Abstract
The aim of our study was to assess the medium-term clinical outcomes of anterior cruciate ligament (ACL) reconstruction using the Ligament Advanced Reinforcement System (LARS) artificial ligament.
A total of 168 patients who underwent arthroscopic ACL reconstruction with the LARS artificial ligament in our department were enrolled in our research. Only 125 met the inclusion/exclusion criteria, and 91 could ultimately be contacted to participate in our research. The mean follow-up was 92 ± 19 months. Physical examinations and a KT-1000 arthrometer were used to evaluate knee laxity. The International Knee Documentation Committee (IKDC) and Lysholm knee scales were evaluated for knee function. The Tegner score was tested for the condition of return to sport. Range of motion (ROM) and the rates of failure and complications were calculated.
Among all patients enrolled in the study, the failure rate was 4.4%, and the overall complication rate was 2.2%. Knee laxity measured by the KT-1000 arthrometer was 1.4 ± 1.5 mm, compared with the preoperative value of 5.1 ± 1.3 mm. The Lysholm score improved from a preoperative value of 54.6 ± 14.3 to a postoperative value of 85.4 ± 12.1. The proportion of return to sport was 86.8% (79/91). The postoperative Tegner score was 4.7 ± 1.3, while its value before injury was 5.5 ± 1.0.
In this study, ACL reconstruction using the LARS artificial ligament has a good prognosis with a low failure and complication rate at a mean follow-up of 91 months.
Keywords: ACL reconstruction, arthroscopy, artificial ligament, LARS
1. Introduction
Anterior cruciate ligament (ACL) injury is a primary cause of knee instability and is associated with secondary damages to the intra- and peri-articular structures of the knee, which may result in articular degeneration.[1] ACL reconstruction is a well-established and acknowledged surgical technique for ACL injury and is currently being applied worldwide.[2]
The graft options for ACL include three main types: autograft, allograft, and synthetic graft. Compared to autograft and allograft, using a synthetic graft can effectively avoid risks of donor site morbidity and disease transmission but can cause higher rates of graft failure and late inflammation.[3,4] Historically, in the late 1980s and early 1990s, synthetic ACL reconstruction was considered suspect, especially due to the Gortex experience with its high ratio of long-term complications, although the short-term clinical results were appealing.[5,6] Tearing of the prosthetic ligament was the most feared and frequent complication.[7,8]
With the development of biomechanics and material science, a novel synthetic ACL graft called the Ligament Advanced Reinforcement System (LARS; Surgical Implants and Devices, Arc-sur-Tille, France) was developed. After decades of discussions and arguments, the use of LARS remains a controversial issue. In 2013, Parchi et al[9] did not record any cases of infections or knee synovitis and only one case of mechanical graft failure. In 2015, a study indicated that LARS should currently not be suggested as a potential graft for primary reconstruction of the ACL based on a minimum 10-year follow-up of 18 patients.[10] An editorial commentary stated that LARS may not be perfect, but LARS clinical outcomes are surprisingly impressive.[11]
The purpose of our study was to evaluate the medium-term clinical outcome of ACL reconstruction with LARS at a single institution from 2004 to 2010. It was hypothesized that using the LARS artificial ligament for ACL reconstruction was effective and safe, with a low failure rate and low incidence of complications.
2. Materials and methods
2.1. Patients and data collection
This work was an observational case series study and was conducted in the orthopedics department of Changhai Hospital from February 2016 to August 2016. This study was conducted under the medical Ethics Committee of Changhai Hospital Affiliated to Second Military Medical University (Permit Number: 2016-008). All participants in this study signed informed consent forms to publish the related data.
From January 2004 to January 2011, 168 patients underwent arthroscopic ACL reconstruction using the LARS artificial ligament in our hospital. ACL rupture was diagnosed based on medical history, physical examination, and MRI examination. All patients were actively engaged in daily work and sports activity before injury. All of them were informed of the benefits and risks of ACL reconstruction with the LARS artificial ligament, and informed consent was signed before the surgery.
