would promote the breach of the syncytiotrophoblast layer. Low-avidity neutralizing IgG can bind the virus and interact with syncytiotrophoblast Fc receptors, thus catalyzing viral transcytosis to the underlying cytotrophoblast (2, 9, 10). As discussed below, coinfections, or polymicrobial infections, are an important factor in allowing pathogens to damage the syncytial layer, thereby permitting the virus to cross and reach the fetal side. Alternatively, the presence of other pathogens could activate latent CMV in the decidual-immune reservoir (7).
Another member of the Herpesviridae family, herpes simplex virus (HSV), is estimated to infect the decidua and/or placenta in 6% to 14% of pregnancies (7, 11) and, like CMV, is more likely to be identified in the decidua than in the placenta (7, 12). Deciduitis and villitis have been described in relation to HSV infections (13), which may explain the association between primary maternal infection with HSV and increased risk of miscarriage and fetal death (14). Heparan sulfate, herpesvirus entry mediator A (HveA), HveB, and HveC are the entry receptors for HSV-1 and -2. They are not expressed on the surface of the syncytiotrophoblast but are expressed on the extravillous trophoblast (15, 16). Finger-Jardim et al. reported a 9% prevalence of HSV-2 in placental samples in asymptomatic patients at the time of delivery, and none reported genital herpes (11). These results suggest that HSV-2 can infect the placenta even in asymptomatic patients. The clinical and biological relevance of HSV-2 infection on those placentas is poorly understood, but as discussed below, the antiviral response originated at the placenta might reach the fetal side and influence fetal development.
The herpesviruses varicella zoster virus and EBV have been isolated in placental tissue and can infect the developing fetus, but cases are extremely rare, and little is known about the conditions for infection (12, 17). While not herpesviruses, human papillomaviruses HPV6, -11, -16, -18, and -31 can also infect the extravillous trophoblast (18, 19); HPV16 and HPV62 have been identified in gestational week-12 chorionic villus (20); and HPV16, -6, -83, and -39 have been characterized full-term placenta (19, 21–23). Zika virus (ZIKV) can also infect multiple cell types of the decidua and placenta and will be discussed in further detail in a later section.
Viral infections and fetal development
Viral infections that are capable of crossing the placental barrier and reaching the fetus can have devastating effects on fetal development (24). Gregg first described the association between fetal viral infection and abnormal development when he discovered the association between prenatal rubella infection and cataract in 1941 (25). There is now a large body of work demonstrating that direct infection of the fetus with CMV, HSV-2, or rubella can cause major neurosensory deficits (26–28), learning disabilities, and psychiatric disorders (29–31). Microcephaly has also been associated with fetal CMV and ZIKV infection (ZIKV is further discussed below) (32, 33). While these examples of direct infection of the fetus have the most severe individual consequences, in utero fetal viral infections are rare. Neonatal HSV infection has been identified in approximately 0.06% of neonates in the US, and only 5% of those infections are associated with intrauterine infection (34). Fetal infection with CMV has an estimated prevalence of 0.5% (28), and congenital rubella has been virtually eliminated in the US (35–37). Conversely, the prevalence of maternal infection or reactivation with CMV, HSV-2, or influenza is high (60%–90%, 18%–22%, and 40%, respectively) (8, 11, 27, 38–43). All these data support the notion that the placenta is actively preventing viral transmission to the fetus; however, viral infections of the placenta, such as that by HSV-2, can occur in asymptomatic patients (11) and can induce systemic and local (placental/decidual) changes, which could still affect fetal development.
While viral infections that do not cross the placenta can affect fetal development, specifically neuronal development, the mechanism is still poorly understood. Original observations identified individuals from a Finnish birth cohort whose mothers were in their second trimester of pregnancy during the 1957 influenza pandemic as having an increased chance of being admitted to a psychiatric hospital and diagnosed with schizophrenia (44). Although several studies following this initial observation had inconclusive results, when researchers identified mothers with influenza only using serological tests, they confirmed that influenza during early-to-mid gestation was associated with an increased risk of schizophrenia in the offspring (45, 46).
The epidemiologic studies referenced above indicate that maternal viral infections do not need to bypass the placental barrier to affect fetal development, and animal models have been invaluable tools for improving our understanding of this complex mechanism. With these models, potential maternal immune pathways and cytokines that could be responsible for behavioral changes in offspring have been identified (47, 48). Recently, in a polyinosinic-polycytidylic acid (poly(I:C)) mouse model of maternal immune activation (MIA), maternal Th17 cells and their effector IL-17a were identified as critical drivers of maternal inflammation–associated defects in fetal brain development and offspring behavior (49). In another study, using the same mouse model of MIA, it was determined that maternal IL-6 is also a critical effector (50). In this study, injecting the pregnant mother with IL-6 alone was able to affect offspring behavior (50). Furthermore, neutralizing maternal IL-6 with antibodies following poly(I:C) treatment prevented the exploratory and social deficits caused by the MIA (50).
To evaluate the role of viral infection in pregnancy and fetal development, we developed a murine model that consists of exposing pregnant mice to murine herpes virus 68 (MHV68). We used the gammaherpes virus MHV68, since it is a latent DNA virus from the Herpesviridae family, the same family for nearly all of the viruses that infect the woman’s reproductive tract (HSV, CMV, EBV, and human herpesviruses HHV6 and HHV7). Our data suggested that, even in the absence of placental passage of the virus, the fetus could be adversely affected by viral invasion of the placenta (51). Morphological analysis of fetuses from mothers with viral infections revealed major developmental changes. Despite the absence of fetal infection, the fetuses of infected mothers had delayed differentiation of the eyes, tails, and limbs (51). They also had hydrocephalus, defined by an increase in the subarachnoid space in the brain, but no changes in the lateral ventricles, abnormal immune infiltration, or white matter damage (51). In the thoracic cavity, the pathological changes were characterized by the presence of hemorrhage inside the lungs and pericardium in all treated animals compared with the controls (51). Interestingly, we also observed a marked increase in the levels of fetal proinflammatory cytokines, including high levels of IFN-γ and TNF-α (51). Collectively, these findings provide strong evidence that, even when the virus does not reach the fetus, the fetus is still affected by the maternal immune response to the infection. This could be a result of the proinflammatory response of the placenta, or it could be due to other physiological changes in the mother or the placenta that are associated with the infection.
