Introduction
People living in rural Appalachia including portions of Kentucky suffer a disproportionate burden of negative health disparities. Heart disease and stroke, the two strongest disability risk factors, are increased in incidence in rural Appalachia compared to non-Appalachian regions.(Behringer & Friedell, 2006) The highest death rates for stroke occur in the southeastern United States (the “stroke belt”), which includes 26 counties in Appalachian Kentucky. This subregion has some of the highest stroke incidence rates in the stroke belt.
Community re-integration after hospitalization is an important goal of rehabilitation given the current emphasis on cost containment of inpatient care and the need to decrease the length of stay.(Forchheimer & Tate, 2004) However, the authors of a previous study determined that over the first year after stroke, participants reported that the process of community reintegration was marked by ongoing changes in their goals.(Wood, Connelly, & Maly, 2010) In addition, stroke survivors may experience further loss of physical function, falls, depression, and poor quality of life.(Carota et al., 2005; Cott, Wiles, & Devitt, 2007; Danzl et al., 2013; Pang, Eng, & Miller, 2007; Rundek et al., 2000; Yates, Lai, Duncan, & Studenski, 2002) High rates of hospital readmissions have been shown to be common within the first 12 months following discharge from an inpatient rehabilitation setting due to a successive stroke or other complications which may have been preventable.(Demaerschalk, Hwang, & Leung, 2010; Olson et al., 2013) Several authors have indicated that individuals with disabilities in rural areas are at increased risk of secondary complications related to a lack of access to specialized support services, lack of care coordination, and limited healthcare provider knowledge about healthcare needs of individuals with complex conditions such as stroke.(Danzl et al., 2015; Danzl, et al., 2013; Lustig, Weems, & Strauser, 2004)
Researchers have determined a significant number of stroke survivors have minimal recall of the acute care phase of their healthcare. (Danzl, et al., 2015; Danzl, et al., 2013; Hunt & Smith, 2004) A lack of foundational stroke knowledge, including stroke prevention, awareness of risk factors, and recognition of warning signs and symptoms, has been shown not only in the patients but also their caregivers. During the period immediately following discharge into the community, family caregivers often report that they were not prepared with the necessary training to enable a successful transition to the home environment. (J. E. Smith & Smith, 2000) These studies emphasize the need for continued education for persons who have had a stroke as well as their caregivers.
In addition to the need for follow-up education, there is an apparent need for navigational support for individuals who have had a stroke transitioning back into their community. Currently, the standard of care for individuals post-stroke who are not receiving follow-up rehabilitation typically involves 1–2 phone calls from a social worker or case manager. For individuals who live in rural communities, these calls usually originate several hours away at an urban acute care facility. This lack of continuity of care at the point of discharge from acute care back to the rural community can lead to the documented high rate of emergency department (ED) visits and re-hospitalization within the first 6 months post-discharge. Recent studies indicate the effectiveness of utilizing allied health professionals (physical therapists [PT], occupational therapists [OT], or nurses), to support access to services in urban settings.(Dewan, Skrypak, Moore, & Wainscoat, 2014; Poston, Dumas, & Edlund, 2014) To date, there have been no reports that have examined the effectiveness of using lay community health workers (CHWs) as navigators to support care transition for people who have had a stroke from the acute care setting back into underserved rural communities.
The purposes of this program assessment were to determine the community navigation required by people who have had a stroke in order to transition back to rural low-resource communities and to facilitate positive health outcomes. Specifically, the goals of this program assessment were to: 1) determine the types of resources accessed (e.g. enrolling in healthcare plans, medication waiver programs, durable medical equipment [DME], etc.) and follow-up education needed to support transitions from acute care to the community, 2) determine the 30-day hospital readmission rates and visits to the ED for participants in the program, and 3) determine the compliance with medications, physician visits, and out-patient rehabilitation visits.
Methods
The Kentucky Care Coordination for Community Transitions (KC3T) program utilizes a specially trained lay CHW as a navigator to support the transition of individuals with stroke and their caregivers from acute in-patient care back to their rural community through facilitation of communication between the clients and the healthcare providers and acquisition of essential resources (health insurance, medications, follow up appointments, etc.). Since the KC3T navigator is from the area she serves, she understands the culture and helps serve as the essential bridge between the healthcare system and that community. The KC3T navigator works closely with the in-patient rehabilitation and discharge planning teams to support essential follow-up education as well as assess healthcare and community resource needs.
