Abstract
Aims
To determine and quantify the prevalence of patient, provider and system level barriers to achieving diabetes care goals; and to examine whether barriers were different for people with poor glycemic control (HbA1c ≥ 10%; 86 mmol/mol) compared to fair glycemic control (7 to <8%; 53–64 mmol/mol).
Methods
We administered a survey by telephone to community-dwelling patients with diabetes, to examine patient-reported barriers and facilitators to care. We compared responses in individuals with HbA1c ≥ 10% (86 mmol/mol) against those with HbA1c between 7–8% (53–64 mmol/mol). We examined associations between HbA1c group and barriers to care, adjusting for sociodemographic factors and diabetes duration.
Results
The survey included 805 people with HbA1c ≥ 10% (86 mmol/mol), and 405 people with HbA1c 7–8% (53–64 mmol/mol). Participants with HbA1c ≥ 10% (86 mmol/mol) reported good access to care, however 20% of participants with HbA1c ≥ 10% (86 mmol/mol) felt that their care was not well-coordinated and 9.6% reported having an unmet health care need. In adjusted analysis, patients with HbA1c ≥10% (86 mmol/mol) were more likely to report lack of confidence and inadequate social support, compared to patients with HbA1c 7–8% (53–64 mmol/mol). They were also significantly more likely not to have drug insurance nor to have received recommended treatments because of cost.
Conclusions
These results reinforce the importance of an individualized, yet multi-faceted approach. Specific attention to financial barriers seems warranted. These findings can inform the development of programs and initiatives to overcome barriers to care, and improve diabetes care and outcomes.
Introduction
Diabetes affects more than 2.4 million Canadians [1], and is associated with high morbidity and mortality [1, 2]. Patients who do not achieve recommended clinical targets, such as glycemic control, are at higher risk of complications and incur higher health care costs [3–5]. Patients with the worst control (HbA1c ≥ 10%; 86 mmol/mol) have a 30% higher risk of myocardial infarction compared to those with HbA1c between 7 and 8% (53–64 mmol/mol) and a fourfold increased risk of microvascular complications [5].
Safe, cost-effective interventions for diabetes are available to reduce the risk of microvascular and macrovascular complications, but these treatments remain underutilized [6–13]. For instance, only 50% of Albertans with diabetes are on statin therapy, which has been shown to reduce cardiovascular risk among people with diabetes [6]. There is an urgent need to understand these care gaps to improve health outcomes in people with diabetes [14].
At the same time, patients with diabetes are burdened by complex treatment regimens including administration of medications, clinical monitoring, and dietary and lifestyle changes [15]. Patients must also make decisions about when and how to seek medical care. Optimal self-management depends on a number of factors, including health status, financial status, access to care, care experience and personal circumstances. A comprehensive understanding of patient, provider, and system-level barriers is needed to inform the development of contextually-tailored interventions to support self-management and improve outcomes for diabetes patients [16].
The purpose of this study was to determine and quantify the prevalence of patient, provider and system-level barriers to achieving diabetes care goals. We also sought to examine whether these barriers differed for people with poor glycemic control (HbA1c ≥ 10% (86 mmol/mol)) compared to fair glycemic control (7 to 8% (53–64 mmol/mol)), within four broad domains: Health status; Health care experience; Self-management; and Financial status.
Patients and methods
We conducted a large, cross-sectional survey administered by telephone interview that asked patients about their health status, health care experience, self-management behaviours and financial barriers. The University of Calgary Conjoint Health Research Ethics Board has approved this research study.
Participants
The target population was community-dwelling adults over 18 years living in the city of Calgary, Alberta and surrounding regions (catchment population 1.5 million), with a diagnosis of diabetes who had an HbA1c ≥ 10% (86 mmol/mol) or between 7 and 8% (53–64 mmol/mol). The sample was drawn from adult outpatient users of Calgary Laboratory Services (CLS) with valid telephone numbers, who had an outpatient HbA1c blood test between October 1, 2013 and April 30, 2014. Only patients with a prior HbA1c test ≥ 7% (53 mmol/mol) were eligible, to ensure that they had an established diagnosis of diabetes. Ordering physicians were notified by facsimile of our intent to contact their patient(s), and was given the option of contacting researchers to exclude individual patients from the survey. We included patients of family physicians, walk-in clinics and specialist clinics, to enable us to reach patients that would otherwise be inaccessible, while still providing ordering physicians the opportunity to exclude their patients if deemed inappropriate.
Recruitment
Patients were contacted by telephone and invited to participate in a survey about diabetes care delivery in Alberta. Interviewers had no information about test results. Patients were asked to provide verbal consent to be interviewed; as the questionnaire was administered by telephone interview, it was infeasible to obtain written consent. All participants were given the option to end the survey at any time. When a participant agreed to participate in the interview, their consent was recorded as an item in the computer-assisted data capture system. The University of Calgary Conjoint Health Research Ethics Board approved this consent procedure. Individuals with gestational diabetes or who were unaware of their diabetes diagnosis were excluded. All patients were contacted between January and May 2014, within 90 days of the date of the HbA1c test to ensure that the survey data was timely and relevant. Standardized scripting was used to explain the purpose of the survey and answer questions regarding information security and privacy.
