Dear Sir,
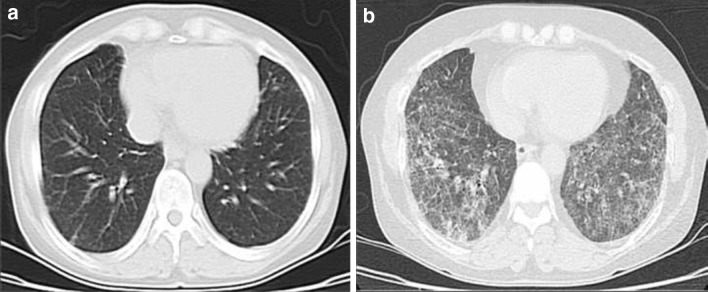
A 52-year-old woman was admitted to our hospital with persistent fatigue and pretibial edema. Serum creatinine was 2.7 mg/dL, and urine analysis revealed hematuria and pyuria. Proteinuria was 3 g/day. Tests for anti-neutrophil cytoplasmic antibody (ANCA) and anti-glomerular basement membrane antibody were negative. Based on renal biopsy, ANCA-negative pauci-immune crescentic glomerulonephritis was diagnosed. No abnormal findings were apparent on the baseline thorax computed tomography (CT) image (Fig. 1a). The patient was started on a pulse methylprednisolone regimen (1 g/day for 3 days) followed by 750 mg cyclophosphamide (CPA) per month. Following the pulse treatments, 1 mg/kg prednisolone was continued for an additional month, with tapering of the steriod dose by 4 mg/week. The maintenance dose of methyprednisolone was 4 mg/day. After the third dose of CPA, patient complained of exertional dyspnea and cough. The serum creatinine level and urinalysis results were normal. However, a second thorax CT showed the presence of a reticular interstitial infiltration with a honey-comb appearance (Fig. 1b). As the concomitant use of certain drugs is able to induce interstitial lung disease, we investigated this possibility but found no suspicious drug history. Infectious etiologies as possible causes of the clinical picture were also considered and subsequently excluded. The diagnosis of CPA-induced early-onset interstitial lung disease was established on clinical and radiological grounds. The CPA was withdrawn from the therapeutic regimen, and treatment with 1 mg/kg prednisolone was started. At follow-up, the dyspnea and cough had disappeared. Baseline and follow-up serum C-reactive protein levels after the treatment were 11.2 and 1.1 mg/dL, respectively.
Fig. 1.
a Baseline thorax computed tomography image before the cyclophosphamide treatment. b Reticular interstitial infiltration with honey-comb appearance after the treatment
The presence of dyspnea and an interstitial pattern in a patient receiving CPA treatment suggests that a possible CPA-induced lung toxicity should be considered [1]. Prompt discontinuation of CPA and treatment with corticosteroids is usually followed by clinical recovery [2]. CPA-induced interstitial lung disease in patients with renal disease is a rare entity. Pulmonary toxicity of this drug is most commonly encountered in oncology patients. However, there have been several reports of an association between CPA treatment and various renal diseases, such as nephrotic syndrome and membranous glomerulonephritis [3, 4].
References
- 1.Hamada K, Nagai S, Kitaichi M, Jin G, Shigematsu M, Nagao T, et al. Cyclophosphamide-induced late-onset lung disease. Intern Med. 2003;42(1):82–87. doi: 10.2169/internalmedicine.42.82. [DOI] [PubMed] [Google Scholar]
- 2.Segura A, Yuste A, Cercos A, López-Tendero P, Gironés R, Pérez-Fidalgo JA, et al. Pulmonary fibrosis induced by cyclophosphamide. Ann Pharmacother. 2001;35(7–8):894–897. doi: 10.1345/aph.10297. [DOI] [PubMed] [Google Scholar]
- 3.Harigaya H, Matsubara K, Nigami H, Baba K. Interstitial pneumonitis probably induced by cyclophosphamide in nephrosis. Acta Paediatr Jpn. 1997;39(3):364–367. doi: 10.1111/j.1442-200X.1997.tb03755.x. [DOI] [PubMed] [Google Scholar]
- 4.Yamada H, Fujimoto T, Ishii Y, Matsuda S. A case of nephrotic syndrome associated with severe interstitial pneumonitis due to cyclophosphamide whose life was saved by steroid pulse therapy. Nihon Jinzo Gakkai Shi. 1995;37(9):518–522. [PubMed] [Google Scholar]