The inclusion criteria were as follows: (1) date of surgery: 2004/1/1-2010/12/30, (2) ACL reconstruction using the LARS system, (3) chondral lesions ≤ Grade 2 (Outerbridge Classification), (4) knee osteoarthritis < Grade III (Kellgren-Lawrence Grading Scale). The exclusion criteria were as follows: (1) revision ACL reconstruction, (2) multiple ligament injuries (medial collateral ligament injury without operation excluded), (3) operation history of knee, (4) trauma history for the contralateral side of the knee. ACL failure is defined as either ACL graft re-rupture diagnosis by MRI or a pivot shift test greater than grade 2, KT-1000 side-to-side difference of >5 mm and extension >5 and flexion deficit >15° according to the contralateral side. Complications included infection, synovitis, failure of fixation, and articular stiffness.
Physical examinations including the Lachman test, Pivot-shift test, and KT-1000 arthrometer measurement (MEDmetric, San Diego, CA) were performed to evaluate knee laxity. Participants were asked to fill in two self-assessment instruments, the International Knee Documentation Committee (IKDC), and the Lysholm knee score. The Tegner score was calculated for the level of return to sport, and the reasons patients could not return to sport were collected. The range of motion (ROM) was measured during follow-ups. Demographic data were also collected, including age, gender, affected side, BMI, duration of follow-up, cause of injury, and time from injury to operation. In order to reduce the effects of patients lost to follow-up, demographic data were compared between follow-up patients and patients lost to follow-up.
2.2. Operative procedure
Routine arthroscopy was performed on all patients, and any meniscal injuries and/or cartilaginous lesions were treated before ACL reconstruction.
ACL reconstruction with LARS was undertaken following isometric surgical principles, which have been previously described.[13] The ACL stumps were routinely preserved. The intra-articular point of the tibial tunnel was positioned at the anteromedial part of the tibial footprint of the ACL from the anteromedial tibial cortex by a tibial aimer with a Kirschner wire inserted. Then, the tibial tunnel was drilled using a 7.5 mm diameter drill bit. The intra-articular femoral tunnel was placed by the transtibial technique at the 11:00-o’clock position (right)/1:00-o’clock position (left). The 7.5 mm diameter drill bit guided by the Kirschner wire was drilled into the femur from the anterolateral thigh into the knee joint. The LARS artificial ligament was introduced into the knee joint from the extra-articular opening of the tibial tunnel, guided by a wire. It was ensured that the full range of knee motion was achieved and there was no impingement among LARS artificial ligaments, the notch, and the PCL. Titanium interference-fit screws (Surgical Implants and Devices) were used for fixation of the LARS artificial ligament at both the tibial and femoral sides with a diameter of 8 mm on the femoral side and 9 mm on the tibial side at a knee flexion of 30° (Fig. 1).
Figure 1.
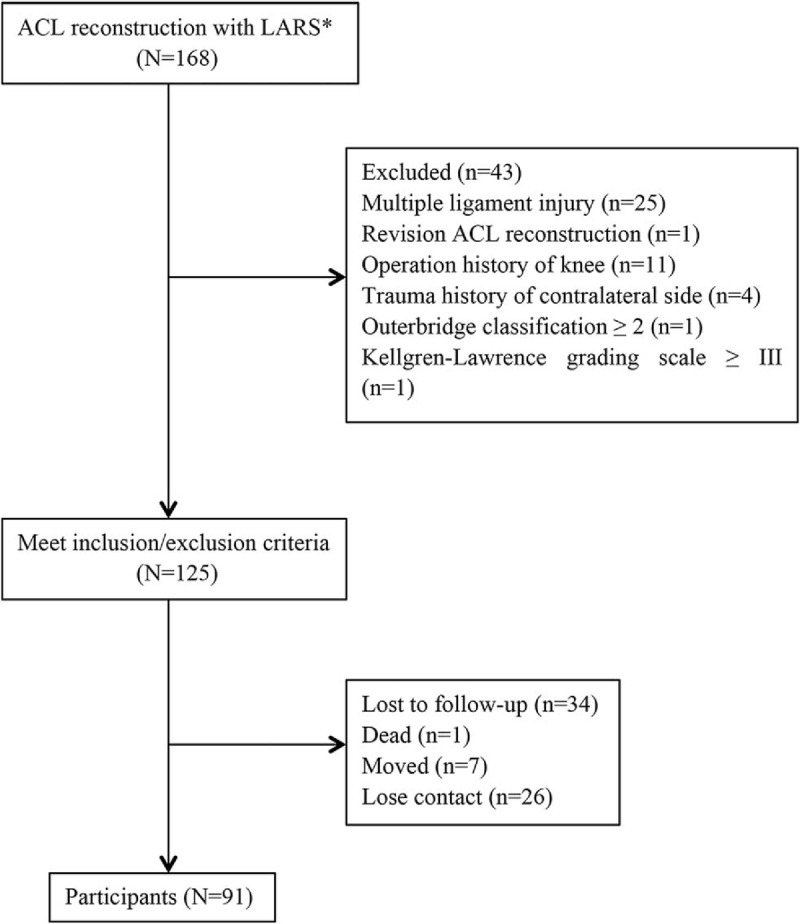
Consort flow diagram of study. ∗LARS = ligament advanced reinforcement system.
