Abstract
Background:
Traditional Chinese medicine Taraxacum officinale has been widely used to treat various inflammatory diseases. Taraxasterol is one of the main active components isolated from Taraxacum officinale. Recently, we have demonstrated that taraxasterol has the in vitro anti-inflammatory effects. This study aims to determine the in vivo anti-inflammatory effects of taraxasterol against animal models.
Materials and Methods:
Anti-inflammatory effects were assessed in four animal models by using dimethylbenzene-induced mouse ear edema, carrageenan-induced rat paw edema, acetic acid-induced mouse vascular permeability and cotton pellet-induced rat granuloma tests.
Results:
Our results demonstrated that taraxasterol dose-dependently attenuated dimethylbenzene-induced mouse ear edema and carrageenan-induced rat paw edema, decreased acetic acid-induced mouse vascular permeability and inhibited cotton pellet-induced rat granuloma formation.
Conclusion:
Our finding indicates that taraxasterol has obvious in vivo anti-inflammatory effects against animal models. It will provide experimental evidences for the traditional use of Taraxacum officinale and taraxasterol in inflammatory diseases.
Keywords: Taraxasterol, ear edema, paw edema, vascular permeability, granuloma
Introduction
Inflammation is the first response of the immune system to irritation or infection caused by numerous stimuli and the normal result of host protective response to tissue injury; it often shows as redness, swelling, pain and dysfunction of tissues and organs (Ialenti et al., 1993; Zhang et al., 2012). On the one hand, inflammation initiates the healing process and eliminates invading pathogens. On the other hand, uncontrolled inflammation causes injury of cells and tissues, and leads to chronic inflammation, chronic diseases and neoplastic transformation (Mantovani et al., 2008; Cai et al., 2014). At present, SAIDs and NSAIDs are used in the treatment of most inflammatory diseases as conventional anti-inflammatory drugs. However, their long-term use, especially at higher doses, may produce many local and systemic adverse effects including gastrointestinal disorders, humoral disturbances and immunodeficiency (Nagatomi and Ando, 1984; Simon, 2003; Roth, 2012). Thus, increasing attention has focused on ethnological medicinal plants as new anti-inflammatory drugs for long-term use because they have fewer side effects.
Taraxacum officinale has been frequently used in traditional medicine because of its choleretic, lactating, diuretic, anti-inflammatory and antirheumatic properties (Kisiel and Barszcz, 2000; Ahmad, 2000). It is widely used to treat various infectious and inflammatory diseases in clinic such as bronchitis, pneumonia, upper respiratory tract infections, hepatitis and mastopathy (Sweeney et al., 2005; Leu et al., 2005). Pharmacological activities of Taraxacum officinale including its anti-inflammatory, anti-angiogenic, anti-nociceptive effects have been in part demonstrated (Schütz et al., 2006; Jeon et al., 2008; Liu et al., 2010). Taraxasterol (Figure 1) is one of main active components isolated from Taraxacum officinale. Recently, we have shown that taraxasterol has anti-inflammatory activity in vitro by regulating proinflammatory cytokine and mediator production through suppressing NF-κΒ and MAPK signaling pathways (Zhang et al., 2012; Xiong et al., 2014). Our studies also demonstrated its protective effects on OVA-induced mouse allergic asthma (Liu et al., 2013) and LPS-induced mouse endotoxic shock (Zhang et al., 2014). Thus, as a part of our on-going screening program to demonstrate the anti-inflammatory activities of natural drugs, we evaluated the in vivo anti-inflammatory effects of taraxasterol against several animal models. Namely, dimethylbenzene-induced ear edema of mice, carrageenan-induced paw edema of rats, acetic acid-induced vascular permeability of mice and cotton pellet-induced granuloma of rats, designed to examine the vasodilatation, edema formation, permeability accentuation and tissue hyperplasia.
Figure 1.
