Abstract
Context
Little is known about how parents of children with advanced cancer classify news they receive about their child’s medical condition.
Objective
To develop concepts of “good news” and “bad news” in discussions of advanced childhood cancer from parent perspectives.
Methods
Parents of children with advanced cancer cared for at three children’s hospitals were asked to share details of conversations in the preceding 3 months that contained “good news” or “bad news” related to their child’s medical condition. We used mixed methods to evaluate parent responses to both open-ended and fixed response items.
Results
Of 104 enrolled parents, 86 (83%) completed the survey. Six (7%) parents reported discussing neither good nor bad news, 18 (21%) reported only bad news, 15 (17%) reported only good news, and 46 (54%) reported both good and bad news (1 missing response). Seventy-six parents (88%) answered free response items. Descriptions of both good and bad news discussions consisted predominantly of “tumor talk” or cancer control. Additional treatment options featured prominently, particularly in discussions of bad news (42%). Child well-being, an important good news theme, encompassed treatment tolerance, symptom reduction, and quality of life.
Conclusion
A majority of parents of children with advanced cancer report discussing both good and bad news in the preceding 3 months. While news related primarily to cancer control, parents also describe good news discussions related to their child’s well-being. Understanding how parents of children with advanced cancer classify and describe the news they receive may enhance efforts to promote family-centered communication.
Keywords: Good News, Bad News, Parental Perceptions, Advanced Childhood Cancer, Hope, Tumor Talk
Introduction
As our culture moves to increase the openness with which we address serious illness, there is increasing focus on conversations between healthcare providers and patients at advanced stages of illness.(1,2) Providers and researchers often characterize conversations with patients with advanced cancer (a prototypical serious illness) in terms of “breaking bad news” or “discussing transitions of care.”(3–6) In the setting of serious illness among adults, special emphasis has been placed on providing realistic prognoses(7) and appraising and improving communication regarding advance care planning.(8,9) While these efforts are vitally important, the scope of communication in serious illness extends beyond planning for end-of-life care.
As treatments for childhood cancers have improved and our understanding of cancer biology has deepened, illness trajectories for even advanced childhood cancers have become less certain.(10–14) Although providing realistic prognoses is equally important in this setting,(15) relative longevity of children with advanced cancer and frequent contact between families and clinicians may occasion communication that is not anchored solely around prognostic discussions. Furthermore, parents of children with advanced cancer may have hopes (for a long life) and expectations (death from disease in weeks to months) that appear contradictory.(16,17) Such psychological frames shape parents’ perceptions and influence their decision-making.(18,19) Previous work suggests that parents may(20) or may not(21) feel tensions between seemingly contradictory hopes and expectations, whereas pediatric healthcare providers frequently do.(21) How, then, do parents of children with advanced cancer characterize conversations with their child’s medical caregivers about their child’s health? We sought to understand concepts of “good news” and “bad news” discussed by pediatric oncology care teams with families of children with advanced cancer, as described by parents.
Methods
The PediQUEST (Pediatric Quality of Life and Evaluation of Symptoms Technology) study was a pilot randomized trial of a supportive care intervention for children with advanced cancer. The primary outcome of interest, results of which have been previously published, was use and impact of the PediQUEST software system, which was designed to collect patient-reported outcomes and to generate feedback for providers.(22) Secondary objectives included understanding parents’ characterizations of conversations with their children’s medical caregivers, including their descriptions of “good news” and “bad news.” Parents were surveyed (see below for a description of the study instrument) at the time of enrollment. To be included in the PediQUEST study, eligible patients were age ≥ 2 years with ≥ 2-week history of progressive, recurrent, or non-responsive cancer and had received cancer care at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, Children’s Hospital of Philadelphia, or Seattle Children’s Hospital. Each institutional review board approved the study. Consecutive families were approached between December 2004 and June 2009, and 104 children enrolled.
Study Instrument
The Survey About Caring for Children with Cancer (SCCC) is a comprehensive, self-administered survey that evaluates parents’ perceptions of the child’s illness. As previously described, it was developed from a literature review and focus groups of parents and medical providers to identify key domains.(17,23) Pretesting was performed to assess content, wording, cognitive validity, and response burden, and items with existing validity evidence were used whenever feasible.
Participating families completed self-administered pencil-and-paper surveys which were returned via self-addressed stamped envelopes to the study team. One parent per family completed the survey, and a $5 coffee card incentive was included with the SCCC. Parents who did not respond within two weeks received two additional reminders.
