Abstract
Background
Alien limb phenomenon occurs in 50–60% of patients with corticobasal syndrome (CBS) and usually presents with an “alien hand” phenomenon. The “alien foot” presentation is rarer and may be misdiagnosed, as foot involvement can lead to erroneous localization of the clinical problem to the knee, hip, or back. Subsequently misdiagnoses such as myelopathy, radiculopathy, functional disorder, stiff leg syndrome, neuromyotonia, and painful leg moving toes syndrome may occur.
Case report
We describe two patients with alien foot symptoms that resulted in multiple opinions from different specialists, multiple diagnostic and therapeutic procedures, and delayed diagnosis. Eventually a diagnosis of CBS was made in both. Alien foot symptoms may be more common than initially thought and can result in a delayed diagnosis of CBS.
Conclusion
The inclusion of this clinical finding in recently proposed diagnostic criteria highlights the need for increased clinical awareness.
Keywords: Alien limb, alien leg, corticobasal syndrome
Introduction
“Alien hand” syndrome has been reported in up to 60% of patients with corticobasal syndrome (CBS).1 The hand moves on its own and frequently does not obey the patient’s commands. Current criteria for the probable diagnosis of CBS include an asymmetric presentation and two of the following: limb rigidity/akinesia, limb dystonia, limb myoclonus plus two of either orobuccal/limb apraxia or cortical sensory deficit or alien limb phenomenon. “Possible CBS” may be diagnosed if there is one of limb rigidity, limb dystonia or limb myoclonus (may be symmetric) and one of orobuccal/limb apraxia, cortical sensory deficit or alien limb phenomenon. An alien hand is commonly recognized as part of CBS, but clinicians may not consider the possibility of an “alien foot” leading to delayed diagnosis and inappropriate investigations and treatment. We present two patients who presented with alien foot symptoms that led to a delayed diagnosis of CBS.
Case reports
Case 1
An 80-year-old male complained of right foot pain and a “tingling” sensation that spread to the right knee. He was referred to an orthopedic surgeon because of lumbosacral spine disease and L4/L5 decompression was performed. However, the symptoms progressed. He developed an involuntary slow abduction/adduction of his toes on the right side. Magnetic resonance imaging (MRI) of the brain showed small vessel ischemic disease (Figure 1A); MRI of the cervical and thoracic spine was normal and the lumbar sacral spine showed postoperative changes. The abnormal movements spread to the ankle with involuntary dorsiflexion and plantar flexion. He stopped driving.
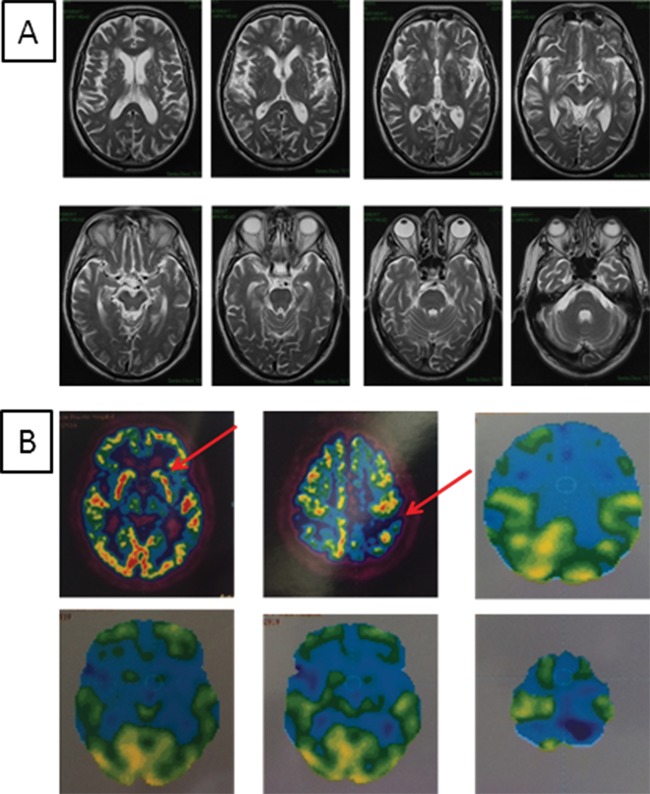
Figure 1. Brain imaging of patient 1. (A) Magnetic resonance imaging brain scan: small vessel ischemic disease. (B) Fludeoxyglucose positron emission tomography and computed tomography: diffuse moderate left basal ganglia hypometabolism, moderate regional left posterior parietal hypometabolism and mild-moderate left frontal hypo metabolism.
