Abstract
Purpose
To evaluate a bacterial dot hybridization (BDH) assay for the diagnosis of bacterial keratitis (BK).
Methods
Sixty-one qualified corneal scrapings from 61 patients with suspected microbial keratitis were collected consecutively and prospectively. Among the 61 patients, 16 cases were BK and 45 cases were non-BK, including fungal keratitis, viral keratitis, parasitic keratitis, and non-microbial keratitis. Molecular diagnosis of BK in these corneal scrapes was performed using the BDH assay with three universal bacterial probes (PB1, PB2, and PB3) and three genus-specific probes (Aci, Klb, and Psu) to detect Acinetobacter, Klebsiella, and Pseudomonas, respectively. Signals were standardized after grayscale image transformation for objective validation using receiver operating characteristic (ROC) curves.
Results
The standardized intensities for the three universal probes differed statistically significantly between the BK group and the non-BK group. Based on the ROC curves, the sensitivities of PB1, PB2, and PB3 were 81.3%, 81.3%, and 93.8%, and the specificities were 71.1%, 88.9%, and 91.1%, respectively. The sensitivity and specificity of the Psu probe were 92% and 100%, respectively, while those of the Aci and Klb probes could not be estimated because there were no BK cases caused by Acinetobacter spp. or Klebsiella spp.
Conclusions
The BDH assay is an effective molecular approach to improve the diagnosis of BK. Because the bias from bacterial contamination on the ocular surface can be minimized with signal standardization, the assay has the potential to be adopted for routine clinical practice.
Introduction
Bacterial keratitis (BK) is the most common microbial keratitis in temperate countries [1,2] and is a leading cause of corneal opacities leading to visual loss worldwide [3-5]. The rapid and fulminant course of BK causes inevitable corneal ulceration and further corneal perforation unless timely treatment is provided [6,7]. Most patients with BK can be cured using fortified antibiotics or fluoroquinolone without microbial identification [8,9]. However, inappropriate use of antibiotics may lead to bacterial resistance to the empirical regimen [10-15] and confusing clinical presentations [16-19], which are difficult to differentially diagnose. Even when the bacterial infection is eventually controlled, patients with delayed diagnosis and ineffective treatment may require keratoplasty to recover corneal clarity and vision [7,20,21]. Therefore, laboratory assessments of clinically suspected BK should not be neglected [22].
Culture is time-consuming and can fail for some fastidious microorganisms; therefore, several different media may be needed to improve the recovery rate [23,24]. Direct microscopy is the most rapid method, but this technique requires large corneal scrapings and expertise [22]. PCR is effective for the diagnosis of almost all kinds of ocular infectious diseases [25-27]; PCR is not only faster than culture but also requires smaller samples than direct microscopy. Several PCR-based diagnostic tests have been widely adopted by physicians and associated medical staff in clinical settings [28,29]. We further found the dot hybridization assay, a PCR-based molecular test, is highly sensitive for the diagnosis of fungal keratitis and is useful for differentiating Acanthamoeba keratitis from herpes keratitis [30,31]. Based on these previous studies, a DNA dot hybridization assay can be expected to provide an add-on diagnostic test for BK.
Contact lens–related BK is the most common BK, especially for young adults and children [32,33]. To assess bacterial bioburden on contact lens care systems, a bacterial dot hybridization (BDH) assay using oligonucleotide probes immobilized on a nylon membrane has been developed [34]. The assay has been used as a tool for assessing and predicting the bacterial bioburden of orthokeratology storage cases [35]. This molecular test is able to detect bacteria at low densities, irrespective of viability status. In a clinical context, this extremely high sensitivity may be undesired because nonviable bacteria and bacterial flora on the ocular surface do not cause infectious keratitis [36]. Therefore, the aim of this study was to assess the clinical potential of the BDH assay for diagnosing BK.
Methods
Participants
All procedures adhered to the Declaration of Helsinki and the ARVO statement on human subjects. Institutional Review Board (IRB)/Ethics Committee approval (approval number 102–2193C) was obtained from the Committee of Medical Ethics and Human Experiments of Chang Gung Memorial Hospital (CGMH, Taiwan). Informed consent was obtained from each subject. Corneal samples from clinically suspected patients were prospectively collected in the Kaohsiung CGMH from January 1, 2013, to December 12, 2014. A DNA sample was extracted within 4 days after each scraping sample was collected. One part of each DNA sample was used for routine PCR examination, and the other was stored at −70 °C for the BDH assay.
Clinical specimens
For clinically suspected microbial keratitis with corneal ulceration, a standard corneal scraping was performed following sterile operating procedures using a #15 sterilized knife under biomicroscopy [31]. For patients with lesions of ≥3 mm, each corneal scrape was divided into three parts; one part was examined using routine culture (aerobic bacteria, anaerobic bacteria, mycobacteria, and fungi), the second part was examined with direct microscopy (Gram stain and acid-fast stain), and the third part was washed in a 1.5 ml sterile microfuge tube containing 1 ml of normal saline and stored at −20 °C before DNA extraction. For patients with lesions between 2 and 3 mm, the corneal scrape was divided into two approximately equivalent parts; one part was examined for culture, and the other part was stored for DNA extraction. Patients with lesions of <2 mm were excluded. For patients with positive bacterial culture results, the bacterial load by culture was routinely estimated according to the semiquantitative method [37] by the Department of Laboratory Medicine of CGMH.
Microbiological examinations to define a true BK sample included direct microscopy, culture, or pathological examination (if available). A true BK sample was defined as at least one positive bacterial detection result in the microbiological examinations. A true non-BK sample was defined as no positive detection results for bacteria in the microbiological examinations.