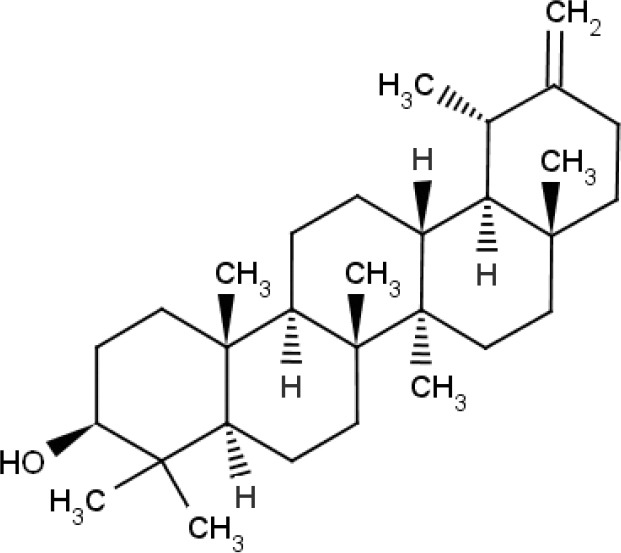
Chemical structure of taraxasterol.
Materials and methods
Animals
Male Wistar rats (200-220 g) and Kunming mice (18-22 g) were obtained from Experimental Animal Centre of Medical College of Yanbian University (Jilin, China). All animals were maintained under standard laboratory conditions for a minimum of one week to fit the experimental environment, and received water and food ad libitum. The experimental processes of all animals were carried out in accordance with the guidelines of the Ethical Committee for the experimental use of animals at Yanbian University (Jilin, China).
Reagents
Taraxasterol (purity was 99.5% based on HPLC analysis) was obtained from Chengdu Fenruisi Biotechnology Company (Sichuan, China). Dexamethasone (DXM) (No.H41020055) was purchased from Changle Pharmaceutical Company (Henan, China). Carrageenan was purchased from Sigma Chemical Company (St. Louis, MO, USA). Dimethylbenzene and other agents (analytical grade) of this study were purchased from Kermel Chemical Reagent Limited Company (Tianjin, China).
Assessment of dimethylbenzene-induced mouse ear edema
Mice were randomly divided into five groups (n=10): taraxasterol groups (2.5, 5 and 10 mg/kg), control group, positive treatment group. Mice in taraxasterol groups were intragastrically given taraxasterol (2.5, 5 and 10 mg/kg, respectively) in 0.5% CMC-Na for 5 days once per day consecutively. Mice in control group were intragastrically given 0.5% CMC-Na. Mice in positive group were intraperitoneally given DXM (2.5 mg/kg) once 1 h prior to dimethylbenzene administration. At 1 h after last drug administration, ear edema was induced by topical application of dimethylbenzene on the mouse right ears. The mouse left ears were used as control. At 1 h after dimethylbenzene induction, the mice were sacrificed under anesthesia, and discs of 6.0 mm diameter were punched out from each ear of each mouse and weighed. The ear edema (mg) = weight of mouse right ear (mg) - weight of mouse left ear (mg) (Wang et al., 2014).
Assessment of carrageenan-induced rat paw edema
Rats were randomly divided into five groups (n=10): taraxasterol groups (2.5, 5 and 10 mg/kg, respectively), control group, positive treatment group. The methods of drug administration were the same as the above described. At 1 h after last drug administration, the right hind paws of rats were injected 0.1 ml of 1% freshly prepared carrageenan suspension by sub plantar. Paw edema was measured immediately prior to and 1, 2, 3, 4 and 5 h after carrageenan induction by wrapping a piece of cotton thread round the paw of each rat and recording the length of the cotton thread (Cai et al., 2014).
