Abstract
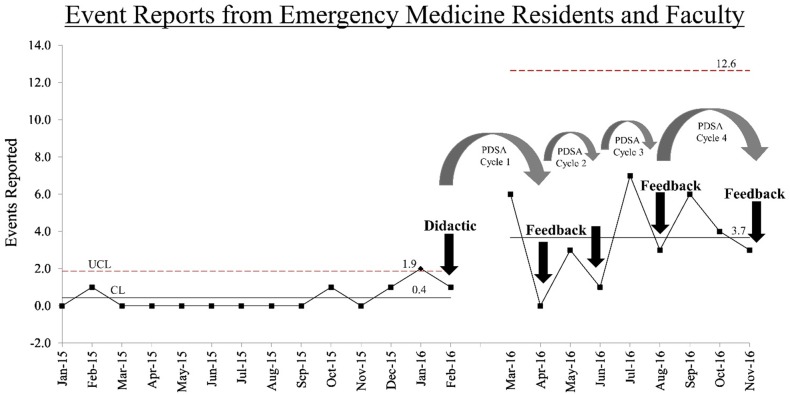
Patient safety event reporting is an important component for fostering a culture of safety. Our tertiary care hospital utilizes a computerized patient safety event reporting system that has been historically underutilized by residents and faculty, despite encouragement of its use. The objective of this quality project was to increase patient safety event reporting within our Emergency Medicine residency program. Knowledge of event reporting was evaluated with a survey. Eighteen residents and five faculty participated in a formal educational session on event reporting followed by feedback every two months on events reported and actions taken. The educational session included description of which events to report and the logistics of accessing the reporting system. Participants received a survey after the educational intervention to assess resident familiarity and comfort with using the system. The total number of events reported was obtained before and after the educational session. After the educational session, residents reported being more confident in knowing what to report as a patient safety event, knowing how to report events, how to access the reporting tool, and how to enter a patient safety event. In the 14 months preceding the educational session, an average of 0.4 events were reported per month from the residency. In the nine months following the educational session, an average of 3.7 events were reported per month by the residency. In addition, the reported events resulted in meaningful actions taken by the hospital to improve patient safety, which were shared with the residents. Improvement efforts including an educational session, feedback to the residency of events reported, and communication of improvements resulting from reported events successfully increased the frequency of safety event reporting in an Emergency Medicine residency.
Problem
Computerized patient safety event reporting was historically underutilized by residents and faculty in an Emergency Medicine residency at an urban tertiary care hospital in Illinois, USA, despite regular encouragement of its use by quality and safety leadership. Event reporting is a necessary component of a culture of safety. Event reporting and review are important areas of focus for the Accreditation Council for Graduate Medical Education Clinical Learning Environment Review.1 The objective of this project was to promote a culture of safety and meet patient safety and quality improvement requirements from the Accreditation Council for Graduate Medical Education in an Emergency Medicine residency by enhancing utilization of our computerized patient safety event reporting system. Although the actual number of patient safety events that occur and should be reported is unknown, a 30% increase within 6 months above the 0.4 average events reported per month at baseline was set as a target. The number of events was tracked by our computerized patient safety event reporting system and was reported back to the residency every other month by the System Director of the Patient Safety Department.
Background
Educational interventions that increase knowledge of what patient safety events to report, demonstrate use of the reporting system, and encourage and educate physicians on their responsibility for patient safety have shown to increase patient safety event reporting.2 3 4 In 2017, Children's Hospital of Pittsburg of University of Pittsburgh Medical Center increased the mean rate of monthly event reporting from 3.6 to 37.8 in a program with 113 graduate trainees by implementing a longitudinal multi-year curriculum to increase safety event reporting.5 Dunbar et al., increased the physician event reporting rate through didactics, feedback on institutional responses to reported events, and Institute for Healthcare Improvement online training modules.6 Though it is not certain what constitutes a target safety event reporting rate, a relatively small percentage of reports are submitted by physicians. A study of over 90,000 event reports from 26 hospitals found that only 1.4% of event reports were submitted by physicians and further efforts should be made to increase physician roles in quality efforts.7 Although reporting frequency increases initially following educational interventions, event reporting sustainability is difficult to maintain.2 Continued education and timely feedback of events reported and resulting system changes help maintain a culture that is committed to ongoing patient safety event reporting.2 3 8
Our institution's event reporting system is accessible via a secure web based portal to all hospital employees, including all of our residents and faculty. The event reporting system requests the type of event, where the event occurred, who (if anyone) was effected by the event, severity of the event, whether there was an equipment malfunction, when the event occurred, a brief description of the event, and optionally anyone else involved in or witness to the event. When an event is submitted it is reviewed by staff in the patient safety department and the determination is made as to what additional action should be taken.