Data collection
Trained interviewers working within the provincial health care system administered the questionnaire. Data were collected using computer-assisted telephone interviews, where participant responses were captured directly into data collection software.
Questionnaire
The survey was organized into four domains: health status, health care experience, self-management, financial barriers; and sociodemographic information. The domains were adapted from the Barriers to Diabetes Self-Care Behaviours Model [17], and modified to include additional information on financial status, which has been identified as a barrier for some patients [18]. Within each domain, key indicators representing patient-reported barriers (Table 1) were chosen based on findings from past studies [17], and were contextualized within health care programming available for individuals with diabetes in the Calgary area. The wording of specific questions was adopted from prior Statistics Canada Health Surveys (CCHS, CSEPHC, SLCDC-DM, BCPCHC, available from www.statcan.gc.ca) and validated questionnaires where possible. Pilot testing indicated that the questions had face validity, were acceptable to patients, and could be answered within a comfortable timeframe.
Table 1. Key indicators of barriers and facilitators to care by survey domain.
| Domain | Subdomains | Key indicators |
|---|---|---|
| Health status |
General health Diabetes status Health risks |
• General health status • Depressive symptoms |
| Health care experience |
Health care team Access to care Communication |
• Regular family doctor/usual place of care • Continuity of care with same family doctor • Accessed allied health care • Accessed specialist if recommended • Accessed specialized diabetes clinic • Accessed community programs • Communication with providers • Coordination of care across providers |
| Self-management |
Medications Lifestyle Patient activation Social support |
• Confidence in being able to follow through with treatments • Having knowledge to prevent further problems • Motivation to do a better job with diabetes self-management • Ability to fill out medical forms • Having adequate social support |
| Financial barriers |
Insurance status Ability to pay |
• Insurance to cover prescription medications? • Difficulty paying for medications • Unable to get diabetes related treatments due to cost • Able to afford healthy foods |
Analysis
Sociodemographic and clinical characteristics of the survey respondents were described by HbA1c category, using summary statistics. We summarized the prevalence of key indicators for those with poor glycemic control (HbA1c ≥ 10%; 86 mmol/mol) and those with fair glycemic control (HbA1c 7 to 8%; 53–64 mmol/mol). Modified Poisson regression [19] was used to determine the association between HbA1c group (HbA1c ≥ 10% (86 mmol/mol) or HbA1c 7 to 8% (53–64 mmol/mol)) and key indicators, adjusting for age, sex, income, ethnicity, community size and diabetes duration. Complementary data, including type of care accessed, reasons for not accessing care, and reasons for having an unmet health care need were summarized descriptively.
Sample size
We determined sample size for statistical comparisons between HbA1c groups. We examined three key indicator variables: proportion with depression, proportion without a regular family doctor, and proportion unable to pay for medications. Based on prior work, we estimated the proportion with each of these indicators among all patients with diabetes: 12–25% with depression [17, 20, 21], 5% without a regular family doctor [22], 12% with difficulty paying for medications [22]. For a desired precision of +/- 5% in prevalence estimate, our most restrictive estimate (25% with depression) yields a minimum sample size of 384, assuming a random sample [23]. For comparisons between groups of glycemic control, assuming two independent samples and a power of 0.80 to detect a minimum detectable absolute difference in prevalence between groups of 10%, 400 patients were required in each sample [23]. To ensure the stability of our estimates and to provide some additional capacity to perform correlational analyses and comparison across sociodemographic groups we chose to aim for 800 completed interviews in patients with HbA1c ≥ 10% (86 mmol/mol), and 400 completed interviews in patients with HbA1c 7–8% (53–64 mmol/mol).