Assessment of acetic acid-induced mouse vascular permeability
Mice were randomly divided into five groups (n=10): taraxasterol groups (2.5, 5 and 10 mg/kg, respectively), control group, positive treatment group. The methods of drug administration were the same as the above described. At 1 hour after last drug administration, the mice were intravenously injected 0.2 ml of 2% Evans blue. Simultaneously, 10 ml/kg of 0.7% acetic acid was abdominally injected. The mice were sacrificed under anesthesia at 30 min after acetic acid injection; mouse abdominal cavity was washed with normal saline solution. The recovered normal wash solution was centrifuged, and the OD value of the supernatant was measured at 590 nm on a microplate reader (Wang et al., 2014).
Assessment of cotton pellet-induced rat granuloma
The sterile cotton pellets were implanted by a single needle incision into both axillae regions of rats under ether anesthesia. Rats were randomly divided into five groups (n=10) once daily for 7 days for taraxasterol groups (2.5, 5 and 10 mg/kg, orally), control group (0.5% CMC-Na, orally), positive group (2.5 mg/kg DXM, intraperitoneally). On day 8, the wet cotton pellets were carefully dissected, weighed and dried at 60°C for 12 h. The granuloma formation was measured by the increase in dry weight of the pellets (Cai et al., 2014).
Statistical analysis
All data are represented as means ± SEMs. Statistical analysis was performed using one-way ANOVA. Statistical significance was accepted at P<0.05.
Results
Effects of taraxasterol on dimethylbenzene-induced mouse ear edema
As shown in Figure 2, topical application of dimethylbenzene significantly caused mouse inflammatory response as judged by ear edema formation. However, compared with dimethylbenzene-induced control group, taraxasterol at 2.5, 5 and 10 mg/kg dose-dependently inhibited ear edema by 19.5%, 42.9% (P<0.05) and 57.2% (P<0.01), respectively. DXM also significantly inhibited dimethylbenzene-induced mouse ear edema (P<0.01).
Figure 2.
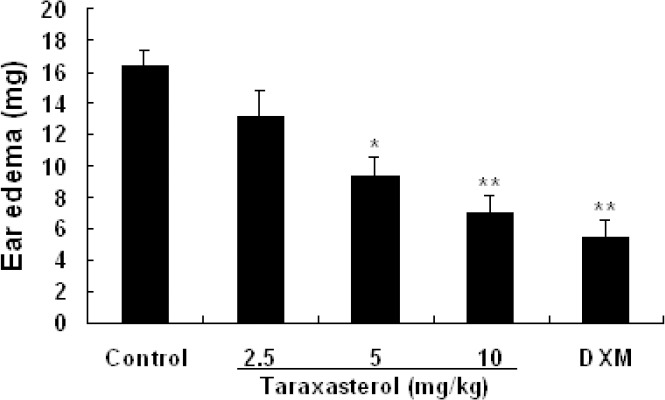
Effects of taraxasterol on dimethylbenzene-induced mouse ear edema. Mice were divided into five groups (n=10 for each group): taraxasterol groups (2.5, 5, 10 mg/kg, respectively), control group (0.5% CMC-Na), and DXM group (2.5mg/kg). Ear edema was induced by topical application of dimethylbenzene on the right ear of each mouse. One hour after dimethylbenzene induction, the ear edema was measured by subtracting the weight of mouse left ear from the weight of mouse right ear. Data represent means ± SEMs. *P<0.05, **P<0.01 vs. control group.
Effects of taraxasterol on carrageenan-induced rat paw edema
As shown in Figure 3, the rat paw edema obviously increased after carrageenan induction. However, compared with carrageenan-induced control group, taraxasterol at 2.5, 5 and 10 mg/kg dose-dependently suppressed paw edema at 1-5 h of carrageenan induction. Taraxasterol at 10 mg/kg suppressed paw edema by 34.5% (P0.01), 41.7% (P0.01), 55.1% (P0.01), 59.4% (P0.01) and 69.4% (P0.01) at 1, 2, 3, 4 and 5 h, respectively. At 3 h after carrageenan induction when edema reached its peak, taraxasterol at 2.5, 5 and 10 mg/kg decreased paw edema by 24.2% (P0.01), 41.5 % (P0.01) and 55.1% (P0.01), respectively. DXM also significantly decreased paw edema of rats (P<0.01).