KC3T provides support over a longer period of time than previously published reports. The KC3T navigator is in contact with the participant a minimum of 1×/week for the first three months and a minimum of 1× every other week for months 4–6.(Dewan, et al., 2014; Egan, Anderson, & McTaggart, 2010; Poston, et al., 2014) This duration of individualized patient centered care is in line with previous reports showing persons who have had a stroke require support over an extended period of time.(Demaerschalk, et al., 2010; Olson, et al., 2013)
The KC3T navigator was initially trained through the nationally recognized Kentucky Homeplace Community Health Worker Program. In addition, since the majority of individuals who have a stroke in our region also have one or more stroke-related risk factors (e.g., diabetes, hypertension, high BMI, smoking, etc.), the KC3T navigator has had additional training in chronic disease management. Specifically, the KC3T navigator is certified in chronic disease self-management (CDSMP) and diabetes self-management (DSMP) through Stanford University, and the Wellness Recovery Action Plan (WRAP), in order to support follow-up education with both the person who had a stroke, as well as the caregiver/family who usually share many of the risk factors for stroke.
Study Population
Participants with acute stroke receiving care at a regional inpatient rehabilitation hospital in southeastern (Appalachian) Kentucky were enrolled in the program. The counties in southeastern Kentucky in which services are provided are among the most economically distressed in the United States, have the greatest frequency of occurrence of stroke as well as the highest incidence of stroke risk factors (i.e. diabetes, hypertension, smoking, obesity, etc.). Prior to discharge from the inpatient rehabilitation facility, the navigator met with the patient and family to discuss the program and sign a consent to participate form. The initial pilot study was approved by the university’s Institutional Review Board. The navigator worked closely with the discharge planning team, the patient and family to assess resource needs and begin the process for obtaining those resources. In the few instances the person’s hospital stay was so short they were discharged prior to meeting with the KC3T navigator, an initial meeting was arranged within 1 week of the person returning to their home.
KC3T Encounter and Services Data
An encounter refers to a home visit, a telephone visit, an office visit, an offsite visit, or service facilitation. The first visit was always in the home in order to assess the home environment and the need for home modifications and DME. During each encounter several services were typically provided including: 1) completing paperwork for accessing agency and/or community resources (access and utilization of healthcare plans, access to medication waiver program, obtaining DME, and other community services), 2) reviewing education (see below) and discharge plan, and 3) assessing the participant’s compliance with rehabilitation and discharge plans. In addition, when not working directly with the person, the KC3T navigator continued spent her time obtaining needed services through time required contacting insurance companies and interfacing with medication waiver programs.
Compliance
Participant compliance with medications, physician visits and outpatient rehabilitation visits were tracked. Compliance with medications was assessed through participant self-report and the KC3T navigator’s documentation of medication waiver submittals to programs providing essential medications. Compliance with primary care physician and out-patient rehabilitation visits was verified through the KC3T navigator’s ongoing communication with the healthcare providers.
KC3T Navigation Primary Outcomes
The project’s primary outcomes were: 1) Number and types of stroke related risk factors, 2) type of follow-up education provided, 3) types of resources accessed (enrolling in healthcare plans, medications waiver program, durable medical equipment, home modifications, etc.), 4) number of 30-day hospital readmissions and ED visits, and 5) compliance with medications, physician visits, and out-patient rehabilitation visits. All data are housed in a specially developed and secure KC3T database and all results are presented as de-identified aggregates.
Results
Demographics
For this initial program assessment 30 individuals (17 females and 13 males) were enrolled between July 1, 2015 and May 31, 2016. The mean age was 65 years old with a range between 38 and 88 years of age. Over the 11 month assessment period 11 individuals transitioned out of the program. Seventy percent (n=21) of the participants were insured through Medicare and all but two were insured through one of the Kentucky-managed care programs.
Risk factors
Thirteen co-morbidities were tracked for enrolled participants (high blood pressure, high cholesterol, atrial fibrillation, previous transient ischemic attack, heart problems, previous stroke, asthma, cancer, COPD, arthritis, depression, kidney disease, and diabetes, plus the risk factor of tobacco use). Of these co-morbidities, those with the highest incidence were high cholesterol (92%), high blood pressure (85%), arthritis (74%), diabetes (63%), and depression (37%). The incidence of multiple co-morbidities was also examined and the results demonstrate a high incidence of multiple co-morbidities for individuals in the KC3T group (figure 1). Seventy percent (n=21) of the participants had 5 or more of the co-morbidities of interest.
Figure 1.