The survey domain of interest for the current analysis is “Delivery of News.” Parents were asked, “During the past 3 months, have you talked with your child’s caregivers about any good news related to his or her medical condition?” Fixed-response survey items then queried conversation characteristics, including persons present for the discussion, type of provider leading the discussion, conversation setting, perceived appropriateness of discussion topic and timing, perceived understanding of the discussion, and perceived degree of sensitivity of the discussant’s manner. Parents were also asked, “Would you please share some of the details of what was discussed during this conversation?” and given space to provide a free text response. Identical items were asked for bad news, with the addition of five 5-point Likert scale fixed-response items that asked to what degree parents were able to express hopes and worries during bad news discussions, to what degree these were addressed, and to what degree parents were able to make suggestions about their child’s care. Additionally, parents were asked about potential care changes that arose from these discussions (“Were changes made in your child’s care based on these discussions with your child’s care team? If yes, please specify,”), the manner in which news was conveyed, (“Is there anything else you would like to add regarding how news was delivered to you and your family?”), and for relevant care context (“Is there anything else you think we should know regarding the medical care of your child during these past months?”).
Analytic Methods
We employed descriptive statistics, including counts, proportions, means, and standard deviations, to describe the cohort of parent respondents, their children, the sites of childhood cancer care, the oncology providers who directed cancer care, and parent-reported conversation characteristics. Deaths of children of parent respondents were recorded through the end of the study data collection period (December 18, 2009). No effort was made to impute missing data. All statistical analyses were performed using Stata software version 10.1 (StataCorp, College Station, Texas).
Parent free text responses to the questions “Would you please share some of the details of what was discussed during this conversation,” for both good news and bad news were subjected to qualitative textual analysis. Because our aim was to understand what parents characterized as “good news” and “bad news,” we maintained parent-reported categorizations. We coded free-text responses to questions about care changes, news delivery, and care context if the respondent reflected on the good news or bad news discussion in these answers. Analysis was iterative and began with open coding, followed by refinement of codes into a codebook, focused coding, and subsequent category construction.(24,25) We then sought to understand how thematic categories related to each other. Open coding, codebook development, and focused coding was performed by one of the authors (AMF), and reviewed by an additional author (VD) for clarity and consistency to ensure trustworthiness. Atlas.ti software version 7.5.10 (Berlin, Germany) was used for data management.
Results
Characteristics of the 86 parents who completed the SCCC (83% of enrolled parents) and their children are shown in Table 1. Most parent respondents were women, and the vast majority were white and non-Hispanic. Children were slightly more likely to be male, with a mean age of 12.1 years. Notably, all three major disease categories (hematologic malignancies, central nervous system (CNS) tumors, and non-CNS solid tumors) were represented, though a majority of children had non-CNS solid tumors. A majority of children were alive at study completion. Most children were cared for primarily by a physician pediatric oncologist, although 22% identified a nurse practitioner as their primary oncology provider. Follow up time from completion of the SCCC to death or the end of data collection ranged from 0.8 months to 58.7 months (median 11.5 months, IQR 6.3–22.4 months). Among children who died (n=37), time from completion of the SCCC to death ranged from 0.8 months to 42.6 months (median 7.3 months, IQR 4.4–13.6 months).
Table 1.
Participant and Child Characteristics at time of Survey Completion
| Characteristic | Mean (SD) | Number (%) |
|---|---|---|
| Parents (n=86) | ||
| Age, years | 43.6 (7.5) | |
| Female sex | 74 (86.0) | |
| Ethnicity (n=84) | ||
| Hispanic | 6 (7.1) | |
| Race (n=82) | ||
| American Indian/Alaskan Native | 0 (0) | |
| Asian | 1 (1.2) | |
| Black or African American | 3 (3.7) | |
| Native Hawaiian or Pacific Islander | 0 (0) | |
| White | 76 (92.7) | |
| Other | 2 (2.4) | |
| Children (n=86) | ||
| Age, yearsa | 12.1 (5.8) | |
| Female sex | 46 (53.5) | |
| Alive at study completionb | 49 (57) | |
| Cancer type (n=86) | ||
| Hematologic malignancy | 28 (32.6) | |
| CNS tumor | 9 (10.5) | |
| Non-CNS solid tumor | 49 (57.0) | |
| Months since diagnosis at time of survey (n=84) | 26.8 (20.1) | |
| Health Care Provider (type by patient, n=79) | ||
| MD | 62 (78.5) | |
| NP | 17 (21.5) | |
| Health Care Site (n=86) | ||
| CHOPc | 21 (24.4) | |
| DF/CHd | 49 (57.0) | |
| SCHe | 16 (18.6) |
Determined at study entry; for some participants, there was a delay between date of entry and date of survey completion.