Figure 3.
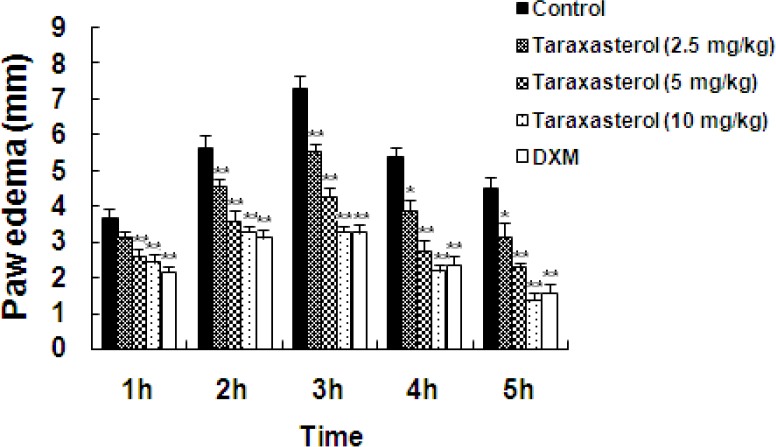
Effects of taraxasterol on carrageenan-induced rat paw edema. Rats were divided into five groups (n=10 for each group): taraxasterol groups (2.5, 5, 10 mg/kg, respectively), control group (0.5% CMC-Na), and DXM group (2.5mg/kg). The right hind paw of each rat was injected 1% freshly prepared carrageenan suspension by sub plantar. Paw edema was measured immediately prior to and 1, 2, 3, 4 and 5 h after carrageenan induction. Data represent means ± SEMs. *P<0.05, **P<0.01 vs. control group.
Effects of taraxasterol on acetic acid-induced mouse vascular permeability
The vascular permeability was represented by the amount of Evans blue extruded into abdominal cavity, which was measured by OD value of the supernatant. As shown in Figure 4, OD value obviously increased after acetic acid induction. Compared with acetic acid-induced control group, taraxasterol at 2.5, 5 and 10 mg/kg exhibited obvious inhibitory effect on acetic acid-induced mouse vascular permeability in a dose-dependent manner, and inhibitory rates were 20.3% (P<0.05), 35.7% (P<0.05) and 54.5% (P<0.01), respectively. DXM also markedly inhibited mouse vascular permeability (P<0.01).
Figure 4.
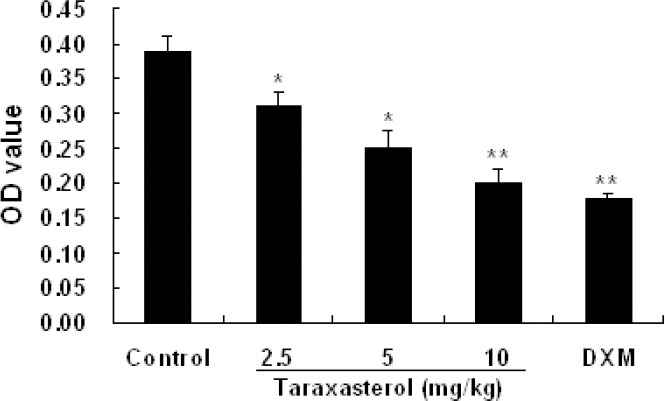
Effects of taraxasterol on acetic acid-induced mouse vascular permeability. Mice were divided into five groups (n=10 for each group): taraxasterol groups (2.5, 5, 10 mg/kg, respectively), control group (0.5% CMC-Na), and DXM group (2.5mg/kg). Mice were injected intravenously with 0.2 ml of 2% Evans blue and injected abdominally 10 ml/kg of 0.7% acetic acid. The OD value of the supernatant in abdominal cavity was measured. Data represent means ± SEMs. * P<0.05, ** P<0.01 vs. control group.