2.3. Rehabilitation
Unlocked functional braces were used for 24 hours in the first 2 weeks after operation and only used during walking between 2 and 4 weeks after surgery. To strengthen the quadriceps, leg-raising exercises with the brace at least 200 times a day were recommended beginning as soon as possible after surgery. A ROM of 45° could be achieved within 2 weeks after the operation and 120° within 8 weeks. Walking without crutches was allowed beginning at least 4 weeks after surgery.
2.4. Statistical analysis
Continuous data with normal distribution were expressed as the mean and standard deviation, and continuous data with non-normal distribution or noncontinuous data were expressed as the median with ranges given. For statistical analyses, the Chi-squared test was used for categorical variables, and Student's t-test was used for continuous variables with normal distribution. A P value of less than 0.05 was considered statistically significant for all analyses. The analyses were performed in SSPS for Windows Release 20.0 (Chicago, IL).
3. Results
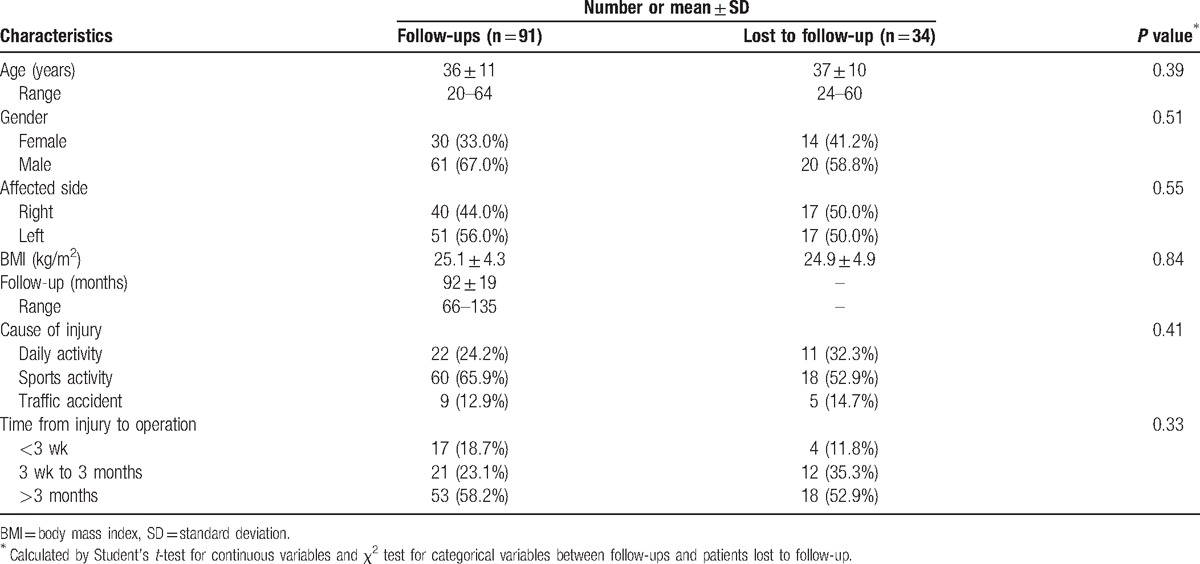
Of all 168 patients, 125 satisfied the inclusion/exclusion criteria, and 34 were lost to follow-up (Fig. 2). Hence, the follow-up rate was 72.8%. A total of 91 patients were eventually enrolled in our research, including 61 males (67.0%) and 30 females (33.0%) (Table 1). The average age was 36 ± 11 years (range, 20–64 years), and the mean duration of follow-up was 92 ± 19 months (range, 66–135 months). The median duration between injury and surgery was 19 weeks (range, 1–1260). Of all patients included, 50 patients (54.9%) suffered from an ACL injury accompanied by meniscus injury. The demographic baseline between follow-ups and patients lost to follow-up showed no significant difference (P > 0.05).