Results
Survey response
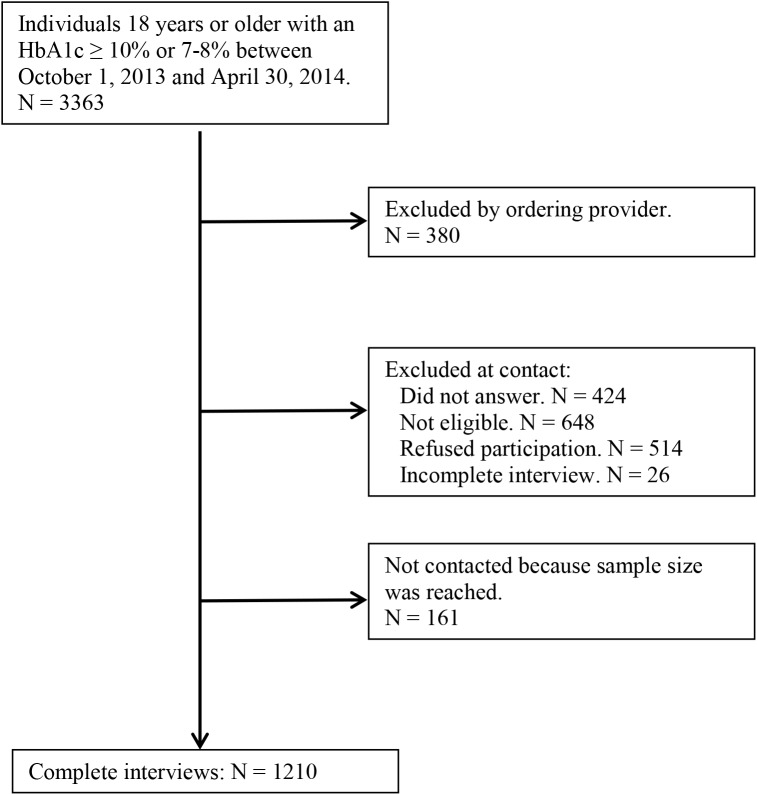
In total, 3363 patients were identified as having HbA1c tests performed; 380 (12.7%) were excluded from contact by the ordering provider. The most common reasons for exclusion were language barrier and dementia. The average age of excluded patients was 65.2 years and 51.6% were male, compared to 60.0 years and 59.4% male for patients not excluded. Of the patients that were eligible for contact, 2822 were called. Of these, 424 did not answer, 648 were disqualified, 514 refused, and 26 did not complete the interview. Ineligibility was most commonly due to language barrier (181), telephone number not in service (154), ineligibility (101), wrong number (65), inability to communicate (55), and other. There were no differences in reasons for exclusion between the HbA1c groups. We thus completed 1210 surveys, with a 44% response rate overall, and a 71% response rate in those who were contacted and qualified to participate (Fig 1). There was no significant difference in response rate by sex or HbA1c group, though we did observe lower response rates in those aged ≥75.
Fig 1. Details of participant selection.
Patient characteristics
Table 2 summarizes patient characteristics by HbA1c group. Patients with HbA1c ≥ 10% (86 mmol/mol) had an average age of 57.1 years, and 60% were male. Most were high school educated (88%), and were employed, retired, or in school (86.2%). Household income varied, with 13.8% having an annual household income of <$20,000. Two-thirds were born in Canada, 71% were white, and over 75% were city dwellers. Compared to the group with HbA1c 7–8% (53–64 mmol/mol), individuals with HbA1c ≥ 10% (86 mmol/mol) were younger and fewer were retired (23.2% vs. 47.3%). Average income was higher in the HbA1c ≥ 10% (86 mmol/mol) group, although this may reflect fewer retirees in this group. There was also a higher proportion of rural/small community dwellers in the HbA1c ≥ 10% (86 mmol/mol) group (15.8% vs. 4.2%).
Table 2. Patient characteristics summarized by HbA1c group [n (%)].
| HbA1c ≥ 10% N = 805 |
HbA1c 7–8% N = 405 |
p-value | |
|---|---|---|---|
| Sociodemographics | |||
| Age in years, mean (s.d.) | 57.1 (12.5) | 64.5 (11.8) | <0.001 |
| Age group | <0.001 | ||
| <50 | 200 (24.8) | 37 (9.1) | |
| 50–64 | 389 (48.3) | 142 (35.1) | |
| 65–74 | 150 (18.6) | 152 (37.5) | |
| 75+ | 66 (8.2) | 74 (18.3) | |
| Male | 60.4 | 58.8 | 0.59 |
| Education–highest level achieved | 0.73 | ||
| Less than high school | 95 (12.0) | 47 (11.9) | |
| High school | 227 (28.6) | 104 (26.3) | |
| Post-secondary but no bachelor’s degree | 279 (35.2) | 151 (38.2) | |
| Bachelor’s degree or higher | 192 (24.2) | 93 (23.5) | |
| Employment | <0.001 | ||
| Employed FT/PT/self-employed | 477 (59.5) | 160 (39.6) | |
| Unemployed, looking for work | 24 (3.0) | 6 (1.5) | |
| Unable to work–sickness or disability | 87 (10.8) | 35 (8.7) | |
| Retired | 186 (23.2) | 191 (47.3) | |
| Other (at school, full-time home-maker) | 28 (3.5) | 12 (3.0) | |
| Household income | 0.03 | ||
| < $20,000 | 99 (13.8) | 46 (12.9) | |
| $20,000 to < $50,000 | 200 (27.9) | 132 (37.1) | |
| $50,000 to < $100,000 | 235 (32.7) | 95 (26.7) | |
| $100,000+ | 184 (25.6) | 83 (23.3) | |
| Unreported | 87 (10.8) | 49 (12.1) | |
| Marital status | 0.67 | ||
| Married/common-law | 539 (67.5) | 275 (68.8) | |
| Widowed/separated/divorced/never married | 259 (32.5) | 125 (31.2) | |
| Born in Canada | 0.86 | ||
| Yes | 532 (66.2) | 269 (66.8) | |
| No | 271 (33.8) | 134 (33.2) | |
| Racial/cultural origin | 0.13 | ||
| White | 564 (71.0) | 306 (76.5) | |
| Aboriginal | 33 (4.2) | 12 (3.0) | |
| Other | 197 (24.8) | 82 (20.5) | |
| Community size | <0.001 | ||
| Large population centre (100,000+) | 615 (76.8) | 368 (90.8) | |