Effects of taraxasterol on cotton pellet-induced rat granuloma
The weight of granulation is an index of granuloma formation, which is used to evaluate chronic inflammation. As shown in Figure 5, granuloma formation was induced in the cotton pellet-induced control group. Compared with cotton pellet-induced control group, taraxasterol at 2.5, 5 and 10 mg/kg dose-dependently inhibited granuloma formation, and inhibitory rates were 10.7% (P<0.05), 33.7% (P<0.01) and 39.7% (P<0.01), respectively. DXM also significantly inhibited rat granuloma induced by cotton pellet (P<0.01).
Figure 5.
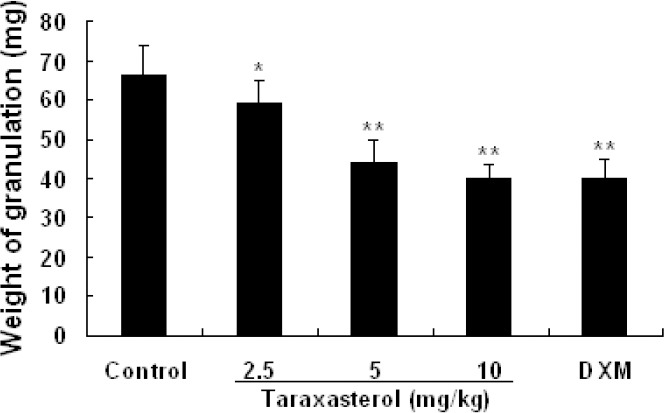
Effects of taraxasterol on cotton pellet-induced rat granuloma. The sterile cotton pellets were implanted by a single needle incision into both axillae regions of rats. Then the rats were divided into five groups (n=10 for each group): taraxasterol groups (2.5, 5, 10 mg/kg, respectively), control group (0.5% CMC-Na), and positive group (2.5 mg/kg DXM). On day 8, the wet cotton pellets were carefully dissected and the granuloma formation was measured by the increase in dry weight of the pellets. Data represent means ± SEMs. * P<0.05, ** P<0.01 vs. control group.
Discussion
Inflammation is a complex physiological response and may be acute and chronic (Medzhitov, 2008). Acute inflammation is characterized by vasodilatation, neutrophils infiltration, permeability accentuation and edema formation (Huang et al., 2011). Chronic inflammation is characterized by tissue proliferation, granuloma and repair (Eddouks et al., 2012). Acute inflammatory response will lead to chronic inflammation.
Edema is a typical inflammatory manifestation both local inflammation and systemic inflammation (Liu et al., 2010). The carrageenan-induced paw edema model is acute, highly reproducible and well-researched model (Morris, 2003). It has been commonly employed to assess the anti-edematous effects of natural drugs (Kang et al., 2010). To evaluate the effects of taraxasterol on acute inflammation, we used carrageenan-induced paw edema in rats as an assay to reflect edema that occurs during the early stages of acute inflammation (Winter et al., 1962; Matsuda and Tanihata, 1992). Generally, the initial edematous response phase that occurs 0-2 h after carrageenan induction, is associated with the exudative stage of inflammation, which is characterized by the release of serotonin, bradykinin and histamine. The late edema phase occurring about 3 h after carrageenan induction when edema reaches its peak volume, is featured by the presence of prostaglandin, which is correlated with migration of leucocytes into the inflamed area (Antonisamy et al., 2011). As expected, treatment of taraxasterol makedly inhibited carrageenan-induced rat paw edema during each phase of edema development.