Figure 2.

Postoperative radiograph of ACL reconstruction using LARS artificial ligament. ACL = anterior cruciate ligament, LARS = Ligament advanced reinforcement system.
Table 1.
Demographic and clinical characteristics of participants.
At the final follow-up, the failure rate of ACL reconstruction using the LARS artificial ligament was 4.4% (4/91). One patient had limited ROM, where the flexion angle of the affected knee was 30° smaller than on the normal side, and one was diagnosed with mechanical graft failure during revision surgery (Fig. 3). Two patients had a side-to-side difference of more than 5 mm. The complication rate was 2.2% (2/91). One patient suffered from a superficial surgical site infection and was cured by antibiotics 7 months after surgery. Screw loosening occurred in another patient due to osteoporosis with replacement by a larger screw 4 months later.
Figure 3.
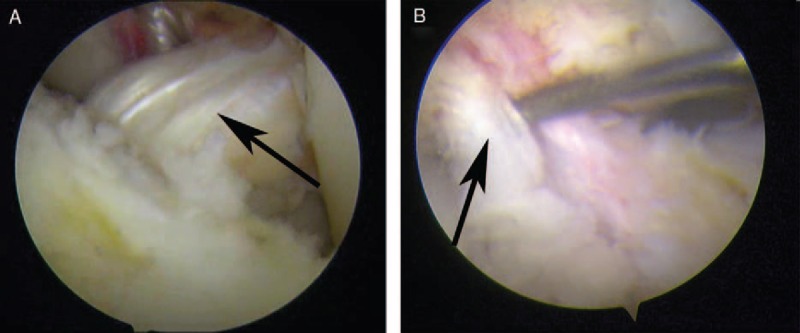
Arthroscopic images of intact and ruptured artificial ligament. (A) intact artificial ligament (black arrow). (B) Ruptured artificial ligament (black arrow).
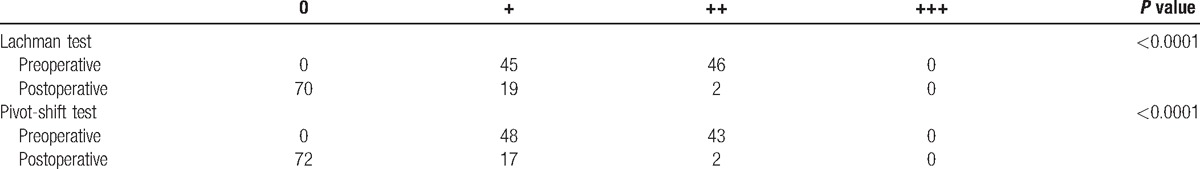
The side-to-side difference in knee laxity measured by a KT-1000 arthrometer was 1.4 ± 1.5 mm (range, 0–4 mm), which was significantly decreased compared with the preoperative value of 5.1 ± 1.3 (range, 4–10 mm) (P< 0.0001). Postoperatively, only 2 patients (2.2%) had a side-to-side difference of more than 5 mm. The results of the Lachman test and pivot-shift test are given in Table 2. Only one patient had obvious ROM limitation compared with the contralateral side.
Table 2.
Preoperative and postoperative physical examination.
The mean Lysholm score improved from 54.6 ± 14.3 (range, 20–90) to 85.4 ± 12.1 (range, 20–100) (P < 0.0001). According to the IKDC score standard, 63 cases were classified as grade C preoperatively, while 28 cases were classified as grade D preoperatively. The final evaluation of IKDC showed 58 cases of grade A, 24 cases of grade B, 6 cases of grade C, and 3 cases of grade D. Compared to the preoperative results, the postoperative IKDC results increased significantly (P < 0.0001). Of all patients enrolled in our research, 12 cases did not return to sports (13.2%). Five cases were mainly due to poor knee function, and five cases were predominantly for psychological reasons. The other 2 cases were influenced by social and economic factors. The mean Tegner score was 4.7 ± 1.3 postoperatively and 5.5 ± 1.0 before injury (P < 0.0001).