DNA extraction and PCR
Before DNA extraction, the thawed corneal scrape in normal saline was transferred to a 1.5 ml microcentrifuge tube and centrifuged at 13,200 ×g in a microcentrifuge for 10 min. A clearly visible pellet at the inner wall near the tip of the microfuge tube was recognized as a qualified corneal scrape. Patients with unqualified scrapes were excluded from the study. DNA in the precipitate after centrifugation was extracted using a commercial kit (DNeasy Blood & Tissue Kit, Qiagen, Valencia, CA) to obtain 100 μl of purified DNA.
One part (2.5 μl) of the purified DNA was used for the routine PCR examination using bacteria-specific universal primers: 2F (5′-TTG TAC ACA CCG CCC GTC-3′) and 10R (5′-TTC GCC TTT CCC TCA CGG TA-3′) [38]. The PCR mixture (25 μl) consisted of 2.5 μl of template DNA, 0.4 μM each primer, and other necessary reagents from a PCR kit (JMR-THS5; JMR Holdings, Inc., St. Augustine, FL). PCR was performed using the following thermocycling conditions: initial denaturation, 95 °C, 3 min; 35 cycles of denaturation (95 °C, 30 s), annealing (55 °C, 45 s), and extension (72 °C, 45 s); and a final extension step at 72 °C for 10 min, with a concentration of 0.4 μM for the forward and reverse primers. A positive control was included in each run using template DNAs of Pseudomonas aeruginosa ATCC 10,944. A negative control was included in each run using replacing the template DNA with sterile water. Amplicons were analyzed with 2% agarose gel electrophoresis and stained with a noncarcinogenic dye (SafeView, NBS Biologicals Ltd., Huntingdon, UK). A band at approximately 1,000 bp was indicative of positive bacterial detection.
Another part (2.5 μl) of the extracted DNA was used for the BDH assay. Bacteria-specific universal primers 13BF (5′-digoxigenin-GTG AAT ACG TTC CCG GGC CT-3′) and 6R (5′-digoxigenin-GGG TTY CCC CRT TCR GAA AT-3′; Y = C or T; R = A or G) were used to amplify a DNA fragment that encompassed a portion of the 16S rRNA gene, the 16S-23S rRNA spacer region, and a portion of the 23S rRNA gene. Each primer was labeled with a digoxigenin molecule at its 5′ end. The PCR conditions and positive and negative controls were the same as those used in the routine PCR examination.
Immobilization of oligonucleotide probes on a nylon membrane
Immobilization of oligonucleotide probes on a nylon membrane was described previously [39]. The universal bacterial probes were designed from conserved sequences at the 3′ end of the 16S rRNA gene, and the genus-specific probes were designed from the 16S-23S rDNA internal transcribed spacer as described previously (Figure 1) [34]. Each probe was diluted 1:1 (final concentration, 10 μM) with a tracking dye solution and spotted on a positively charged nylon membrane (Roche, Mannheim, Germany) using a spotter (SR-A300; EZlife Technology, Taipei, Taiwan) [34]. A digoxigenin-labeled irrelevant probe (code M; 5′-digoxigenin-GCA TAT CAA TAA GCG GAG GA-3′) was used as a marker and spotted on the membrane to form a cross (0.6 cm × 0.4 cm). After all the probes were spotted, the membrane was exposed to an ultraviolet (UV) shortwave (Stratalinker 1800; Stratagene, La Jolla, CA) for 30 s to fix the probes on the membrane.
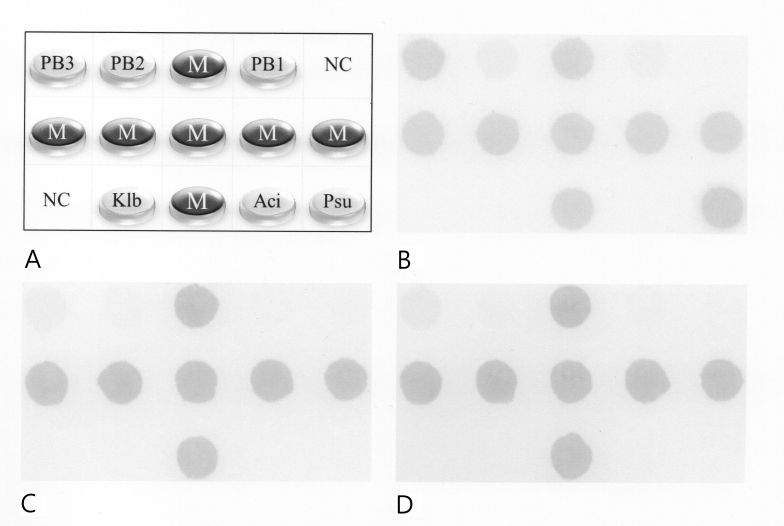
Figure 1.
The bacterial dot hybridization assay. A: Layout of oligonucleotide probes on the array (0.6 cm × 0.4 cm). The universal bacteria probes PB1, PB2, and PB3 were designed from a conserved region at the 3′ end of the 16S rRNA gene. Dots labeled “NC” were negative controls (tracking dye only). Dots labeled “M” were position markers, that is, an irrelevant digoxigenin-labeled oligonucleotide. Dots labeled “Psu,” “Aci,” and “Klb” were genus-specific probes used to identify the Pseudomonas, Acinetobacter, and Klebsiella species, respectively. Probe sequences for all dots were shown in our previous study [34]. B−D: Representative hybridization patterns for 10 ng, 10 pg, and 10 fg of P. aeruginosa DNA.
The BDH assay
A 10-µl aliquot of the PCR product was used for the BDH assay. The procedures for prehybridization and hybridization (55 °C for 60 min) have been described previously [39]. The reagents used in this study included alkaline phosphatase-conjugated anti-digoxigenin antibodies (Anti-Digoxigenin-AP, Fab fragments, catalog no. 11,093,274,910; Roche) and color development using phosphatase substrates (NBT/BCIP Stock Solution, catalog no. 11,681,451,001; Roche). The hybridized spots (400 μm in diameter) could be read by the naked eye. Images of the hybridized arrays were captured with a scanner (Perfection V600 Photo; Epson, Tokyo, Japan).