Viral infection and PTB: cervical infection
Cervical viral infection can increase the risk for PTB, defined as birth before 37 weeks’ gestation in women. Many viruses have been reported to infect the cervix, including HHV6, HHV7 (52), HSV (53), CMV (2, 54), EBV (55), and HPV (56), the most common viral infection of the cervix. Despite the prevalence, there were historical challenges associated with measuring viral infections in biological fluids and tissues from the lower reproductive track. With improved molecular techniques (sensitive PCR assays), we are beginning to identify viral infections as potential risk factors for PTB (53, 56–58). For example, Zuo et al. showed that cervical HPV infection was associated with PTB (56), while others determined that genital HSV was also associated with PTB (53, 59). One of these studies included nearly 700,000 women and reported that untreated genital herpes infection nearly doubled the risk of PTB (53). In a mouse model, we have shown that the murine herpesvirus MHV68 targets the pregnant cervix and induces dramatic molecular and functional changes in that tissue (58). We observed that high levels of sex hormones associated with pregnancy enhanced the susceptibility to cervical infection by upregulating cervical integrins (58). In addition, MHV68 infection of the cervix in pregnant mice reduced the expression of innate immune factors such as TLRs and defensins (58). These changes in the pregnant cervix were associated with increased ascending infection compared with that detected in uninfected pregnant mice (Figure 2A) (58). In a separate study, pregnant mice received HSV-2 intravaginally, which induced tissue remodeling in the stroma that was reminiscent of cervical ripening (60). Infection of human cervical epithelial cells with HSV-2 caused activation of SRC kinase, which stabilized the estrogen receptor (ER) (60). Interestingly, HSV-2 also upregulated hyaluronic acid (HA), which was dependent on the increased ER levels (60). Since HA is associated with changes in tissue structure and function, we postulate that viral infection of cervical epithelial cells results in increased HA synthesis, thus affecting stromal architecture and premature cervical ripening (Figure 2A).
Figure 2. Mouse models of viral infection during pregnancy.
Herpesviruses target the pregnant cervix and induce dramatic molecular and functional changes. (A) High sex hormone levels associated with pregnancy enhance cervical susceptibility to infection by causing upregulation in the cervix of integrins and HA, receptors for herpes infection. (B) Infection of cervical epithelial cells results in activated SRC kinase, which stabilizes the ER. These changes are also associated with reduced expression of innate immune factors such as TLRs and defensins, as well as tissue remodeling in the stroma that is reminiscent of cervical ripening.
Viral infection and PTB: in utero or systemic infection
Several studies have demonstrated an association between maternal, placental, or amniotic fluid viral detection and PTB. One case-control study identified a higher frequency of HPV in the extravillous trophoblast of women suffering from spontaneous PTB compared with women delivering at term, with no association with low- or high-risk HPV strains (18). Another retrospective study examined over 2,400 cases of pregnancy over an 11-year period and discovered that cervical infection with high-risk HPV was highly associated with abnormal placental pathology and PTB (56). The presence of adeno-associated virus (AAV) in amniotic cells was also associated with an increased risk of PTB, although the authors did not determine whether AAV DNA was present in the placenta (61).
Maternal infections with influenza and hepatitis have also been associated with preterm labor. Data collected from the 2009 influenza H1N1 pandemic revealed that women with H1N1 were more likely to have adverse pregnancy outcomes, such as spontaneous miscarriage and preterm birth (62–64). The rate of PTB correlated with maternal disease severity (65), and, moreover, vaccination against H1N1 reduced the rates of PTB and low birth weight (66–69). Maternal hepatitis B virus (HBV) infection was also associated with PTB, although the underlying mechanism was not determined (70).
The only mechanistic insights we have with regard to virus-associated PTB are those gleaned from animal models. Initial studies consisted of administration of TLR ligands, such as Poly(I:C), to pregnant WT or Tlr3-KO mice to mimic viral signaling during pregnancy (71, 72). This induced preterm labor in WT but not Tlr3-KO mice, indicating that TLR3 signaling could cause PTB (71). Although these animal studies strongly support a role for viral infections in PTB, the majority of the clinical findings in patients with PTB are associated with an inflammatory process caused by bacterial infections (73). Our animal studies using a live virus have suggested that the actual mechanism associated with infection-induced PTB is more complex. We showed that pregnant mice injected with a DNA virus of the Herpesviridae family did not suffer PTB, but the virus infected the placenta (51). The viral infection of the placenta was associated with hyperresponsiveness to low concentrations of bacterial endotoxin, which led to PTB (51). At the molecular level, viral infections modified the function of pattern recognition receptors (PRRs), such as TLRs, and affected the quantity as well as the quality of their responses. We demonstrated in both in vivo and in vitro studies that the virus downregulated the placental type I IFN, IFN-β, thus releasing the intrinsic regulation of TLR4-mediated proinflammatory cytokines in the trophoblast and allowing its cells to respond to the endotoxin challenge (ref. 74 and Figure 2B). Given these findings, we proposed that many of these infection-related pregnancy complications are polymicrobial in nature and involve an initial infection, viral (first hit), that modifies the response of the PRRs to the second infection, bacterial (second hit). Together, these pathogens result in a dysregulated inflammatory response that triggers preterm delivery. This mechanism needs further elucidation if we are to develop new methods for prevention and therapy.
Viral infections and early placental development
The invasive extravillous trophoblast is responsible for anchoring the placenta and invading the maternal spiral arteries early in pregnancy, thus ensuring adequate blood flow and communication between mother and fetus (75–77). If these cells are dysregulated and this process disrupted, there is increased risk for pregnancy complications (78). For example, first-trimester trophoblasts infected with CMV demonstrate reduced cell invasion, increased apoptosis (2, 79), higher expression of proinflammatory cytokines (80), and reduced HLA-G expression (81, 82). CMV infection is also associated with fetal growth restriction, spontaneous pregnancy loss (82–84), and preeclampsia (85, 86), all of which are outcomes that can result from insufficient placental development. HSV infection also results in loss of HLA-G (87), cell death, and reduced human chorionic gonadotropin secretion (88). These changes in trophoblast function could explain why both HSV-1 and HSV-2 have been associated with spontaneous pregnancy loss (89) and IUGR pregnancies (82, 84). AAV2 also induces trophoblast apoptosis and reduces cell invasion (18, 90, 91) and is associated with spontaneous miscarriage, stillbirth (92), and preeclampsia (82, 91, 93). Collectively, these results demonstrate that viral infection of the trophoblast can alter placental function and could result in suboptimal conditions for fetal growth and development.
Viral infection and maternal health
Pregnant women have higher mortality rates and complications associated with viral infections compared with the general population, but the reason for the increased susceptibility is not well defined (94). The maternal immune response can be beneficially or detrimentally affected by pregnancy, depending on the environmental conditions and the stage of the pregnancy. It is well established that the immunological changes associated with pregnancy can result in the amelioration of some autoimmune disorders, such as multiple sclerosis or rheumatoid arthritis (95), but can also increase the severity of several types of viral infections. For example, pregnant women have higher mortality rates associated with varicella virus infection, which is 10 times more likely to be complicated by pneumonia during pregnancy (94, 96, 97). They are more susceptible to rubeola (also known as measles), and the infection is more likely to cause death (98, 99). Furthermore, during the 2009 H1N1 influenza pandemic, pregnant women developed more severe flu-related complications, in some cases leadings to hospitalization and death, when compared with the general population (41, 62, 64, 100–105), and this was confirmed to have also occurred during the 1918 H1N1 (106, 107) and 1957 H5N1 pandemics (108, 109).