| Medium population centre (30,000–99,999) | 59 (7.4) | 20 (5.0) | |
| Small population centre (1,000–29,999) | 82 (10.2) | 11 (2.7) | |
| Rural area | 45 (5.6) | 6 (1.5) | |
| Diabetes treatment | |||
| Duration of diabetes | 0.62 | ||
| < 1 year | 34 (4.2) | 22 (5.5) | |
| 1 to 5 years | 202 (25.1) | 91 (22.6) | |
| 6 to 10 years | 205 (25.5) | 108 (26.8) | |
| > 10 years | 363 (45.2) | 182 (45.2) | |
| Number of prescribed medications | 0.18 | ||
| 0–2 | 139 (17.3) | 68 (16.9) | |
| 3–4 | 250 (31.2) | 103 (25.6) | |
| 5–9 | 318 (39.6) | 182 (45.3) | |
| 10+ | 95 (11.8) | 49 (12.2) | |
| Insulin | 493 (61.2) | 166 (41.2) | <0.001 |
| Other diabetic agents | 603 (75.3) | 294 (73.3) | 0.46 |
| Anti-hypertensive agents | 538 (67.1) | 302 (75.1) | 0.004 |
| Cholesterol-lowering agents | 501 (62.8) | 292 (73.0) | <0.001 |
| ASA | 371 (46.2) | 242 (59.8) | <0.001 |
| Health status | |||
| General health status | 0.015 | ||
| Excellent/very good | 199 (24.9) | 126 (31.3) | |
| Good | 351 (43.9) | 171 (42.4) | |
| Fair/poor | 249 (31.2) | 106 (26.3) | |
| Hypertension | 544(67.9) | 296 (73.4) | 0.048 |
| Retinopathy | 133 (17.1) | 59 (15.4) | 0.46 |
| Heart disease | 164 (20.5) | 99 (24.7) | 0.10 |
| Neuropathy | 182 (23.6) | 83 (21.7) | 0.48 |
| Obesity | 0.002 | ||
| Non-obese (BMI < 30) | 380 (48.5) | 223 (57.3) | |
| Obese (BMI 30–40) | 323 (41.2) | 139 (35.7) | |
| Morbidly obese (BMI > 40) | 81 (10.3) | 27 (6.9) | |
| Depressive symptoms | 338 (42.2) | 141 (34.8) | 0.013 |
| Current smoker | 102 (12.8) | 40 (9.9) | 0.15 |
Health status
Nearly half of participants reported having diabetes for over 10 years, and over half were taking five or more medications, with no difference between groups. 61.2% of patients with HbA1c ≥ 10% (86 mmol/mol) were on insulin, which was significantly greater than those with HbA1c 7–8% (53–64 mmol/mol) (i.e., 41.2%). Conversely, the proportion of participants in the HbA1c ≥ 10% (86 mmol/mol) group that were on anti-hypertensive (67.1%) and/or cardioprotective medications (62.8% for lowering cholesterol and 46.2% for ASA therapy) was significantly lower than in the HbA1c 7–8% (53–64 mmol/mol) group. Patients with HbA1c ≥10% (86 mmol/mol) were significantly more likely to report fair or poor health status (31.2% vs. 26.3%), obesity (51.5% vs. 42.8%) and depressive symptoms (42.2% vs. 34.8%).
Health care experience
Nearly all patients in our survey (98%) reported having a regular family doctor or usual place of care, and 90% and 93% of those with HbA1c ≥10% (86 mmol/mol) and HbA1c 7–8% (53–64 mmol/mol), respectively, reported seeing the same doctor most or all of the time (Table 3). Patients with HbA1c ≥10% (86 mmol/mol) saw their family doctor more frequently than those with HbA1c 7–8% (53–64 mmol/mol), with 20% of patients reporting more than six visits in the prior 12 months. Patients with HbA1c ≥10% (86 mmol/mol) were also more likely to have seen an allied health care practitioner (77.5% vs. 69.6%) and were more likely to have been referred to a specialist (47.1% vs. 36.1%). When asked specifically about encounters with other health care professionals, pharmacists were the most prevalent (56%), followed by diabetes nurse (40%), dietician (35%), social worker (6.7%) and mental health worker (6.7%). Patients reported accessing a range of community programs, including group education, group exercise, and support groups, with no significant differences between groups. Finally, 9.6% of patients with HbA1c ≥ 10% (86 mmol/mol) reported that they had an unmet health care need related to diabetes in the last 12 months, compared with 4.8% of those with HbA1c 7–8% (53–64 mmol/mol). The most commonly cited reasons for having an unmet health care need were unsatisfactory care and/or communication, long wait times and cost.