Baseline measurement
For this project, two measures were evaluated. The first measure was frequency of patient safety events reported in an Emergency Medicine residency by faculty and residents for 14 months prior to the intervention. In the 14 months preceding the intervention, an average of 0.4 events per month were reported from the residency, less than 10% of total patient safety events reported by all faculty and residents at the institution. EM residents represent 7% of the institution's residents and reported only 2% of all patient safety events submitted by the institution's residents. The second measure was evaluation of event reporting knowledge, evaluated by a voluntary anonymous survey (Supplemental Figure 1). The survey was given to all Emergency Medicine residents and faculty that were available to attend the session. 15/18 residents and 4/5 faculty were available and completed the survey.
bmjqir.u223876.w5716supp_fig1.pdf (156.1KB, pdf)
Design
Based on the low frequency of patient safety events reported by Emergency Medicine faculty and residents and lack of confidence in knowing what events to report, how to access the reporting tool, and how to use the reporting system, additional education on event reporting was developed. The target group for improvement was a three year Emergency Medicine residency with a total of 18 residents that contribute approximately 50% of their time at the study hospital and five faculty attendings that work exclusively at the study hospital. To address the problem, an educational intervention was designed and presented at an Emergency Medicine conference by the System Director of the Patient Safety Department. The didactic session outlined the purpose of event reporting, defined a patient safety event, and described the different event severity categories with specific examples for each category. A demonstration on where to find and how to use the reporting system was shared with the residency. The total number of events in each category (example-medication/fluid, lab/specimen), the number of events reported per month at the hospital, and the number of events reported by the Emergency Medicine residency (<0.1% of total events reported) for the previous year were shared. The session concluded with an explanation of what happens after an event is reported, which depending on the event severity may include a Plan, Do, Study, Act (PDSA) cycle, cause mapping, or Root Cause Analysis (RCA). To create event reporting momentum and to overcome sustainability issues reported previously, a periodic feedback system was designed to provide follow up to the Emergency Medicine residency on events reported and specific actions taken by the organization to address the patient safety events. Feedback sessions were given every other month during an Emergency Medicine conference by the System Director of the Patient Safety Department. Changes in the number of patient safety events reported were analyzed by an independent measures t-test.
Strategy
PDSA Cycle 1
To enhance knowledge of the event reporting system and increase frequency of patient safety events reported, Emergency Medicine residents and faculty participated in an educational didactic session. Familiarity of patient safety event reporting was evaluated with a survey (Supplemental Figure 2). The frequency of events reported was collected continuously and compared to 14 months of baseline data. Based on previous reports, we hypothesized the didactic session would initially increase the number of events reported followed by a decrease over time. Similar to previous studies, frequency of events reported initially increased but fell back to baseline levels the following month, supporting the need for an ongoing feedback mechanism.
bmjqir.u223876.w5716supp_fig2.pdf (93.5KB, pdf)
PDSA Cycle 2
To maintain increased frequency of patient safety events reported, feedback was provided to residents and faculty on what events were reported by the residency and specific actions taken by the organization to address the problems and prevent them from occurring again in the future. Data was collected continuously and compared to baseline and PDSA Cycle 1 data. We hypothesized feedback would augment event reporting frequency. An increase in event reporting was observed the month following the feedback session. However, frequency of reporting decreased the following month, although the number of reported events was higher than baseline levels. Providing feedback is a successful short-term strategy to increase patient safety event reporting.
