Abstract
Offering a choice of influenza vaccine type may increase vaccine coverage and reduce disease burden, but it is more costly. This study calculated the public health impact and cost-effectiveness of 4 strategies: no choice, pediatric choice, adult choice, or choice for both age groups. Using agent-based modeling, individuals were simulated as they interacted with others, and influenza was tracked as it spread through a population in Washington, DC. Influenza vaccination coverage derived from data from the Centers for Disease Control and Prevention was increased by 6.5% (range, 3.25%–11.25%), reflecting changes due to vaccine choice. With moderate influenza infectivity, the number of cases averaged 1,117,285 for no choice, 1,083,126 for pediatric choice, 1,009,026 for adult choice, and 975,818 for choice for both age groups. Averted cases increased with increased coverage and were highest for the choice-for-both-age-groups strategy; adult choice also reduced cases in children. In cost-effectiveness analysis, choice for both age groups was dominant when choice increased vaccine coverage by ≥3.25%. Offering a choice of influenza vaccines, with reasonable resultant increases in coverage, decreased influenza cases by >100,000 with a favorable cost-effectiveness profile. Clinical trials testing the predictions made based on these simulation results and deliberation of policies and procedures to facilitate choice should be considered.
Keywords: agent-based modeling, cost-effectiveness, influenza, influenza vaccine, vaccine choice
Influenza causes 3,000 to 49,000 (mean = 23,607) deaths in the United States every year (1). In addition, approximately 226,000 primary influenza-related hospitalizations occur annually in the United States, climbing to more than 400,000 in some epidemics (2). Annual vaccination is the primary means to prevent influenza, but uptake remains below national goals for universal coverage (https://www.cdc.gov/flu/fluvaxview/). Several vaccine options are available to meet the recommended annual vaccination of all persons older than 6 months, including live attenuated influenza vaccine (LAIV) and inactivated influenza vaccine (IIV) in quadrivalent, trivalent, and high-dose forms (3). Delivery routes include intramuscular (IM), intradermal (ID), and intranasal (i.e., LAIV). Allowing individuals to choose the influenza vaccine they receive increased immunization coverage in a randomized trial (4). Many children and adults prefer a particular vaccine type or administration route (5–9), but differing recommended vaccines among age groups and differing contraindications for individual vaccines complicate the choice landscape. Moreover, providing choice options for influenza vaccine may lead to increased costs. A discussion by providers with patients about those options takes more time than simply offering a single type. With choice, vaccine-related ordering, stocking, tracking, and reporting are more complex, and additional costs are incurred when multiple vaccine types are used in a given practice setting. Currently, IIV is the least expensive option, whereas high-dose IIV and LAIV are more expensive (10).
A key research question is whether gains in influenza vaccination coverage and the subsequent potential reduction in influenza disease burden that vaccine choice may provide are offset by the potential increased costs of offering that choice. Answering this question is a complex process, because such a cost-effectiveness (CE) analysis requires: 1) simulating the complex and dynamic spread of influenza in scenarios that vary vaccination coverage levels; 2) accounting for choice of vaccine types and their contraindications; and 3) accounting for vaccine-induced herd immunity.
This study estimates the public health impact and CE of offering a choice of vaccines based on the simulated spread of influenza through spatially and temporally heterogeneous interactions among individuals in a synthetic population representing the Washington, DC–5-county metropolitan region.
METHODS
This study comprised 2 steps. First, a previously published agent-based model (ABM) (11–14) was used to predict epidemiologic outcomes in the DC metropolitan population during a single influenza season under various vaccine choice options. Second, using those results, CE was analyzed from a societal perspective. This study did not require IRB approval because it did not involve human subjects, and only secondary, anonymous data were used for model parameterization.
ABM of the DC metropolitan area synthetic population
Using a version of the Framework for Reconstructing Epidemic Dynamics (FRED) (15) ABM, which was modified to enable fine-grained control of age-specific vaccine coverage, simulations were conducted for the DC metropolitan statistical area using a synthetic population of the combined areas of Baltimore-Towson, Maryland; Washington-Arlington-Alexandria, DC–Virginia–Maryland–West Virginia; Winchester, Virginia–West Virginia; Lexington Park, Maryland; and Culpeper, Virginia, based on US Census 2010 (16). The model contained 7,858,207 virtual people (i.e., “agents”), who were assigned to households that represented the geospatial population density and demographics at the census tract level.
Each agent was assigned to a household and to age-appropriate outside locations: school-aged children to schools and working adults to a workplace. On each weekday, agents start in their households, coming into contact with other household members. Then, children leave for school and adults for work, coming in contact with others at those locations. Finally, they mix in their neighborhoods and their communities in the evening. On weekends, mixing occurs primarily in households and neighborhoods, with only 20% of adults working (17).
Influenza transmission
On a given day, each agent may be in one of 4 influenza disease states: susceptible, exposed, infectious, or recovered. The influenza epidemic was simulated by randomly selecting 100 agents and assigning them to the infectious state, a process referred to as “seeding.” These infected agents encounter susceptible agents as they visit their households, schools, and workplaces. When exposed, an agent moves from the susceptible state to the exposed state for a latent period drawn from a distribution with a mean of 1.9 days. At the conclusion of the latent period, the agent moves to the infectious state for an infectious period drawn from a distribution with a mean of 4.1 days. When an agent in the infectious state comes in contact with agents in the susceptible state, influenza may be transmitted, in which case any newly infected agent moves to the exposed state. One-third (33%) of the agents who enter the infectious state are asymptomatic and are 50% less infectious than a symptomatic agent (18, 19). Half (50%) of all symptomatic agents stay home from school or work, thus limiting contact with others who may be in the susceptible state. These parameters and assumptions are consistent with previously published ABM studies (17, 20–25).