The hybridization signal intensity was quantified using ImageJ (developed by Wayne Rasband, National Institutes of Health, Bethesda, MD) and described previously [34]. Briefly, each captured image was adjusted to a fixed size (300 pixels × 200 pixels) and transformed to grayscale. The gray level of each hybridized dot was detected and recorded. Gray levels in the image background were estimated by averaging the negative controls (NC; tracing dye only). The mean gray levels of the markers were calculated by averaging the levels of all the marker dots. The corrected intensity of the markers was obtained by subtracting the background level from the mean gray level of the markers. Similarly, the corrected intensity of a bacterial probe was obtained by subtracting the background level from the gray level of a bacterial probe. The standardized intensity of a bacterial probe was defined as the corrected intensity of the bacterial probe divided by the corrected intensity of the markers in the same image.
Statistical analysis
Mann-Whitney U tests were used to analyze the differences in the age and standardized intensities of the probes between groups (p < 0.05 was considered statistically different). Differences in demographic parameters and risk factors (other than age) between groups were analyzed using Fisher’s exact tests. Receiver operating characteristic (ROC) curve analysis was used to determine the signal thresholds of the universal bacterial probes according to the defined true BK and non-BK samples. The Spearman correlation coefficient was used to analyze the correlation between the probe intensity and the bacterial load by culture [37] using an online calculator (Social Science Statistics).
Results
Participants
A total of 61 patients with corneal ulcer (61 eyes) with suspected microbial keratitis, consisting of 16 patients with BK and 45 patients with non-BK, participated in this study (Table 1). Among the patients with BK, one had bacterial and fungal polymicrobial keratitis. The patients with non-BK had herpes simplex keratitis (n = 1), fungal keratitis (n = 19), Acanthamoeba keratitis (n = 1), microsporidia keratitis (n = 1), and non-microbial keratitis (n= 23). There were no statistically significant differences between the two groups with respect to demography, risk factors, and complications, except the BK group had a higher frequency of hypopyon formation (p<0.028; Table 1). The patients with hypopyon in the BK group were all infected with P. aeruginosa.
Table 1. Demographic data for corneal ulcer patients with suspected microbial keratitis.
| Bacterial keratitis (n = 16) | Non-bacterial keratitis (n = 45) | P-valuec | |
|---|---|---|---|
| Sex, F:M |
6:10 |
16:29 |
1.000 |
| Age, mean ± S.D. |
54.4 ± 14.6 |
54.7 ± 19.3 |
0.755 |
| Laterality, OD:OS |
11:5 |
29:16 |
1.000 |
| Ocular risk factors |
|
|
|
| Wear contact lens, N (%) |
3 (18.8%) |
8 (18.8%) |
1.000 |
| Trauma, N (%) |
5 (31.3%) |
13 (28.9%) |
1.000 |
| Othersa, N (%) |
4 (25.0%) |
18 (40.0%) |
0.370 |
| Untraceable, N (%) |
4 (25.0%) |
6 (13.3%) |
0.431 |
| Systemic risk factors |
|
|
|
| Diabetes mellitus, N (%) |
4 (25.0%) |
7 (15.6%) |
0.457 |
| Cancer, N (%) |
1 ( 6.3%) |
0 ( 0.0%) |
0.262 |
| Untraceable, N (%) |
11 (68.8%) |
38 (84.4%) |
0.270 |
| Complications |
|
|
|
| Hypopyon, N (%) |
7 (43.8%) |
5 (11.1%) |
0.028 |
| Surgeryb, N (%) | 2 (12.5%) | 7 (15.6%) | 1.000 |
aThis item included swimming, farming work, neovascular glaucoma, pseudophakic bullous keratopathy, phthisis cornea, instillation of topical corticosteroids or anti-glaucoma agents. bSurgery was indicated by refractory to medical therapy and severe corneal melting to perforation. The surgical modalities included amniotic membrane transplantation, anterior lamellar keratoplasty, penetrating keratoplasty, and evisceration. cMann–Whitney U test was used to compare the continuous variable (age), while Fisher’s exact test was used to compare the categorical variables (i.e., variables other than age). P < 0.05 was statistically significant.
Patients with corneal ulcer with suspected microbial keratitis assessed using the BDH assay with universal bacterial probes
The signals of the universal bacteria probes (probes PB1, PB2, and PB3) were generally different (PB3 > PB2 > PB1) within the BK group (Figure 1B). Although the signals obtained using these probes were lower for patients in the non-BK group than in the BK group (Figure 1C,D), they were detectable by the naked eye, especially for PB3. These results implied that the BDH assay can detect bacterial contamination from ocular surface flora.
To examine the capacities of the three universal bacterial probes to differentiate BK from non-BK, the standardized intensities of the three probes were compared (Figure 2A). The average signal intensities, in decreasing order, were PB3 > PB2 > PB1 for the BK group and the non-BK group. The signals of all three universal bacterial probes were statistically significantly different between the two groups (Figure 2A).