The anti-inflammatory activity of taraxasterol was also determined by dimethylbenzene-induced mouse ear edema. The dimethylbenzene-induced mouse ear edema is a preliminary and widely used model for screening potential anti-inflammatory drugs (He et al., 2013). Topical application of dimethylbenzene significantly elicited inflammatory response of mice, in this process of inflammation, vasodilatation brings about plasma extravasations and inflammatory mediator releases, which trigger the acute inflammation response (Eddouks et al., 2012). Consistent with the result of carrageenan-induced rat paw edema, taraxasterol markedly inhibited dimethylbenzene-induced mouse ear edema. The inhibitory effect of ear edema indicated that taraxasterol attenuated vasodilatations and plasma extravasations of neurogenic inflammation, which are crucial in controlling the early stage of acute inflammation.
In the inflammatory response, increased vascular permeability is an early and important vascular event (Khor et al., 2009). Acetic acid challenge brings about increases in the level of mediators such as prostaglandin, histamine, and serotonin in peritoneal fluids, which in turn lead to a dilation of the capillary vessels and an increase in vascular permeability (Eddouks et al., 2012). Therfore, the vascular permeability was measured to further indicate the anti-inflammatory activities of taraxasterol, which showed marked decreased effects on acetic acid-induced mouse vascular permeability. This result consolidates that the anti-inflammatory activities of taraxasterol on the acute phase of inflammation are associated with prevention of vasodilation and may be mediated by inhibiting the releases of inflammatory mediators.
Granulomatous inflammation is a focal chronic inflammatory response to tissue injury induced by a poor soluble substance, which is characterized by the proliferation and accumulation of leukocytes (Hirsh and Johnson, 1984). The induction of granuloma by inserting cotton pellet subcutaneously into a rat is widely used to evaluate the effect of anti-inflammatory drugs on the proliferative and transudative phases of chronic inflammation (Swingle and Shideman, 1972; Eddouks et al., 2012). In this study, taraxasterol significantly inhibited cotton pellet-induced rat granuloma formation, it indicates that taraxasterol might inhibit the proliferative phase of the chronic inflammatory process.
The in vivo anti-inflammatory activities of taraxasterol were investigated by using several acute and chronic inflammatory animal models in this study. Our study shows that taraxasterol inhibits inflammatory response, as judged by attenuation of dimethylbenzene-induced ear edema and carrageenan-induced paw edema, inhibition of acetic acid-induced vascular permeability and cotton pellet-induced granuloma formation. It indicates that taraxasterol has anti-inflammatory effects on in vivo animal models, and the results are in agreement with our reported studies in vitro (Liu et al., 2010; Liu et al., 2013; Zhang et al., 2014). In conclusion, based on our previous and present studies, taraxasterol has considerable anti-inflammatory activities in vivo and in vitro, and it may become a potential source of natural anti-inflammatory drugs.
Acknowledgment
This work was supported by the grants from the National Natural Science Foundation of China (No. 31260622 and 31660727), and the Scientific and Technological Development Planning Funding Project of Jilin Province (No. 20160204016NY). All authors have no conflict of interest to declare.