The transmission of influenza in the model was calibrated according to the procedure described in Grefenstette et al. (15). Parameters for the ABM transmission model are summarized in Table 1. The transmissibility of the influenza epidemic was set by attack rates which were translated to the basic reproduction number (R0), as described by Grefenstette et al. (15). Transmissibility in the base case, named “moderate infectivity,” matched as closely as possible the age-specific attack rates published in Molinari et al. (26) and translated to an R0 of 1.3. In sensitivity analyses, transmissibility was varied from R0 = 1.0 (mild infectivity) to R0 = 1.6 (high infectivity). Because of the large population size and spatially and temporally heterogeneous nature of an ABM, small outbreaks can occur even with an R0 = 1.0.
Table 1.
Key Parameters Used in the Agent-Based Model of a Synthetic Population
| Parameter | % | Vaccine Received, % | No. | Range | Reference No. | ||||
|---|---|---|---|---|---|---|---|---|---|
| LAIV | IIV-IM | IIV-ID | IIV-HD | Minimum | Maximum | ||||
| Coverage by age, years | |||||||||
| 6–23 months | 70.4 | 0.0 | 100.0 | 0.0 | 0.0 | 69.6 | 71.2 | Adapted from (38, 39) | |
| 2–4 | 68.1 | 52.0 | 48.0 | 0.0 | 0.0 | 67.3 | 68.9 | ||
| 5–8 | 61.0 | 52.0 | 48.0 | 0.0 | 0.0 | 60.2 | 61.8 | ||
| 9–17 | 52.9 | 52.0 | 48.0 | 0.0 | 0.0 | 52.1 | 53.7 | ||
| 18–49 | 32.3 | 2.0 | 97.0 | 1.0 | 0.0 | 31.9 | 32.7 | ||
| 50–64 | 45.3 | 0.0 | 99.0 | 1.0 | 0.0 | 44.9 | 45.7 | ||
| 65–106 | 65.0 | 0.0 | 67.0 | 0.0 | 33.0 | 64.6 | 65.4 | ||
| LAIV contraindications by age, years | |||||||||
| 2–4 | 8.8 | (40) | |||||||
| 5–17 | 1.0 | ||||||||
| Absolute vaccine coverage increases with choice | 6.5 | 3.25 | 11.25 | (3) | |||||
| Vaccine cost, dollars | |||||||||
| IIV-IM | 10.69 | 0.00 | 21.38 | (9) | |||||
| LAIV | 23.70 | 0.00 | 47.40 | ||||||
| IIV-ID | 15.69 | 0.00 | 31.38 | ||||||
| IIV-HD | 23.69 | 0.00 | 47.38 | (41) | |||||
| Vaccine administration cost, dollars | 25.08 | (28) | |||||||
| Increased cost of choice | 5.0 | 2.5 | 7.5 | (42) | |||||
| Latent period, days | 1.9 | 1 | 2 | (17, 20–25, 43) | |||||
| Infectious period, days | 4.1 | 3 | 6 | ||||||
| Asymptomatic rate | 33.0 | ||||||||
| Asymptomatic reduction in infectivity | 50.0 | ||||||||
| Symptomatic absenteeism | 50.0 | ||||||||
| Vaccine effectiveness | 59.0 | (44) | |||||||
Abbreviations: HD, high dose; ID, intradermal; IIV, inactivated influenza vaccine; IM, intramuscular; LAIV, live attenuated influenza vaccine.
Vaccine effectiveness and choice
In the ABM, each vaccine had an age-specific vaccine effectiveness that was defined as the probability of that vaccine producing full and permanent immunity against influenza. That is, 14 days after receiving an influenza vaccine, an agent will have a probability of becoming immune equal to the vaccine effectiveness and a probability of remaining susceptible equal to 1 minus the vaccine effectiveness. Because this study modeled only a single season, waning immunity was not considered.
The baseline vaccination strategy, wherein adults and children accepted the only offered vaccine, was designated as no choice. The likelihood of vaccination in the no-choice strategy was based on the mean observed monthly vaccination rates over 5 influenza seasons from 2009–2010 to 2013–2014 (https://www.cdc.gov/flu/fluvaxview/).
Three additional strategies were considered, in which agents could choose between 2 age-appropriate alternative vaccines. In the pediatric-choice strategy, children aged 2–18 years “chose” randomly between IIV-IM and LAIV. In the adult-choice strategy, adults aged 19–65 years “chose” either IIV-IM or IIV-ID. The latter vaccine choice in each strategy represented needle-sparing vaccine-delivery options (LAIV is a nasal spray, and the ID needle is only 1.5-mm long). The fourth strategy was choice in both age groups: Options were offered to both adults and children. Coverage for no choice and adjustments for coverage distributions between pairs of vaccines can be found in Table 1.
The vaccine coverage within the respective targeted age strata in pediatric choice, adult choice, and choice in both age groups for the base case was assumed to be 6.5% greater than that in the no-choice baseline strategy. In sensitivity analyses, changes in vaccine coverage due to choice were varied between 3.25% and 11.25%. In addition to the baseline epidemic, 9 experiments were conducted using 3 coverage increases for each of the 3 choice strategies.