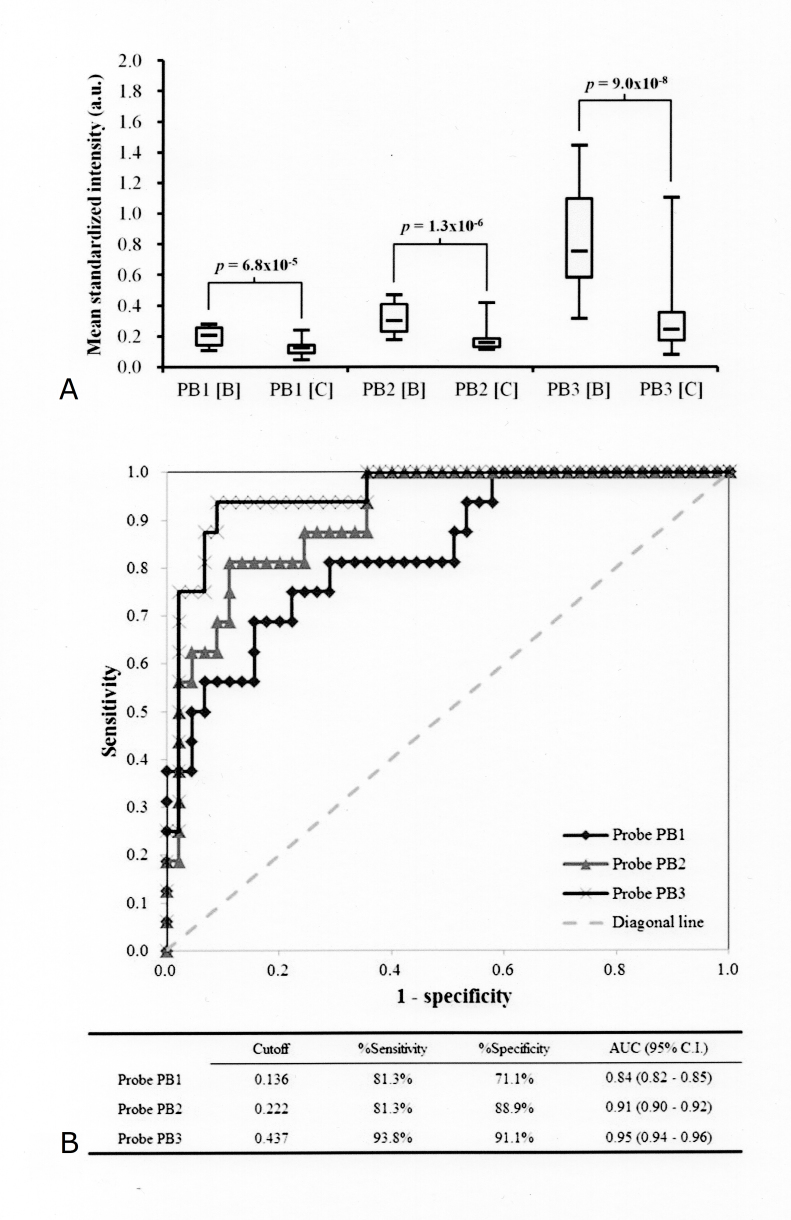
Figure 2.
The probe PB3 is the most valid probe among the three universal bacteria probes for diagnosing bacterial keratitis. A: Comparison of standardized hybridization intensities between bacterial keratitis [B] (n = 16) and non-bacterial keratitis [C] (n = 45) for the three universal bacteria probes (PB1, PB2, and PB3). B: Determination of the signal cutoff values for the three universal bacteria probes (PB1, PB2, and PB3) based on the defined groups: true bacterial keratitis (n = 16) versus non-bacterial keratitis (n = 45). The cutoff values were obtained based on a receiver operating characteristic (ROC) curve analysis. The inserted table summarizes the performance of the cutoff values for PB1, PB2, and PB3 to differentiate bacterial keratitis and non-bacterial keratitis. AUC, area under the curve; CI, confidence interval.
To account for the interfering signals from ocular surface flora, ROC plots were used to determine the signal thresholds for the three bacterial universal probes according to the defined BK cases (Figure 2B). Corresponding to the cutoff points of the three probes, the sensitivities of the probes PB1, PB2, and PB3 were 81.3%, 81.3%, and 93.8%, and the specificities of the three probes were 71.1%, 88.9%, and 91.1%, respectively. Based on the area under the ROC curve, the probe effectiveness for differentiating BK from non-BK was PB3 > PB2 > PB1 (Figure 2B).
Target bacterial detection by the genus-specific probes using the BDH assay
Among the 61 subjects, no positive signals were detected for the Aci and Klb probes, and there were no positive cultures of Acinetobacter spp. and Klebsiella spp. These results indicated 100% specificity and negative predictive rates, and no false positives for the two probes.
In a comparison of the standardized signal intensities among the patients with non-BK, the patients with non-Pseudomonas BK, and the patients with Pseudomonas BK, the mean signal intensities for the Psu probe were statistically significantly different (Figure 3A). The signal cutoff value for the Psu probe was determined based on the ROC plot according to the culture results for the 61 subjects (Figure 3B). The sensitivity and specificity for the genus-specific probe Psu were 92% and 100%, respectively.
Figure 3.
The probe Psu is a highly sensitive genus-specific probe for diagnosing Pseudomonas keratitis. A: Comparison of standardized hybridization intensities between Pseudomonas keratitis (Psu BK; n = 13) and non-Pseudomonas keratitis, including non-bacterial keratitis (non-BK; n = 45) and non-Pseudomonas bacterial keratitis (non-Psu BK; n = 3) for the Pseudomonas-specific probe (Psu). B: Determination of the signal cutoff values of the probe Psu based on the two groups: Pseudomonas keratitis (n = 13) and non-Pseudomonas keratitis (n = 48). The cutoff values were obtained with a receiver operating characteristic (ROC) analysis. The inserted table summarizes the performance of the cutoff value of Psu to identify Pseudomonas keratitis. AUC, area under the curve; CI, confidence interval.