December 18, 2009
CHOP=Children’s Hospital of Philadelphia
DF/CH=Dana-Farber and Boston Children’s Cancer and Blood Disorders Center
SCH=Seattle Children’s Hospital
Conversation Characteristics and Child Outcomes
Overall, 61 parents reported discussing good news with their child’s provider, and 64 parents reported discussing bad news with their child’s provider. A majority of parents (n=46, 53%) reported discussing both good and bad news with their child’s caregivers in the preceding 3 months (Table 2). Children participated in most good news (42/56, 75%) and bad news (39/61, 64%) discussions. Most discussions were led by the primary oncologist (good news: 53/56, 95%; bad news: 51/62, 82%), and most occurred in the outpatient setting (good news: 38/54, 70%; bad news: 35/60, 58%). A vast majority of parents reported that both good news (45/56, 80%) and bad news (51/62, 82%) were discussed in a very sensitive manner, and that the timing of the discussion was appropriate (100% for good news, 5 missing; 95% for bad news, 2 missing). Furthermore, responding parents reported that they clearly understood “a great deal” or “a lot” of what was being discussed in good news (50/55, 91%) and bad news (55/62, 89%) discussions. Care changes were not reported for any of the children whose parents reported discussing only good news, whereas two-thirds to three quarters of children whose parents reported discussing mixed news or only bad news were reported to have experienced changes in care (Table 2). The cumulative incidence of death was highest among children whose parents reported discussing bad news only (56%), and lowest among those who discussed good news only (27%, Table 2).
Table 2.
Parent Perceptions of Type of News Discussed, Changes in Care, and Child Outcomes
| Parent Perception of Type of News Discussed | Number (%) | Changes in Carea Number (%) | Child Deceased at Study Conclusion Number (%)b |
|---|---|---|---|
| Good news only | 15 (17) | 0 (0) | 4 (27) |
| Bad news only | 18 (21) | 12 (67) | 10 (56) |
| Good and bad news | 46 (54) | 34 (74) | 20 (44) |
| No news discussed | 6 (7) | N/A | 2 (33) |
| Missing | 1 (1) | N/A | 1 (100) |
| Total | 86 (100) | 46 (54) | 37 (43) |
Changes in child’s care that parent reported related to discussions characterized as containing good news and/or bad news. Parents who replied “no” to “During the past 3 months, have you talked with your child’s caregivers about any good/bad news related to her medical condition” were instructed to skip this question.
Percentage of children deceased out of the total number for each reported news type
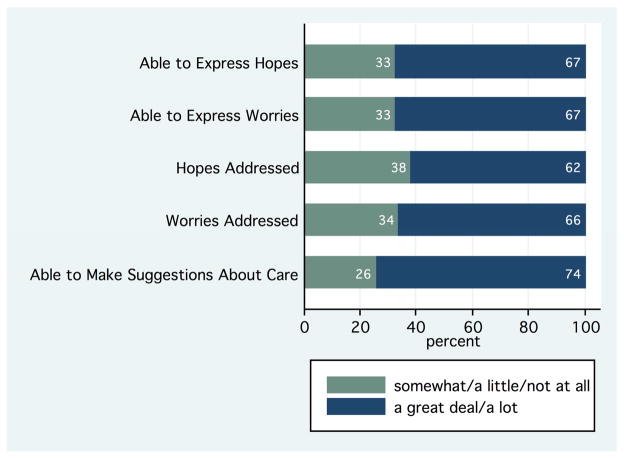
Expression of Hopes and Worries
Figure 1 summarizes parents’ reports of the extent to which they could express their hopes and worries during discussions of bad news, and how sufficiently these hopes and worries were addressed. A majority of parents were able to express their hopes and worries “a lot” or “a great deal” and most also reported that these were addressed “a lot” or “a great deal.” However, approximately one-third of parents reported incomplete ability to share hopes and worries. In exploratory subgroup analyses, these parents did not differ with regard to religiosity, education, race, ethnicity, or income. Notably, nearly three-quarters of parents who reported discussing bad news felt able to make suggestions about their child’s care. Although there was substantial overlap in parents who expressed inability to share hopes and/or worries and those who felt unable to make suggestions about their child’s care, only six parents reported “somewhat/a little/not at all” in response to all five items. Appraisal of the free text comments by these six parents revealed that two of the six were concerned with discussing worries in front of the ill child: “I did not want to address many worries in front of my daughter at that time;” “I do not want any type of bad news delivered in front of my child.” Thus, understanding parents’ desired setting and circumstances for discussions may facilitate greater expression of hopes and worries.