Simulations
Using the Framework for Reconstructing Epidemic Dynamics ABM, 756 simulations were conducted in total. For each vaccination strategy, 189 individual simulations (accounting for inherent stochasticity as well as sensitivity analyses) were averaged, resulting in age-specific numbers of influenza cases. These estimates from the ABM provided highly accurate input for estimations for the CE analyses. All simulations were run on the Olympus High Performance Computing Cluster at the Pittsburgh Supercomputing Center in Pittsburgh, Pennsylvania.
CE and data sources
A decision analysis model was used to calculate, from a societal perspective, the CE of vaccination strategies using the incremental cost-effectiveness ratio (ICER)—the difference in cost between strategies divided by the difference in effectiveness between strategies, measured as quality-adjusted life years (QALYs) lost.
Costs and health outcomes for the CE analysis were derived from: 1) influenza vaccination costs based on vaccination likelihood; 2) the costs and likelihood of hospitalization and mortality due to influenza; and 3) the age-specific population likelihood of influenza disease from the ABM. Costs were the total medical costs associated with vaccination plus those associated with influenza health outcomes during the modeled season.
Total influenza vaccination costs included base costs of each vaccine multiplied by the likelihood of vaccination, adjusted by the proportion of the population vaccinated with each vaccine under the experimental strategies. Unit costs of vaccines were $10.69 for IIV-IM, $23.70 for LAIV, $15.69 for IIV-ID, and $23.69 for IIV-HD (27). Vaccine costs also included fixed administration costs common to all vaccines of $25.08, based on Medicare reimbursement data (28), irrespective of the recipient's age. Where choice occurred, an additional 5% administrative and 5% material cost, (varied between 2.5% and 7.5% in sensitivity analyses) was added to each respective vaccine cost component. For example, the average cost of a vaccine choice strategy when the vaccine given was IIV-IM was ($10.69 × 1.05) + ($25.08 × 1.05) = $37.56 compared to $35.77 ($10.69 + $25.08) when no choice was offered. The total vaccination cost in choice strategies, calculated within the ABM, was also varied from 0%–200% of the original value in the decision analysis model.
Average influenza costs per case (Table 2) were calculated from published data (26) after inflating to 2014 US dollars using the US Consumer Price Index. These illness costs include all hospitalized and fatal cases as well as those less severely affected. Using the ABM influenza case outputs, the decision analysis model used literature-based, age-specific population probabilities of influenza hospitalization and mortality (Table 2) to calculate influenza-related QALY losses (Appendix Table 1). Lost QALYs for nonhospitalized cases were modeled based on published data on the probabilities of being a high-risk case and/or requiring an office visit and their respective days of lost productivity (26). QALY losses due to influenza hospitalization were similarly based on days of lost productivity due to that event (26). Lifetime QALYs lost due to fatal influenza were estimated based on age group–specific life expectancies from US life tables and discounted at 3% per year. In sensitivity analyses, all influenza illness-related disutilities were varied from 50%–150% from their base case values.
Table 2.
Average Cost Per Influenza Case, Hospitalization Rate, and Mortality Rate, According to Age Groupa in an Agent-Based Model of a Synthetic Population
| Age Group, years | Average Cost Per Case, $ | Hospitalization Rate, % | Mortality Rate, % | |||
|---|---|---|---|---|---|---|
| Base | Range | Base | Range | Base | Range | |
| 6 months to 4 years | 388 | 161–878 | 1.41 | 0.47–2.35 | 0.0040 | 0.0013–0.0067 |
| 5–17 | 109 | 92–261 | 0.06 | 0.02–0.1 | 0.0010 | 0.0003–0.0017 |
| 18–49 | 265 | 122–742 | 0.42 | 0.14–0.7 | 0.009 | 0.003–0.015 |
| 50–64 | 1,146 | 489–2,984 | 1.93 | 0.64–3.21 | 0.134 | 0.0447–0.223 |
| ≥65 | 1,653 | 432–3,702 | 4.21 | 1.4–7.0 | 1.170 | 0.39–1.95 |
a Adapted from Molinari et al. (26).
RESULTS
No choice at baseline
At baseline, no choice with mild infectivity resulted in an average of 426,634 influenza cases, distributed by age group as follows: 8,075 in children aged 0–<2 years, 248,663 in children aged 2–<18 years, 155,744 in adults aged 18–<65 years, and 14,150 in those ≥65 years. For high infectivity, an average of 1,686,669 cases occurred, distributed by age group as follows: 37,890 in children aged 0–<2 years, 673,761 in children aged 2–<18 years, 881,918 in adults aged 18–<65, and 93,097 in those aged ≥65 years (values rounded to nearest integer).