Further MRI of the lumbar spine imaging showed a tight right L4 nerve root in the lateral recess. He received nerve root injections and a foot splint for a “foot drop.” Nine months later, at the age of 81 years, he had a right L5 decompression by a different orthopedic surgeon with no improvement. At this point neurological opinion was sought. Neurological examination at age 81 showed repetitive movements of his right foot, and flexion extension of the toes. The diagnoses considered included an unusual organic disorder such as gait apraxia, “conversion disorder,” or “consciously derived” disorder. A second opinion was sought from a movement disorder specialist. Initially he was unable to walk during that assessment but after an hour he was able to run, and a diagnosis of a functional disorder was made. At age 82 he was seen by a third neurologist and a diagnosis of “painful leg moving toes” was made because of the slow adduction–abduction toe movements, but a diagnosis of atypical stiff leg syndrome was also considered. Anti-glutamic acid decarboxylase antibodies were negative.
Conduction studies of the right peroneal and tibial motor nerves were normal. Needle electromyography (EMG) found no evidence of motor axonal loss in the right-sided L4, L5 or S1 myotomes but brief runs of normal motor unit activity were recorded in tibialis anterior, peroneus longus, extensor hallucis longus and medial gastrocnemius muscles, synchronous with visible involuntary movements in the right lower limb. Motor unit activity was absent at rest and did not occur synchronously in antagonist muscles, making stiff limb syndrome unlikely. A later video shows some jerky foot movements consistent with myoclonus and undefined toe movements (Video 1). The remaining neurological examination was normal, including cognition clonazepam (1 mg morning, 0.5 mg afternoon, 0.5 mg evening) and amitriptyline (25 mg morning, 50 mg evening) did not help.
Video 1. Patient 1: Abduction and adduction of the toes on the right side, involuntary dorsiflexion and flexion of the right ankle and myoclonus.
Owing to ongoing pain in his right leg, he was started on a fentanyl transdermal patch 12 µg/hour by a pain specialist.
At age 82 he was referred to another specialty movement disorder clinic. By this stage, the patient described the right leg as “having its own mind.” There were now some involuntary movements in his right hand and left leg. When standing, the doctor had to stand on his right foot to hold it in place (Video 2). By the age of 83, right-sided bradykinesia, stooped posture, and shuffling gait had developed. Frontal release signs (grasp and palmomental reflexes) developed. He developed right-hand stimulus-sensitive myoclonus, astereognosia, ideomotor apraxia, rigidity, and “magnetism” (the patient’s hand follows the examiner’s hand as if attracted to it like a magnet) (Video 3). Reflexes were brisk (Medical Research Council scale grade 3) with spastic catch at the knees but flexor plantar responses. Pinprick sensation was decreased up to the right ankle. Proprioception and vibration were grossly impaired up to the knee on the right side and mildly impaired on the left. Pregabalin 25 mg twice a day and levodopa/carbidopa (Levodopa 100 mg/carbidopa 25 mg (up to three times daily)) were introduced. Fludeoxyglucose (18F) positron emission tomography and computed tomography PET/CT showed diffuse moderate left basal ganglia hypometabolism, moderate regional left posterior parietal hypometabolism, and mild–moderate left frontal hypometabolism (Figure 1B). He was diagnosed with CBS. A year later, the patient’s cognition deteriorated further (Montreal Cognitive Assessment Test score 20/30). The patient is currently bed-bound in a residential care facility.
Video 2. Patient 1: Involuntary movements of the right leg “alien leg”. In order for the patient to stand up the doctor had to stand on his right foot to hold it in place.
Video 3. Patient 1: Right alien leg, magnetism, grasp and stimulus sensitive myoclonus in both hands.
Case 2
A 72-year-old female presented with a 2-year history of falls and inability to stop when rushing the net while playing tennis. She was seen at three different hospitals and by multiple specialists (old age medicine, orthopedic surgeon, neurologist) but no definite diagnosis was made. She had a family history of parkinsonism (grandmother and two first cousins).
She stated: “when I was climbing a step, suddenly I found myself sitting down” or “I had to crawl back to bed as I felt that my legs could not bear the weight underneath me.” She had difficulty putting her left foot into her shoe as the foot was moving involuntarily and “had a mind of its own” (Video 4). She felt unsteady and was concerned that the left leg “will let her down.” She stopped playing tennis as she noted that her left leg did not obey her when moving side to side on the court.
Video 4. Patient 1: Left alien leg, difficulty putting a shoe on.
At 72 years there was no eye movement abnormality, no agraphesthesia, and no astereognosis. She was unsteady on tandem gait and failed a pull test. She had a stimulus-subtle sensitive myoclonus in both hands (worse on the right). There was mild rigidity with decreased coordination of the left leg and irregular “wiggling movements” were noted in the tibialis anterior. There was no increased sweating or cramping to suggest neuromyotonia. Power was normal and reflexes were brisk throughout. Sensation was normal.