Despite these clear associations between pregnancy and virus-induced morbidity, there is still little known about how pregnancy affects the mother’s response to viral pathogens. There is growing evidence suggesting that the placental response to virus is directly responsible for disease severity. For example, pregnant women infected with Lassa fever had higher mortality rates than did nonpregnant women with the infection (110). The Lassa virus replicates at very high levels in the placenta (111), and the risk of maternal death increases with the length of gestation (110) and the size of the placenta. Furthermore, evacuation of the uterus significantly improves the mother’s chances of survival (110). Since the placenta regulates the maternal immune system and can itself respond to pathogens, it is probably an important mediator of the maternal response to viral infection, regardless of whether the placenta is directly infected (112).
ZIKV and pregnancy
The recent ZIKV outbreak in Brazil has refocused our attention on the risks associated with viral infections during pregnancy. This virus, a member of the family Flaviviridae, is transmitted by mosquito bite and is also potentially sexually transmitted (113–117). While historically an infection has been described as causing symptoms ranging from fever and rash to Guillain-Barre syndrome (118–124), during the most recent outbreak there was also a startling increase in the incidence of fetal brain and CNS abnormalities when mothers acquired the virus during pregnancy (32, 125–134). A causal link between ZIKV and these defects was established when the ZIKV genome was identified in the amniotic fluid of women whose fetuses had microcephaly detected during fetal ultrasound (125–127, 132, 133, 135). Researchers also identified ZIKV in placentas from miscarriages and IUGR pregnancies, suggesting that ZIKV also affects placental function and could increase the risk of several pregnancy complications (126, 132, 136). There is now a global push to understand how ZIKV affects pregnancy and fetal brain development.
Like all viruses, ZIKV requires cellular expression of receptors that permit viral binding and entry into that cell. Several of these receptors have been identified, including the TAM kinase receptors AXL and TYRO3, in addition to the C-type lectin DC-SIGN and the glycoprotein TIM1 (137). An important study by the Harris and Pereira laboratories recently determined that AXL and TYRO3 receptors had variable expression in placental cells that could be affected by the culture of primary cells. These proteins were expressed by amniotic epithelia, and AXL was also expressed by the cytotrophoblast, Hofbauer cells, and placental fibroblasts, but this expression was variable depending on the gestational stage, the donor, and whether the cells were cultured (138). In contrast, TIM1 was invariably expressed at mid- and late gestation in amniotic epithelia, syncytiotrophoblast, Hofbauer cells, and invasive cytotrophoblast (138). They also examined ZIKV in primary placental cells and explants. Amniotic epithelia from mid-gestation had higher viral titers than did late-gestation epithelia, and mid-gestation proliferating cytotrophoblast and invasive cytotrophoblast were also viral targets (138). Of note, infection of the cytotrophoblast in early gestation was associated with loss of proliferation (138), which could contribute to ZIKV-associated miscarriage and growth restriction. Finally, this study found that placental fibroblasts and Hofbauer cells were infected by ZIKV (138), with similar findings reported by others (139). These cells are closely associated with the fetal vasculature and could be responsible for harboring virus that can be more easily transmitted to the fetus.
We found that, unlike Flavivirus yellow fever, ZIKV infection induces apoptosis in first-trimester trophoblasts, prevents differentiation of these cells into spheroid cultures, and induces the collapse of preformed trophoblast-derived spheroids (140). Furthermore, there is a growing interest in additional factors responsible for the teratogenic effects observed in some patients infected with ZIKV. Since the seroprevalence of HSV-1 and HSV-2 was found to be higher in Brazil’s North region (141), which reported the majority of microcephaly cases (132), we tested the hypothesis that the immune response to HSV-2 could have an effect on ZIKV infection. Indeed, we observed that HSV-2 infection of trophoblasts could enhance the expression of TAM receptors, which facilitate entry of ZIKV into the cell. Using a mouse model resistant to ZIKV infection, we demonstrate that HSV-2 infection enhances placental sensitivity to ZIKV infection (140).
Microcephaly is the most severe birth defect associated with ZIKV and occurs via direct infection of the fetus during the first or second trimester of pregnancy (126, 132, 133, 135). The mechanism of virus-associated microcephaly is still unknown, but recent studies suggest that direct infection of the brain dysregulates development. Viral antigens infecting glial cells and neurons have been identified in the brains of fetuses with microcephaly, and these infections are associated with microcalcifications (126, 132, 136). Human cortical progenitors and human brain organoids can also be infected by ZIKV, which results in increased cell death and fewer proliferative zones, respectively (142). While animal models will require further validation, preliminary work with mice has demonstrated that similar placental types are susceptible to infection (143), the virus infects the fetal brain (113, 142), and fetal infection results in signs of microcephaly (113, 142). ZIKV infection of the lower reproductive tract of pregnant mice has also been shown to result in viral transmission to the fetus (113).
Conclusions and perspectives
Viral infections during pregnancy can affect fetal development and maternal mortality and are therefore a major clinical problem worldwide (Figure 3). Unfortunately, we do not yet have the appropriate tools to prevent infection and treat pregnant women during pandemics such as influenza, Ebola, and ZIKV. The complexity of pregnancy and the immunologic changes associated with the acceptance of the fetus makes it challenging to improve the way we treat pregnant women. To progress, we must gain a better understanding of how viruses infect and affect the placenta at different stages of gestation and how direct and indirect fetal infections affect development. We also need to determine why pregnant women respond differently to infections than do their nonpregnant counterparts. These studies will provide the first step toward improving the clinical care provided to pregnant women and their unborn children.
Figure 3. Maternal viral infections and associated outcomes.

Viral infection at the maternal-fetal interface can affect the mother as well as fetal development. The placenta functions as a physiologic and immunologic barrier to prevent viral transfer from the mother to the fetus. However, the immunologic response to infection might reach the fetal circulation or predispose the mother to abnormal responses to other microorganisms, with potential pregnancy complications such as IUGR, PTB, or even early pregnancy loss. Fetal infection can cause pregnancy loss and is associated with hearing loss, cataract, microcephaly, and psychiatric disorders in the fetus.
Acknowledgments
This work was funded in part by a grant from the National Institute of Allergy and Infectious Diseases (NIAID), NIH (1R56AI124356-01).
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Reference information:J Clin Invest. 2017;127(5):1591–1599.
https://doi.org/10.1172/JCI87490.
Contributor Information
Karen Racicot, Email: karen.racicot@hc.msu.edu.
Gil Mor, Email: gil.mor@yale.edu.