Table 3. Patient responses by survey domain.
| HbA1c ≥ 10% | HbA1c 7–8% | p-value | |
|---|---|---|---|
| Health care experience | |||
| Regular family doctor/usual place of primary care | 785 (97.5) | 398 (98.3) | 0.40 |
| Continuity with primary care physician | 713 (89.8) | 372 (93.0) | 0.07 |
| # of visits with family doctor in last 12 months | 0.001 | ||
| 0 | 30 (3.7) | 23 (5.7) | |
| 1 | 49 (6.1) | 42 (10.4) | |
| 2–6 | 559 (69.7) | 276 (68.3) | |
| >6 | 164 (20.5) | 63 (15.6) | |
| Use of allied health care in past 12 months | 624 (77.5) | 281 (69.6) | 0.003 |
| Referred to a specialist for diabetes | 379 (47.3) | 146 (36.1) | <0.001 |
| Specialist care in past 12 months (if referred, n = 525) | 270 (71.2) | 111 (76.0) | 0.27 |
| Contact with diabetes clinic in past 12 months | 167 (20.8) | 62 (15.4) | 0.023 |
| Use of community programs past 12 months | 143 (17.8) | 60 (14.9) | 0.20 |
| Unmet health care need in last 12 months | 75 (9.6%) | 19 (4.8%) | 0.005 |
| Suboptimal provider communication | 137 (17.8) | 64 (16.4) | 0.53 |
| Suboptimal coordination of care | 143 (20.1) | 48 (14.2) | 0.02 |
| Self-management | |||
| Patient activation | |||
| Not confident can follow through | 32 (4.0) | 5 (1.2) | 0.008 |
| Don’t know how to prevent further problems | 84 (10.6) | 27 (6.9) | 0.038 |
| Motivated to do a better job managing diabetes | 0.001 | ||
| Strongly agree/agree | 596 (74.5) | 270 (67.0) | |
| Disagree/strongly disagree | 46 (5.8) | 16 (4.0) | |
| N/A (already doing a good job) | 158 (19.8) | 117 (29.0) | |
| Lacking confidence in filling out medical forms | 312 (39.8) | 142 (36.1) | 0.22 |
| Not enough information re managing diabetes | 143 (18.0) | 66 (16.4) | 0.49 |
| Enough social support re diabetes | 0.01 | ||
| Always/often | 455 (59.9) | 252 (67.4) | |
| Sometimes | 108 (14.2) | 47 (12.6) | |
| Rarely/never | 197 (25.9) | 75 (20.0) | |
| Financial barriers | |||
| No drug insurance | 108 (13.4) | 36 (8.9) | 0.02 |
| Difficulty paying for drugs/equip/services (always/often/sometimes) | 233 (29.4) | 95 (23.6) | 0.03 |
| Did not get needed treatments because of cost (always/often/sometimes) | 119 (15.0) | 36 (9.0) | 0.003 |
| Unable to afford healthy foods (always/often/sometimes) | 164 (20.8) | 56 (14.1) | 0.005 |
Patients who did not have a family doctor were asked to provide a reason, with the most common response being that their family doctor had retired or moved (51.6%). Of patients who were referred to a specialist physician but did not see one (24% for HbA1c 7–8% (53–64 mmol/mol) and 29% for HbA1c ≥ 10% (86 mmol/mol)), the most common reasons for not going were that it ended up not being necessary, long wait times and lack of time. 17.8% of participants with HbA1c ≥ 10% (86 mmol/mol) felt that provider communication was suboptimal, with no difference between groups; patients with HbA1c ≥10% (86 mmol/mol) were significantly more likely to report suboptimal provider coordination of care (20.1% vs. 14.2%).
Self-management and financial barriers
Despite poor glycemic control, individuals with HbA1c ≥ 10% (86 mmol/mol) were more likely to be motivated (74.5% vs. 67.0%) than those with HbA1c 7–8% (53–64 mmol/mol), but also more likely to report lack of confidence in being able to follow through with their treatment plan (4.0% vs. 1.2%) and/or lack of skills to prevent disease related-complications (10.6% vs. 6.9%). Individuals with HbA1c ≥ 10% (86 mmol/mol) were less likely to have good social support (59.9% vs. 67.4%), and were more likely to have financial barriers to care, compared with the HbA1c 7–8% (53–64 mmol/mol) group. Specifically, more individuals with HbA1c ≥ 10% (86 mmol/mol) did not have drug insurance (13.4% vs. 8.9%), and reported not being able to access medications and/or medical supplies due to cost (15.0% vs. 9.0%), or to afford healthy foods (20.8% vs. 14.1%) (Table 3).