Results of choice on the epidemic curve
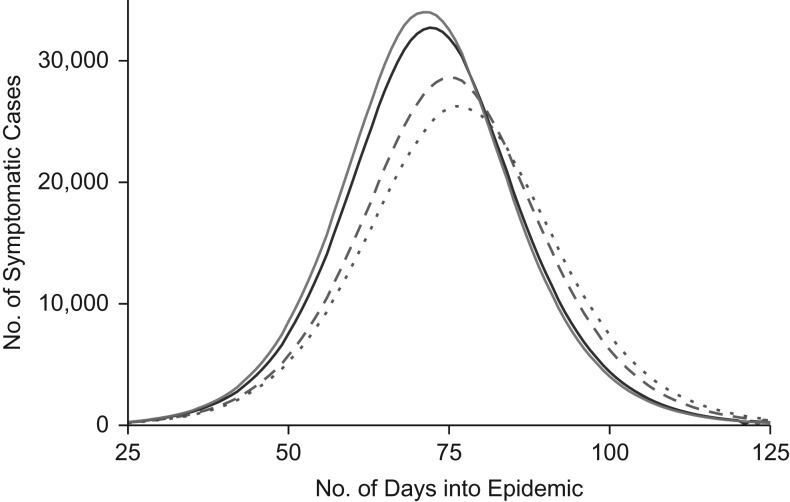
The epidemic curves for the base case of moderate influenza infectivity and a 6.5% increase in vaccine coverage for the 4 choice scenarios are displayed in Figure 1. The number of cases is fewer and the peak-onset date is delayed for choice strategies with larger differences observed in the choice-for-both-age-groups and adult-choice strategies.
Figure 1.
Epidemic curves for the base case of moderate influenza infectivity and a 6.5% increase in vaccine coverage due to choice strategies in an agent-based model of a synthetic population. The number of symptomatic cases over time is shown under conditions of no choice (solid gray), pediatric choice (solid black), adult choice (dashed gray), and choice for both age groups (dotted gray). Note that a weekly moving average was applied to smooth out the pronounced “weekend effect.”
Results of 6.5% increase in coverage due to choice across a range of infectivity values
When influenza was modeled with mild, moderate, and high infectivity, the number of cases increased with increasing infectivity of the influenza virus, but strategies that offered choice resulted in fewer influenza cases than the no-choice strategy. See Table 3.
Table 3.
Number of Cases of Influenza Predicted With 3 Vaccination Choice Strategies and 3 Levels of Influenza Infectivity in an Agent-Based Model of a Synthetic Population
| Infectivity | R0 | Vaccination Strategy | |||
|---|---|---|---|---|---|
| No Choice, No. of Cases |
Pediatric Choicea, No. of Cases |
Adult Choicea, No. of Cases |
Choice for Both Age Groups, No. of Cases |
||
| Mild | 1.0 | 426,634 | 387,863 | 308,103 | 272,073 |
| Moderate | 1.3 | 1,117,285 | 1,083,126 | 1,009,026 | 975,818 |
| High | 1.6 | 1,686,676 | 1,647,022 | 1,554,622 | 1,516,159 |
Abbreviation: R0, reproduction number.
a Pediatric choice was between live attenuated influenza vaccine and inactivated influenza vaccine–intramuscular delivery, and adult choice was between inactivated influenza vaccine–intramuscular delivery and inactivated influenza vaccine–intradermal delivery.
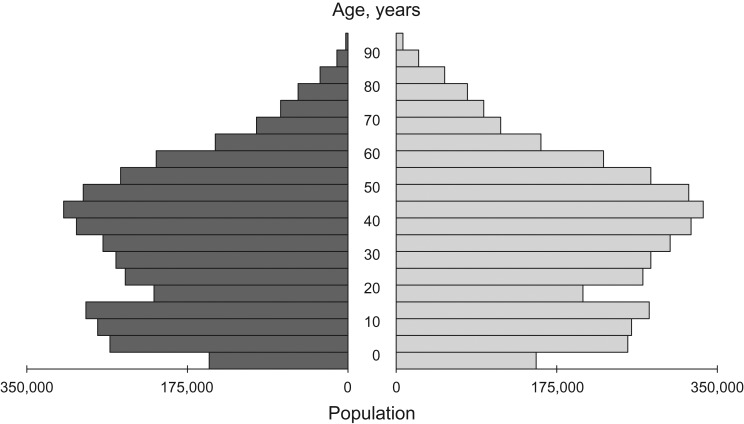
Web Figure 1 (available at http://aje.oxfordjournals.org/) depicts the changes in influenza cases averted by age, resulting from increases in vaccine coverage due to vaccine choice for three infectivity levels. In all models, 2 peaks of averted cases occurred, one in school-aged children and the other in adults aged approximately 40 years, and the highest numbers of averted cases across infectivity levels occurred for the choice-for-both-age-groups strategy. The largest increases in averted cases across strategies were seen in models with mild infectivity of influenza virus compared with more severe seasons. Pediatric choice resulted in virtually no change in the high-infectivity model. Notably, the choice-for-both-age-groups and adult-choice conditions reduced the number of influenza cases in both children and middle-aged adults. The largest age group of the DC metropolitan area population is adults aged in their 40s (see age histogram in Figure 2). When graphed as a fraction of the population, the averted cases among adults peaked at the same age, but at a lower level (data not shown). These 2 peaks suggest strong herd immunity among adults and their school-aged children.
Figure 2.
Age distribution according to sex in the Washington, DC, synthetic population. The age distribution of the population for men and boys is shown in dark gray in the left portion of the figure, and that for women and girls is shown in light gray in the right portion of the figure.
