Abstract
Rationale
Falls are common among older adults and may be related to depressive symptoms (DS). With advancing age, there is an onset of chronic conditions, sensory impairments, and activity limitations that are associated with falls and with depressive disorders. Prior cross-sectional studies have observed significant associations between DS and subsequent falls as well as between fractures and subsequent clinical depression and DS.
Objective
The directionality of these observed relationship between falls and DS is in need of elaboration given that cross-sectional study designs can yield biased estimates of the DS-falls relationship.
Methods
Using 2006–2010 Health and Retirement Study data, cross-lagged panel structural equation models were used to evaluate associations between falls and DS among 7,233 community-dwelling adults ages ≥65. Structural coefficients between falls and DS (in 2006➔2008, 2008➔2010) were estimated.
Results
A good-fitting model was found: Controlling for baseline (2006) physical functioning, vision, chronic conditions, and social support and neighborhood social cohesion, falls were not associated with subsequent DS, but a 0.5 standard deviation increase in 2006 DS was associated with a 30% increase in fall risk two years later. This DS-falls relationship was no longer significant when use of psychiatric medications, which positively associated with falls, was included in the model.
Conclusion
Using sophisticated methods and a large U.S. sample, we found larger magnitudes of effect in the DS-falls relationship than in prior studies—highlighting the risk of falls for older adults with DS. Medical providers might assess older individuals for DS as well as use of psychotropic medications as part of a broadened falls prevention approach. National guidelines for fall risk assessments as well as quality indicators for fall prevention should include assessment for clinical depression.
Keywords: depression; falls; older adults; structural equation modeling, depressive symptomatology
Clinical depression is relatively uncommon among older U.S. adults—only 4% of those 60 years or older report clinical depression (CDC 2005–2006)—but depressive symptoms (DS) are much more prevalent (Williamson & Schulz, 1992). Among older adults screened from 1998–2004, approximately 15% reported having DS (Federal Interagency Forum, 2008). DS comprise symptoms of unease and somatic complaints including depressed mood that may accompany, but do not necessarily indicate, clinical depression (Berkman et al., 1986). Major life events and reductions in physical capabilities may result in loss of social support and self-esteem that can then lead to DS in older adults.(Aneshensel et al., 1984) Older adults may be victims of accidents including falls that impact physical health and role status (Schoenmakers et al., 2011). Falls may be particularly burdensome because they can reduce the capacity to engage in daily activities (Lazarus & DeLongis, 1983). With advancing age, there is an onset of chronic conditions, sensory impairments, and activity limitations that can lead to falls. Chronic medical conditions such as cardiovascular disease and diabetes are also associated with anxiety and depressive disorders (Aina & Susman, 2006). Given the aging of the U.S. population, especially with the older adult population expected to double in the next forty years (Ortman et al., 2014), an increase in chronic medical conditions and related depressive disorders may be expected.
Falls and DS: Multiple Potential Pathways
Several studies have observed significant associations between DS and falls (Eggermont et al., 2012; Iaboni & Flint, 2012; Spangler et al., 2008; van den Berg et al., 2011) and others have observed a relationship between fractures and both clinical depression and DS (Lenze et al., 2007; Mossey et al., 1990; Scaf-Klomp et al., 2003). However, the directionality of the observed relationship between falls and DS is in need of elaboration. Falls often result in diminished physical capacity, which can result in restricted activities and emotional distress (Peirce et al., 2000). A meta-analysis (Deandrea et al., 2010) and other studies observed significant associations between DS and falls (Eggermont et al., 2012; Iaboni & Flint, 2012; van den Berg et al., 2011).
There are three potential explanations for these findings—or three “pathways” linking DS and falls. One explanation for these findings (“DS-falls pathway”) is that persons with DS have increased fall risk due to factors associated with depression. Some of these factors are fear of falling, fatigue, distractedness, poor nutritional status, or unsteadiness in walking (due to gait changes) (Iaboni & Flint, 2012). A second possibility is that falls lead to DS (“falls-DS pathway”). Also, there are indications that falls are related to anxiety and fear, as well as reductions in self-esteem (Boyd & Stevens, 2009), which may result in increased DS. Activity restriction has been shown to be associated with DS and depression (Painter et al., 2012). However, few studies have explored this potential pathway. Several studies have noted a relationship between fractures and clinical depression and DS (Iaboni & Flint, 2012; Lenze et al., 2007; Mossey et al., 1989; Scaf-Klomp et al., 2003). The third possibility is that there are shared risk factors for DS and falls (“shared pathway”). Several joint risk factors (measured at baseline) have been found to be associated with both future falls and depression (measured 12 months later), such as baseline physical activity, medical problems, and social activities, as well as baseline depression and falls (Biderman et al., 2002).