References
- 1.Salzberger B, Myerson D, Boeckh M. Circulating cytomegalovirus (CMV)-infected endothelial cells in marrow transplant patients with CMV disease and CMV infection. J Infect Dis. 1997;176(3):778–781. doi: 10.1086/517300. [DOI] [PubMed] [Google Scholar]
- 2.Fisher S, Genbacev O, Maidji E, Pereira L. Human cytomegalovirus infection of placental cytotrophoblasts in vitro and in utero: implications for transmission and pathogenesis. J Virol. 2000;74(15):6808–6820. doi: 10.1128/JVI.74.15.6808-6820.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Compton T, Nowlin DM, Cooper NR. Initiation of human cytomegalovirus infection requires initial interaction with cell surface heparan sulfate. Virology. 1993;193(2):834–841. doi: 10.1006/viro.1993.1192. [DOI] [PubMed] [Google Scholar]
- 4.Feire AL, Koss H, Compton T. Cellular integrins function as entry receptors for human cytomegalovirus via a highly conserved disintegrin-like domain. Proc Natl Acad Sci U S A. 2004;101(43):15470–15475. doi: 10.1073/pnas.0406821101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isaacson MK, Feire AL, Compton T. Epidermal growth factor receptor is not required for human cytomegalovirus entry or signaling. J Virol. 2007;81(12):6241–6247. doi: 10.1128/JVI.00169-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vanarsdall AL, Wisner TW, Lei H, Kazlauskas A, Johnson DC. PDGF receptor-α does not promote HCMV entry into epithelial and endothelial cells but increased quantities stimulate entry by an abnormal pathway. PLoS Pathog. 2012;8(9):e1002905. doi: 10.1371/journal.ppat.1002905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pereira L, Maidji E, McDonagh S, Genbacev O, Fisher S. Human cytomegalovirus transmission from the uterus to the placenta correlates with the presence of pathogenic bacteria and maternal immunity. J Virol. 2003;77(24):13301–13314. doi: 10.1128/JVI.77.24.13301-13314.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonagh S, Maidji E, Ma W, Chang HT, Fisher S, Pereira L. Viral and bacterial pathogens at the maternal-fetal interface. J Infect Dis. 2004;190(4):826–834. doi: 10.1086/422330. [DOI] [PubMed] [Google Scholar]
- 9.Maidji E, McDonagh S, Genbacev O, Tabata T, Pereira L. Maternal antibodies enhance or prevent cytomegalovirus infection in the placenta by neonatal Fc receptor-mediated transcytosis. Am J Pathol. 2006;168(4):1210–1226. doi: 10.2353/ajpath.2006.050482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robbins JR, Bakardjiev AI. Pathogens and the placental fortress. Curr Opin Microbiol. 2012;15(1):36–43. doi: 10.1016/j.mib.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finger-Jardim F, et al. Herpes simplex virus: prevalence in placental tissue and incidence in neonatal cord blood samples. J Med Virol. 2014;86(3):519–524. doi: 10.1002/jmv.23817. [DOI] [PubMed] [Google Scholar]
- 12.Avgil M, Ornoy A. Herpes simplex virus and Epstein-Barr virus infections in pregnancy: consequences of neonatal or intrauterine infection. Reprod Toxicol. 2006;21(4):436–445. doi: 10.1016/j.reprotox.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Granat M, Morag A, Margalioth EJ, Leviner E, Ornoy A. Fetal outcome following primary herpetic gingivostomatitis in early pregnancy. Morphological study and updated appraisal. Isr J Med Sci. 1986;22(6):455–459. [PubMed] [Google Scholar]
- 14.Grönroos M, Honkonen E, Terho P, Punnonen R. Cervical and serum IgA and serum IgG antibodies to Chlamydia trachomatis and herpes simplex virus in threatened abortion: a prospective study. Br J Obstet Gynaecol. 1983;90(2):167–170. doi: 10.1111/j.1471-0528.1983.tb08903.x. [DOI] [PubMed] [Google Scholar]
- 15.Koi H, et al. Syncytiotrophoblast is a barrier to maternal-fetal transmission of herpes simplex virus. Biol Reprod. 2002;67(5):1572–1579. doi: 10.1095/biolreprod.102.004325. [DOI] [PubMed] [Google Scholar]
- 16.Parry S, et al. Transduction of human trophoblastic cells by replication-deficient recombinant viral vectors. Promoting cellular differentiation affects virus entry. Am J Pathol. 1998;152(6):1521–1529. [PMC free article] [PubMed] [Google Scholar]
- 17.Hollier LM, Grissom H. Human herpes viruses in pregnancy: cytomegalovirus, Epstein-Barr virus, and varicella zoster virus. Clin Perinatol. 2005;32(3):671–696. doi: 10.1016/j.clp.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Gomez LM, Ma Y, Ho C, McGrath CM, Nelson DB, Parry S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum Reprod. 2008;23(3):709–715. doi: 10.1093/humrep/dem404. [DOI] [PubMed] [Google Scholar]
- 19.Slatter TL, Hung NG, Clow WM, Royds JA, Devenish CJ, Hung NA. A clinicopathological study of episomal papillomavirus infection of the human placenta and pregnancy complications. Mod Pathol. 2015;28(10):1369–1382. doi: 10.1038/modpathol.2015.88. [DOI] [PubMed] [Google Scholar]
- 20.Weyn C, et al. Evidence of human papillomavirus in the placenta. J Infect Dis. 2011;203(3):341–343. doi: 10.1093/infdis/jiq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SM, et al. Risk of vertical transmission of human papillomavirus throughout pregnancy: a prospective study. PLoS One. 2013;8(6):e66368. doi: 10.1371/journal.pone.0066368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rombaldi RL, Serafini EP, Mandelli J, Zimmermann E, Losquiavo KP. Transplacental transmission of Human Papillomavirus. Virol J. 2008;5:106. doi: 10.1186/1743-422X-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarkola ME, Grenman SE, Rintala MA, Syrjanen KJ, Syrjanen SM. Human papillomavirus in the placenta and umbilical cord blood. Acta Obstet Gynecol Scand. 2008;87(11):1181–1188. doi: 10.1080/00016340802468308. [DOI] [PubMed] [Google Scholar]
- 24.Cordeiro CN, Tsimis M, Burd I. Infections and brain development. Obstet Gynecol Surv. 2015;70(10):644–655. doi: 10.1097/OGX.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gregg NM. Congenital cataract following German measles in the mother. 1941. Epidemiol Infect. 1991;107(1):iii–xiv; discussion xiii. doi: 10.1017/s0950268800048627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Enright AM, Prober CG. Neonatal herpes infection: diagnosis, treatment and prevention. Semin Neonatol. 2002;7(4):283–291. doi: 10.1016/s1084-2756(02)90115-6. [DOI] [PubMed] [Google Scholar]
- 27.Kenneson A, Cannon MJ. Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol. 2007;17(4):253–276. doi: 10.1002/rmv.535. [DOI] [PubMed] [Google Scholar]