Results of various coverage increases across ages by choice strategy
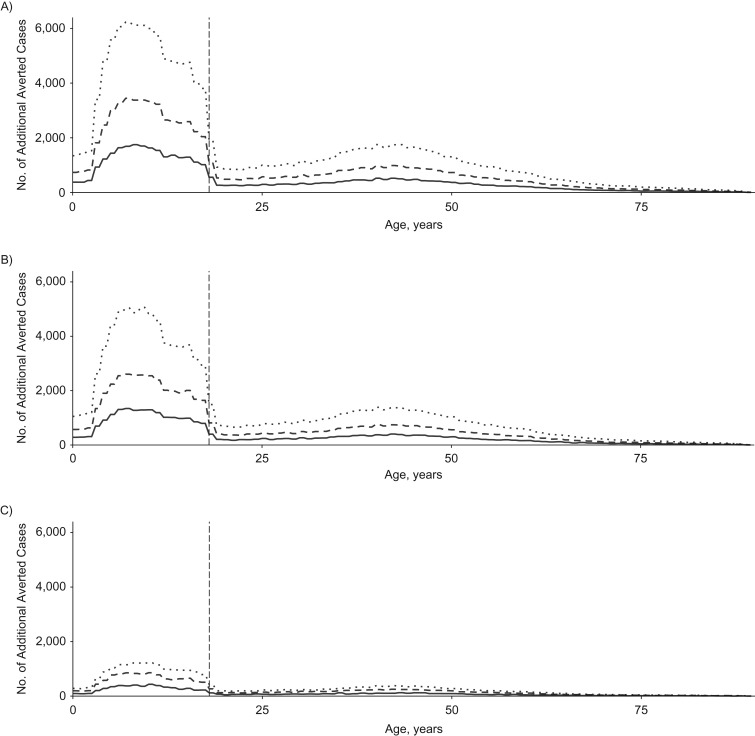
Figure 3 shows the influenza cases averted due to 3 increased coverage levels (3.25%, 6.5%, and 11.25%) as a result of offering vaccine choice when influenza infectivity is mild. Additional cases averted increased with increased coverage and are highest for the choice-for-both-age-groups strategy. For a 3.25% coverage increase with mild infectivity, cases averted averaged 14,621 for the pediatric-choice strategy (Figure 3A), 57,125 for the adult-choice strategy, and 75,462 for the choice-for-both-age-groups strategy. For an increase in coverage of 11.25% at mild infectivity (Figure 3C), cases averted averaged 54,497 for the pediatric-choice strategy, 218,765 for the adult-choice strategy, and 283,574 for the choice-for-both-age-groups strategy. Again, children benefited when choice was offered to adults. Extensive sensitivity analyses varying vaccine effectiveness resulted in no substantial changes in these results.
Figure 3.
Additional averted cases across ages according to strategy and increases in influenza vaccine coverage level at mild influenza infectivity in an agent-based model of a synthetic population. The number of additional cases averted (relative to the no-choice condition) against age in years at the 3 levels of coverage increase due to choice is shown for choice in both age groups (A), adult choice (B), and pediatric choice (C). In each of the 3 plots, an increase in coverage of 3.5% is shown with a solid line, 6.5% is shown with a dashed line, and 11.25% is shown with a dotted line. The dashed gray vertical line intercepts the x-axis at a value of 18 years (of age).
CE analysis
In the CE analysis using the burden-of-disease data from the ABM, the choice-for-both-age-groups strategy was less costly and more effective (i.e., dominant) compared with strategies offering choice to adults only, children only, or no choice at all. Table 4 shows the QALYs lost and incremental costs and effectiveness for the 4 choice strategies for the base case of 6.5% increased vaccine coverage. The choice-for-both-age-groups strategy was similarly dominant when vaccine choice increased coverage by 3.25% or 11.25% in sensitivity analyses (data not shown).
Table 4.
Cost-Effectiveness Analysis When Vaccine Choice Increases Coverage by 6.5% in an Agent-Based Model of a Synthetic Population
| Strategy | Cost | Incremental Cost | QALYs Lost | Incremental Effectiveness | Incremental CE Ratio |
| Choice in Both Groups | $52.28 | −0.00152 | |||
| Adult Choicea | $53.63 | $1.35 | −0.001582 | −0.000063 | Dominated |
| Pediatric Choicea | $57.45 | $5.17 | −0.001727 | −0.000207 | Dominated |
| No Choice | $58.88 | $6.60 | −0.001793 | −0.000273 | Dominated |
Abbreviations: CE, cost-effectiveness; QALY, quality adjusted life year.
a Pediatric choice was between live attenuated influenza vaccine and inactivated influenza vaccine–intramuscular delivery, and adult choice was between inactivated influenza vaccine–intramuscular delivery and inactivated influenza vaccine–intradermal delivery.
To test the robustness of these results, we performed another series of sensitivity analyses within the decision analysis model. Individual variations in illness costs, hospitalization or mortality risk, or QALYs lost due to illness events did not affect the dominance of the choice-for-both-age-groups strategy over other strategies when coverage increased 6.5% through vaccine choice. The choice-for-both-age-groups strategy was no longer dominant when influenza case rates were less than 6% of those listed above. Thus, for moderate infectivity models, influenza cases (no choice, average = 1,117,285; pediatric choice, average = 1,083,126; adult choice, average = 1,009,026; and choice for both age groups, average = 975,818) would each need to be reduced by more than 94% (due to a perhaps implausibly mild influenza season) to make choice for both age groups lose its dominance. The other sensitive parameter was vaccination cost for choice strategies when costs were doubled. Vaccination cost was derived from the ABM in which the additional costs of offering a choice of vaccines was determined to be $5–$26 per person, depending upon the age group. Choice for both age groups was no longer cost-saving when vaccine choice increased coverage by 6.5%. However, the choice-for-both-age-groups strategy in this situation cost $22,587 per QALY gained compared with other strategies, a value that is well within contemporary US CE benchmarks of $100,000 or more per QALY gained (29). Similar results (Table 5) occurred when the other choice-related vaccine coverage scenarios were similarly tested.