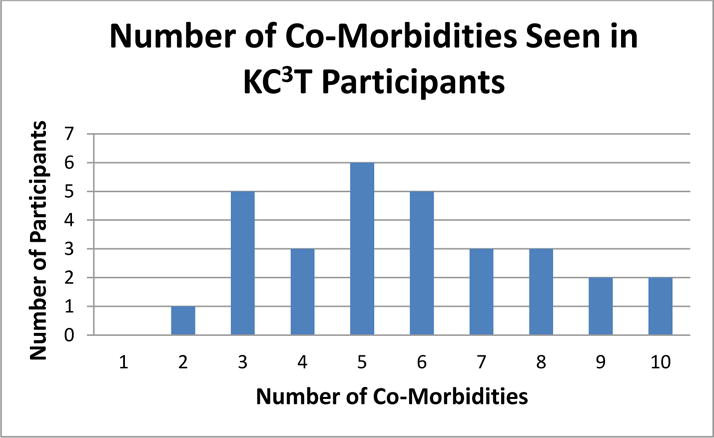
Demonstrates the high level of co-morbidities borne by the stroke population in southeastern Kentucky. Twenty one of the KC3T participants (70%) had 5 or more co-morbidities.
Encounters and Services Provided
There were 214 encounters performed by the KC3T navigator during the assessment period. Because of the distances needed to travel in the rural mountainous region, the majority of encounters were provided in the form of phone visits. Overall, the KC3T navigator provided 516 related services, of which provision of follow-up education made up 81% (n= 417). Fifty seven percent of participants (n=17) required assistance in obtaining essential DME, 37% (n=11) required assistance in enrolling in insurance and 43% (n=13) required assistance accessing essential medications.
Educational Reviews Provided
Over the course of the program assessment period, the KC3T navigator conducted 417 reviews of the educational materials provided to the participants and their caregivers (figure 2). The follow-up education was provided in collaboration with the rehabilitation care and discharge team and fell into five topic areas: 1) the stroke process, 2) medication management, 3) transfers and mobility, 4) chronic disease management, and 5) caregiver and family education. With respect to chronic disease management, the topic areas that were covered included management of hypertension, diabetes, high cholesterol, atrial fibrillation, and COPD, proper nutrition, smoking cessation, and compliance with medications.
Figure 2.
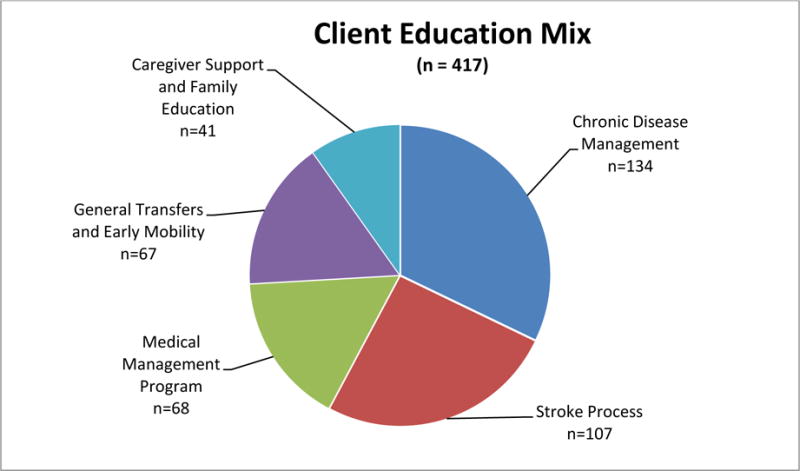
Demonstrates the topic areas covered by the KC3T navigator as part of the follow-up education. As demonstrated, chronic disease management education comprised 32% of the follow-up education followed by review of the stroke process.
Compliance Rates
With respect to compliance with medications, 92% (n=25) of the KC3T participants were compliant with their medications at the time of their navigator encounters. With respect to physician and out-patient rehabilitation visits, 96% (n=26) of the KC3T participants attended all scheduled physician visits and 70% (n=19) of the KC3T participants attended all of their scheduled out-patient rehabilitation visits.
Emergency Department (ED) Visits and Hospital Readmissions
In order to examine the effectiveness of KC3T to decrease 30-day ED visits and hospital readmissions, de-identified data with respect to 30-day hospital readmissions and ED visits were collected from 12 individuals who were treated at a regional inpatient rehabilitation hospital in southeastern Kentucky for stroke but chose not to participate in the KC3T program. Over the assessment period there were no 30-day ED visits by individuals in the KC3T program (Figure 4). In contrast, 83% (n=10) of those not recieving KC3T support had visited the ED at least one time within 30 days of discharge from inpatient rehabilitation. Two of these individuals had 5 ED visits and one person had 7 ED visits.