Association between the standardized probe signals and the bacterial load by culture for the patients with BK
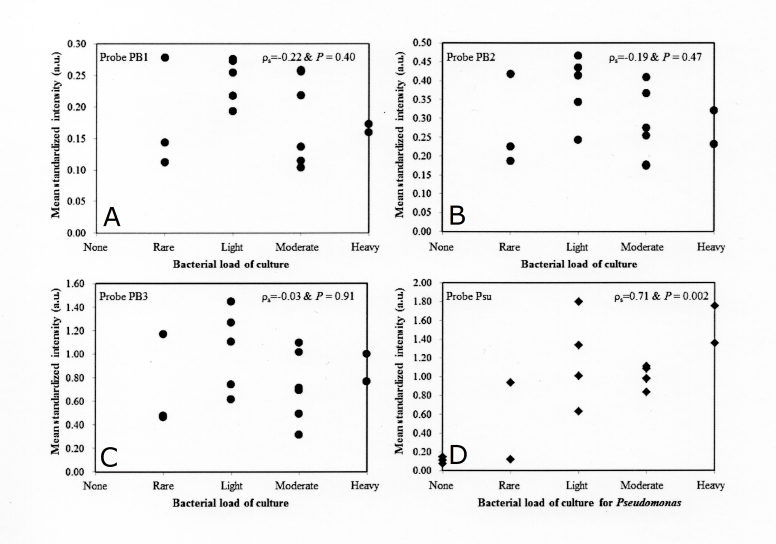
For the patients with BK, the signal of all three universal bacterial probes was not correlated with the bacterial load by culture (Figure 4A-C). However, the signal for the Psu probe was statistically significantly correlated with the bacterial load by culture for the patients with BK (Figure 4D). Therefore, the probe Psu might have the potential to estimate the severity of Pseudomonas keratitis clinically.
Figure 4.
Correlation analysis between the probe signal and the bacterial load by culture for the 16 patients with bacterial keratitis. A–C: The standardized intensities of the three universal bacterial probes (PB1, PB2, and PB3) with the corresponding bacterial load by culture for each patient are shown. D: The standardized intensities for the Psu probe with the corresponding bacterial load by culture for Pseudomonas spp. for each patient are shown. ρ, Spearman correlation coefficient; p<0.05 was considered statistically significant.
Discussion
False-positive results are a particular concern with respect to the molecular diagnosis of BK because the ocular surface harbors non-viable bacteria and bacterial flora [36]. Using the BDH assay, which was originally developed to assess the bacterial bioburden of the orthokeratology storage case (Figure 1A) [34], positive signals were detected with universal bacterial probes for several patients with non-BK (Figures 1C,D), consistent with these concerns. However, the probe signals were statistically significantly weaker for the patients with non-BK compared with those for the patients with BK using the BDH assay (Figure 2A and 3A). According to the analysis of the ROC plots, all universal bacterial probes had clinical potential for BK diagnosis, especially PB3 (Figure 2B). Furthermore, for the genus-specific probes, Psu was highly sensitive and specific for the diagnosis of Pseudomonas keratitis (Figure 3B).
For all patients, the signal intensities for the probes Aci and Klb were similar to the image background (Figure 1B–D). The two probes might be used to exclude the pathogen-caused Acinetobacter and Klebsiella infections. However, the clinical utility of the two probes could not be assessed in this study because none of the patients had Acinetobacter and Klebsiella infections. Therefore, for each patient, only the diagnostic results using the universal bacterial probes (PB1, PB2, and PB3) and the Pseudomonas-specific probe (Psu) in the BDH assay were acquired according to the cutoff values determined in the ROC analysis (Figures 2B and Figure 3B).
Among the 16 patients with BK, two patients with BK (cases 2 and 18) had false-negative results using PB1 and PB2 but tested positive using PB3 (Table 2). This result may reflect the differences in the detection limits among the probes. The detection limits for probes PB1, PB2, and PB3 are 1 pg/μl, 100 fg/μl, and 10 fg/μl, respectively [34]. Probe PB3 had the lowest detection limit for bacteria and the highest sensitivity (93.8%) for diagnosing BK. One patient (case 13) infected with Staphylococcus hemolyticus had false-negative results for the three universal probes. Because routine PCR was less sensitive than the three universal probes, detection failure using all three probes for this patient was concluded because positive results for bacteria were obtained using routine PCR.
Table 2. Patients with positive results for bacteria as determined by microscopy, culture, PCR, and/or the bacterial dot assay.
| Case |
Age |
Sex |
Microscopya |
Culture |
PCRd |
Bacterial dot assay |
|||
|---|---|---|---|---|---|---|---|---|---|
| no. |
probe BP1 |
probe BP2 |
probe BP3 |
probe Psu |
|||||
| True positive cases by the probe BP3 | |||||||||
| 2 |
25 |
F |
GNBb |
P. aeruginosa |
+ |
− |
− |
+ |
+ |
| 18 |
57 |
F |
Yeast |
Glucose non-fermenter; mold |
− |
− |
− |
+ |
− |
| 20 |
57 |
F |
NDc |
M. fortuitum |
− |
+ |
+ |
+ |
− |
| 23 |
62 |
M |
− |
P. aeruginosa; S. epidermidis |
+ |
+ |
+ |
+ |
+ |
| 26 |
42 |
M |
− |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 27 |
63 |
M |
− |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 28 |
75 |
M |
− |
P. aeruginosa |
− |
+ |
+ |
+ |
+ |
| 29 |
41 |
F |
− |
P. aeruginosa |
− |
+ |
+ |
+ |
− |
| 32 |
58 |
M |
GNB |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 33 |
74 |
F |
GNB |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 35 |
43 |
M |
− |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 39 |
56 |
F |
ND |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 42 |
69 |
M |
GNB |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 45 |
30 |
M |
GNB |
P. aeruginosa |
+ |
+ |
+ |
+ |
+ |
| 50 | 56 | M | − | P. aeruginosa | + | + | + | + | + |
| False negative cases by the probe BP3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 13 | 63 | M | ND | S. haemolyticus | + | − | − | − | − |
| False positive cases by the probe BP3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 3 |
59 |
M |
− |
Mold |
− |
+ |
+ |
+ |
− |
| 17 |
77 |
M |
Yeast |
Yeast |
− |
+ |
+ |
+ |
− |
| 22 |
72 |
M |
ND |
Yeast |
− |
+ |
+ |
+ |
− |
| 49 | 65 | F | − | Mold | − | + | + | + | − |
| Cases with true negatives by the probe BP3 but false negatives by the probes BP1 or BP2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 9 |
50 |
F |
− |
Mold |
− |
+ |
− |
− |
− |
| 19 |
51 |
F |
− |
− |
−e |
+ |
− |
− |
− |
| 21 |
69 |
F |
ND |
− |
− |
+ |
− |
− |
− |
| 24 |
71 |
M |
− |
Candida spp. |
− |
+ |
+ |
− |
− |
| 25 |
62 |
M |
ND |
− |
− |
+ |
− |
− |
− |
| 30 |
72 |
M |
− |
− |
− |
+ |
− |
− |
− |
| 31 |
20 |
M |
− |
Acanthamoeba spp. |
− |
+ |
− |
− |
− |
| 36 |
47 |
M |
ND |
− |
− |
+ |
− |
− |
− |
| 37 |
27 |
M |
ND |
− |
− |
+ |
− |
− |
− |
| 38 | 74 | M | − | − | − f | + | − | − | − |
aMicroscopy examination by Gram stain and acid fast stain. bGNB, gram-negative bacilli. cND, not done. dPCR, polymerase chain reaction for bacteria. eNegative PCR result for bacteria but positive PCR result for microsporidia. fNegative PCR result for bacteria but positive PCR result for herpes simplex virus.