Table 5.
Sensitivity Analysis Showing Variation of Increased Coverage Due to Choice Strategies When the Vaccination Costs Are Doubled in an Agent-Based Model of a Synthetic Population
| Increase in Coverage With Choice | Incremental Cost-Effectiveness of Choice for Both Groups |
|---|---|
| 3.25% | $61,378/QALY gained |
| 6.50% | $22,587/QALY gained |
| 11.25% | $6,956/QALY gained |
Abbreviation: QALY, quality adjusted life year.
a Pediatric choice was between live attenuated influenza vaccine and inactivated influenza vaccine–intramuscular delivery, and adult choice was between inactivated influenza vaccine–intramuscular delivery and inactivated influenza vaccine–intradermal delivery.
DISCUSSION
This study used a simulated population of a large metropolitan area and the capability of ABM to model influenza vaccine choice strategies. Two findings with important public health implications resulted from this study. The first result was that offering a choice of influenza vaccine type, with its presumed increase in vaccine uptake, significantly decreased disease burden by reducing the number of influenza cases. In fact, the greater the change due to choice on coverage, the larger the public health benefit. Offering a choice of vaccines for all vaccinees aged 2 years or older (i.e., the choice-for-both-age-groups strategy) averted the largest number of cases of influenza overall. While the benefit of vaccine choice was observed in all ages, the changes were most pronounced in children.
The likelihood of increased influenza vaccine uptake due to a choice in vaccine types has some foundation in the literature. LAIV use varied widely by state, from 21% to 48% in 2013–2014 (30). The 2 states with the lowest childhood influenza vaccination rates overall had LAIV use below the US average (30). Thus, choice of a needle-free vaccine for children may result in greater uptake. Among adults, Nowalk et al. (4) found that offering a choice of vaccines to workers aged 18–49 years significantly increased uptake of vaccine.
Vaccine distribution data suggest that more choice is provided to children than to adults 19–64 years of age, with only 1% of adults receiving LAIV (31). Greater use of vaccine choice could affect influenza epidemiology in the United States and, if so, should be encouraged. Financial incentives either for achieving higher vaccination rates or for increasing choice are one option, as research has shown that financial incentives can affect clinical practice (32, 33) and are generally effective for providing a change in activity or quality of care (34). However, offering a choice of vaccines faces some practical limitations. The combination of a limited shelf life of LAIV and its higher cost may limit its use in some settings. Second, LAIV and IIV-ID are each manufactured by a single producer; thus, if an interruption of the manufacturing process occurs, the entire market for that product would be affected, which would limit vaccine options.
Despite the higher cost of alternative vaccines compared with IIV, choice for both age groups dominated the other strategies; that is, it was more effective and less costly. Results were robust to variation in sensitivity analyses, changed only by marked decreases in the baseline risk of influenza, as manifested by the influenza case frequency, or by doubling vaccination costs in choice strategies. Even with those higher vaccination costs, the choice-for-both-age-groups strategy remained well within economically reasonable ranges. Overall, vaccine choice is a viable option for reducing influenza burden in the United States, with the potential to decrease total costs due to influenza and its prevention.
The second finding with considerable public health implication is the association between vaccine choice strategies that included adults and lower influenza among children. In this study, the synthetic population of the DC metropolitan area comprised a preponderance of adults aged in their 40s. Many of the children of these individuals would likely have been of school age. Protection of children by vaccinating adults has been suggested for parents of newborns using a cocooning strategy (35–37). With the finding that increased vaccination of adults reduced the burden of influenza in children, due to herd immunity affecting the transmission of influenza, the idea of cocooning may be extended to influenza vaccination. This protection of children through increased vaccine uptake as a result of vaccine choice among adults should be explored further using ABM in different demographic regions. If confirmed, this finding would give added rationale to the Center for Disease Control and Prevention's historic change in recommendations—from a strategy based on vaccinating persons at high risk of complications to the current strategy of universal vaccination (3).
In addition to repeating the ABM in other regions with different population age distributions, several other subsequent steps could be considered, including confirmation of these findings in a different ABM entirely or using equation-based modeling. Federal vaccine policy-makers might consider undertaking formal deliberations about recommending a choice of influenza vaccines, given that there are survey data (5–9), clinical trials (4), and now modeling data to support this practice. Insurers, practice managers, and clinician leaders might consider and test ways to foster vaccine choice, towards the goal of improved coverage.
Strengths and limitations
The ABM was robust and the analyses were relatively insensitive to tested changes in parameters, including infectivity. However, simulations cannot take the place of randomized trial data and are subject to the population and to the parameters included. Hence, we used conservative estimates of vaccine effectiveness derived from meta-analyses. ABM is complex and time-consuming to run, requiring a supercomputer cluster; thus, we limited the number of sensitivity analyses and number of choice strategies. With additional resources, a broader range of strategies could be considered.