Figure 1.
Expression of and Attention to Hopes and Worries During Bad News Discussions
Perceptions of ability to express hopes and worries, attention to expressed hopes and worries, and ability to make suggestions for their child’s care among parents who reported bad news discussions in the preceding 3 months; all numbers are percentages (total n=61, 61, 60, 59, 62).
Free-Response Items and Emergent Themes
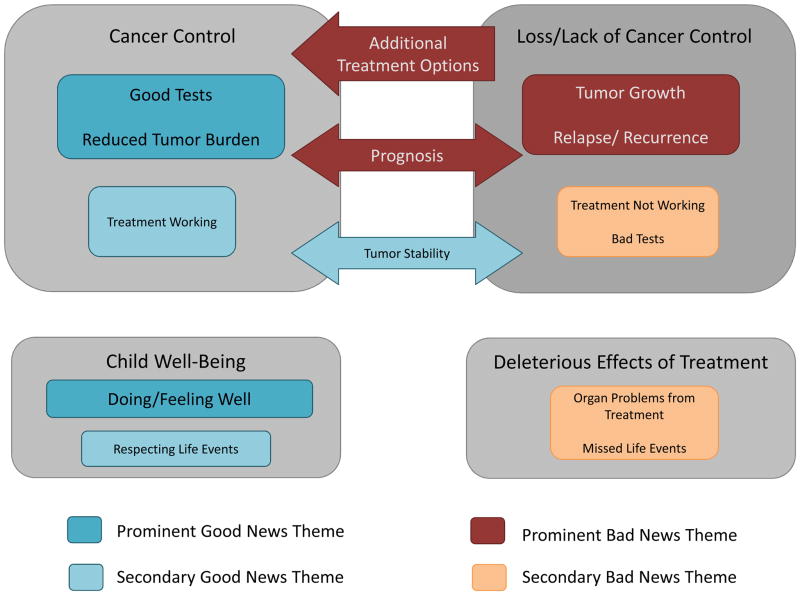
Seventy-six parents (88%) answered free response items that asked participants to share details of what was discussed during their conversations with their child’s medical caregivers. Figure 2 summarizes the major thematic categories and their interconnectedness. A list of themes and illustrative quotes are displayed in Table 3. The organizing thematic categories for good news discussions were cancer control and child well-being, whereas the organizing thematic categories for bad news discussions were loss/lack of cancer control and deleterious effects of treatment.
Figure 2.
Schema of Thematic Categories
This figure visually summarizes the good news and bad news themes parents perceived and demonstrates their relative prominence and interrelationships. Together, the top two boxes constitute “Tumor Talk,” whereas the bottom two boxes concern the greater context of the child’s overall health and life. Prominent themes were the most frequently endorsed, and each were endorsed by 15% or more of parent respondents. Prominent bad news themes are displayed in cranberry and secondary bad news themes are displayed in light orange. Prominent good news themes are displayed in teal and secondary good news themes are displayed in light blue. Cancer control and loss/lack of cancer control are perceived as dynamic, interrelated states, bridged by discussions of tumor stability, prognosis, and additional treatment options (shown as arrows). Child well-being and the deleterious effects of treatment may not be related to the state of cancer control/lack of control.
Table 3.
