Abstract
Purpose
Superior rectus transposition (SRT) has been popularized for the treatment of abduction deficiencies. Potential complications include induced vertical deviation and torsion. A new procedure, the inferior rectus transposition (IRT) may be similarly beneficial for patients at risk for post-operative vertical deviation or incyclotropia. The purpose of this study is to describe the outcomes of patients undergoing IRT.
Design
Prospective, interventional case series
Methods
Five patients in an academic pediatric ophthalmology and strabismus practice with a complete lateral rectus palsy who underwent IRT were studied. Changes in anomalous head posture, ocular rotations, ocular alignment, and torsion from pre-operative to post-operative were compared.
Results
Patient ages ranged from 19–89 years. There was a significant correction in the angle of esotropia (ET) from 39±17Δ (14–55Δ) to 12±9.8Δ (0–22Δ) postoperatively (P=0.02). Two of five patients had preoperative hypertropia of the affected eye (1.4±2.2Δ; Range 2 – 5Δ). One of those had no vertical deviation postoperatively and one patient resulted in 2Δ hypotropia. One patient without vertical misalignment preoperatively developed a small postoperative vertical deviation. Torticollis significantly improved from 31.4±11.6° to 5±5.8° (P=0.004). All patients improved abduction with a mean of −4.4±0.5 pre-operatively to −3.4±0.9 post-operatively (P=0.07).
Conclusions
Initial postoperative follow up in patients with abducens palsy undergoing IRT demonstrates a significant improvement in ocular alignment and torticollis. In patients with preoperative hypertropia, IRT resulted in a downward shifting effect on the operated eye. IRT may be a beneficial procedure for patients with preoperative hypertropia or intorsion requiring transposition procedures. Future studies with larger populations and longer follow-up will be required before this procedure can be recommended.
Introduction
Complete loss of abduction secondary to an abducens palsy is a difficult clinical situation for which there are a multitude of possible surgeries. In attempt to improve abduction and the field of signal binocular vision, the first partial tendon transposition was described by Hummelshein in 1907.1 Since that time, several variations on the transposition procedure have been introduced, including full-tendon vertical rectus transpositions (VRT),2 the addition of augmentation sutures,3 combining transpositions with medial rectus recession and/or botulinum toxin, and most recently, superior rectus transposition (SRT).4 Recent interest in the SRT has led to several published studies evaluating the efficacy of this procedure in improving ocular alignment, head posture, and abduction.4–6 However, other authors have discussed the potential of inducing intorsion or hypertropia with the use of SRT in certain patients.6,7
Despite the many variations of transposition procedures for complete loss of abduction, there is no specific procedure that is useful as a single procedure for patients who may be at risk for (or already demonstrate) hypertropia or incyclotropia of the affected eye. For this reason, we have performed an inferior rectus transposition (IRT) procedure on these patients, which is similar to the SRT, but instead transposes the inferior rectus muscle to the inferior border of the lateral rectus muscle. Herein we report our experience in our first five patients undergoing this procedure.
Methods
This prospective observational study was approved by the University of California, Los Angeles Institutional Review Board and conformed to the requirements of the United States Health Insurance Portability and Accountability act. The clinical records of all consecutive patients undergoing IRT were reviewed after they underwent surgery. Those subjects who had at least 3 months of post-operative follow-up were included in the analysis. The IRT procedure consisted of a transposition of the inferior rectus to the inferior border of the lateral rectus with the placement of a muscle-to-muscle augmentation suture, combined with a medial rectus recession on an adjustable suture in some cases. The detailed procedure for the IRT was standardized for all patients. A radial fornix conjunctival incision was fashioned inferotemporally. The inferior rectus muscle was isolated on a muscle hook and carefully cleaned from surrounding connective tissue with special attention to clear attachments to the eyelid retractors. A spring-loaded muscle clamp was placed on the inferior rectus muscle and the muscle was detached from the sclera. A double-armed 6-0 polyglactin 910 suture was secured on the inferior rectus muscle. The muscle was transposed temporally. The new insertion of the inferior rectus muscle extended between the inferior corner of the insertion of the lateral rectus muscle and the temporal corner of the insertion of the inferior rectus muscle. The suture was placed on an adjustable bow tie technique. A posterior augmentation adjustable suture was created by placing a single-armed 6-0 polyglactin 910 suture between the lateral rectus muscle and the inferior rectus muscle 8 mm posterior to the muscle insertions capturing approximately 1/3 of the width of the muscles. The inferior rectus muscle was dragged temporally. The posterior augmentation suture was secured and placed on an adjustable bow tie technique with a bolster suture. The radial conjunctival incision was closed with multiple interrupted 8-0 polyglactin 910 sutures in a fashion that allowed the anterior muscle insertion adjustable suture and the posterior augmentation suture to be exposed. In some cases, a medial rectus recession using an adjustable suture was also performed. All patients were evaluated in the recovery room for postoperative adjustment prior to being discharged with the goal of orthotropia in primary position.