Conclusions
According to our modeling, the strategy of offering a choice of influenza vaccines for adults and children, with reasonable resultant coverage increases, decreased influenza cases by more than 100,000 in a US metropolitan region. In this population, providing adults with vaccine choice reduced influenza in children. Clinical trials testing the predictions made based on these simulation results and deliberation of policies and procedures to facilitate choice should be considered.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Pittsburgh Supercomputing Center, Carnegie Mellon University, Pittsburgh, Pennsylvania (Jay V. DePasse, Shawn T. Brown); Department of Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania (Kenneth J. Smith); Department of Family Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania (Jonathan M. Raviotta, Mary Patricia Nowalk, Richard K. Zimmerman); and Department of Mathematics, Soongsil University, Seoul, Republic of Korea (Eunha Shim).
This work was supported in part by the National Institute of General Medical Sciences (grant R01 GM111121).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
R.K.Z. has active research grants from Sanofi Pasteur, Pfizer Inc., and Merck & Co. Inc. M.P.N. and J.M.R. have research grant funding from Pfizer Inc. and Merck & Co. Inc. The other authors report no conflicts.
Appendix Table 1.
Quality Adjusted Life Years Lost Due to Influenza Illness, Hospitalization, and Mortality According to Age Group in an Agent-Based Model of a Synthetic Population
| Age Group, years | Loss of QALYs When Ill But Not Hospitalizeda | Loss of QALYs When Hospitalizedb | Loss of QALYs Due to Deathc |
| 6 months to 2 years | 0.00339 | 0.0252 | 30.91 |
| 3–4 | 0.00339 | 0.0252 | 30.7 |
| 5–9 | 0.0024 | 0.0287 | 30.25 |
| 10–17 | 0.0024 | 0.0287 | 29.45 |
| 18–49 | 0.00212 | 0.0366 | 25.52 |
| 50–64 | 0.00421 | 0.0456 | 18.41 |
| ≥65 | 0.0113 | 0.0426 | 10.25 |
Abbreviation: QALY, quality adjusted life year.
a Disutility of nonhospitalized influenza were calculated from Molinari et al. (26).
b Disutility of hospitalized influenza were calculated from Molinari et al. (26).
c Losses due to mortality were calculated from mortality table life expectancy (45), discounted at 3% per year. Listed values were varied by 50% in sensitivity analyses.
REFERENCES
- 1. Centers for Disease Control and Prevention (CDC) Interim adjusted estimates of seasonal influenza vaccine effectiveness—United States, February 2013. MMWR Morb Mortal Wkly Rep. 2013;62(7):119–123. [PMC free article] [PubMed] [Google Scholar]
- 2. Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the united states. JAMA. 2003;289(2):179–186. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention (CDC) Early estimates of seasonal influenza vaccine effectiveness—United States, January 2013. MMWR Morb Mortal Wkly Rep. 2013;62(2):32–35. [PMC free article] [PubMed] [Google Scholar]
- 4. Nowalk MP, Lin CJ, Toback SL, et al. Improving influenza vaccination rates in the workplace: a randomized trial. Am J Prev Med. 2010;38(3):237–246. [DOI] [PubMed] [Google Scholar]
- 5. Flood EM, Block SL, Hall MC, et al. Children's perceptions of influenza illness and preferences for influenza vaccine. J Pediatr Health Care. 2011;25(3):171–179. [DOI] [PubMed] [Google Scholar]
- 6. Flood EM, Ryan KJ, Rousculp MD, et al. A survey of children's preferences for influenza vaccine attributes. Vaccine. 2011;29(26):4334–4340. [DOI] [PubMed] [Google Scholar]
- 7. Flood EM, Ryan KJ, Rousculp MD, et al. Parent preferences for pediatric influenza vaccine attributes. Clin Pediatr (Phila). 2011;50(4):338–347. [DOI] [PubMed] [Google Scholar]
- 8. Arnou R, Frank M, Hagel T, et al. Willingness to vaccinate or get vaccinated with an intradermal seasonal influenza vaccine: a survey of general practitioners and the general public in France and Germany. Adv Ther. 2011;28(7):555–565. [DOI] [PubMed] [Google Scholar]
- 9. Reygrobellet C, Viala-Danten M, Meunier J, et al. Perception and acceptance of intradermal influenza vaccination: patient reported outcomes from phase 3 clinical trials. Hum Vaccin. 2010;6(4):336–345. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention VFC CDC vaccines price list archives. 2015. http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/archive.html. Published September 23, 2008. Updated March 21, 2017. Accessed January 22, 2016.