- 28.Cheeran MC, Lokensgard JR, Schleiss MR. Neuropathogenesis of congenital cytomegalovirus infection: disease mechanisms and prospects for intervention. Clin Microbiol Rev. 2009;22(1):99–126. doi: 10.1128/CMR.00023-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buka SL, Tsuang MT, Torrey EF, Klebanoff MA, Wagner RL, Yolken RH. Maternal cytokine levels during pregnancy and adult psychosis. Brain Behav Immun. 2001;15(4):411–420. doi: 10.1006/brbi.2001.0644. [DOI] [PubMed] [Google Scholar]
- 30.Buka SL, Cannon TD, Torrey EF, Yolken RH, Collaborative Study Group on the Perinatal Origins of Severe Psychiatric Disorders Maternal exposure to herpes simplex virus and risk of psychosis among adult offspring. Biol Psychiatry. 2008;63(8):809–815. doi: 10.1016/j.biopsych.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 31.Goldstein JM, et al. Prenatal maternal immune disruption and sex-dependent risk for psychoses. Psychol Med. 2014;44(15):3249–3261. doi: 10.1017/S0033291714000683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cauchemez S, et al. Association between Zika virus and microcephaly in French Polynesia, 2013–2015: a retrospective study. Lancet. 2016;387(10033):2125–2132. doi: 10.1016/S0140-6736(16)00651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahlfors K, Ivarsson SA, Bjerre I. Microcephaly and congenital cytomegalovirus infection: a combined prospective and retrospective study of a Swedish infant population. Pediatrics. 1986;78(6):1058–1063. [PubMed] [Google Scholar]
- 34.Jones CA. Vertical transmission of genital herpes: prevention and treatment options. Drugs. 2009;69(4):421–434. doi: 10.2165/00003495-200969040-00003. [DOI] [PubMed] [Google Scholar]
- 35.Reef SE, Cochi SL. The evidence for the elimination of rubella and congenital rubella syndrome in the United States: a public health achievement. Clin Infect Dis. 2006;43(suppl 3):S123–S125. doi: 10.1086/505943. [DOI] [PubMed] [Google Scholar]
- 36.Meissner HC, Reef SE, Cochi S. Elimination of rubella from the United States: a milestone on the road to global elimination. Pediatrics. 2006;117(3):933–935. doi: 10.1542/peds.2005-1760. [DOI] [PubMed] [Google Scholar]
- 37.Reef SE, et al. The changing epidemiology of rubella in the 1990s: on the verge of elimination and new challenges for control and prevention. JAMA. 2002;287(4):464–472. doi: 10.1001/jama.287.4.464. [DOI] [PubMed] [Google Scholar]
- 38.Gibson CS, et al. Neurotropic viruses and cerebral palsy: population based case-control study. BMJ. 2006;332(7533):76–80. doi: 10.1136/bmj.38668.616806.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Callaghan WM, Chu SY, Jamieson DJ. Deaths from seasonal influenza among pregnant women in the United States, 1998–2005. Obstet Gynecol. 2010;115(5):919–923. doi: 10.1097/AOG.0b013e3181d99d85. [DOI] [PubMed] [Google Scholar]
- 40.Chan KH, et al. Wild type and mutant 2009 pandemic influenza A (H1N1) viruses cause more severe disease and higher mortality in pregnant BALB/c mice. PLoS One. 2010;5(10):e13757. doi: 10.1371/journal.pone.0013757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Creanga AA, et al. Seasonal and 2009 pandemic influenza A (H1N1) virus infection during pregnancy: a population-based study of hospitalized cases. Am J Obstet Gynecol. 2011;204(6 suppl 1):S38–S45. doi: 10.1016/j.ajog.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 42.Shi L, Tu N, Patterson PH. Maternal influenza infection is likely to alter fetal brain development indirectly: the virus is not detected in the fetus. Int J Dev Neurosci. 2005;23(2–3):299–305. doi: 10.1016/j.ijdevneu.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 43.Silasi M, Cardenas I, Kwon JY, Racicot K, Aldo P, Mor G. Viral infections during pregnancy. Am J Reprod Immunol. 2015;73(3):199–213. doi: 10.1111/aji.12355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mednick SA, Machon RA, Huttunen MO, Bonett D. Adult schizophrenia following prenatal exposure to an influenza epidemic. Arch Gen Psychiatry. 1988;45(2):189–192. doi: 10.1001/archpsyc.1988.01800260109013. [DOI] [PubMed] [Google Scholar]
- 45.Brown AS, et al. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Arch Gen Psychiatry. 2004;61(8):774–780. doi: 10.1001/archpsyc.61.8.774. [DOI] [PubMed] [Google Scholar]
- 46.Brown AS. Prenatal infection as a risk factor for schizophrenia. Schizophr Bull. 2006;32(2):200–202. doi: 10.1093/schbul/sbj052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burd I, Welling J, Kannan G, Johnston MV. Excitotoxicity as a common mechanism for fetal neuronal injury with hypoxia and intrauterine inflammation. Adv Pharmacol. 2016;76:85–101. doi: 10.1016/bs.apha.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 48.Dell’Ovo V, Rosenzweig J, Burd I, Merabova N, Darbinian N, Goetzl L. An animal model for chorioamnionitis at term. Am J Obstet Gynecol. 2015;213(3):387.e1–387.10. doi: 10.1016/j.ajog.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choi G, et al. The maternal IL17a pathway in mice promotes autism phenotypes in offspring. Science. 2016;351(6276):(6276) doi: 10.1126/science.aad0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith SE, Li J, Garbett K, Mirnics K, Patterson PH. Maternal immune activation alters fetal brain development through interleukin-6. J Neurosci. 2007;27(40):10695–10702. doi: 10.1523/JNEUROSCI.2178-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cardenas I, et al. Viral infection of the placenta leads to fetal inflammation and sensitization to bacterial products predisposing to preterm labor. J Immunol. 2010;185(2):1248–1257. doi: 10.4049/jimmunol.1000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caserta MT, Hall CB, Schnabel K, Lofthus G, McDermott MP. Human herpesvirus (HHV)-6 and HHV-7 infections in pregnant women. J Infect Dis. 2007;196(9):1296–1303. doi: 10.1086/522430. [DOI] [PubMed] [Google Scholar]
- 53.Li DK, et al. Genital herpes and its treatment in relation to preterm delivery. Am J Epidemiol. 2014;180(11):1109–1117. doi: 10.1093/aje/kwu242. [DOI] [PubMed] [Google Scholar]
- 54.Tanaka K, et al. Screening for vaginal shedding of cytomegalovirus in healthy pregnant women using real-time PCR: correlation of CMV in the vagina and adverse outcome of pregnancy. J Med Virol. 2006;78(6):757–759. doi: 10.1002/jmv.20619. [DOI] [PubMed] [Google Scholar]
- 55.Taylor Y, Melvin WT, Sewell HF, Flannelly G, Walker F. Prevalence of Epstein-Barr virus in the cervix. J Clin Pathol. 1994;47(1):92–93. doi: 10.1136/jcp.47.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zuo Z, Goel S, Carter JE. Association of cervical cytology and HPV DNA status during pregnancy with placental abnormalities and preterm birth. Am J Clin Pathol. 2011;136(2):260–265. doi: 10.1309/AJCP93JMIUEKRPIW. [DOI] [PubMed] [Google Scholar]