Within the KC3T participant group, there was one person who was readmitted to the hospital within 30 days of discharge back to their home (figure 3). This readmission was for treatment of an infection from a prior cancer-related surgery. In fact, it was during a home visit that the person asked the navigator to check the surgical site that was causing the person distress. After assessing the site, the KC3T navigator directed the person to contact their primary care physician immediately and the patient was then appropriately admitted to the hospital for treatment. In contrast to the KC3T group, 42% (n=5) of the control group reported a readmission to the hospital within 30 days of discharge from acute inpatient rehabilitation.
Figure 3.
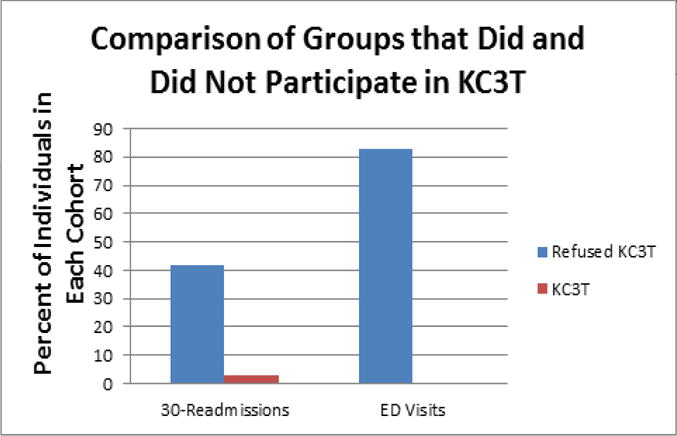
Demonstrates the difference in the number of 30-day readmissions and ED visits between those individuals who received services through KC3T and those who did not.
Support Group
Another result of this program was the development of a stroke survivor and caregiver support group that meets each month. This group provided an opportunity for peer support as well as additional education on various topics that are generated by the group. The meetings are held at the regional rehabilitation hospital, which provides the opportunity for patients and caregivers who are currently going through acute rehabilitation the opportunity to receive peer support from people who have already transitioned back to the community.
Discussion
Previous work had indicated a lack of community-based stroke rehabilitation services as well as distrust of existing primary care providers’ knowledge for providing care for individuals with complex conditions such as stroke. These conditions may be examples of why significant health disparities continue to exist in central Appalachia and the need exists for a care transitions navigator to bridge the transition from the acute care setting back to the community. The KC3T program was developed specifically to overcome these persistent health and healthcare disparities and to support the transition of individuals with neurological conditions such as stroke.
Health navigation has been increasingly employed for people with cancer with success in increasing screening and reducing time to care.(Feltner, Ely, Whitler, Gross, & Dignan, 2012; Ramsey et al., 2009) Researchers have recently examined the effectiveness of utilizing allied health professionals (PT, OT, or nurses) to support access to services.(Dewan, et al., 2014; Egan, et al., 2010; Poston, et al., 2014) While these previous studies using healthcare professionals have demonstrated a decrease in 30-day readmission rates, they were significantly more costly to provide due to salary requirements and are did not employee navigators from the local communities. In addition, they did not provide the range of services that the KC3T navigator provides.
Because the KC3T navigator is a specially trained lay CHW, and not a professional such as a nurse, PT or OT, we propose this KC3T program is more economical to conduct and is truly community based. This is especially true given the amount of support KC3T provides its participants. The model is also unique in being implemented in a low-resources rural area that has historically been plagued by economic, environmental, educational, and healthcare related problems.
Caregivers are infrequently trained to assist the patient in activities such as bathing, administering medication, performing rehabilitation, or helping a patient up after a fall.(Kerr & Smith, 2001) Only rarely is advice given regarding the psychological and emotional impact of a stroke and how to assist the patient in managing these complex feelings.(J. E. Smith & Smith, 2000) Information and assistance in accessing health care services once the patient has been discharged into the community are also difficult to obtain. Patients and caregivers report not routinely being provided with information on how to access the next step in the sequence of care. They are then left to locate the necessary services, schedule appropriate appointments, arrange for their payment, and provide medical history by themselves.(J. E. Smith & Smith, 2000) Financial aid can also be difficult to obtain if they do not receive information regarding the existence of funds and how to access them.(J. E. Smith & Smith, 2000) In other instances, progression through the care continuum is perceived to happen too quickly, before the caregiver can prepare the home, modify his/her job or reduce work hours, or sell their home to move in with the stroke patient.(J. E. Smith & Smith, 2000) Another contributor to fragmentation is related to the onus being on the patient to initiate follow-up visits and progress evaluations, especially once discharged from the acute setting.(L. N. Smith, Lawrence, Kerr, Langhorne, & Lees, 2004; L. N. Smith et al., 2004) This results in the patient and/or family caregiver initiating most contacts with the health care system, especially after the transition to community care. Programs such as KC3T provide the essential support for both the person who had the stroke and also the caregivers in order to facilitate a more successful transition back to the community.