Among the 45 patients with non-BK, four patients (cases 3, 17, 22, and 49) who had the same false-positive results using the three universal probes were all infected by fungi (Table 2). Three cases were caused by trauma (by a tree branch, leaf, and insect, individually), and the other case had a preexisting phthisis cornea. Cocolonization of nonviable or fastidious bacteria on the uneven cornea surface was suggested for the four patients. In addition, one sample of a patient (case 24) with Candida keratitis obtained false-positive results using PB1 and PB2 but negative results using PB3. Another nine patients with non-BK, including one fungal keratitis case (case 9), one microsporidia keratitis (case 19), one Acanthamoeba keratitis case (case 31), and one herpes keratitis case (case 38), were false positive using PB1 but negative using PB2 and PB3. Therefore, probe PB1 should be used cautiously to exclude BK from fungal keratitis, microsporidia keratitis, Acanthamoeba keratitis, and herpes keratitis owing to the probe’s low specificity (only 71.1%).
Only one patient (case 29) with BK infected with P. aeruginosa was negative using the Pseudomonas-specific probe (Psu; Table 2). Sampling failure was excluded because all three universal bacterial probes were positive. However, the corneal scrape may have included too few Pseudomonas spp. because the standardized signal intensities for the three universal bacteria probes were only slightly higher than their cutoff values and the bacterial load for the cultures was rare. No false positive was identified for the probe Psu. In addition, only probe Psu was statistically significantly correlated with the bacterial load of culture (Figure 4). Intuitively, the bacterial load may be correlated with the severity of the bacterial infection. Therefore, Psu has clinical value not only to detect or exclude Pseudomonas keratitis but also to roughly estimate the Pseudomonas density in the scraped samples.
The assay requires minimal instrumentation and can be completed with a turnaround time of about 6 h. Therefore, this molecular technique has potential to improve BK diagnosis. It is easy to acquire the intensity of each probe using free software (ImageJ) and to transfer data to a predesigned worksheet (Microsoft Excel) to report standardized intensities and final diagnoses. For a routine clinical practice, the procedures can be improved by writing a mobile application for automation. Therefore, this assay has routine diagnostic value, especially if the array is commercialized.
The BDH assay has some limitations. An inherent drawback of DNA-based techniques is the potential detection of nonviable or microorganism contaminants, especially airborne bacteria. Additionally, positive and negative controls should be concomitantly performed when using the molecular technique. It is difficult for general users to prepare the array and reagents for hybridization; therefore, the procedure should be performed by well-trained laboratory staff with sterile techniques, appropriate control groups during PCR and hybridization, qualified reagents free of bacterial DNA, and daily ultraviolet sterilization in the laboratory. Although the BDH assay is more sensitive than direct microscopy and faster than culture, the assay cannot be used to immediately choose the empirical regimen of topical antibiotics as direct microscopy or later adjust the antibiotics with the susceptibility test of culture.
The detection limit of the probe PB3 for P. aeruginosa ATCC 10,944, Acinetobacter baumannii ATCC 15,884, and Klebsiella pneumoniae ATCC 11,644 was determined in our previous study [34]. However, in addition to Pseudomonas, Klebsiella, and Acinetobacter species, other bacterial species, including Staphylococcus, Streptococcus, and Moraxella, are also prominent in many epidemiological reports on BK. Therefore, serial tenfold dilutions of genomic DNA extracted from Staphylococcus aureus BCRB 14,957, Staphylococcus epidermidis BCRC 10,785, Streptococcus pneumoniae BCRC 10,794, and Moraxella catarrhalis BCRC 10,628 were analyzed in addition to that from the original species to ensure that the probe PB3 detected these other organisms with equal sensitivity. The experiment showed the detection limit of the probe PB3 is about 10–100 fg (2–12 bacterial cells) for all the bacterial reference strains mentioned above. Therefore, we believe the probe PB3 is sensitive enough to detect most causative pathogens of BK.
In conclusion, the BDH assay is a useful technique for the add-on investigation of BK. In addition to the assay’s good performance, the method has a short turnaround time (6 h). The current assay can facilitate the rapid diagnosis of fulminant Pseudomonas keratitis and estimate the Pseudomonas load of the infected cornea. Although the BDH assay has potential to detect Acinetobacter and Klebsiella keratitis, additional cases are needed to assess the clinical performance of the assay for diagnosing the two keratitis pathogens.