4. Discussion
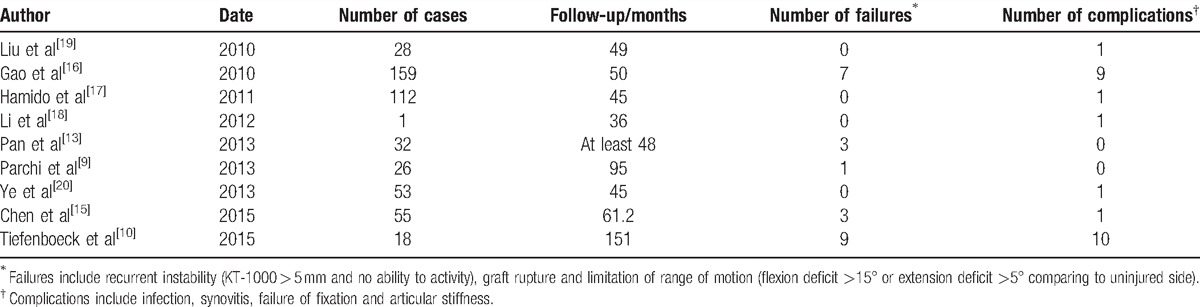
The most importing findings of this study were the low failure rate and the low complication rate. The failure rate was 4.4% (4/91), including two cases of recurrent instability, one case of limitation of ROM and one artificial graft rupture. According to a review of the recent literature, the failure rate was 4.75% (23/484) in all studies where the mean follow-up was longer than 3 years (Table 3).[9,10,12,14–19] There were 9 cases of graft rupture and 14 cases of recurrent instability. Among these 9 cases, 6 were due to a new trauma, and 1 case was injury in a high-level sport activity. One patient who suffered artificial graft rupture in our research was a judoka and returned to judo training. He was re-injured in daily training. Hence, the possibility of graft rupture without new injuries was comparatively low. Pan et al[12] reported similarly good clinical results after ACL reconstruction using bone-patellar tendon-bone (BPTB) autografts or LARS artificial grafts at a midterm follow-up. The rate of recurrent instability was 9.38% (3/32) for LARS and 6.67% (2/30) for BPTB autografts. Dericks reported that the failure rate was 4% in 220 cases receiving ACL reconstruction with the LARS artificial ligament after a mean follow-up of 2.5 years, which was similar to our results.[13] Since the graft was located in a nonanatomic and isometric placement, the tensional force in vivo was less, and the graft survival was higher than for an anatomically reconstructed graft.
Table 3.
Review of ACL reconstruction with LARS ligament.
The overall complication rate in our research was 2.2% (2/91), with one case of screw loosening and one case of infection. No synovitis occurred in our study, and synovitis appears to be a rare complication closely related to imperfect graft positioning.[20] However, when the complication of synovitis does occur, it can be very severe. Li et al[17] reported a case of rare serious knee synovitis 3 years postoperatively, possibly due to poor remodelling of the artificial ligament. Bone impingement caused by malposition of the bone tunnel has often been a primary reason for failure and complications.[21] Infection and screw loosening/pain related to screws were most frequently reported.[10,15] Based on observation of the histological characteristics and ultrastructure of the LARS ligament in vitro, inflammation and foreign body reaction were enhanced, but the LARS ligament had good in-growth capability based on the findings of fibrous connective tissue formation.[22] Although the complication rate was not high, methods to promote the biocompatibility of the LARS artificial ligament needed further study.
The LARS artificial ligament was initially invented by JP Laboureau and made of polyethylene terephthalate (PET). It was a “scaffold” graft but has not yet been Food and Drug Administration (FDA) approved in the United States, and its use for the most part has occurred in France and Australia. LARS can be divided into two parts: the intra-articular portion and the extra-articular portion. The intra-articular portion consists of longitudinal external rotation fibers with no transverse fibres, in imitation of the ACL anatomical structure, while the extra-articular portion is woven of longitudinal and transverse fibers to avoid ligament deformation. LARS has good biomechanics in terms of resisting tension, flexion, and torsion load.[23,24]
Knee functions were evaluated by assessing the IKDC score and the Lysholm knee score. The Tegner score was tested for the ability to return to sport. Similar to previous studies, the IKDC score and the Lysholm score both increased significantly.[9,15,16] It indicated a good recovery of knee function. However, the Tegner score showed a significant difference between the pre-injury and postoperative periods. There was no case in which the postoperative level of activity was higher than pre-injury, and only 46 cases could return to the pre-injury level of activity. Moreover, 12 cases could not return or refused to engage in sport activities. The reasons for the decrease in the Tegner score included multiple factors. After detailed inquiries, psychological factors played an important role, as most of them feared another injury. Only 5 cases could not return to sport activity due to knee dysfunction. Another reason some refused to return to sport activity was social and economic factors, as they complained of being busy with work and having limited time. Eleven patients were students before the injury and had since taken a job, so they gave up playing football or basketball for personal reasons.