Health care professionals are also affected by the lack of information: the medical records that each of them holds about the patients they have treated are not shared across care environments, which can lead to medical errors and incomplete information, duplication, and increased financial costs. The result is that they must obtain medical information from the patient and re-administer tests when new patients arrive in their system of care. The use of care transitions navigators, such as in the KC3T program, supports communication across care environments.
Need for Follow-up Education
Goal setting is essential in any rehabilitation plan, but goals change across the care continuum.(Laver, Halbert, Stewart, & Crotty, 2010; S. Magasi, Hammel, Heinemann, Whiteneck, & Bogner, 2009; S. R. Magasi, Heinemann, & Whiteneck, 2008) Researchers have shown that the time needed to adjust, the lack of knowledge about recovery, differences in readiness to set goals, and the passive role assigned to patients all contribute to a lack of collaborative effort in setting goals in acute and rehabilitation settings.(Danzl, et al., 2013; S. R. Magasi, et al., 2008) A recent study by Sanders et al. (2014),(Sanders et al., 2014) showed that even after receiving recommended stroke education, only 12% of the subjects could identify all 5 warning signs for stroke, 43% could name all of their personal risk factors, and fewer than half could identify the type of stroke they had suffered. These findings indicate the need for follow-up education beyond that which is provided during the acute rehabilitation stay. The results of our study agree with this assessment; the single largest service provided by the KC3T navigator was follow-up education to both the person who had the stroke as well as their family/caregiver.
A study by Wolfe et al., 2010,(Wolfe et al., 2010) examined the efficacy of providing tailored evidence-based education to providers, patients and caregivers at multiple time points post-stroke. This study provided the education through email or postal mail and found no improvement in risk factor management. This is in line with our current study that demonstrated the need for extensive hands-on educations provided extensively over a long period of weeks and months in person or by telephone.
Utilization of Costly Healthcare Environments
Multiple authors have shown that readmission is common within the first 12 months following discharge from an inpatient rehabilitation setting due to a successive stroke or another complication which may have been prevented (eg. fractures from falls, pneumonia, urinary tract infections, anxiety).(Bravata, Ho, Meehan, Brass, & Concato, 2007; Demaerschalk, et al., 2010; Fonarow et al., 2012; Lichtman, Leifheit-Limson, Jones, Wang, & Goldstein, 2013) Research examining care coordination for people with cancer and stroke demonstrate a shift from utilization of more costly specialists and hospital care to more efficient primary care with reduced hospitalizations. (Claiborne, 2006; Feltner, et al., 2012; Ramsey, et al., 2009) The results from the KC3T program agree with these findings, in that the use of the a specially trained CHW as the KC3T navigator was able to shift visits from the ED to the primary care physician and there was only one 30-day readmission, which was not stroke related.
Improvement in Compliance by Patients
Barriers to well-controlled risk factors and medication compliance include inadequate follow-up and monitoring of stroke survivors by healthcare professionals, ineffective education of patients regarding risk modification and event prevention, and inadequate self-management by patients.(Wolfe, et al., 2010) Possible reasons for the minimal compliance with physician and rehabilitation visits can include a lack of transportation and lack of gas money to drive the considerable distances to attend visits. Our previous work has shown both of these reasons to be very real in our rural communities and are a focus of continued resource development. With respect to compliance with medication, troubles with financial hardship to afford the medications as well as accessing the available waiver systems have been reported. The KC3T navigator is specially trained to help support the participants in enrolling in the medication waiver programs so they can access the medication they require. This support likely translated into the high medication compliance rates reported in this program assessment.
Treatment adherence rates have also been shown to improve with the patients’ and caregivers’ level of knowledge.(T. A. Miller, 2016; Zhang, Terry, & McHorney, 2014) To that end, the overall largest service provided by the KC3T navigator was follow-up education and chronic disease management.
Stroke best practices recommend including relatives throughout the continuum of stroke care. (E. L. Miller et al., 2010) However, a study by Rochette et al., 2014,(Rochette, Racine, Lefebvre, Bastien, & Tellier, 2014) demonstrated a gap remaining between actual and ideal services for relatives of individuals who have had a stroke. The KC3T program has been developed to provide education and support not only to the individuals who had the stroke, but also to their family and caregivers to support their care duties as well as to support their own chronic disease management/prevention, because they tend to have many of the same risk factors as their loved ones.