Acknowledgments
The authors acknowledge the Genomic & Proteomic Core Laboratory, Department of Medical Research, Chang Gung Memorial Hospital at Kaohsiung for supplying the arrayer. This work was supported by Chang Gung Research Proposal (CMRPG8C0762), the Ministry of Science and Technology (Grant No. MOST 103–2314-B-182A-044, MOST 104–2314-B-182A-101-MY3). The sponsors or funding organizations had no role in the design or conduct of this research. A part of the study result had been presented in the Asia-Pacific Academy of Ophthalmology Congress 2016.
References
- 1.Shah A, Sachdev A, Coggon D, Hossain P. Geographic variations in microbial keratitis: an analysis of the peer-reviewed literature. Br J Ophthalmol. 2011;95:762–7. doi: 10.1136/bjo.2009.169607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong HS, Corbett MC. Corneal infections in the 21st century. Postgrad Med J. 2015;91:565–71. doi: 10.1136/postgradmedj-2015-133323. [DOI] [PubMed] [Google Scholar]
- 3.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 4.Taube MA, del Mar Cendra M, Elsahn A, Christodoulides M, Hossain P. Pattern recognition receptors in microbial keratitis. Eye (Lond) 2015;29:1399–415. doi: 10.1038/eye.2015.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–21. [PMC free article] [PubMed] [Google Scholar]
- 6.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–21. [PMC free article] [PubMed] [Google Scholar]
- 7.Ti SE, Scott JA, Janardhanan P, Tan DT. Therapeutic keratoplasty for advanced suppurative keratitis. Am J Ophthalmol. 2007;143:755–62. doi: 10.1016/j.ajo.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Al-Shehri A, Jastaneiah S, Wagoner MD. Changing trends in the clinical course and outcome of bacterial keratitis at King Khaled Eye Specialist Hospital. Int Ophthalmol. 2009;29:143–52. doi: 10.1007/s10792-008-9206-6. [DOI] [PubMed] [Google Scholar]
- 9.Park J, Lee KM, Zhou H, Rabin M, Jwo K, Burton WB, Gritz DC. Community practice patterns for bacterial corneal ulcer evaluation and treatment. Eye Contact Lens. 2015;41:12–8. doi: 10.1097/ICL.0000000000000059. [DOI] [PubMed] [Google Scholar]
- 10.Ray KJ, Prajna L, Srinivasan M, Geetha M, Karpagam R, Glidden D, Oldenburg CE, Sun CQ, McLeod SD, Acharya NR, Lietman TM. Fluoroquinolone treatment and susceptibility of isolates from bacterial keratitis. JAMA Ophthalmol. 2013;131:310–3. doi: 10.1001/jamaophthalmol.2013.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandes M, Vira D, Medikonda R, Kumar N. Extensively and pan-drug resistant Pseudomonas aeruginosa keratitis: clinical features, risk factors, and outcome. Graefes Arch Clin Exp Ophthalmol. 2016;254:315–22. doi: 10.1007/s00417-015-3208-7. [DOI] [PubMed] [Google Scholar]
- 12.Jain R, Murthy SI, Motukupally SR. Clinical outcomes of corneal graft infections caused by multi-drug resistant Pseudomonas aeruginosa. Cornea. 2014;33:22–6. doi: 10.1097/ICO.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 13.Jain R, Murthy SI, Motukupally SR, Jain M. Use of topical colistin in multiple drug-resistant Pseudomonas aeruginosa bacterial keratitis. Cornea. 2014;33:923–7. doi: 10.1097/ICO.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 14.Vazirani J, Wurity S, Ali MH. Multidrug-resistant Pseudomonas aeruginosa keratitis: risk factors, clinical characteristics, and outcomes. Ophthalmology. 2015;122:2110–4. doi: 10.1016/j.ophtha.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Oldenburg CE, Lalitha P, Srinivasan M, Rajaraman R, Ravindran M, Mascarenhas J, Borkar DS, Ray KJ, Zegans ME, McLeod SD, Porco TC, Lietman TM, Acharya NR. Emerging moxifloxacin resistance in Pseudomonas aeruginosa keratitis isolates in South India. Ophthalmic Epidemiol. 2013;20:155–8. doi: 10.3109/09286586.2013.790978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlgren MA, Lingappan A, Wilhelmus KR. The clinical diagnosis of microbial keratitis. Am J Ophthalmol. 2007;143:940–4. doi: 10.1016/j.ajo.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leck A, Burton M. Distinguishing fungal and bacterial keratitis on clinical signs. Community Eye Health. 2015;28:6–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Mascarenhas J, Srinivasan M, Chen M, Rajaraman R, Ravindran M, Lalitha P, Oldenburg CE, Ray KJ, Glidden DV, Costanza S, Lietman TM, Acharya NR. Differentiation of etiologic agents of bacterial keratitis from presentation characteristics. Int Ophthalmol. 2012;32:531–8. doi: 10.1007/s10792-012-9601-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalmon C, Porco TC, Lietman TM, Prajna NV, Prajna L, Das MR, Kumar JA, Mascarenhas J, Margolis TP, Whitcher JP, Jeng BH, Keenan JD, Chan MF, McLeod SD, Acharya NR. The clinical differentiation of bacterial and fungal keratitis: a photographic survey. Invest Ophthalmol Vis Sci. 2012;53:1787–91. doi: 10.1167/iovs.11-8478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma N, Sachdev R, Jhanji V, Titiyal JS, Vajpayee RB. Therapeutic keratoplasty for microbial keratitis. Curr Opin Ophthalmol. 2010;21:293–300. doi: 10.1097/ICU.0b013e32833a8e23. [DOI] [PubMed] [Google Scholar]