- 57.Cardenas I, et al. Placental viral infection sensitizes to endotoxin-induced pre-term labor: a double hit hypothesis. Am J Reprod Immunol. 2011;65(2):110–117. doi: 10.1111/j.1600-0897.2010.00908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Racicot K, et al. Viral infection of the pregnant cervix predisposes to ascending bacterial infection. J Immunol. 2013;191(2):934–941. doi: 10.4049/jimmunol.1300661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brown ZA, Benedetti J, Selke S, Ashley R, Watts DH, Corey L. Asymptomatic maternal shedding of herpes simplex virus at the onset of labor: relationship to preterm labor. Obstet Gynecol. 1996;87(4):483–488. doi: 10.1016/0029-7844(95)00457-2. [DOI] [PubMed] [Google Scholar]
- 60.McGee D, Poncil S, McAuliffe M, Smith A, Racicot K. Cervical viral infection causes estrogen receptor stabilization and premature cervical ripening. Am J Reprod Immunol. 2016;76:G86 [Google Scholar]
- 61.Burguete T, et al. Evidence for infection of the human embryo with adeno-associated virus in pregnancy. Hum Reprod. 1999;14(9):2396–2401. doi: 10.1093/humrep/14.9.2396. [DOI] [PubMed] [Google Scholar]
- 62.Creanga AA, et al. Severity of 2009 pandemic influenza A (H1N1) virus infection in pregnant women. Obstet Gynecol. 2010;115(4):717–726. doi: 10.1097/AOG.0b013e3181d57947. [DOI] [PubMed] [Google Scholar]
- 63.ANZIC Influenza Investigators Australasian Maternity Outcomes Surveillance System Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ. 2010;340:c1279. doi: 10.1136/bmj.c1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Siston AM, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303(15):1517–1525. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Michaan N, et al. Maternal and neonatal outcome of pregnant women infected with H1N1 influenza virus (swine flu) J Matern Fetal Neonatal Med. 2012;25(2):130–132. doi: 10.3109/14767058.2011.562569. [DOI] [PubMed] [Google Scholar]
- 66.Nakai A, Saito S, Unno N, Kubo T, Minakami H. Review of the pandemic (H1N1) 2009 among pregnant Japanese women. J Obstet Gynaecol Res. 2012;38(5):757–762. doi: 10.1111/j.1447-0756.2011.01812.x. [DOI] [PubMed] [Google Scholar]
- 67.Källén B, Olausson PO. Vaccination against H1N1 influenza with Pandemrix during pregnancy and delivery outcome: a Swedish register study. BJOG. 2012;119(13):1583–1590. doi: 10.1111/j.1471-0528.2012.03470.x. [DOI] [PubMed] [Google Scholar]
- 68.Richards JL, et al. Neonatal outcomes after antenatal influenza immunization during the 2009 H1N1 influenza pandemic: impact on preterm birth, birth weight, and small for gestational age birth. Clin Infect Dis. 2013;56(9):1216–1222. doi: 10.1093/cid/cit045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fell DB, et al. H1N1 influenza vaccination during pregnancy and fetal and neonatal outcomes. Am J Public Health. 2012;102(6):e33–e40. doi: 10.2105/AJPH.2011.300606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reddick KL, Jhaveri R, Gandhi M, James AH, Swamy GK. Pregnancy outcomes associated with viral hepatitis. J Viral Hepat. 2011;18(7):e394–e398. doi: 10.1111/j.1365-2893.2011.01436.x. [DOI] [PubMed] [Google Scholar]
- 71.Koga K, et al. Activation of TLR3 in the trophoblast is associated with preterm delivery. Am J Reprod Immunol. 2009;61(3):196–212. doi: 10.1111/j.1600-0897.2008.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ilievski V, Lu SJ, Hirsch E. Activation of toll-like receptors 2 or 3 and preterm delivery in the mouse. Reprod Sci. 2007;14(4):315–320. doi: 10.1177/1933719107302959. [DOI] [PubMed] [Google Scholar]
- 73.Kim CJ, Romero R, Chaemsaithong P, Kim JS. Chronic inflammation of the placenta: definition, classification, pathogenesis, and clinical significance. Am J Obstet Gynecol. 2015;213(4 suppl):S53–S69. doi: 10.1016/j.ajog.2015.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Racicot K, et al. Type I interferon regulates the placental inflammatory response to bacteria and is targeted by virus: mechanism of polymicrobial infection-induced preterm birth. Am J Reprod Immunol. 2016;75(4):451–460. doi: 10.1111/aji.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Norwitz ER, Schust DJ, Fisher SJ. Implantation and the survival of early pregnancy. N Engl J Med. 2001;345(19):1400–1408. doi: 10.1056/NEJMra000763. [DOI] [PubMed] [Google Scholar]
- 76.Charnock-Jones DS, Kaufmann P, Mayhew TM. Aspects of human fetoplacental vasculogenesis and angiogenesis. I. Molecular regulation. Placenta. 2004;25(2–3):103–113. doi: 10.1016/j.placenta.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 77.Kaufmann P, Mayhew TM, Charnock-Jones DS. Aspects of human fetoplacental vasculogenesis and angiogenesis. II. Changes during normal pregnancy. Placenta. 2004;25(2–3):114–126. doi: 10.1016/j.placenta.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 78.Mayhew TM, Charnock-Jones DS, Kaufmann P. Aspects of human fetoplacental vasculogenesis and angiogenesis. III. Changes in complicated pregnancies. Placenta. 2004;25(2–3):127–139. doi: 10.1016/j.placenta.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 79.Liu T, et al. Role of human cytomegalovirus in the proliferation and invasion of extravillous cytotrophoblasts isolated from early placentae. Int J Clin Exp Med. 2015;8(10):17248–17260. [PMC free article] [PubMed] [Google Scholar]
- 80.Chou D, Ma Y, Zhang J, McGrath C, Parry S. Cytomegalovirus infection of trophoblast cells elicits an inflammatory response: a possible mechanism of placental dysfunction. Am J Obstet Gynecol. 2006;194(2):535–541. doi: 10.1016/j.ajog.2005.07.073. [DOI] [PubMed] [Google Scholar]
- 81.Jun Y, et al. Human cytomegalovirus gene products US3 and US6 down-regulate trophoblast class I MHC molecules. J Immunol. 2000;164(2):805–811. doi: 10.4049/jimmunol.164.2.805. [DOI] [PubMed] [Google Scholar]
- 82.Arechavaleta-Velasco F, Koi H, Strauss JF, Parry S. Viral infection of the trophoblast: time to take a serious look at its role in abnormal implantation and placentation? J Reprod Immunol. 2002;55(1–2):113–121. doi: 10.1016/s0165-0378(01)00143-7. [DOI] [PubMed] [Google Scholar]
- 83.Griffiths P, Baboonian C. A prospective study of primary ctyomegalovirus infection during pregnancy. Br J Obstet Gynaecol. 1984;91(4):307–315. doi: 10.1111/j.1471-0528.1984.tb05915.x. [DOI] [PubMed] [Google Scholar]
- 84.Brown ZA, et al. Effects on infants of a first episode of genital herpes during pregnancy. N Engl J Med. 1987;317(20):1246–1251. doi: 10.1056/NEJM198711123172002. [DOI] [PubMed] [Google Scholar]