One direct result of the KC3T program was the development of a stroke survivor and caregiver support group in Appalachian rural Kentucky that meets each month and is the only support group of its type within the region. This group provides an opportunity for peer support as well as additional education on various topics that are generated by the group. The meetings are held at the regional rehabilitation hospital, which provides the opportunity for patients and caregivers who are currently going through acute rehabilitation the opportunity to receive peer support prior from former patients to their discharge back to the community. Participants in the group are engaged in the process and determine topics to be covered by guest speakers and periodic brainstorming sessions are held so that each member can provide feedback on topics that are meaningful to them as they continue their community integration and recovery. Guest speakers are then selected based upon the group’s recommendations. Topics have ranged from respite care and community based services to diabetes and cardiac education. As a result of their involvement in the topic selection, attendance has remained stable and an improved understanding of the educational topic has occurred, resulting in improved outcomes.
Limitations
While the results from this initial program assessment are very promising, there are several limitations that must be addressed. First, the current program only covers a small geographic area of 7 counties. In order to determine the true efficacy of this program it will need to be scaled up to include a much larger population and region. This work is in the proposal stage. In addition, we would like to determine whether this program can be effective in the urban setting. Secondly, the current program only has one navigator, which has limited the sample size of patients who can be enrolled in the program. In order to establish the scalability of this model, additional navigators will need to be trained and the service area expanded to include additional rural communities. Finally, future studies will examine the effectiveness of KC3T in improving patient and caregiver quality of life by including measures such as the Stroke Impact Scale and a caregiver burden scale as program outcome measures.
Conclusion
The Kentucky Care Coordination for Community Transitions (KC3T) appears to effectively support community transitions for individuals with who have had a stroke and their caregivers living in rural Kentucky through the facilitation of access to medical, social, and environmental services.
Acknowledgments
We would also like to thank all of the individuals who participated in the program. The authors would like to acknowledge Ms. Julie Brock for her work in developing the manuscript.
Funding: The pilot study was originally funded through a small grant through the University of Kentucky Center for Clinical and Translational Sciences (NIH CTSA UL1TR000117). The KC3T program is currently funded through a collaborative agreement between the Appalachian Regional Healthcare and the University of Kentucky.
Footnotes
Conflict of Interest: P Kitzman is the Director of the KC3T program and K. Hudson is the KC3T Navigator.
Contributor Information
Patrick Kitzman, Professor, Department of Rehabilitation Sciences, University of Kentucky, College of Health Sciences, Lexington, KY.
Keisha Hudson, KC3T Navigator, University of Kentucky, Center for Excellence in Rural Health, Hazard, KY.
Violet Sylvia, Director for Rehabilitation Services, Appalachian Regional Healthcare.
Frances Feltner, Director of the Center for Excellence in Rural Health, Hazard KY.
Johnnie Lovins, Rural Health External Community Health Worker Director, Center for Excellence in Rural Health, Hazard, KY.
References
- Behringer B, Friedell GH. Appalachia: where place matters in health. [Editorial Research Support, U.S. Gov’t, P.H.S.] Preventing chronic disease. 2006;3(4):A113. [PMC free article] [PubMed] [Google Scholar]
- Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J. Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the medicare population. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S.] Stroke; a journal of cerebral circulation. 2007;38(6):1899–1904. doi: 10.1161/STROKEAHA.106.481465. [DOI] [PubMed] [Google Scholar]
- Carota A, Berney A, Aybek S, Iaria G, Staub F, Ghika-Schmid F, et al. A prospective study of predictors of poststroke depression. [Research Support, Non-U.S. Gov’t] Neurology. 2005;64(3):428–433. doi: 10.1212/01.WNL.0000150935.05940.2D. [DOI] [PubMed] [Google Scholar]
