El Niño and cholera in Africa
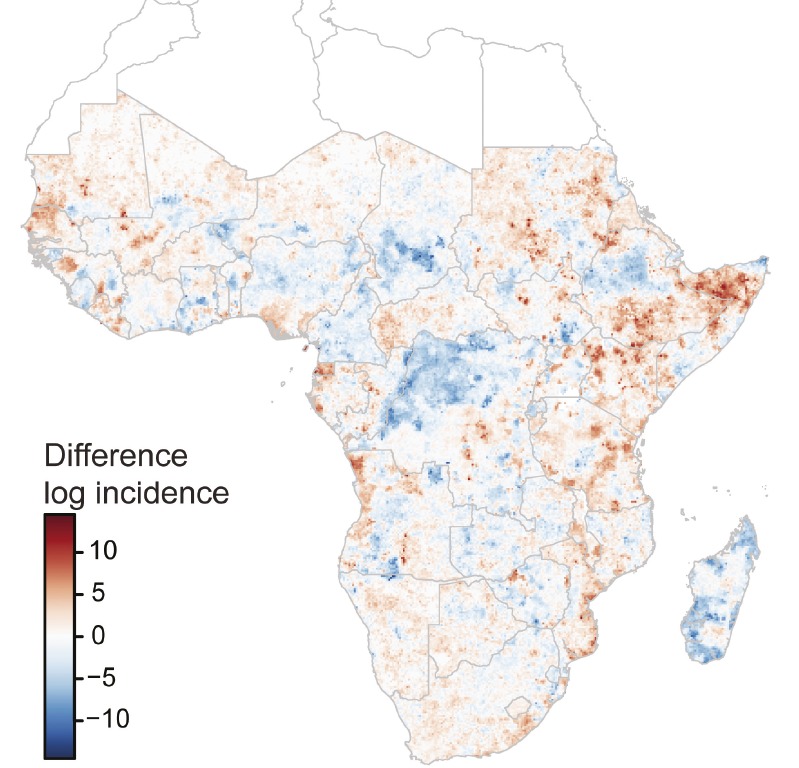
Cholera incidence rates between El Niño and non-El Niño years throughout Africa.
Cholera outbreaks have long been linked to climatic factors, particularly the El Niño Southern Oscillation, but little evidence supports such a link in Africa. Using datasets comprising more than 17,000 annual observations of cholera incidence, Sean Moore et al. (pp. 4436–4441) mapped the locations of cholera incidence throughout Africa at a fine scale during the years 2000–2014. The total number of cholera cases did not vary between El Niño years and non-El Niño years, but the geographic distribution of cases shifted, with approximately 50,000 additional cases in East Africa and 30,000 fewer cases in southern Africa during El Niño years than during non-El Niño years. Overall, 177 million people live in areas where cholera incidence increased during El Niño years by at least 1 per 100,000 people. Within regions where the association between El Niño and increased cholera incidence was strongest, cholera incidence tripled during El Niño years. Effective care during cholera outbreaks can drastically reduce mortality, and current climate forecasts can predict El Niño events up to 12 months in advance. Therefore, increasing disease surveillance and preparedness in response to El Niño predictions could help reduce cholera-associated mortality, according to the authors. — B.D.
Seizure-induced brain dysfunction and exosomes
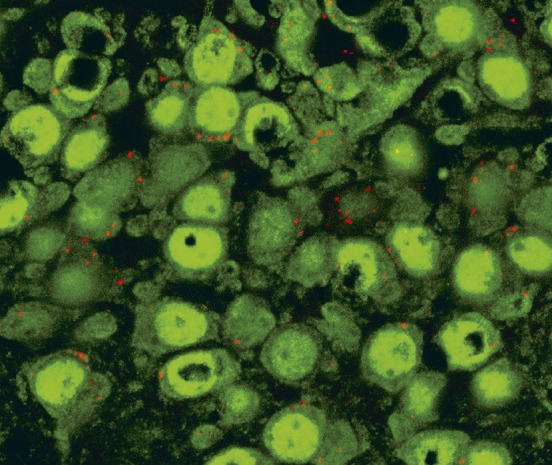
A1-exosomes (red) targeting hippocampal neurons (green) within 6 hours of intranasal administration.
Status epilepticus (SE), a prolonged period of continuous or recurring seizures without regaining consciousness, is a condition that can lead to persistent neuroinflammation, neurodegeneration, and aberrant neurogenesis, as well as cognitive and memory impairments. Bone marrow-derived stem cells have shown potential for alleviating the adverse consequences of SE, but clinical therapies based on stem cells face considerable challenges. Qianfa Long et al. (pp. E3536–E3545) investigated the effects of intranasal administration of extracellular vesicles (EVs) derived from human mesenchymal stem cells in a mouse model of SE. The EVs, called A1-exosomes, have been shown to have robust antiinflammatory properties. Mice that received exosomes following SE exhibited lower levels of proinflammatory cytokines and microglial activation, and higher levels of antiinflammatory cytokines, in the hippocampus than mice that did not receive exosomes, indicating reduced inflammation in exosome-treated mice. Mice that received exosomes also lost fewer hippocampal neurons than mice that did not receive exosomes, and did not exhibit the cognitive and memory impairment or abnormal neurogenesis observed in the nonexosome-treated mice following SE. The results suggest the therapeutic potential of stem cell-derived EVs for preventing chronic hippocampus dysfunction induced by SE, according to the authors. — B.D.