The following pre-operative and post-operative characteristics were recorded from the patients’ medical record: age at onset, age at surgery, visual acuity, pre-operative motor alignment at distance and near as well as at distance in sursumversion, dextroversion, levoversion, and deorsumversion, degrees of torticollis, an assessment of ocular ductions, and torsion.
In general, visual acuity was assessed using best refractive correction with projected Snellen optotypes. Ocular alignment was assessed using cover/uncover and prism and alternate cover testing at distance (20 feet) in the seven cardinal gaze positions. Motor alignment at near was assessed at 14 inches. All motor evaluations were performed using spectacle correction. Torticollis was estimated by the experienced strabismologist or measured with a goniometer, in the patient’s habitual head position in degrees. Torticollis was assessed with the subject viewing a distant target. Ocular ductions were measured using a standard 6-point scale with −4 signifying inability to cross the midline, and 0 indicating normal duction. Torsion was assessed objectively by measuring fundus torsion (evaluating the position of the fovea relative to the optic nerve) or subjectively with double Maddox rod testing, depending on patient age and ability.
Statistical analysis
Statistical analyses were performed using Microsoft Excel (Microsoft, Redmond WA). Pre-operative and post-operative values were compared using a paired t-test. A p-value <0.05 was considered statistically significant.
Results
Five patients underwent unilateral IRT for abducens palsy (eTable). The first patient that this procedure was performed on was Patient 1. The procedure was done because the patient had fairly severe deficiency of upgaze secondary to dorsal midbrain syndrome. For this reason, the decision was made to try an IRT since we felt that SRT would be less predictable. After achieving a good result, we tried the procedure on two patients (Patients 2 and 5) who had small pre-operative hypertropias since we had rarely seen hypertropia as a complication after SRT at our center. After those two patients underwent the procedure without complication, we performed the procedure for patient 3, who had a subtle difference in her abduction deficit, being slightly worse inferiorly than superiorly. The patients’ ages ranged from 19 – 89 years. Patient characteristics are depicted in Table 1 and the eTable. Table 2 depicts the changes in strabismus measurements for all patients. Overall, there was a marked improvement in the esotropic deviation from 39±17Δ (range 14–55 PD) to 12±9.8Δ (range 0 – 22Δ) (p=0.02) and torticollis from 31.4±11.6° (0 – 40°) to 5±5.8° (range 0 – 15°) (p=0.004) post-operatively. Pre-operative hypertropic deviation improved from 1.4±2.2Δ (0 – 5Δ) to 0.2±1.8Δ (range 0 to −2Δ) (p=0.37). There was an improvement in abduction for all patients with an average improvement from −4.4±0.5 (range −4 to −5) to −3.4±0.9 (range 0 to −4), p=0.07. None of the patients developed clinically significant torsion postoperatively. Figure 1 shows the range of horizontal movement in patients 1 and 5, pre-operatively and post-operatively. Videos for patients 1, 2, and 5 depict pre-operative and post-operative eye movements in eSupplements 1–3.
Table 1.