Thematic Categories of Good and Bad News and Illustrative Quotes
| Type of News | Category | Code | Parents Endorsing | Quotations |
|---|---|---|---|---|
| Good News | n=51 (%) | |||
| Cancer Control | Good Tests | 12 (24) | “Current treatment child was on
appeared to be working and lowering AFP” “Perfect match for BMT!” “The test results showed no neuroblastoma in his bone marrow or his head – Specifically in the soft tissue around brain.” |
|
| Reduced Tumor Burden | 9 (18) | “Transplant did clear most of
cancer.” “50% shrinkage of tumors on CT scan in Feb” “Secondary tumors (lung metastases) are shrinking again following 2 rounds on new regimen” |
||
| Additional Treatment Options | 7 (14) | “MIBG therapy would be an option for treatment. Also, stem cell harvest was a possible option” | ||
| Treatment Working | 5 (10) | “Chemotherapy put cancer in remission!” | ||
| Tumor Stability | 3 (6) | “Last scan was stable” | ||
| Prognosis | 2 (4) | “That his cancer was curable and they (doctors) had a very hopeful outlook for my son.” | ||
| Child Well-Being | Doing/Feeling Well | 8 (16) | “Our son has been feeling the best yet
since his diagnosis last July and we are now preparing for
transplant” “Child’s great energy, disposition, appetite improvement” |
|
| Respecting Life Eventsa | 3 (6) | “We were able to make a “Make A Wish” trip without worry.” | ||
| Bad News | n=59 (%) | |||
| Loss/Lack of Cancer Control | Additional Treatment Options | 25 (42) | “What to do next? Chemo options,
trials, tumor freezing.” “We would try decitabine (usually reserved for adults) and would see if it would help, but unlikely to be a cure.” |
|
| Relapse/Recurrence | 17 (29) | “Another tumor. We all hoped it
wouldn’t happen, but expected
it.” “Secondary tumors (lung metastasis) re-appeared during consolidation phase of first treatment protocol.” |
||
| Tumor Growth | 11 (19) | “Four new osteosarcoma tumors were found and removed from [child’s] right lung, 2 more than the CT scan revealed.” | ||
| Prognosis | 11 (19) | “That my child’s condition was
nearing her death” “Statistics do not show good prognosis for ALL patients with recurrence” “At the beginning his doctors never talked much about a prognosis, only that they expected that treatment should make it go away. Now that he’s relapsed they seem ready to give up.” |
||
| Bad Tests | 8 (14) | “We discussed the latest CT scan having shown tumor growth” | ||
| Treatment Not Working | 6 (10) | “It was explained that my
child’s first round of chemo did not
work” “The third treatment protocol did not stop the cancer from growing.” |
||
| Tumor Stability | 2 (3) | “Test results not good. Just bad news when things still haven’t changed.” | ||
| Deleterious Effects of Treatment | Organ Problems from Treatment | 5 (8) | “Possible med changes because of renal
problems”; “Left kidney function only 10%;” “[Child] hospitalized for typhlitis (bowel obstruction and infection) related to chemo” |
|
| Missed Life Events | 2 (3) | “Current treatment will involve a lot of inpatient time, so our child will miss a lot of school over the next year or so.” |
In addition to parent descriptions of “good news” conversations, this code arose from parent responses to the item “Were changes made in your child’s care based on these discussions with your child’s care team? If yes, please specify”
Good News
Parents described discussing good news about their child’s cancer, and specifically, control of that cancer. Parents indicated that news of cancer control often came in the form of good test results: “scan results showing shrinkage of the tumor;” “Current treatment [child] was on appeared to be working and lowering AFP.” Parents wrote of reduced tumor burdens, and even tumor stability, as good news. Additional treatment options were described as the driving good in some good news discussions: “tumor dead, nodes + but Phase II trial available.” A minor theme that emerged was the primary oncology provider’s reaction as a source of good news: “I’m very happy because the MDs were happy with how [child] is doing.” Another important good news category that emerged from parents’ reports was that of child well-being—even in the face of poor or uncertain cancer control. “Although all believe that [child’s] relapsed leukemia is going to be fatal, the discussions have focused on the fact that he has been doing well and holding steady in the last month.” As such, while much of the news parents interpreted as good centered on cancer control, good news was possible even in the absence of cancer control.
Bad News
Bad news of loss or lack of cancer control also often came by way of bad test results. Bad test results were reported as indicating relapse/recurrence, tumor growth, or, at times, tumor stability: “Test results not good. Just bad news when things still haven’t changed.” Bad news discussions frequently quantified the loss of cancer control: “Four new osteosarcoma tumors were found and removed from [child’s] right lung, 2 more than the CT scan revealed.” In the face of losing cancer control, additional treatment options were often described as ameliorating the effect of the bad news: “MRI showed progression of tumors on topotecan. We were devastated but then had a new treatment plan ready.” Notably, additional treatment options were not always cancer-directed: “Dr. did a great job discussing what they could offer to minimize pain, seizures, etc.” Apart from issues of loss/lack of cancer control, prognostic implications, and additional treatment options, bad news discussion descriptions also highlighted other losses and anticipated losses, such as deleterious effects of disease or treatment on the body and on quality of life.