References
- 1.Ahmad V.U, Yasmeen S, Ali Z, Khan M.A, Choudhary M.I, Akhtar F, Miana G.A, Zahid M. Taraxacin a new guaianolide from Taraxacum wallichii. J. Nat. Prod. 2000;63:1010–1011. doi: 10.1021/np990495+. [DOI] [PubMed] [Google Scholar]
- 2.Antonisamy P, Duraipandiyan V, Ignacimuthu S. Anti-inflammatory, analgesic and antipyretic effects of friedelin isolated from Azima tetracantha Lam. in mouse and rat models. J. Pharm. Pharmacol. 2011;63:1070–1077. doi: 10.1111/j.2042-7158.2011.01300.x. [DOI] [PubMed] [Google Scholar]
- 3.Cai C.Y, Chen Y.C, Zhong S.P, Ji B, Wang J.Z, Bai X.T, Shi G.G. Anti-inflammatory activity of N-butanol extract from Ipomoea stolonifera in vivo and in vitro. Plos One. 2014;9:e95931. doi: 10.1371/journal.pone.0095931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eddouks M, Chattopadhyay D, Zeggwagh N.A. Animal models as tools to investigate antidiabetic and anti-inflammatory plants. Evid. Based Complement. Alternat. Med. 2012;2012:14. doi: 10.1155/2012/142087. Article ID 142087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He X.Y, Liu Q.C, Peng W, Huang Y.L, Wu C.J. Bioactivities and serum pharmacochemistry of Qi-Wei-Xiao-Yan-Tang. Pharm. Biol. 2013;51:629–634. doi: 10.3109/13880209.2012.761243. [DOI] [PubMed] [Google Scholar]
- 6.Hirsh B.C, Johnson W.C. Concepts of granulomatous inflammation. Int. J. Dermatol. 1984;23:90–100. doi: 10.1111/j.1365-4362.1984.tb05679.x. [DOI] [PubMed] [Google Scholar]
- 7.Huang M.H, Wang B.S, Chiu C.S, Amagaya S, Hsieh W.T, Huang S.S, Shied P.H, Huangd G.J. Antioxidant, antinociceptive, and anti-inflammatory activities of Xanthii Fructus extract. J. Ethnopharmacol. 2011;135:545–552. doi: 10.1016/j.jep.2011.03.057. [DOI] [PubMed] [Google Scholar]
- 8.Ialenti A, Moncada S, Di Rosa M. Modulation of adjuvant arthritis by endogenous nitric oxide. Br. J. Pharmacol. 1993;110:701–706. doi: 10.1111/j.1476-5381.1993.tb13868.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeon H.J, Kang H.J, Jung H.J, Kang Y.S, Lim C.J, Kim Y.M, Park E.H. Anti-inflammatory activity of Taraxacum officinale. J. Ethnopharmacol. 2008;115:82–88. doi: 10.1016/j.jep.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Kang M, Jung I, Hur J, Kim S.H, Lee J.H, Kang J.Y, Jung K.C, Kim K.S, Yoo M.C, Park D.S, Lee J.D, Cho Y.B. The analgesic and anti-inflammatory effect of WIN-34B, a new herbal formula for osteoarthritis composed of Lonicera japonica Thunb and Anemarrhena asphodeloides BUNGE in vivo. J. Ethnopharmacol. 2010;131:485–496. doi: 10.1016/j.jep.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Khor Y.H, Teoh A.K.Y, Lam S.M, Mo D.C, Weston S, Reid D.W. Increased vascular permeability precedes cellular inflammation control deteriorates. Clin. Exp. Allergy. 2009;39:1659–1667. doi: 10.1111/j.1365-2222.2009.03349.x. [DOI] [PubMed] [Google Scholar]
- 12.Kisiel W, Barszcz B. Further sesquiterpenoids and phenolics from Taraxacum officinale. Fitoterapia. 2000;71:269–273. doi: 10.1016/s0367-326x(99)00158-6. [DOI] [PubMed] [Google Scholar]
- 13.Leu Y.L, Wang Y.L, Huang S.C, Shi L.S. Chemical constituents from roots of Taraxacum formosanum. Chem. Pharma. Bull. 2005;53:853–855. doi: 10.1248/cpb.53.853. [DOI] [PubMed] [Google Scholar]