PDSA Cycles 3-4
To further increase and sustain heightened event reporting numbers, encouragement and feedback sessions were continued with the aim to produce a lasting change in culture and a sustained increase in reporting levels. Frequency of events reported were compared to baseline and individual PDSA Cycles. Providing feedback of events reported and actions taken increased event reporting frequency the month after the feedback sessions. Although reporting frequency again fell the following months, event reporting remained above baseline levels. Incorporation of a long-term feedback mechanism into residency conferences is important for sustainability of patient safety event reporting.
Results
The pre-didactic survey identified a knowledge gap on what is considered a reportable patient safety event and how to use the reporting technology. After participation in the didactic session, residents reported feeling more confident in knowing what to report as a patient safety event (78% vs. 11%, P<0.001), knowing how to report events (94% vs. 37%, P<0.001), and how to enter a patient safety event (94% vs. 26%, P<0.001). In the 14 months preceding the educational session, an average of 0.4 events per month were reported from the residency. One of these events was submitted by a resident and five were submitted by faculty. In the nine months following the educational session, an average of 3.7 events per month were reported by the Emergency Medicine residency. Fourteen of these events were reported by residents and 19 were reported by faculty (p=0.02 and p<0.01, compared to baseline) (Figure 1). The System Director of the Patient Safety Department confirmed that all accounts from the residency were classified as reportable patient safety events. Events reported by Emergency Medicine residents since the beginning of the improvement phase represented 29% of events submitted by all residents, however Emergency Medicine residents comprise only 7% of the institution's residents. Event reporting was significantly enhanced in the months following the initial didactic and feedback sessions compared to months without a feedback session (p=0.02). The reported events resulted in meaningful actions taken by the hospital to improve patient safety, which were shared with residents (Table 1). Residents have stated they look forward to the patient safety reporting feedback and outcomes of the reports they have submitted. The residency has requested that the System Director of the Patient Safety Department continue to report back to the residency every other month with follow-up on their submitted patient safety reports.
Figure 1. Event reporting in an Emergency Medicine residency increased following an educational session on event reporting and feedback every two months.
Table 1.
Examples of patient safety events, severity of events, and organizational outcomes in an Emergency Medicine residency.
| Example Event Type | Severity | Organizational Outcome |
|---|---|---|
| Diagnostic Imaging-Patient Taken to CT without Proper Communication | Unsafe Condition | Patient Hand-Off Document Developed for all Patients Leaving the Emergency Department |
| Lab/Specimen-Results Issue Involving Point of Care Testing (i-STAT) | Unsafe Condition | Quality Control Completed. Cartridges Collected and Returned to Manufacturer for Investigation. |
| Medication/Fluid-Incorrect Medication Available in Formulary | Unsafe Condition | Option Inactivated |
| Diagnostic Imaging-Ordered and Completed on Incorrect Patient | No Harm-Reached Patient | Identified Trend: 10% of Reported Diagnostic Imaging Safety Events Involve an Incorrect Patient |
| Lab/Specimen-Results Issue Involving Point of Care Testing (i-STAT) | No Harm-Reached Patient | Education Material Developed for Emergency Department Physicians and Staff Regarding i-STAT Limitations |
| Airway Management-Delayed Intubation | Harm-Temporary Intervention Needed | Immediate: “Airway Box” Placed on Inpatient Rehab Crash Cart. In Progress: Patient Safety Debriefing and Proactive Risk Assessment |
The financial implications of increased event reporting are hard to quantify. Reducing waits and delays and providing effective and efficient services are important to quality patient care. In this study, the most frequently reported events involved delayed laboratory results. Reported events led to the development of patient hand-off documents, updated medication forms, dissemination of educational materials to Emergency Department physicians and staff, and placement of life saving materials at appropriate locations throughout the hospital.