- 85.Xie F, von Dadelszen P, Nadeau J. CMV infection, TLR-2 and -4 expression, and cytokine profiles in early-onset preeclampsia with HELLP syndrome. Am J Reprod Immunol. 2014;71(4):379–386. doi: 10.1111/aji.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.von Dadelszen P, et al. Levels of antibodies against cytomegalovirus and Chlamydophila pneumoniae are increased in early onset pre-eclampsia. BJOG. 2003;110(8):725–730. [PubMed] [Google Scholar]
- 87.Schust DJ, Hill AB, Ploegh HL. Herpes simplex virus blocks intracellular transport of HLA-G in placentally derived human cells. J Immunol. 1996;157(8):3375–3380. [PubMed] [Google Scholar]
- 88.Nørskov-Lauritsen N, Aboagye-Mathisen G, Juhl CB, Petersen PM, Zachar V, Ebbesen P. Herpes simplex virus infection of cultured human term trophoblast. J Med Virol. 1992;36(3):162–166. doi: 10.1002/jmv.1890360303. [DOI] [PubMed] [Google Scholar]
- 89.Robb J, Benirschke K, Barmeyer R. Intrauterine latent herpes simplex virus infection and spontaneous abortion. Hum Pathol. 1986;17(12):1196–1209. doi: 10.1016/S0046-8177(86)80561-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Koi H, et al. Differential expression of the coxsackievirus and adenovirus receptor regulates adenovirus infection of the placenta. Biol Reprod. 2001;64(3):1001–1009. doi: 10.1095/biolreprod64.3.1001. [DOI] [PubMed] [Google Scholar]
- 91.Arechavaleta-Velasco F, Ma Y, Zhang J, McGrath CM, Parry S. Adeno-associated virus-2 (AAV-2) causes trophoblast dysfunction, and placental AAV-2 infection is associated with preeclampsia. Am J Pathol. 2006;168(6):1951–1959. doi: 10.2353/ajpath.2006.050781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Arechavaleta-Velasco F, et al. Adverse reproductive outcomes in urban women with adeno-associated virus-2 infections in early pregnancy. Hum Reprod. 2008;23(1):29–36. doi: 10.1093/humrep/dem360. [DOI] [PubMed] [Google Scholar]
- 93.Tobiasch E, et al. Detection of adeno-associated virus DNA in human genital tissue and in material from spontaneous abortion. J Med Virol. 1994;44(2):215–222. doi: 10.1002/jmv.1890440218. [DOI] [PubMed] [Google Scholar]
- 94.Jamieson DJ, Theiler RN, Rasmussen SA. Emerging infections and pregnancy. Emerging Infect Dis. 2006;12(11):1638–1643. doi: 10.3201/eid1211.060152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Piccinni MP, Lombardelli L, Logiodice F, Kullolli O, Parronchi P, Romagnani S. How pregnancy can affect autoimmune diseases progression? Clin Mol Allergy. 2016;14:11. doi: 10.1186/s12948-016-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Haake DA, Zakowski PC, Haake DL, Bryson YJ. Early treatment with acyclovir for varicella pneumonia in otherwise healthy adults: retrospective controlled study and review. Rev Infect Dis. 1990;12(5):788–798. doi: 10.1093/clinids/12.5.788. [DOI] [PubMed] [Google Scholar]
- 97.Paryani SG, Arvin AM. Intrauterine infection with varicella-zoster virus after maternal varicella. N Engl J Med. 1986;314(24):1542–1546. doi: 10.1056/NEJM198606123142403. [DOI] [PubMed] [Google Scholar]
- 98.Atmar RL, Englund JA, Hammill H. Complications of measles during pregnancy. Clin Infect Dis. 1992;14(1):217–226. doi: 10.1093/clinids/14.1.217. [DOI] [PubMed] [Google Scholar]
- 99.Christensen P, Schmidt H, Bang H, Andersen JM, Jordal B, Jensen O. An epidemic of measles in southern Greenland, 1951; measles in virgin soil. II. The epidemic proper. Acta Med Scand. 1953;144(6):430–449. doi: 10.1111/j.0954-6820.1953.tb15717.x. [DOI] [PubMed] [Google Scholar]
- 100.Anderson BL, Rouse DJ, Fitzsimmons C. Clinical characteristics of pregnant women with influenza-like illness during the 2009 H1N1 pandemic and use of a standardized management algorithm. Am J Obstet Gynecol. 2011;204(6 suppl 1):S31–S37. doi: 10.1016/j.ajog.2011.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ellington SR, et al. Pandemic 2009 influenza A (H1N1) in 71 critically ill pregnant women in California. Am J Obstet Gynecol. 2011;204(6 suppl 1):S21–S30. doi: 10.1016/j.ajog.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 102.Jamieson DJ, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009;374(9688):451–458. doi: 10.1016/S0140-6736(09)61304-0. [DOI] [PubMed] [Google Scholar]
- 103.Louie JK, Acosta M, Jamieson DJ, Honein MA, California Pandemic (H1N1) Working Group Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362(1):27–35. doi: 10.1056/NEJMoa0910444. [DOI] [PubMed] [Google Scholar]
- 104.Marcelin G, et al. Fatal outcome of pandemic H1N1 2009 influenza virus infection is associated with immunopathology and impaired lung repair, not enhanced viral burden, in pregnant mice. J Virol. 2011;85(21):11208–11219. doi: 10.1128/JVI.00654-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rasmussen SA, et al. Preparing for influenza after 2009 H1N1: special considerations for pregnant women and newborns. Am J Obstet Gynecol. 2011;204(6 suppl 1):S13–S20. doi: 10.1016/j.ajog.2011.01.048. [DOI] [PubMed] [Google Scholar]
- 106.Watanabe T, Kawaoka Y. Pathogenesis of the 1918 pandemic influenza virus. PLoS Pathog. 2011;7(1):e1001218. doi: 10.1371/journal.ppat.1001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Harris J. Influenza in pregnant women. JAMA. 1919;72(14):978–980. [Google Scholar]
- 108.Hardy JM, Azarowicz EN, Mannini A, Medearis DN, Cooke RE. The effect of Asian influenza on the outcome of pregnancy, Baltimore, 1957–1958. Am J Public Health Nations Health. 1961;51:1182–1188. doi: 10.2105/AJPH.51.8.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Freeman DW, Barno A. Deaths from Asian influenza associated with pregnancy. Am J Obstet Gynecol. 1959;78:1172–1175. doi: 10.1016/0002-9378(59)90570-8. [DOI] [PubMed] [Google Scholar]
- 110.Price ME, Fisher-Hoch SP, Craven RB, McCormick JB. A prospective study of maternal and fetal outcome in acute Lassa fever infection during pregnancy. BMJ. 1988;297(6648):584–587. doi: 10.1136/bmj.297.6648.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bello OO, Akinajo OR, Odubamowo KH, Oluwasola TA. Lassa fever in pregnancy: report of 2 cases seen at the University College Hospital, Ibadan. Case Rep Obstet Gynecol. 2016;2016:9673683. doi: 10.1155/2016/9673683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Racicot K, Aldo P, El-Guindy A, Kwon JY, Romero R, Mor G. Cutting edge: fetal/placental type I IFN can affect maternal survival fetal viral load during viral infection. J Immunol. 2017;198(8):3029–3032. doi: 10.4049/jimmunol.1601824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yockey LJ, et al. Vaginal exposure to Zika virus during pregnancy leads to fetal brain infection. Cell. 2016;166(5):1247–1256.e4. doi: 10.1016/j.cell.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Dick GW, Kitchen SF, Haddow AJ. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46(5):509–520. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 115.Mansuy JM, et al. Zika virus: high infectious viral load in semen, a new sexually transmitted pathogen? Lancet Infect Dis. 2016;16(4):405. doi: 10.1016/S1473-3099(16)00138-9. [DOI] [PubMed] [Google Scholar]