- 21.Anshu A, Parthasarathy A, Mehta JS, Htoon HM, Tan DT. Outcomes of therapeutic deep lamellar keratoplasty and penetrating keratoplasty for advanced infectious keratitis: a comparative study. Ophthalmology. 2009;116:615–23. doi: 10.1016/j.ophtha.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 22.Sharma S, Kunimoto DY, Gopinathan U, Athmanathan S, Garg P, Rao GN. Evaluation of corneal scraping smear examination methods in the diagnosis of bacterial and fungal keratitis: a survey of eight years of laboratory experience. Cornea. 2002;21:643–7. doi: 10.1097/00003226-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Bhadange Y, Sharma S, Das S, Sahu SK. Role of liquid culture media in the laboratory diagnosis of microbial keratitis. Am J Ophthalmol. 2013;156:745–51. doi: 10.1016/j.ajo.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 24.McLeod SD, Kumar A, Cevallos V, Srinivasan M, Whitcher JP. Reliability of transport medium in the laboratory evaluation of corneal ulcers. Am J Ophthalmol. 2005;140:1027–31. doi: 10.1016/j.ajo.2005.06.042. [DOI] [PubMed] [Google Scholar]
- 25.Sugita S, Ogawa M, Shimizu N, Morio T, Ohguro N, Nakai K, Maruyama K, Nagata K, Takeda A, Usui Y, Sonoda KH, Takeuchi M, Mochizuki M. Use of a comprehensive polymerase chain reaction system for diagnosis of ocular infectious diseases. Ophthalmology. 2013;120:1761–8. doi: 10.1016/j.ophtha.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 26.Joseph J, Sharma S, Murthy SI, Krishna PV, Garg P, Nutheti R, Kenneth J, Balasubramanian D. Microsporidial keratitis in India: 16S rRNA gene-based PCR assay for diagnosis and species identification of microsporidia in clinical samples. Invest Ophthalmol Vis Sci. 2006;47:4468–73. doi: 10.1167/iovs.06-0376. [DOI] [PubMed] [Google Scholar]
- 27.Taravati P, Lam D, Van Gelder RN. Role of molecular diagnostics in ocular microbiology. Curr Ophthalmol Rep. 2013;1:1. doi: 10.1007/s40135-013-0025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schacht O. Molecular approaches to infectious disease assays. MLO Med Lab Obs. 2014;46:18. [PubMed] [Google Scholar]
- 29.Powell S, Crowther Z. The impact of molecular approaches to infectious disease diagnostics. MLO Med Lab Obs. 2015;47:18–9. [PubMed] [Google Scholar]
- 30.Kuo MT, Chang HC, Cheng CK, Chien CC, Fang PC, Chang TC. A highly sensitive method for molecular diagnosis of fungal keratitis: a dot hybridization assay. Ophthalmology. 2012;119:2434–42. doi: 10.1016/j.ophtha.2012.06.049. [DOI] [PubMed] [Google Scholar]
- 31.Kuo MT, Fang PC, Yu HJ, Chao TL, Chien CC, Chen SH, Wang JR, Tseng SL, Lai YH, Hsiao CC, Chang TC. A multiplex dot hybridization assay for detection and differentiation of Acanthamoeba and herpes keratitis. Invest Ophthalmol Vis Sci. 2016;57:2158–63. doi: 10.1167/iovs.15-17741. [DOI] [PubMed] [Google Scholar]
- 32.Hsiao C, Yeung L, Ma DK, Chen YF, Lin HC, Tan HY, Huang SC, Lin KK. Pediatric microbial keratitis in taiwanese children: a review of hospital cases. Arch Ophthalmol. 2007;125:603–9. doi: 10.1001/archopht.125.5.603. [DOI] [PubMed] [Google Scholar]
- 33.Lee YS, Tan HY, Yeh LK, Lin HC, Ma DH, Chen HC, Chen SY, Chen PY, Hsiao CH. Pediatric microbial keratitis in Taiwan: clinical and microbiological profiles, 1998–2002 versus 2008–2012. Am J Ophthalmol. 2014;157:1090–6. doi: 10.1016/j.ajo.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 34.Kuo MT, Chien CC, Lo J, Hsiao CC, Tseng SL, Lai YH, Fang PC, Chang TC. A DNA dot hybridization model for assessment of bacterial bioburden in orthokeratology lens storage cases. Invest Ophthalmol Vis Sci. 2015;56:445–50. doi: 10.1167/iovs.14-15920. [DOI] [PubMed] [Google Scholar]
- 35.Fang PC, Lo J, Chang TC, Chien CC, Hsiao CC, Tseng SL, Lai YH, Kuo MT. Bacterial bioburden decrease in orthokeratology lens storage cases after forewarning: assessment by DNA dot hybridization assay. Eye Contact Lens. 2016 doi: 10.1097/ICL.0000000000000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lo J, Fang PC, Chien CC, Hsiao CC, Tseng SL, Lai YH, Kuo MT. PCR analysis for assessment of bacterial bioburden in orthokeratology lens cases. Mol Vis. 2016;22:1–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Fujitani S, Cohen-Melamed MH, Tuttle RP, Delgado E, Taira Y, Darby JM. Comparison of semi-quantitative endotracheal aspirates to quantitative non-bronchoscopic bronchoalveolar lavage in diagnosing ventilator-associated pneumonia. Respir Care. 2009;54:1453–61. [PubMed] [Google Scholar]
- 38.Lin YT, Vaneechoutte M, Huang AH, Teng LJ, Chen HM, Su SL, Chang TC. Identification of clinically important anaerobic bacteria by an oligonucleotide array. J Clin Microbiol. 2010;48:1283–90. doi: 10.1128/JCM.01620-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hsiao CR, Huang L, Bouchara JP, Barton R, Li HC, Chang TC. Identification of medically important molds by an oligonucleotide array. J Clin Microbiol. 2005;43:3760–8. doi: 10.1128/JCM.43.8.3760-3768.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]