- 11. Lee BY, Brown ST, Bailey RR, et al. The benefits to all of ensuring equal and timely access to influenza vaccines in poor communities. Health Aff (Millwood). 2011;30(6):1141–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee BY, Brown ST, Cooley P, et al. Vaccination deep into a pandemic wave potential mechanisms for a “third wave” and the impact of vaccination. Am J Prev Med. 2010;39(5):e21–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee BY, Brown ST, Cooley PC, et al. A computer simulation of employee vaccination to mitigate an influenza epidemic. Am J Prev Med. 2010;38(3):247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee BY, Brown ST, Korch GW, et al. A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine. 2010;28(31):4875–4879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grefenstette JJ, Brown ST, Rosenfeld R, et al. FRED (a Framework for Reconstructing Epidemic Dynamics): an open-source software system for modeling infectious diseases and control strategies using census-based populations. BMC Public Health. 2013;13:940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wheaton WD, Cajka JC, Chasteen BM, et al. Synthesized Population Databases: A US Geospatial Database for Agent-Based Models. http://www.rti.org/pubs/mr-0010-0905-wheaton.pdf Research Triangle Park, NC: RTI Press; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee BY, Tai JH, Bailey RR, et al. The timing of influenza vaccination for older adults (65 years and older). Vaccine. 2009;27(50):7110–7115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Elveback LR, Fox JP, Ackerman E, et al. An influenza simulation model for immunization studies. Am J Epidemiol. 1976;103(2):152–165. [DOI] [PubMed] [Google Scholar]
- 19. Longini IM Jr, Halloran ME, Nizam A, et al. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159(7):623–633. [DOI] [PubMed] [Google Scholar]
- 20. Ferguson NM, Cummings DA, Cauchemez S, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437(7056):209–214. [DOI] [PubMed] [Google Scholar]
- 21. Ferguson NM, Cummings DA, Fraser C, et al. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Germann TC, Kadau K, Longini IM Jr, et al. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA. 2006;103(15):5935–5940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Halloran ME, Ferguson NM, Eubank S, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci USA. 2008;105(12):4639–4644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cooley P, Brown S, Cajka J, et al. The role of subway travel in an influenza epidemic: a New York City simulation. J Urban Health. 2011;88(5):982–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cooley P, Lee BY, Brown S, et al. Protecting health care workers: a pandemic simulation based on Allegheny County. Influenza Other Respir Viruses. 2010;4(2):61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention Vaccines for Children Program (VFC). 2015. http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/. Updated March 1, 2017. Accessed January 22, 2016.
- 28. Centers for Medicare & Medicaid Services Physician Fee Schedule Search. 2016. https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx. Updated January 19, 2017. Accessed January 22, 2016.
- 29. Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–797. [DOI] [PubMed] [Google Scholar]
- 30. Kahn KE, Santibanez TA, Zhai Y, et al. Influenza vaccination type, live, attenuated influenza vaccine (LAIV) versus inactivated influenza vaccine (IIV), received by children, United States, 2011–12 through 2013–14 influenza seasons. Vaccine. 2015;33(39):5196–5203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Antonova E, Ambrose CS, Kern D, et al. Seasonal influenza vaccination trends from 2007–2011 in privately insured children and adults in the United States. Vaccine. 2014;32(48):6563–6568. [DOI] [PubMed] [Google Scholar]
- 32. Fairbrother G, Siegel MJ, Friedman S, et al. Impact of financial incentives on documented immunization rates in the inner city: results of a randomized controlled trial. Ambul Pediatr. 2001;1(4):206–212. [DOI] [PubMed] [Google Scholar]
- 33. Kouides RW, Bennett NM, Lewis B, et al. Performance-based physician reimbursement and influenza immunization rates in the elderly. The Primary-Care Physicians of Monroe County. Am J Prev Med. 1998;14(2):89–95. [DOI] [PubMed] [Google Scholar]
- 34. Flodgren G, Eccles MP, Shepperd S, et al. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev. 2011(7):CD009255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guzman-Cottrill JA, Phillipi CA, Dolan SA, et al. Free vaccine programs to cocoon high-risk infants and children against influenza and pertussis. Am J Infect Control. 2012;40(9):872–876. [DOI] [PubMed] [Google Scholar]
- 36. Moriarty LF, Omer SB. Infants and the seasonal influenza vaccine. A global perspective on safety, effectiveness, and alternate forms of protection. Hum Vaccin Immunother. 2014;10(9):2721–2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Maltezou HC, Fotiou A, Antonakopoulos N, et al. Impact of postpartum influenza vaccination of mothers and household contacts in preventing febrile episodes, influenza-like illness, healthcare seeking, and administration of antibiotics in young infants during the 2012–2013 influenza season. Clin Infect Dis. 2013;57(11):1520–1526. [DOI] [PubMed] [Google Scholar]
- 38. Santibanez TA, O'Halloran A, Zhai Y, et al. Flu Vaccination Coverage, United States, 2013-14 Influenza Season. 2014. http://www.cdc.gov/flu/fluvaxview/coverage-1314estimates.htm. Updated January 28, 2016. Accessed July 1, 2016.
- 39. Health Industry Distributors Association 2014 Influenza Vaccine Production and Distribution Market Brief. Alexandria, VA: Health Industry Distributors Association; 2014. [Google Scholar]
- 40. Zimmerman RK, Lauderdale DS, Tan SM, et al. Prevalence of high-risk indications for influenza vaccine varies by age, race, and income. Vaccine. 2010;28(39):6470–6477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Influena vaccine for 2015–2016. Med Lett Drugs Ther. 2015;57(1477):125–127. [PubMed] [Google Scholar]
- 42. Glazner JE, Beaty B, Berman S. Cost of vaccine administration among pediatric practices. Pediatrics. 2009;124(suppl 5):S492–S498. [DOI] [PubMed] [Google Scholar]
- 43. Lee BY, Bailey RR, Wiringa AE, et al. Economics of employer-sponsored workplace vaccination to prevent pandemic and seasonal influenza. Vaccine. 2010;28(37):5952–5959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Osterholm MT, Kelley NS, Sommer A, et al. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(1):36–44. [DOI] [PubMed] [Google Scholar]
- 45. Arias E. United States Life Tables, 2011. Natl Vital Stat Rep. 2015;64(11):1–63. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.