Although the survey item structure encouraged parents to report on “good” news and “bad” news discussions separately, parents conveyed a sense that news could be more challenging to classify: “At this point in my child’s treatment, assessing news as ‘good’ or ‘bad’ is difficult for us. I will say, however, that all news has been delivered to us in a clear, professional, and sensitive manner, both over the phone and in clinic.” One participant articulated the ambiguity of a reduction in tumor burden (“Yes, transplant did clear most but we still have small amount to clear”), indicating that the reduction signaled both good and bad news.
Discussion
In this cross-sectional, multi-institutional survey of parents of children with advanced cancer, most parents reported discussing both good and bad news over the prior three months with their child’s medical caregivers. Much of these discussions center on “tumor talk” or cancer control: discussions of test and imaging results, whether treatment is working, and whether tumors are growing or receding. This study is based on parent assessment of which discussions entailed “good” and “bad” news. Overall, details of parents’ reports and the apparent pattern of child outcomes support the accuracy of their perceptions. Notably, none of the parents who reported discussing only good news reported changes in their child’s care related to such discussions (Table 2). Likewise, the cumulative incidence of death was higher among children of parents who described discussing only bad news. Importantly, the descriptors “good” and “bad” were imposed by the survey items, and may not have been parents’ preferred terms to characterize these discussions with their child’s care team. Indeed, parents’ descriptions of “good” and “bad” news discussions suggest that their conceptions of illness are nuanced, rather than dichotomous, which is consistent with prior reports.(16,21)
Apart from the characterization of these conversations as “good news” and “bad news” conversations, parents’ answers suggest that these discussions are conducted in a sensitive manner, are well-understood, and frequently allow for expression of and attention to parents’ hopes and worries. However, it is worth noting that approximately one-third of parents reported limited ability to express hopes and worries, suggesting that for these parents and their children, shared decision-making and goal-concordant care may have been more difficult to achieve. Interestingly, children were present for most good (75%) and bad (64%) news discussions, although it is unclear whether or not this matched parent preferences.
From parents’ characterizations of discussions, a picture emerges of fleeting triumphs and serial setbacks, as cancer grows, is whittled away, returns, is rebuffed, and so on. This dynamic, fluid picture of ground gained and lost stands somewhat in contrast to the lexicon of “breaking bad news,” which may evoke discussions that signal a discrete, unambiguous change in the illness trajectory. Instead, parents describe a nuanced and uncertain reality of living with and caring for a child with advanced cancer, wherein even the concepts of “good” and “bad” are difficult to distinguish from one another. Understanding how parents of children with advanced cancer classify, describe, and interpret discussions with their child’s medical caregivers may enhance efforts to promote family-centered communication, with implications for training and practice. In particular, the finding that approximately one-third of parents reported incomplete abilities to express hopes and worries in the context of self-described “bad news” discussions suggests that our current approaches to discussions in advanced childhood cancer may limit parents’ agency.
Importantly, what emerges from this report is how much high-stakes communication occurs outside of advance care planning discussions. Although prognosis was a common parent-identified theme, explicit discussions of end-of-life care and decision-making, such as preferred location of death(26) and resuscitation status, are completely absent from parents’ descriptions. Because such conversations often occur more proximate to death(17) (despite recognition that earlier discussions are likely more desirable), it is quite possible that such discussions occurred after parents completed this baseline survey. At least, that would be expected based on expert recommendations,(27–29) as such conversations are highly relevant to this group of children; at the conclusion of the PediQUEST study, 43% of children of enrolled parents who completed the survey had died, and the median time to death from survey completion was 7.3 months, though time to death ranged widely.