Patients undergoing inferior rectus transposition
| ID | Age | Procedure | Pre-Op. Alignment | Post- Alignment | Pre-Op. Torticollis | Post-Op. Torticollis | Pre-Op. Abduction | Post-Op. Abduction | Pre-Op. Adduction | Post-Op. Adduction |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 19 yrs | MRrec 6 mm and IRT OD with PF | 55Δ ET | Orthotropic | 35° | 0° | −4 | −1 | 0 | 0 |
| 2 | 80 yrs | MRrec 3 mm and IRT OS with PF | 42Δ ET, 5Δ HT | 22Δ ET, 2Δ Hypo | 30° | 5° | −5 | −4 | 0 | 0 |
| 3 | 89 yrs | MRrec 6 mm and IRT with PF OS | 53Δ | ET 22Δ | ET 40° | 15° | −5 | −4 | 0 | 0 |
| 4 | 64 years | IRT with PF OS | 30Δ ET | 10Δ ET, 3Δ HT | 40° | 2° | −4 | −2 | 0 | 0 |
| 5 | 76 yrs | IRT with PF OD | 14Δ ET, 2Δ HT | 6Δ ET | 12° | 3° | −4 | −3 | 0 | 0 |
ET: esotropia, HT: hypertropia; MRrec: medial rectus recession (with adjustable sutures in all cases), IRT: inferior rectus transposition (with adjustable sutures in all cases); PF: posterior fixation suture
Table 2.
Mean and Standard Deviation of Pre-Operative and Post-Operative Findings in Patients Undergoing Inferior Rectus Transposition
| Esotropia | Hypertropia | Torticollis | Abduction | Excyclotorsion | |
|---|---|---|---|---|---|
| Pre-Operative | 39±17Δ | 1.4±2.2Δ | 31.4±11.6° | −4.4±0.5 | 0±0 |
| Post-Operative | 12±9.8Δ | 0.2±1.8Δ | 5±5.8° | −3.4±0.9 | 0±0 |
| p-value* | 0.02† | 0.37 | 0.004† | 0.07 | N.A. |
Student’s t-test
p<0.05
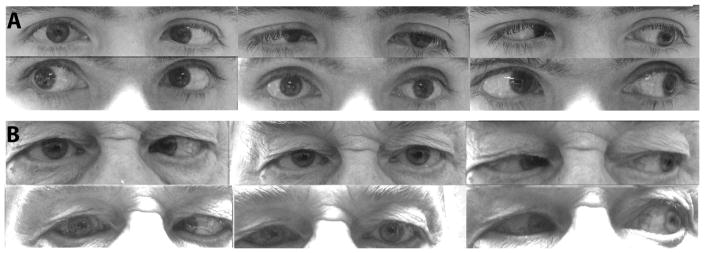
Figure 1.
A. Patient 1 Top row demonstrates ocular rotations pre-operatively. Bottom row demonstrates ocular rotations after inferior rectus transposition. B. Patient 5. Top row demonstrates ocular rotations pre-operatively. Bottom row demonstrates ocular rotations after inferior rectus transposition.
Two patients had a preoperative hypertropia of the involved eye. One of those patients with a preoperative vertical deviation of 2Δ resulted in resolution of their vertical deviation postoperatively. One patient with a preoperative hypertropia of 5 Δ and had a resultant 2Δ of postoperative hypotropia. This patient had no induced torsional effect from the surgery. One patient (patient 4) without preoperative vertical misalignment had an induced vertical deviation postoperatively. Interestingly, this post-operative vertical deviation was not present initially but developed at the post-operative month 3 visit. In addition, at that visit, the patient had an increased amount of esotropia (from 5 PD to 10 PD). This constellation of findings was consistent with a slight slippage inferiorly of the transposed inferior rectus; however, the patient was happy with her alignment, and so no further procedures were performed.
All of the patients were evaluated in the recovery room approximately 2 hours after surgery had ended, and after they were completely discharged. Patients were measured using a 20/400 target at approximately 20 feet away using the proper prescription. Two patients underwent further medial rectus muscle recession for small residual esotropia. All patients were able to fuse in the recovery room with orthotropia in primary position and no face turn or a small face turn. In all patients, no adjustment was performed to the point where the adduction of the operated eye was affected in order to avoid a resultant adduction deficiency and exotropia in contralateral gaze.