Lessons and limitations
Completion of the project further validated the importance of closing the communication loop between the patient safety organization and event reporters to maintain sustainability of increased event reporting. It was a challenge to maintain increased reporting during months without a feedback session and it is unknown if reporting frequency would fall back to baseline if feedback sessions were stopped completely. A limitation of the study was that it was performed at a single institution in a single residency program and results cannot be generalized. There was no turnover in faculty for the duration of the study though a graduating class of six residents was replaced by six new entering residents. Faculty and residents submitting event reports were aware these events would be reported back on a bi-monthly basis and two of the authors participated in the project. The study period was relatively short, including a baseline period of 14 months and a post-intervention period of nine months. However, we continue to collect and monitor patient safety event reporting frequency and outcomes. Additionally, the actual number of patient safety events that occur and should be reported is unknown.
Conclusion
The goal of this quality project was to increase patient safety event reporting within our Emergency Medicine residency program. An educational session on the types of events to report and how to use the reporting tool enhanced resident confidence in knowing what to report as a patient safety event and knowing how to access and use the reporting tool. An educational session, feedback to the residency of events reported, and communication of improvements resulting from reported events successfully increased the frequency of safety event reporting in an Emergency Medicine residency. In addition, the reported events resulted in meaningful actions taken by the hospital to improve patient safety. As previously reported, the educational intervention alone was not effective in sustaining increased event reporting frequency.3 Ongoing feedback of events reported and resulting system changes are needed to create and maintain culture change.
The intervention was implemented solely in the Emergency Medicine residency program at a single institution. Use of didactic and feedback sessions in additional residency programs within the institution has the potential to improve patient safety hospital wide. Buy in from stakeholders, department directors and resident leaders is critical for success. Educating physicians on their responsibility for patient safety and the quality improvement requirements from the Accreditation Council for Graduate Medical Education is important. Future directions include development of a communication mechanism that provides residency specific reporting numbers, which may encourage reporting competition and compliance. Development of an event reporting mobile application has the potential to further reduce reporting barriers such as lack of physician time and opportunities to access the reporting tool. Including residents in RCA or similar processes specific to their reported patient safety events is an opportunity for individual investment in system change. While not every event reported led to a specific organizational action or change, the reporting of unsafe conditions and near misses helped identify organizational trends and prioritize opportunities for future quality work.
Acknowledgments
The Emergency Medicine Residents and Faculty of the Southern Illinois University School of Medicine
Footnotes
Declaration of interests: I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.
Ethical approval: The submission has been reviewed by the local institutional review board. It was determined that this project was not research involving human subjects.
References
- 1.Wagner R, Koh N, Patow C, Newton R, Casey B, Weiss K. Detailed findings from the CLER National Report of Findings 2016. J Grad Med Educ. 2016. May;8:35–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louis M, Hussain L, Dhanraj D et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016;16:73–80. [PMC free article] [PubMed] [Google Scholar]
- 3.Boike J, Bortman J, Radosta J et al. Patient safety event reporting expectation: does it influence residents' attitudes and reporting behaviors? J Patient Saf. 2013. Jun;9:59–67. [DOI] [PubMed] [Google Scholar]
- 4.Jericho B, Tassone R, Centomani N et al. An assessment of an educational intervention on resident physician attitudes, knowledge, and skills related to adverse event reporting. J Grad Med Educ. 2010. Jun;2:188–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox M, Bump G, Butler G, Chen L, Buchert A. Making residents part of the safety culture: improving error reporting and reducing harms. J Patient Saf. 2017. Jan 30. [DOI] [PubMed] [Google Scholar]
- 6.Dunbar A 3rd, Cupit M, Vath R et al. An improvement approach to integrate teaching teams in the reporting of safety events. Pediatrics. 2017. Feb;139. [DOI] [PubMed] [Google Scholar]
- 7.Milch C, Salem D, Pauker S, Lundquist T, Sumar S, Chen J. Voluntary electronic reporting of medical errors and adverse events. An analysis of 92,547 reports from 26 acute care hospitals. J Gen Intern Med. 2006. Feb;21:165–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaldjian L, Jones E, Wu B, Forman-Hoffman V, Levi B, Rosenthal G. Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med. 2008. Jan 14;168:40–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqir.u223876.w5716supp_fig1.pdf (156.1KB, pdf)
bmjqir.u223876.w5716supp_fig2.pdf (93.5KB, pdf)