- 116.Rowland A, Washington CI, Sheffield JS, Pardo-Villamizar CA, Segars JH. Zika virus infection in semen: a call to action and research. J Assist Reprod Genet. 2016;33(4):435–437. doi: 10.1007/s10815-016-0684-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Venturi G, et al. An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill. 2016;21(8):30148. doi: 10.2807/1560-7917.ES.2016.21.8.30148. [DOI] [PubMed] [Google Scholar]
- 118.Brasil P, et al. Zika virus outbreak in Rio de Janeiro, Brazil: clinical characterization, epidemiological and virological aspects. PLoS Negl Trop Dis. 2016;10(4):e0004636. doi: 10.1371/journal.pntd.0004636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Brasil P, et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N Engl J Med. 2016;375(24):2321–2334. doi: 10.1056/NEJMoa1602412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Brasil P, et al. Guillain-Barre syndrome associated with Zika virus infection. Lancet. 2016;387(10026):1482. doi: 10.1016/S0140-6736(16)30058-7. [DOI] [PubMed] [Google Scholar]
- 121.Faria NR, et al. Zika virus in the Americas: early epidemiological and genetic findings. Science. 2016;352(6283):345–349. doi: 10.1126/science.aaf5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Heukelbach J, Alencar CH, Kelvin AA, de Oliveira WK, Pamplona de Goes Cavalcanti L. Zika virus outbreak in Brazil. J Infect Dev Ctries. 2016;10(2):116–120. doi: 10.3855/jidc.8217. [DOI] [PubMed] [Google Scholar]
- 123.Teixeira MG, Costa Mda C, de Oliveira WK, Nunes ML, Rodrigues LC. The epidemic of Zika virus-related microcephaly in Brazil: detection, control, etiology, and future scenarios. Am J Public Health. 2016;106(4):601–605. doi: 10.2105/AJPH.2016.303113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Calvet GA, Santos FB, Sequeira PC. Zika virus infection: epidemiology, clinical manifestations and diagnosis. Curr Opin Infect Dis. 2016;29(5):459–466. doi: 10.1097/QCO.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 125.Calvet G, et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. 2016;16(6):653–660. doi: 10.1016/S1473-3099(16)00095-5. [DOI] [PubMed] [Google Scholar]
- 126.de Oliveira CS, da Costa Vasconcelos PF. Microcephaly and Zika virus. J Pediatr (Rio J) 2016;92(2):103–105. doi: 10.1016/j.jped.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 127.Driggers RW, et al. Zika virus infection with prolonged maternal viremia and fetal brain abnormalities. N Engl J Med. 2016;374(22):2142–2151. doi: 10.1056/NEJMoa1601824. [DOI] [PubMed] [Google Scholar]
- 128.Dyer O. Zika virus spreads across Americas as concerns mount over birth defects. BMJ. 2015;351:h6983. doi: 10.1136/bmj.h6983. [DOI] [PubMed] [Google Scholar]
- 129.Garcez PP, et al. Zika virus impairs growth in human neurospheres and brain organoids. Science. 2016;352(6287):816–818. doi: 10.1126/science.aaf6116. [DOI] [PubMed] [Google Scholar]
- 130.Heymann DL, et al. Zika virus and microcephaly: why is this situation a PHEIC? Lancet. 2016;387(10020):719–721. doi: 10.1016/S0140-6736(16)00320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kleber de Oliveira W, et al. Increase in reported prevalence of microcephaly in infants born to women living in areas with confirmed Zika virus transmission during the first trimester of pregnancy — Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(9):242–247. doi: 10.15585/mmwr.mm6509e2. [DOI] [PubMed] [Google Scholar]
- 132.Mlakar J, et al. Zika virus associated with microcephaly. N Engl J Med. 2016;374(10):951–958. doi: 10.1056/NEJMoa1600651. [DOI] [PubMed] [Google Scholar]
- 133.Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects — reviewing the evidence for causality. N Engl J Med. 2016;374(20):1981–1987. doi: 10.1056/NEJMsr1604338. [DOI] [PubMed] [Google Scholar]
- 134.Ventura CV, et al. and Ventura LO. Ophthalmological findings in infants with microcephaly and presumable intra-uterus Zika virus infection. Arq Bras Oftalmol. 2016;79(1):1–3. doi: 10.5935/0004-2749.20160002. [DOI] [PubMed] [Google Scholar]
- 135.Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de Filippis AM. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol. 2016;47(1):6–7. doi: 10.1002/uog.15831. [DOI] [PubMed] [Google Scholar]
- 136.Martines RB, et al. Pathology of congenital Zika syndrome in Brazil: a case series. Lancet. 2016;388(10047):898–904. doi: 10.1016/S0140-6736(16)30883-2. [DOI] [PubMed] [Google Scholar]
- 137.Hamel R, et al. Biology of Zika virus infection in human skin cells. J Virol. 2015;89(17):8880–8896. doi: 10.1128/JVI.00354-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tabata T, et al. Zika virus targets different primary human placental cells, suggesting two routes for vertical transmission. Cell Host Microbe. 2016;20(2):155–166. doi: 10.1016/j.chom.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jurado KA, et al. Zika virus productively infects primary human placenta-specific macrophages. JCI Insight. 2016;1(13):e88461. doi: 10.1172/jci.insight.88461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Aldo P, You Y, Szigeti K, Horvath TL, Lindenbach B, Mor G. HSV-2 enhances ZIKV infection of the placenta and induces apoptosis in first-trimester trophoblast cells. Am J Reprod Immunol. 2016;76(5):348–357. doi: 10.1111/aji.12578. [DOI] [PubMed] [Google Scholar]
- 141.Clemens SA, Farhat CK. Seroprevalence of herpes simplex 1-2 antibodies in Brazil. Rev Saude Publica. 2010;44(4):726–734. doi: 10.1590/S0034-89102010000400017. [DOI] [PubMed] [Google Scholar]
- 142.Cugola FR, et al. The Brazilian Zika virus strain causes birth defects in experimental models. Nature. 2016;534(7606):267–271. doi: 10.1038/nature18296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bayer A, et al. Type III interferons produced by human placental trophoblasts confer protection against Zika virus infection. Cell Host Microbe. 2016;19(5):705–712. doi: 10.1016/j.chom.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]