- Claiborne N. Effectiveness of a care coordination model for stroke survivors: a randomized study. [Randomized Controlled Trial] Health & social work. 2006;31(2):87–96. doi: 10.1093/hsw/31.2.87. [DOI] [PubMed] [Google Scholar]
- Cott CA, Wiles R, Devitt R. Continuity, transition and participation: preparing clients for life in the community post-stroke. Disability and rehabilitation. 2007;29(20–21):1566–1574. doi: 10.1080/09638280701618588. [DOI] [PubMed] [Google Scholar]
- Danzl MM, Harrison A, Hunter EG, Kuperstein J, Sylvia V, Maddy K, et al. “A Lot of Things Passed Me by”: Rural Stroke Survivors’ and Caregivers’ Experience of Receiving Education From Health Care Providers. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2015 doi: 10.1111/jrh.12124. [DOI] [PubMed] [Google Scholar]
- Danzl MM, Hunter EG, Campbell S, Sylvia V, Kuperstein J, Maddy K, et al. “Living with a ball and chain”: the experience of stroke for individuals and their caregivers in rural Appalachian Kentucky. [Research Support, N.I.H., Extramural] The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2013;29(4):368–382. doi: 10.1111/jrh.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demaerschalk BM, Hwang HM, Leung G. US cost burden of ischemic stroke: a systematic literature review. [Research Support, Non-U.S. Gov’t Review] The American journal of managed care. 2010;16(7):525–533. [PubMed] [Google Scholar]
- Dewan B, Skrypak M, Moore J, Wainscoat R. A service evaluation of the feasibility of a community-based consultant and stroke navigator review of health and social care needs in stroke survivors 6 weeks after hospital discharge. Clinical medicine. 2014;14(2):134–140. doi: 10.7861/clinmedicine.14-2-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan M, Anderson S, McTaggart J. Community navigation for stroke survivors and their care partners: description and evaluation. [Research Support, Non-U.S. Gov’t] Topics in Stroke Rehabilitation. 2010;17(3):183–190. doi: 10.1310/tsr1703-183. [DOI] [PubMed] [Google Scholar]
- Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Social work in health care. 2012;51(5):430–440. doi: 10.1080/00981389.2012.657296. [DOI] [PubMed] [Google Scholar]
- Fonarow GC, Pan W, Saver JL, Smith EE, Reeves MJ, Broderick JP, et al. Comparison of 30-day mortality models for profiling hospital performance in acute ischemic stroke with vs without adjustment for stroke severity. [Comparative Study Research Support, Non-U.S. Gov’t] JAMA : the journal of the American Medical Association. 2012;308(3):257–264. doi: 10.1001/jama.2012.7870. [DOI] [PubMed] [Google Scholar]
- Forchheimer M, Tate DG. Enhancing community re-integration following spinal cord injury. NeuroRehabilitation. 2004;19(2):103–113. [PubMed] [Google Scholar]
- Hunt D, Smith JA. The personal experience of carers of stroke survivors: an interpretative phenomenological analysis. Disability and rehabilitation. 2004;26(16):1000–1011. doi: 10.1080/09638280410001702423. [DOI] [PubMed] [Google Scholar]
- Kerr SM, Smith LN. Stroke: an exploration of the experience of informal caregiving. [Research Support, Non-U.S. Gov’t] Clinical rehabilitation. 2001;15(4):428–436. doi: 10.1191/026921501678310234. [DOI] [PubMed] [Google Scholar]
- Laver K, Halbert J, Stewart M, Crotty M. Patient readiness and ability to set recovery goals during the first 6 months after stroke. Journal of allied health. 2010;39(4):e149–154. [PubMed] [Google Scholar]
- Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] Stroke; a journal of cerebral circulation. 2013;44(12):3429–3435. doi: 10.1161/STROKEAHA.113.003165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustig DC, Weems GH, Strauser DR. Rehabilitation Service Patterns: A Rural/Urban Comparison of Success Factors. Journal OF Rehabilitation. 2004;70(3):13–19. [Google Scholar]
- Magasi S, Hammel J, Heinemann A, Whiteneck G, Bogner J. Participation: a comparative analysis of multiple rehabilitation stakeholders’ perspectives. [Comparative Study] Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2009;41(11):936–944. doi: 10.2340/16501977-0450. [DOI] [PubMed] [Google Scholar]
- Magasi SR, Heinemann AW, Whiteneck GG. Participation following traumatic spinal cord injury: an evidence-based review for research. [Congresses Research Support, U.S. Gov’t, Non-P.H.S.] The journal of spinal cord medicine. 2008;31(2):145–156. doi: 10.1080/10790268.2008.11760705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller EL, Murray L, Richard L, Zaorowitz RD, Bakas T, Clark P. Comprehensive overview of nursing and interdisciplinary rehabilitation care of stroke patient: a scientific statement from the American Heart Association. Stroke; a journal of cerebral circulation. 2010;41:2402–2448. doi: 10.1161/STR.0b013e3181e7512b. [DOI] [PubMed] [Google Scholar]
- Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. [Review] Patient education and counseling. 2016;99(7):1079–1086. doi: 10.1016/j.pec.2016.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson DM, Cox M, Pan W, Sacco RL, Fonarow GC, Zorowitz R, et al. Death and rehospitalization after transient ischemic attack or acute ischemic stroke: one-year outcomes from the adherence evaluation of acute ischemic stroke-longitudinal registry. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.] Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2013;22(7):e181–188. doi: 10.1016/j.jstrokecerebrovasdis.2012.11.001. [DOI] [PubMed] [Google Scholar]
- Pang MY, Eng JJ, Miller WC. Determinants of satisfaction with community reintegration in older adults with chronic stroke: role of balance self-efficacy. [Research Support, Non-U.S. Gov’t] Physical therapy. 2007;87(3):282–291. doi: 10.2522/ptj.20060142. [DOI] [PubMed] [Google Scholar]
- Poston KM, Dumas BP, Edlund BJ. Outcomes of a quality improvement project implementing stroke discharge advocacy to reduce 30-day readmission rates. Journal of nursing care quality. 2014;29(3):237–244. doi: 10.1097/NCQ.0000000000000040. [DOI] [PubMed] [Google Scholar]
- Ramsey S, Whitley E, Mears VW, McKoy JM, Everhart RM, Caswell RJ, et al. Evaluating the cost-effectiveness of cancer patient navigation programs: conceptual and practical issues. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Review] Cancer. 2009;115(23):5394–5403. doi: 10.1002/cncr.24603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochette A, Racine E, Lefebvre H, Bastien J, Tellier M. Actual and ideal services in acute care and rehabilitation for relatives post-stroke from three perspectives: Relatives, stroke clients and health professionals. [Multicenter Study Research Support, Non-U.S. Gov’t] Journal of rehabilitation medicine. 2014;46(1):16–22. doi: 10.2340/16501977-1228. [DOI] [PubMed] [Google Scholar]
- Rundek T, Mast H, Hartmann A, Boden-Albala B, Lennihan L, Lin IF, et al. Predictors of resource use after acute hospitalization: the Northern Manhattan Stroke Study. [Research Support, U.S. Gov’t, P.H.S.] Neurology. 2000;55(8):1180–1187. doi: 10.1212/wnl.55.8.1180. [DOI] [PubMed] [Google Scholar]
- Sanders K, Schnepel L, Smotherman C, Livingood W, Dodani S, Antonios N, et al. Assessing the impact of health literacy on education retention of stroke patients. [Research Support, Non-U.S. Gov’t] Preventing chronic disease. 2014;11:E55. doi: 10.5888/pcd11.130259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JE, Smith DL. No map, no guide. Family caregivers’ perspectives on their journeys through the system. [Research Support, Non-U.S. Gov’t] Care management journals : Journal of case management ; The journal of long term home health care. 2000;2(1):27–33. [PubMed] [Google Scholar]
- Smith LN, Lawrence M, Kerr SM, Langhorne P, Lees KR. Informal carers’ experience of caring for stroke survivors. [Research Support, Non-U.S. Gov’t] Journal of advanced nursing. 2004;46(3):235–244. doi: 10.1111/j.1365-2648.2004.02983.x. [DOI] [PubMed] [Google Scholar]
- Smith LN, Norrie J, Kerr SM, Lawrence IM, Langhorne P, Lees KR. Impact and influences on caregiver outcomes at one year post-stroke. [Research Support, Non-U.S. Gov’t] Cerebrovascular diseases. 2004;18(2):145–153. doi: 10.1159/000079268. [DOI] [PubMed] [Google Scholar]
- Wolfe CD, Redfern J, Rudd AG, Grieve AP, Heuschmann PU, McKevitt C. Cluster randomized controlled trial of a patient and general practitioner intervention to improve the management of multiple risk factors after stroke: stop stroke. [Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Review] Stroke; a journal of cerebral circulation. 2010;41(11):2470–2476. doi: 10.1161/STROKEAHA.110.588046. [DOI] [PubMed] [Google Scholar]
- Wood JP, Connelly DM, Maly MR. ‘Getting back to real living’: A qualitative study of the process of community reintegration after stroke. Clinical rehabilitation. 2010;24(11):1045–1056. doi: 10.1177/0269215510375901. [DOI] [PubMed] [Google Scholar]
- Yates JS, Lai SM, Duncan PW, Studenski S. Falls in community-dwelling stroke survivors: an accumulated impairments model. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S. Research Support, U.S. Gov’t, P.H.S.] Journal of rehabilitation research and development. 2002;39(3):385–394. [PubMed] [Google Scholar]
- Zhang NJ, Terry A, McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. [Meta-Analysis Review] The Annals of pharmacotherapy. 2014;48(6):741–751. doi: 10.1177/1060028014526562. [DOI] [PubMed] [Google Scholar]