Investigations for falls were normal, including a 24-hour blood pressure monitor, Holter monitor, tilt test, and routine blood tests. Lumbar puncture showed a slightly increased protein level at 76 mg/dL (normal, <45 mg/dL). MRI of the brain was normal and MRI of the lumbar spine showed modest spondylosis at L1/2, L2/3 and L5/S1 without nerve root impingement.
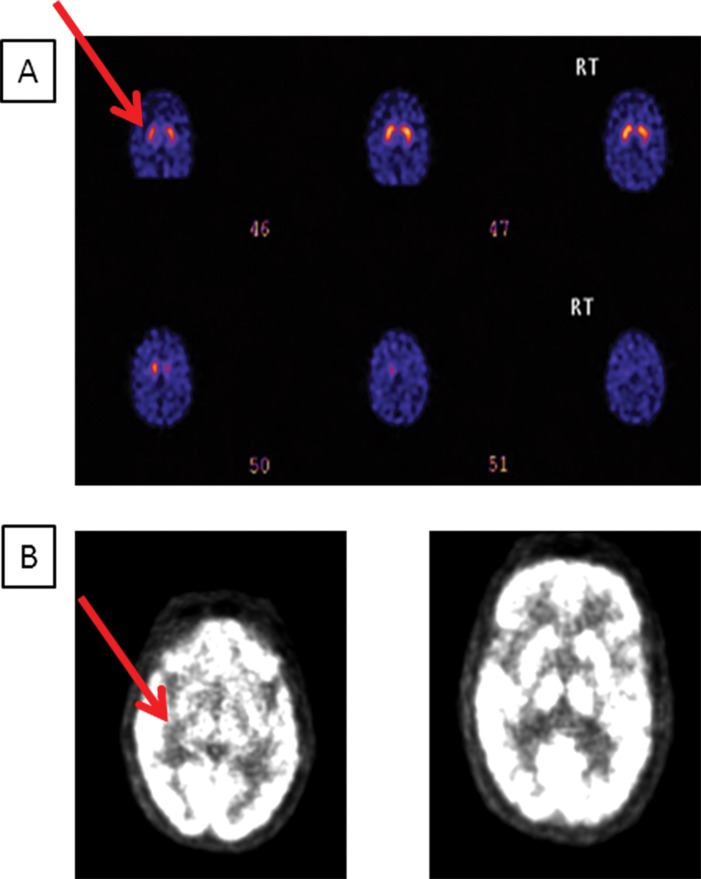
A nuclear magnetic dopaminergic brain scan (DAT scan) showed subtle decreased uptake of tracer in the left posterior putamen (Figure 2A). 18F PET/CT showed reduced metabolic activity in the bilateral insula, perisylvian regions, and midline pre-frontal cortex (Figure 2B). There was additional right parietal and basal ganglia hypometabolism suggestive of the diagnosis of CBS. EMG/NCS showed no evidence of myotonia or myokymia. She was diagnosed with CBS.
Figure 2. (A) Patient 2 nuclear magnetic dopaminergic brain scan: subtle left tracer uptake reduction in the putamen. (B) Patient 2 fludeoxyglucose positron emission tomography and computed tomography: reduced metabolic activity in the bilateral insula, perisylvian regions and midline pre-frontal cortex.
The patient required a walking aid by the age of 73 years, a rollator by 74, and wheelchair by 76. At 78 years she was anarthric. The patient also developed bilateral hand myoclonus, masked facies, and rigidity in all limbs.
She lives in a residential care setting requiring assistance for all her activities of daily living.
Discussion
Alien limb phenomenon is rare at presentation of CBS, but may develop in 50–60% of patients.1 While the alien limb phenomenon is generally understood as an involuntary movement of a limb, an accepted definition remains unclear and there is significant variation in the description of this sign.
Thus the diagnosis is challenging.
Alien limb usually presents with an alien hand phenomenon. It rarely presents as an alien foot. Hu et al.2 reported a 58-year-old female with paresthesia and involuntary toe wiggling/complex multidirectional movements of the leg and foot for 2 years before a diagnosis of CBS. MRI of the brain sometimes shows focal atrophy contralateral to the alien limb.
In our first patient MRI showed only microvascular changes and was entirely normal in the second.
A review of 108 cases of pathologically confirmed corticobasal degeneration from the Mayo clinic showed that the alien limb phenomenon is more common (65%) with the left-sided CBS (right-sided hemisphere involvement).3 It is possible that complex cortical phenomena such as an alien limb are under diagnosed in right-sided CBS (left-hemisphere involvement) similar to the right-sided neglect associated with left parietal lobe damage. Three alien limb variants are recognized: two anterior (including frontal and callosal) and a posterior.