Compared to previous research, the short-term results were appealing, but the long-term follow-up results were controversial. Tiefenboeck et al indicated that the LARS artificial ligament should not be suggested as a potential graft for primary ACL reconstruction based on research at a minimum follow-up of 10 years. However, this research might not accurately represent the long-term results of the LARS ligament because the sample size was small (n = 18).[10] The same problem was present in another study at a mean follow-up of 8 years (n = 29), but this study documented a good result for the LARS ligament.[9] To ensure the follow-up time as well as the sample size, patients who accepted ACL reconstruction over at least 7 years in our hospital were enrolled in our research. The results tended to support LARS ligaments for primary ACL reconstruction.
There were two limitations in our study. First, the follow-up rate was comparatively low due to changes in contact information and geographical factors. However, the demographic data between follow-ups and patients lost to follow-up showed no significant difference, which indicated good representativeness of the follow-up data. Second, no control group was evaluated because there were not enough cases of other surgical methods for long-term evaluation.
5. Conclusions
In this research, ACL reconstruction using the LARS artificial ligament has a good prognosis with a low failure rate and complication rate for at least 7 years. It can serve as a suitable choice for fast recovery of the anterior cruciate ligament.
Acknowledgments
We are grateful for the cooperation of all the volunteer participants and the staff working in the patient centre and inpatient departments.
Footnotes
Abbreviations: ACL = anterior cruciate ligament, BPTB = one-patellar tendon-bone, FDA = Food and Drug Administration, IKDC = the International Knee Documentation Committee, LARS = the Ligament Advanced Reinforcement System, PET = polyethylene terephthalate, ROM = range of motion.
JZ, XC, and WW designed the study, analyzed the data and wrote the manuscript; all authors followed up the patients and collected the information; J.Z, XC, WW, HX, and XW are responsible for the follow-ups of the LARS artificial graft.
Z-YJ, C-CX, and WW are co-first authors; they contributed equally to the work.
XH WX are co-corresponding authors.
Disclosure: There are no financial or personal relationships with other people or organizations that could potentially inappropriately influence (bias) our work and conclusions.
Funding: Scholar Fund of Second Military Medical University (2016JS24); Tengfei Project (16T016); Zonghe Project (2016JS24).
Level of confidence: Level IV, case series with no comparison groups.
The authors have no conflict of interest to disclose.
References
- [1].Nyland J, Mattocks A, Kibbe S, et al. Anterior cruciate ligament reconstruction, rehabilitation, and return to play: 2015 update. Open Access J Sports Med 2016;7:21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vaishya R, Agarwal AK, Ingole S, et al. Current trends in anterior cruciate ligament reconstruction: a review. Cureus 2015;7:e378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mascarenhas R, MacDonald PB. Anterior cruciate ligament reconstruction: a look at prosthetics—past, present and possible future. Mcgill J Med 2008;11:29–37. [PMC free article] [PubMed] [Google Scholar]
- [4].Shaerf DA, Pastides PS, Sarraf KM, et al. Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop 2014;5:23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rushton N, Dandy DJ, Naylor CP. The clinical, arthroscopic and histological findings after replacement of the anterior cruciate ligament with carbon-fibre. J Bone Joint Surg Br 1983;65:308–9. [DOI] [PubMed] [Google Scholar]
- [6].Ventura A, Terzaghi C, Legnani C, et al. Synthetic grafts for anterior cruciate ligament rupture: 19-year outcome study. Knee 2010;17:108–13. [DOI] [PubMed] [Google Scholar]