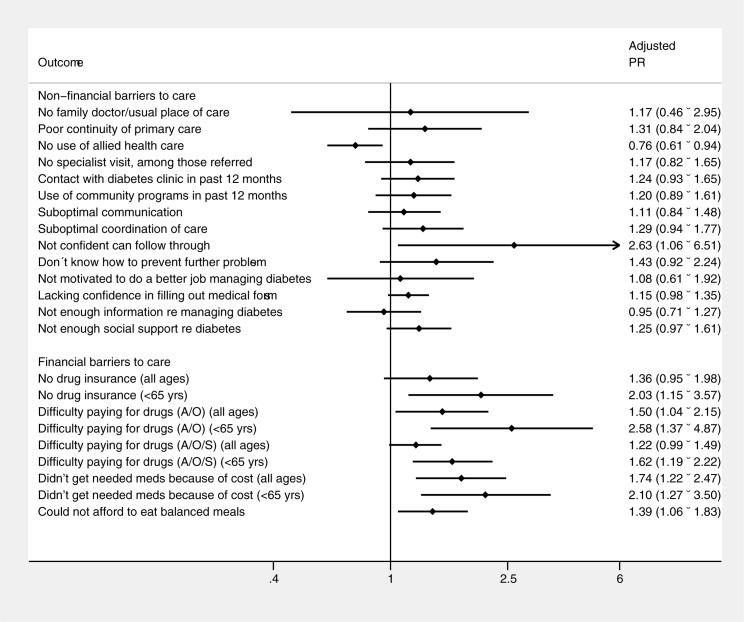
Adjusted comparisons between HbA1c groups for key indicators
We examined the statistical association between HbA1c group and the prevalence of key indicators of barriers and facilitators to care, adjusting for sociodemographic factors and duration of diabetes (Fig 2). After adjustment for covariates, we found that participants with HbA1c ≥ 10% (86 mmol/mol) remained more likely to report a lack of confidence (PRR 2.36, 95% CI 1.06–6.51). We found significant associations between having an HbA1c ≥ 10% (86 mmol/mol) and financial barriers, with a stronger association among those under 65 (i.e., a population of individuals who have to pay a premium to access government-sponsored drug insurance). Participants with HbA1c ≥10% (86 mmol/mol) were more likely to report not having drug insurance (PRR 2.03, 95% CI 1.15–3.57, for those under 65), not getting needed medications because of cost (PRR 1.74, 95% CI 1.22–2.47, for all participants) and difficulty affording balanced meals (PRR 1.39, 95% CI 1.06–1.83, for all participants).
Fig 2. Adjusted prevalence ratios for barriers to care in participants with HbA1c ≥ 10% compared with participants with HbA1c 7–8%.
Conclusions
In this population-based survey of individuals with diabetes, we examined factors associated with diabetes care and potential barriers to care across several domains, and compared responses from patients with poor glycemic control to those with fair glycemic control. We found that, in general, people with HbA1c ≥ 10% (86 mmol/mol) were younger but in worse health than those with HbA1c 7–8% (53–64 mmol/mol). We found few differences in access to care between groups but noted that patients with HbA1c ≥ 10% (86 mmol/mol) were more likely to struggle with confidence and appeared to have fewer social supports. Financial barriers were significantly more common in patients with HbA1c ≥ 10% (86 mmol/mol), and these were multifactorial. Given the cross-sectional nature of this survey, it is not possible to comment on causation. However, the data may be used to generate hypotheses regarding targeted strategies to improve diabetes management and outcomes in this population.
Disparities in glycemic control in this population are unlikely to be related to lack of access to care. Those with HbA1c ≥ 10% (86 mmol/mol) reported seeing their family physician and other members of the health care team (allied health practitioners and specialists) more often than those with HbA1c 7–8% (53–64 mmol/mol). However, nearly one quarter of patients with HbA1c ≥ 10% (86 mmol/mol) had not seen an allied health care practitioner for diabetes. Given the evidence for improvement in disease control with the use of interdisciplinary teams [14], this represents a potential opportunity to improve care. Further involvement of care teams may also improve perceived coordination of care [14], which was more commonly reported as suboptimal by patients with poor glycemic control.
Low motivation to improve self-management skills does not seem to be a common barrier for patients with poor or adequate glycemic control. However, only 18% of individuals with HbA1c ≥ 10% (86 mmol/mol) felt they needed more information, which may reflect low confidence in being able to put information into use. Low levels of social support in this group may be a factor, as lack of social support has been linked to low adherence and low self-efficacy [24, 25]. Similarly, depressive symptoms were more common in the HbA1c ≥ 10% (86 mmol/mol) group, and depression has been associated with low adherence to both lifestyle changes and medications [17, 26, 27]. Treatment strategies that aim to increase patient empowerment, and enhance social support via peer support may be useful in addressing these barriers. Specifically, personalized care planning has been shown to improve self-care and lead to improvements in glycemic control [28].
We found that patients with HbA1c ≥ 10% (86 mmol/mol) were more likely to report financial barriers, including not having drug insurance, not getting needed treatments because of cost, and not being able to afford a healthy diet. These results align with studies from other jurisdictions noting an association between cost and glycemic control [17, 29, 30]. Financial barriers increase the risk of non-adherence and are associated with higher utilization of acute care services among chronic disease patients [18, 31]. Our finding may be due to the fact that patients with HbA1c ≥ 10% (86 mmol/mol) were more likely to be under 65 years than those with HbA1c 7–8% (53–64 mmol/mol); financial barriers to obtaining requisite treatments were less common in patients over 65 years, which is the age at which Alberta residents receive universal medication insurance. Access to affordable, healthy food is essential for diabetes self-management and individuals with food insecurity are limited in their ability to prepare appropriate foods and maintain adequate meal spacing [32]. Food insecurity and medication non-adherence often coexist [33, 34]. Increasing access to universal medication insurance and nutritional assistance programs are potential strategies for overcoming financial barriers [34, 35]. Patient navigator programs, in which trained personnel assist patients in accessing available resources, are another potential approach to mitigating financial barriers to care [36, 37].