- 14.Liu J.T, Xiong H.Z, Cheng Y, Cui C.D, Zhang X, Xu L, Zhang X.M. Effects of taraxasterol on ovalbumin-induced allergic asthma in mice. J. Ethnopharmacol. 2013;148:787–793. doi: 10.1016/j.jep.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Liu L.B, Xiong H.Z, Ping J.Q, Ju Y.L, Zhang X.M. Taraxacum officinale protects against lipopolysaccharide-induced acute lung injury in mice. J. Ethnopharmacol. 2010;130:389–394. doi: 10.1016/j.jep.2010.05.029. [DOI] [PubMed] [Google Scholar]
- 16.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 17.Matsuda R, Tanihata S. Suppressive effect of sialic acid on the prostaglandin E2-mediated edema in carrageenin-induced inflammation of rat hind paws. Nihon Yakurigaku Zasshi. 1992;99:363–372. doi: 10.1254/fpj.99.363. [DOI] [PubMed] [Google Scholar]
- 18.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 19.Morris C.J. “Carrageenan-induced paw edema in the rat and mouse”. In: Winyard P.G, Wiloughby D.A, editors. “In Inflammation Protocols”. New Jersey: Humana Press Inc; 2003. pp. 115–121. [DOI] [PubMed] [Google Scholar]
- 20.Nagatomi H, Ando K. Studies on the anti-inflammatory activity and ulcerogenic adverse effect of thiazole derivatives, especially 2-amino-thiazolea-cetic acid derivatives. Arzneimittelforschung. 1984;34:599–603. [PubMed] [Google Scholar]
- 21.Roth S.H. Coming to terms with nonsteroidal anti-inflammatory drug gastropathy. Drugs. 2012;72:873–879. doi: 10.2165/11633740-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 22.Schütz K, Carle R, Schieber A. Taraxacum-a review on its phytochemical and pharmacological profile. J. Ethnopharmacol. 2006;107:313–323. doi: 10.1016/j.jep.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 23.Simon R.A. Prevention and treatment of reactions to NSAIDs. Clin. Rev. Allergy Immunol. 2003;24:189–198. doi: 10.1385/CRIAI:24:2:189. [DOI] [PubMed] [Google Scholar]
- 24.Sweeney B, Vora M, Ulbricht C, Basch E. Evidence-based systematic review of dandelion (Taraxacum officinale) by natural standard research collaboration. J. Herb. Pharmacother. 2005;5:79–93. [PubMed] [Google Scholar]
- 25.Swingle K.F, Shideman F.E. Phases of the inflammatory response to subcutaneous implantation of a cotton pellet and their modification by certain anti-inflammatory agents. J. Pharmacol. Exp. Ther. 1972;183:226–234. [PubMed] [Google Scholar]
- 26.Wang Q.S, Yang L, Cui W.Y, Chen L, Jiang Y.H. Anti-inflammatory and anti-nociceptive activities of methanol extract from aerial part of Phlomis younghubandii Mukerjee. Plos one. 2014;9:e89149. doi: 10.1371/journal.pone.0089149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Winter C.A, Risely E.A, Nuss G.W. Carrageenin-induced edema in hind paw of the rat as an assay for antiinflammatory drugs. Proc. Soc. Exp. Biol. Med. 1962;111:544–577. doi: 10.3181/00379727-111-27849. [DOI] [PubMed] [Google Scholar]
- 28.Xiong H.Z, Cheng Y, Zhang X, Zhang X.M. Effects of taraxasterol on iNOS and COX-2 expression in LPS-induced RAW 264.7 macrophages. J. Ethnopharmacol. 2014;155:753–757. doi: 10.1016/j.jep.2014.06.023. [DOI] [PubMed] [Google Scholar]
- 29.Zhang X.M, Xiong H.Z, Li H.Y, Cheng Y. Protective effect of taraxasterol against LPS-induced endotoxic shock by modulating inflammatory responses in mice. Immunopharmacol. Immunotoxicol. 2014;36:11–16. doi: 10.3109/08923973.2013.861482. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X.M, Xiong H.Z, Liu L.B. Effects of taraxasterol on inflammatory responses in lipopolysaccharide-induced RAW 264.7 macrophages. J. Ethnopharmacol. 2012;141:206–211. doi: 10.1016/j.jep.2012.02.020. [DOI] [PubMed] [Google Scholar]