This study has several limitations. One methodologic limitation is in the approach to sampling. Qualitative data collection and subsequent analysis can be strengthened by the use of theoretical sampling, an approach which requires that additional sampling be possible once analysis has begun and initial categories are emerging from the data.(25) Due to the nature of the data (survey responses completed prior to the current analysis), such an approach to sampling was not possible for this study. Likewise, because parents completed written free response items without interaction with an interviewer, there was no opportunity to probe, clarify, or build upon these initial parent responses. As such, the thematic categories identified in this study, and their apparent interconnections, are less richly characterized and explored than they would be in the setting of theoretical sampling and in-depth interviews. Furthermore, asking parents to recall discussions from the preceding three months might be expected to lead to preferential recollection of “bad news” discussions, so the reported prevalence of good news and bad news discussions may reflect recall bias. However, the strengths of this study are the relatively large sample of respondents, the geographic distribution of respondents, and the high response rate.
Overall, findings suggest that both good news and bad news discussions are prevalent in the setting of advanced childhood cancer, and that these discussions are most often focused on “tumor talk” as well as child well-being. Importantly, parents describe a nuanced and uncertain reality of living with and caring for a child with advanced cancer. Central to our understanding of decision-making, care quality, and quality of life for children with advanced cancer are the conceptual models of illness that children, their parents, and health care providers bring to conversations. Future work should further refine these concepts, as well as their value to parents, and explore connections between illness conceptions, communication perceptions, and decision-making among parents of children with advanced cancer.
Acknowledgments
The PediQUEST study (Evaluation of Pediatric Quality of Life and Evaluation of Symptoms Technology in Children with Cancer) was supported by grants NIH/NCI 1K07 CA096746-01, Charles H. Hood Foundation Child Health Research Award, and American Cancer Society Pilot and Exploratory Project Award in Palliative Care of Cancer Patients and Their Families. Dr. Feraco was supported by grant 5T32HL007574. The authors would like to acknowledge the families who, in sharing their experiences, gave so generously of their words and their time.
Abbreviations
- CNS
Central nervous system
- CHOP
Children’s Hospital of Philadelphia
- DF/CH
Dana-Farber and Boston Children’s Cancer and Blood Disorders Center
- IQR
interquartile range
- PediQUEST
Pediatric Quality of Life and Evaluation of Symptoms Technology
- SCH
Seattle Children’s Hospital’
- SD
Standard Deviation
- SCCC
Survey about Caring for Children with Cancer
Footnotes
Disclosures
The authors have no financial disclosures relevant to this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bernacki RE, Block SD American College of Physicians High Value Care Task Force. Communication about serious illness care goals: A review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994–2003. doi: 10.1001/jamainternmed.2014.5271. [DOI] [PubMed] [Google Scholar]
- 2.Feudtner C. The breadth of hopes. N Engl J Med. 2009;361(24):2306–2307. doi: 10.1056/NEJMp0906516. [DOI] [PubMed] [Google Scholar]
- 3.Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167(5):453–460. doi: 10.1001/archinte.167.5.453. [DOI] [PubMed] [Google Scholar]
- 4.Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55(3):164–177. doi: 10.3322/canjclin.55.3.164. [DOI] [PubMed] [Google Scholar]
- 5.Baile WF, Buckman R, Lenzi R, et al. SPIKES-A six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 6.Orgel E, McCarter R, Jacobs S. A failing medical educational model: A self-assessment by physicians at all levels of training of ability and comfort to deliver bad news. J Palliat Med. 2010;13(6):677–683. doi: 10.1089/jpm.2009.0338. [DOI] [PubMed] [Google Scholar]