- [7].Savarese A, Lunghi E, Budassi P, et al. Remarks on the complications following ACL reconstruction using synthetic ligaments. Ital J Orthop Traumatol 1993;19:79–86. [PubMed] [Google Scholar]
- [8].Drogset JO, Grontvedt T, Robak OR, et al. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am 2006;88:944–52. [DOI] [PubMed] [Google Scholar]
- [9].Parchi PD, Gianluca C, Dolfi L, et al. Anterior cruciate ligament reconstruction with LARS artificial ligament results at a mean follow-up of eight years. Int Orthop 2013;37:1567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tiefenboeck TM, Thurmaier E, Tiefenboeck MM, et al. Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS system at a minimum follow-up of 10years. Knee 2015;22:565–8. [DOI] [PubMed] [Google Scholar]
- [11].Lubowitz JH. Editorial commentary: synthetic ACL grafts are more important than clinical nonbelievers may realize. Arthroscopy 2015;31:969–70. [DOI] [PubMed] [Google Scholar]
- [12].Pan X, Wen H, Wang L, et al. Bone-patellar tendon-bone autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Eur J Orthop Surg Traumatol 2013;23:819–23. [DOI] [PubMed] [Google Scholar]
- [13].Dericks G. Ligament advanced reinforcement system anterior cruciate ligament reconstruction. Oper Tech Sports Med 1995;3:187–205. [Google Scholar]
- [14].Chen J, Gu A, Jiang H, et al. A comparison of acute and chronic anterior cruciate ligament reconstruction using LARS artificial ligaments: a randomized prospective study with a 5-year follow-up. Arch Orthop Trauma Surg 2015;135:95–102. [DOI] [PubMed] [Google Scholar]
- [15].Gao K, Chen S, Wang L, et al. Anterior cruciate ligament reconstruction with LARS artificial ligament: a multicenter study with 3- to 5-year follow-up. Arthroscopy 2010;26:515–23. [DOI] [PubMed] [Google Scholar]
- [16].Hamido F, Misfer AK, Al Harran H, et al. The use of the LARS artificial ligament to augment a short or undersized ACL hamstrings tendon graft. Knee 2011;18:373–8. [DOI] [PubMed] [Google Scholar]
- [17].Li H, Yao Z, Jiang J, et al. Biologic failure of a ligament advanced reinforcement system artificial ligament in anterior cruciate ligament reconstruction: a report of serious knee synovitis. Arthroscopy 2012;28:583–6. [DOI] [PubMed] [Google Scholar]
- [18].Liu ZT, Zhang XL, Jiang Y, et al. Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int Orthop 2010;34:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ye JX, Shen GS, Zhou HB, et al. Arthroscopic reconstruction of the anterior cruciate ligament with the LARS artificial ligament: thirty-six to fifty-two months follow-up study. Eur Rev Med Pharmacol Sci 2013;17:1438–46. [PubMed] [Google Scholar]
- [20].Razi M, Salehi S, Dadgostar H, et al. Timing of anterior cruciate ligament reconstruction and incidence of meniscal and chondral injury within the knee. Int J Prev Med 2013;4(suppl 1):S98–103. [PMC free article] [PubMed] [Google Scholar]
- [21].Amis AA, Kempson SA. Failure mechanisms of polyester fiber anterior cruciate ligament implants: a human retrieval and laboratory study. J Biomed Mater Res 1999;48:534–9. [DOI] [PubMed] [Google Scholar]
- [22].Yu SB, Yang RH, Zuo ZN, et al. Histological characteristics and ultrastructure of polyethylene terephthalate LARS ligament after the reconstruction of anterior cruciate ligament in rabbits. Int J Clin Exp Med 2014;7:2511–8. [PMC free article] [PubMed] [Google Scholar]
- [23].Hagemeister N, Duval N, Yahia L, et al. Comparison of two methods for reconstruction of the posterior cruciate ligament using a computer based method: quantitative evaluation of laxity, three-dimensional kinematics and ligament deformation measurement in cadaver knees. Knee 2002;9:291–9. [DOI] [PubMed] [Google Scholar]
- [24].Viateau V, Manassero M, Anagnostou F, et al. Biological and biomechanical evaluation of the ligament advanced reinforcement system (LARS AC) in a sheep model of anterior cruciate ligament replacement: a 3-month and 12-month study. Arthroscopy 2013;29:1079–88. [DOI] [PubMed] [Google Scholar]