The frontal variant is due to lesions of the cingulate cortex, dominant medial prefrontal cortex, supplementary motor area, or the corpus callosum. The callosal variant results from callosal injury. The posterior variant may be due to thalamic, parietal, or occipital lobe injury. A distinct pathological location has not been definitely associated with the alien limb phenomenon as exceptions and overlap are frequent.3,4
Foot and leg involvement can lead to erroneous localization of the problem to knee, hip, or back. As a result misdiagnoses may be seen such as myelopathy, radiculopathy, amyotrophic lateral sclerosis, neuromyotonia, stiff leg syndrome, functional movement disorder, or painful leg moving toes syndrome.5,6 Similarly erroneous diagnoses of cervical radiculopathy, cervical myelopathy, neuropathy, and painful arm-moving fingers syndrome may occur with the alien arm phenomenon; however, an alien hand/arm is usually diagnosed quicker than an alien foot/leg. When CBS presents with complex cortical phenomena such as an alien limb, paresthesia, apraxia, or primary progressive aphasia without parkinsonism the diagnosis may be delayed or missed.
Why is the alien hand phenomenon more common than the alien foot? Perhaps because the hand has a much bigger cortical representation; hence, the neuropathology is more likely to affect the area. Or perhaps an alien foot/leg is more frequently thought to be back, hip, or knee problems, leading to referral to the wrong specialty.
Inappropriate investigations, procedures and operations can often result. It is important to acknowledge that the abduction–adduction toe movements in our first patient are regarded as specific for painful leg–moving toes syndrome and their presence outside this syndrome is unusual.
CBS is usually a sporadic disease; however, our second patient had a family history of parkinsonism. Intriguingly, the original description of Corticobasal Ganglionic Degeneration by Reibez et al.7 included an Irish patient with a strong family history of parkinsonism.
Both cases highlight the difficult diagnostic path when a patient is seen by multiple specialists (family physician, old age medicine, orthopedic surgeon, neurologists), resulting in unnecessary procedures and operations.
Eventually a diagnosis of CBS was made in both.
It is important that clinicians are aware of the “alien leg” phenomenon given that this is now included in the diagnostic criteria for CBS.8
Footnotes
Funding: None.
Financial Disclosures: None.
Conflict of Interest: The authors report no conflict of interest.
Ethics Statement: All patients that appear on video have provided written informed consent; authorization for the videotaping and for publication of the videotape was provided.
References
- 1.Lang A, Boeve B, Bergeron C. Corticobasal syndrome. In: Jankovic J, Tolosa E, editors. Parkinson’s disease and movement disorders. fifth edition. Lippincott Williams and Wilkins, a Wolters Kluwer business; Philadelphia, USA: 2007. pp. 186–203. [Google Scholar]
- 2.Hu WT, Josephs KA, Ahiskog E, et al. MRI correlates of alien leg-like phenomenon in corticobasal degeneration. Mov Dis J. 2005;20:870–873. doi: 10.1002/mds.20451. doi: 10.1002/mds.20451. [DOI] [PubMed] [Google Scholar]
- 3.Graff-Radford, Rubin MN, Jones DT, et al. The alien limb phenomenon. J Neurol. 2013:1880–1888. doi: 10.1007/s00415-013-6898-y. doi: 10.1007/s00415-013-6898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarva H, Deil A, Severt WL. Pathophysiology and treatment of alien hand syndrome. Tremor Other Hyperkinet Mov. 2014:4. doi: 10.7916/D8VX0F48. doi: 10.7916/D8VX0F48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gozubatik-Celik G, Gunduz A, Oguz S, Kiziltan G, Ertan S. An unusual case of corticobasal syndrome. Arch Neuropsychiatry. 2014;51:410–411. doi: 10.5152/npa.2014.7663. doi: 10.5152/npa.2014.7663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneider JA, Watts RL, Gearing M, Brewer RP, Mirra SS. Corticobasal degeneration: neuropathologic and clinical heterogeneity. Neurology. 1997;48:959–69. doi: 10.1212/wnl.48.4.959. doi: 10.1212/WNL.48.4.959. [DOI] [PubMed] [Google Scholar]
- 7.Rebeiz JJ, Kolodny EH, Richardson EP. Corticodentatonigral degeneration with neuronal achromasia: a progressive disorder of late adult life. Trans Am Neurol Assoc. 1967;92:23–26. [PubMed] [Google Scholar]
- 8.Armstrong MJ, Litvan I, Lang AE, et al. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013;80:496–503. doi: 10.1212/WNL.0b013e31827f0fd1. doi: 10.1212/WNL.0b013e31827f0fd1. [DOI] [PMC free article] [PubMed] [Google Scholar]