- 7.Gramling R, Gajary-Coots E, Stanek S, et al. Design of, and enrollment in, the palliative care communication research initiative: A direct-observation cohort study. BMC Palliat Care. 2015;14:40015-0037-8. doi: 10.1186/s12904-015-0037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernacki R, Hutchings M, Vick J, et al. Development of the serious illness care program: A randomised controlled trial of a palliative care communication intervention. BMJ Open. 2015;5(10):e009032-2015-009032. doi: 10.1136/bmjopen-2015-009032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halpern SD, Loewenstein G, Volpp KG, et al. Default options in advance directives influence how patients set goals for end-of-life care. Health Aff (Millwood) 2013;32(2):408–417. doi: 10.1377/hlthaff.2012.0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pui CH, Yang JJ, Hunger SP, et al. Childhood acute lymphoblastic leukemia: Progress through collaboration. J Clin Oncol. 2015;33(27):2938–2948. doi: 10.1200/JCO.2014.59.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huo JS, Symons HJ, Robey N, et al. Persistent multiyear control of relapsed T-cell acute lymphoblastic leukemia with successive donor lymphocyte infusions: A case report. Pediatr Blood Cancer. 2016 doi: 10.1002/pbc.25971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koocher GP, O’Malley JE, O’Malley JE. The damocles syndrome: Psychosocial consequences of surviving childhood cancer. New York: McGraw-Hill; 1981. p. 219. [Google Scholar]
- 13.Chou AJ, Merola PR, Wexler LH, et al. Treatment of osteosarcoma at first recurrence after contemporary therapy: The memorial sloan-kettering cancer center experience. Cancer. 2005;104(10):2214–2221. doi: 10.1002/cncr.21417. [DOI] [PubMed] [Google Scholar]
- 14.Yu AL, Gilman AL, Ozkaynak MF, et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med. 2010;363(14):1324–1334. doi: 10.1056/NEJMoa0911123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg AR, Orellana L, Kang TI, et al. Differences in parent-provider concordance regarding prognosis and goals of care among children with advanced cancer. J Clin Oncol. 2014;32(27):3005–3011. doi: 10.1200/JCO.2014.55.4659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamihara J, Nyborn JA, Olcese ME, Nickerson T, Mack JW. Parental hope for children with advanced cancer. Pediatrics. 2015;135(5):868–874. doi: 10.1542/peds.2014-2855. [DOI] [PubMed] [Google Scholar]
- 17.Wolfe J, Klar N, Grier HE, et al. Understanding of prognosis among parents of children who died of cancer: Impact on treatment goals and integration of palliative care. JAMA. 2000;284(19):2469–2475. doi: 10.1001/jama.284.19.2469. [DOI] [PubMed] [Google Scholar]
- 18.Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: Parental optimism and the parent-physician interaction. J Clin Oncol. 2007;25(11):1357–1362. doi: 10.1200/JCO.2006.08.3170. [DOI] [PubMed] [Google Scholar]
- 19.Mack JW, Joffe S, Hilden JM, et al. Parents’ views of cancer-directed therapy for children with no realistic chance for cure. J Clin Oncol. 2008;26(29):4759–4764. doi: 10.1200/JCO.2007.15.6059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenberg AR, Dussel V, Kang T, et al. Psychological distress in parents of children with advanced cancer. JAMA Pediatr. 2013;167(6):537–543. doi: 10.1001/jamapediatrics.2013.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reder EA, Serwint JR. Until the last breath: Exploring the concept of hope for parents and health care professionals during a child’s serious illness. Arch Pediatr Adolesc Med. 2009;163(7):653–657. doi: 10.1001/archpediatrics.2009.87. [DOI] [PubMed] [Google Scholar]
- 22.Wolfe J, Orellana L, Cook EF, et al. Improving the care of children with advanced cancer by using an electronic patient-reported feedback intervention: Results from the PediQUEST randomized controlled trial. J Clin Oncol. 2014;32(11):1119–1126. doi: 10.1200/JCO.2013.51.5981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342(5):326–333. doi: 10.1056/NEJM200002033420506. [DOI] [PubMed] [Google Scholar]
- 24.Pope C, Ziebland S, Mays N. Qualitative research in health care. analysing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London; Thousand Oaks, Calif: Sage Publications; 2006. p. 208. [Google Scholar]
- 26.Dussel V, Kreicbergs U, Hilden JM, et al. Looking beyond where children die: Determinants and effects of planning a child’s location of death. J Pain Symptom Manage. 2009;37(1):33–43. doi: 10.1016/j.jpainsymman.2007.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wiener L, Feudtner C, Hinds P, Wolfe J, Mack J. Deeper conversations need not wait until the end. J Clin Oncol. 2015;33(33):3974. doi: 10.1200/JCO.2015.62.3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaye EC, Friebert S, Baker JN. Early integration of palliative care for children with high-risk cancer and their families. Pediatr Blood Cancer. 2016;63(4):593–597. doi: 10.1002/pbc.25848. [DOI] [PubMed] [Google Scholar]
- 29.Institute of Medicine Committee on Palliative and End-of-Life Care for Children and Their Families. Chapter 4, communication, goal setting, and care planning. In: Field MJ, Behrman RE, editors. When children die: Improving palliative and end-of-life care for children and their families. Washington, DC: National Academies Press; 2003. [Accessed July 26, 2016]. pp. 104pp. 105–140. http://www.ncbi.nlm.nih.gov/books/NBK220802/ [PubMed] [Google Scholar]