Discussion
Vertical rectus transposition surgery was introduced more than a century ago by Hummelshein.1 Since that time, several variations have been reported, and benefits of the procedure such as improved field of binocular single vision and improved abduction have been reported.8 Given the relatively high incidence of vertical deviations after VRT as well as the risk of anterior segment ischemia,9,10 the SRT was introduced in 2006 by Johnston et al.11 The procedure was further popularized by Mehendale, et al.4 Despite excellent reported results, and a low risk of complications, the SRT may place certain patients at risk for post-operative incyclotropia or hypertropia.6,7 Patients at risk for these complications include younger patients, as well as patients with pre-operative hypertropia or incyclotropia.7 We have therefore designed a procedure by which the benefits of a transposition procedure can be obtained without worsening, and with the potential to improve, a pre-existing hypertropia or incyclotropia.
Since the introduction of rectus muscle transposition, there has been debate regarding the risk-benefit ratio of the procedure compared to the more simple medial rectus recession. When compared to medial rectus recession, the VRT procedure reportedly has a larger effect on the size of the diplopia-free binocular visual field, as well as abduction improvement.8 The SRT has also been compared to simple medial rectus recession procedures, and similarly results in a significantly better improvement in abduction as well as long-term esotropia control.5,6 Despite these advantages, many clinicians continue to prefer medial rectus recession as the first procedure for patients with Duane syndrome, or a recess/resect procedure for patients with abducens palsy, given the risks associated with rectus muscle transposition, including anterior segment ischemia, induced vertical deviation, and over-correction.7,9,10 Despite these risks, in our clinical practice, we prefer to utilize transposition procedures as the primary surgery for patients with complete loss of abduction, and in doing so have increasingly utilized SRT procedures. With the knowledge that some patients who have completely lost abduction may have a co-existent hypertropia or incyclotropia, we felt it necessary to create a complementary procedure to the SRT for this population.
In our series of five patients undergoing IRT, we initially chose the procedure out of concern for the vertical deviation. Induced vertical deviations appear to be less common in patients undergoing superior rectus muscle transposition (SRT) without inferior rectus muscle transposition.4 However it has been our experience that hypertropias are more common than hypotropias following SRT. We initially performed IRT in patients with abduction paralysis who also had an ipsilateral hypertropia. In our experience, only one of our patients undergoing IRT had a postoperative hypertropia and this occurred after three months potentially secondary to slippage of the inferior rectus, given that it appeared on examination at the same time as a small increase in the patient’s esotropia. Another possibility is that her adjustable posterior fixation suture was loosened or weakened, as she did not demonstrate any limitation to downgaze.
In our series, the youngest patient had the best abduction improvement following IRT. This patient also had the largest preoperative deviation in the primary position. Conversely, two older patients (patients 2 and 3) with large deviations and more limited abduction (−5) who had orthotropia postoperatively after adjustment had recurrent esotropia in primary position. Both patients were able to wear prism glasses or compensate their deviation with a face turn.
Mehendale et al. reported 7 patients with abduction paralysis who underwent superior rectus muscle augmented transposition combined with medial rectus recession and found a mean esotropic correction of 36.7Δ, 31° correction of torticollis and 1.8 improvement in abduction.4 However, their values for mean correction of esotropia, torticollis and abduction included 10 patients with Duane syndrome in addition to their seven patients with abducens palsies. Two (28%) of their patients developed an induced vertical deviation. Three of six (50%) patients with postoperative torsion measurements developed asymptomatic intorsion. Following IRT, we found a mean esotropic correction of 27.8Δ, 24° correction in torticollis and 1.9 improvement in abduction. One (20%) patient had an induced 2Δ hypotropia and one had an induced hypertropia of 3Δ. None of the IRT patients developed postoperative symptomatic extorsion. Although our mean esotropic correction is similar to the results of Mehendale et al., our population is smaller in size and includes a wide range of results. Therefore, it is premature to make direct comparisons. In addition, in Mehendale’s series, patient age ranged from 6 to 60 years, compared to our series where all except one patient were older than 63 years. Therefore, our two populations may not be directly comparable as age may be a factor influencing results following transposition surgery. In addition, we found a mean vertical correction towards hypotropia of 1.2Δ. Mehendale et all did not report the magnitude of induced vertical deviation following SRT in their 2 patients who reportedly had vertical deviations postoperatively. It remains unknown if some patients with preoperative hypotropia resulted in an upward vertical shift after SRT. In our own previous series of patients undergoing SRT,7 we found that the mean induced torsion by SRT was approximately 4.7 degrees in a cohort of 11 subjects.