Our study has several strengths, including large sample size, comparison of responses between HbA1c groups, breadth of the survey questions, and excellent response rate. Some limitations are also worth considering. First, our inclusion criteria may have led to underrepresentation of certain ethnic groups due to language restrictions, and limited our ability to reach vulnerable patients who are not regularly accessing care and are less likely to get routine blood work done. Second, patient responses may reflect the specific resources and services available in the region, and potentially limit the generalizability of our findings. Third, we did not capture data for some lifestyle elements (e.g., sleep, description of employment, physical activity and leisure activities) that may influence diabetes self-care. Finally, the cross-sectional nature of the survey prevents us from drawing conclusions regarding causality.
In conclusion, we found that patients with poor glycemic control face multiple barriers to care, and though similar barriers were reported by those with HbA1c 7–8% (53–64 mmol/mol), significantly more individuals with poor glycemic control reported financial barriers. Given the heterogeneity of barriers across individuals, tailored strategies to overcome modifiable barriers, in light of the significant financial burden of diabetes, are urgently needed.
Data Availability
Study data are owned by the authors and held by the Interdisciplinary Chronic Disease Collaboration (ICDC), a research team at the University of Calgary. Data inquiries should be directed to icdc@ucalgary.ca. Data requests would first have to be made to ICDC. If the request is accepted, a joint application would have to made to our ethics board and if granted, the data can be made available to qualified researchers.
Funding Statement
This study was funded by a Canadian Diabetes Association operating grant and by an Alberta Innovates - Health Solutions (AI-HS) team grant to the Interdisciplinary Chronic Disease Collaboration (ICDC). The funders were not involved in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Report from the National Diabetes Surveillance System: Diabetes in Canada, 2009. Public Health Agency of Canada. 2009.
- 2.Diabetes in Canada: Facts and figures from a public health perspective. Public Health Agency of Canada. 2011. [PubMed]
- 3.McBrien KA, Manns BJ, Chui B, Klarenbach SW, Rabi D, Ravani P, et al. Health Care Costs in People With Diabetes and Their Association With Glycemic Control and Kidney Function. Diabetes Care. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141(6):421–31. [DOI] [PubMed] [Google Scholar]
- 5.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manns BJ, Tonelli M, Zhang J, Campbell DJ, Sargious P, Ayyalasomayajula B, et al. Enrolment in primary care networks: impact on outcomes and processes of care for patients with diabetes. CMAJ. 2012;184(2):E144–52. doi: 10.1503/cmaj.110755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McAlister FA, Majumdar SR, Eurich DT, Johnson JA. The effect of specialist care within the first year on subsequent outcomes in 24,232 adults with new-onset diabetes mellitus: population-based cohort study. Qual Saf Health Care. 2007;16(1):6–11. doi: 10.1136/qshc.2006.018648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah BR, Hux JE, Austin PC. Diabetes is not treated as a coronary artery disease risk equivalent. Diabetes Care. 2007;30(2):381–3. doi: 10.2337/dc06-1654 [DOI] [PubMed] [Google Scholar]
- 9.Sirois C, Moisan J, Poirier P, Gregoire JP. Suboptimal use of cardioprotective drugs in newly treated elderly individuals with type 2 diabetes. Diabetes Care. 2007;30(7):1880–2. doi: 10.2337/dc06-2257 [DOI] [PubMed] [Google Scholar]
- 10.Supina AL, Guirguis LM, Majumdar SR, Lewanczuk RZ, Lee TK, Toth EL, et al. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther. 2004;26(4):598–606. [DOI] [PubMed] [Google Scholar]
- 11.Tonelli M, Bohm C, Pandeya S, Gill J, Levin A, Kiberd BA. Cardiac risk factors and the use of cardioprotective medications in patients with chronic renal insufficiency. Am J Kidney Dis. 2001;37(3):484–9. [PubMed] [Google Scholar]
- 12.Tonelli M, Gill J, Pandeya S, Bohm C, Levin A, Kiberd BA. Barriers to blood pressure control and angiotensin enzyme inhibitor use in Canadian patients with chronic renal insufficiency. Nephrol Dial Transplant. 2002;17(8):1426–33. [DOI] [PubMed] [Google Scholar]
- 13.Toth EL, Majumdar SR, Guirguis LM, Lewanczuk RZ, Lee TK, Johnson JA. Compliance with clinical practice guidelines for type 2 diabetes in rural patients: treatment gaps and opportunities for improvement. Pharmacotherapy. 2003;23(5):659–65. [DOI] [PubMed] [Google Scholar]
- 14.Tricco AC, Ivers NM, Grimshaw JM, Moher D, Turner L, Galipeau J, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–61. doi: 10.1016/S0140-6736(12)60480-2 [DOI] [PubMed] [Google Scholar]