Despite this study reporting the first five patients undergoing our IRT procedure at our institution, our results must be understood within the context of their limitations. First, this is a small study and the results cannot be widely applied. In addition, follow-up time was relatively short at a minimum of 8 weeks, and binocular single visual fields were not performed. However, despite these limitations, we believe that our results are important to disseminate at this time, so that this procedure can be considered in the appropriate patient population.
In conclusion, the IRT procedure may be useful in patients who wish to reap the benefits of transposition procedures such as improved abduction, but are at risk for post-operative incyclotropia such as patients with a partial third nerve palsy and inferior oblique palsy. In addition, in patients with abducens palsy who have a pre-existing hypertropia, this procedure may be useful to address both the esotropia and hypertropia by operating on a single vertical rectus muscle. However, we must proceed with caution, as longer follow-up and larger studies are needed. Future studies should include a larger sample of patients to define the long-term efficacy as well as possible post-operative complications of this procedure.
Supplementary Material
Acknowledgments
Funding/Support: NIH/NEI K23EY021762 (SLP), Research to Prevent Blindness (FGV, SLP)
Financial Disclosures: No financial disclosures (all authors)
Other acknowledgements: None
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hummelshein E. Uber Schnentransplantation am Ague. Ophthal Gesselschft. 1907;34:248–253. [Google Scholar]
- 2.Schillinger RJ. A new type of tendon transplant operation for abducens paralysis. J Int Coll Surg. 1959 May;31(5):593–600. [PubMed] [Google Scholar]
- 3.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997 Mar;1(1):20–30. doi: 10.1016/s1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 4.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012 Feb;130(2):195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tibrewal S, Sachdeva V, Ali MH, Kekunnaya R. Comparison of augmented superior rectus transposition with medial rectus recession for surgical management of esotropic Duane retraction syndrome. J AAPOS. 2015 Jun;19(3):199–205. doi: 10.1016/j.jaapos.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Yang S, MacKinnon S, Dagi LR, Hunter DG. Superior rectus transposition vs medial rectus recession for treatment of esotropic Duane syndrome. JAMA Ophthalmol. 2014 Jun;132(6):669–675. doi: 10.1001/jamaophthalmol.2014.358. [DOI] [PubMed] [Google Scholar]
- 7.Velez FG, Oltra E, Isenberg SJ, Pineles SL. Assessment of torsion after superior rectus transposition with or without medial rectus recession for Duane syndrome and abducens nerve palsy. J AAPOS. 2014 Oct;18(5):457–460. doi: 10.1016/j.jaapos.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenbaum AL. Costenbader Lecture. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004 Oct;8(5):409–419. doi: 10.1016/j.jaapos.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Murdock TJ, Kushner BJ. Anterior segment ischemia after surgery on 2 vertical rectus muscles augmented with lateral fixation sutures. J AAPOS. 2001 Oct;5(5):323–324. doi: 10.1067/mpa.2001.118668. [DOI] [PubMed] [Google Scholar]
- 10.Ruth AL, Velez FG, Rosenbaum AL. Management of vertical deviations after vertical rectus transposition surgery. J AAPOS. 2009 Feb;13(1):16–19. doi: 10.1016/j.jaapos.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Johnston SC, Crouch ERJ, Crouch ER. An innovative approach to transposition surgery is effective in treatment of Duane’s syndrome with esotropia [ARVO abstract] Invest Ophthalmol Vis Sci. 2006;47 e-abstract 2475. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.