- 15.Bohlen K, Scoville E, Shippee ND, May CR, Montori VM. Overwhelmed patients: a videographic analysis of how patients with type 2 diabetes and clinicians articulate and address treatment burden during clinical encounters. Diabetes Care. 2012;35(1):47–9. doi: 10.2337/dc11-1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q. 2001;79(2):281–315. doi: 10.1111/1468-0009.00206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daly JM, Hartz AJ, Xu Y, Levy BT, James PA, Merchant ML, et al. An assessment of attitudes, behaviors, and outcomes of patients with type 2 diabetes. Journal of the American Board of Family Medicine: JABFM. 2009;22(3):280–90. doi: 10.3122/jabfm.2009.03.080114 [DOI] [PubMed] [Google Scholar]
- 18.Campbell DJ, King-Shier K, Hemmelgarn BR, Sanmartin C, Ronksley PE, Weaver RG, et al. Self-reported financial barriers to care among patients with cardiovascular-related chronic conditions. Health reports. 2014;25(5):3–12. [PubMed] [Google Scholar]
- 19.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–6. [DOI] [PubMed] [Google Scholar]
- 20.Bresee LC, Svenson LW, Patten SB. Chapter 10: Diabetes and Mental Health Disorders in Alberta. In: Alberta Diabetes Atlas 2011. Edmonton: Institute of Health Economics; 2011. p. 163–75. [Google Scholar]
- 21.Papelbaum M, Moreira RO, Coutinho W, Kupfer R, Zagury L, Freitas S, et al. Depression, glycemic control and type 2 diabetes. Diabetology & metabolic syndrome. 2011;3(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barriers to Care for People with Chronic Health Conditions (BCPCHC) Survey—Working Paper. Calgary: University of Calgary, 2013. [Google Scholar]
- 23.Aday LA, Cornelius LJ. Designing and Conducting Health Surveys—A Comprehensive Guide. Third edition ed. USA: Jossey-Bass; 2006. [Google Scholar]
- 24.Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care. 2012;35(6):1239–45. doi: 10.2337/dc11-2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosland AM, Heisler M, Choi HJ, Silveira MJ, Piette JD. Family influences on self-management among functionally independent adults with diabetes or heart failure: do family members hinder as much as they help? Chronic illness. 2010;6(1):22–33. doi: 10.1177/1742395309354608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lerman I, Diaz JP, Ibarguengoitia ME, Perez FJ, Villa AR, Velasco ML, et al. Nonadherence to insulin therapy in low-income, type 2 diabetic patients. Endocrine practice: official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2009;15(1):41–6. [DOI] [PubMed] [Google Scholar]
- 27.Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60. [DOI] [PubMed] [Google Scholar]
- 28.Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane database of systematic reviews (Online). 2015;(3):CD010523 doi: 10.1002/14651858.CD010523.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social Determinants of Health, Cost-related Nonadherence, and Cost-reducing Behaviors Among Adults With Diabetes: Findings From the National Health Interview Survey. Med Care. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tamir O, Wainstein J, Abadi-Korek I, Horowitz E, Shemer J. The patient-perceived difficulty in diabetes treatment (PDDT) scale identifies barriers to care. Diabetes/metabolism research and reviews. 2012;28(3):246–51. doi: 10.1002/dmrr.1300 [DOI] [PubMed] [Google Scholar]
- 31.Bailey GR, Barner JC, Weems JK, Leckbee G, Solis R, Montemayor D, et al. Assessing barriers to medication adherence in underserved patients with diabetes in Texas. The Diabetes educator. 2012;38(2):271–9. doi: 10.1177/0145721711436134 [DOI] [PubMed] [Google Scholar]
- 32.Chan J, DeMelo M, Gingras J, Gucciardi E. Challenges of Diabetes Self-Management in Adults Affected by Food Insecurity in a Large Urban Centre of Ontario, Canada. International journal of endocrinology. 2015;2015:903468 doi: 10.1155/2015/903468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heerman WJ, Wallston KA, Osborn CY, Bian A, Schlundt DG, Barto SD, et al. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabetic medicine: a journal of the British Diabetic Association. 2016;33(6):844–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayer VL, McDonough K, Seligman H, Mitra N, Long JA. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Public health nutrition. 2016;19(6):1103–11. doi: 10.1017/S1368980015002323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang KL, Ghali WA, Manns BJ. Addressing cost-related barriers to prescription drug use in Canada. CMAJ. 2014;186(4):276–80. doi: 10.1503/cmaj.121637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Freeman HP. The history, principles, and future of patient navigation: commentary. Seminars in oncology nursing. 2013;29(2):72–5. doi: 10.1016/j.soncn.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 37.Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA: a cancer journal for clinicians. 2011;61(4):237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Study data are owned by the authors and held by the Interdisciplinary Chronic Disease Collaboration (ICDC), a research team at the University of Calgary. Data inquiries should be directed to icdc@ucalgary.ca. Data requests would first have to be made to ICDC. If the request is accepted, a joint application would have to made to our ethics board and if granted, the data can be made available to qualified researchers.