One study reported increased depression scores after participants may have completed physical rehabilitation from a fall-related injury, suggesting that increased DS may be greater over time as older adults comprehend the extent of their physical limitations and loss of independence following an injury (Scaf-Klomp et al., 2003). However, other research suggests that major depressive disorders risks are greater among those with hip fracture immediately following the injury instead of after a delay (Lenze et al., 2007). Thus, it is possible that we will not observe associations between falls and increased DS measured two years later. Some of the studies examining the association between falls and DS are cross-sectional (Ni Mhaolain et al., 2012; van Haastregt et al., 2008), while others are longitudinal but the settings are outside of the U.S. (Biderman et al., 2002; Ni Mhaolain et al., 2012; Peel et al., 2007; van den Berg et al., 2011), over a decade old (Whooley et al., 1999), or are restricted to a local study sample (Biderman et al., 2002; Eggermont et al., 2012). Of several studies directly examining the falls-DS pathway (Bentler et al., 2009; Lenze et al., 2007; Scaf-Klomp et al., 2003), one is a non-U.S. study, and another is confined to a small, local cohort (Lenze et al., 2007) and thus is not representative of the U.S. community-dwelling older adult population.
Cross-sectional study designs can yield biased estimates of the DS and falls relationship. Second, ignoring the possibility that falls also result in later DS does not account for the various temporal aspects of the relationship. As such, some studies may overstate the strength of the relationship between DS and later falls. Finally, studies on falls and DS have typically controlled for physiological, sociodemographic, and treatment-related factors, but not social support or neighborhood social cohesion (Eggermont et al., 2012; Whooley et al., 1999).
The study uses a sample of community-dwelling older adults, examining the three potential pathways—the DS-falls, falls-DS, and shared pathways. We hypothesize that, after controlling for baseline health status, social support and neighborhood social cohesion: (1) DS will be associated with fall risks two-years later and (2) falls will be associated with DS two years later.
Methods
The current study uses data from the 2006, 2008, and 2010 waves of the Health and Retirement Study (HRS), a national longitudinal study of older Americans primarily conducted by telephone. The HRS includes multiple respondent cohorts (with new cohorts introduced each six years) and aims to include a sample that is representative of the population comprising U.S. citizens who are 50 years or older. The HRS uses a multi-stage area probability sampling design (HRS, 2011). Overall response rates during the 2006–2010 period were approximately 90% among those individuals the HRS attempted to interview (excluding those who asked to be removed from the sample and those who died) (HRS, 2011) (http://hrsonline.isr.umich.edu/). Also included are data from the HRS Participant Lifestyle Questionnaire (PQ), which began its first wave in 2006. A random half of the 2006 sample received an enhanced in-person interview and those completing at least part of that interview received the PQ leave-behind self-administered survey. The response rate for the PQ survey in 2006 was 82%. Data from respondents with survey proxy respondents were not included, as proxies were not asked about depressive symptoms. There were 7,233 older adults in each survey wave (3,276 responded to the 2006 PQ survey), with an average age of 73 (SD: 6); 59% of the sample were female, 76% were white, 14% African-American, 7% Hispanic, and 4% other. In a sensitivity analysis, psychosocial variables (social cohesion and social support) were imputed for missing observations in 2006, 2008, and 2010, and model results were unchanged. Variables used in the analysis are described below; for a more complete description of these variables, see Table A1.
Variables
Dependent variables
We examined two dependent variables. First, we identified whether any fall (non-injurious or injurious) occurred in each year of the study (2006, 2008, 2010) using self-reported data. Second, we measured DS as latent variables in each year of the study using responses to the Center for Epidemiological Studies Depression Scale (CES-D) 8-item short-form (Radloff, 1977). See Table A2 for further details.
Latent predictor variables
Three latent predictor variables—social support, social cohesion, and poor health—were measured in 2006. These factors were included because they may influence both depression and fall risk (Hoffman et al., 2016; Stafford et al., 2011). The social support and social cohesion (psychosocial) variables were not available for all individuals in each of the three survey waves examined, due to the fact that the PQ survey was administered to a random half of eligible respondents in each survey wave (HRS, 2013). For those individuals administered the PQ survey in 2006, psychosocial variables were available in 2006 and 2010 and for those administered the PQ survey in 2008, those variables were available only in 2008. Accordingly, we only measured psychosocial variables in 2006. (Variables taken from the HRS, including those used in the poor health latent factor, were available in all years.)
Observed predictor variables
Additional variables were used to measure health status in 2006. We used an index of chronic illnesses (0–5), which is a count of osteoarthritis, stroke, heart disease, high blood pressure, and diabetes, where presence of a given chronic condition contributes one point to the index. These specific conditions are available in the HRS and have been associated with falls and falls risk (Deandrea et al., 2010). Chronic risk factors pose consistent fall risks due to underlying conditions that affect sensory, cognitive, neurologic, or musculoskeletal functioning (Tinetti, 1989). We also measured self-rated eyesight (1–6 where 1=legally blind and 6=excellent), as eyesight problems are a known risk factor for falls (Deandrea et al., 2010; Tinetti et al., 1988). For use in a sensitivity analysis, we also assessed whether individuals used psychiatric medications (tranquilizers, antidepressants, or pills for nerves).
Study Design
Cross-lagged panel analyses (Kenny & Harackiewicz, 1979) using structural equation modeling (SEM) were employed. This analytic approach makes it possible to simultaneously examine DS and falls as predictors and dependent variables. SEMs have measurement and structural model components. The measurement model involves the relationships between observed measures and underlying latent constructs, while the structural model specifies the structural, or “causal” relationships between the constructs as well as other observed variables in the model (Anderson & Gerbing, 1988).
Figure 1 shows estimates of structural associations between falls and DS with time periods of 1, 2, and 3 (i.e., 2006, 2008, and 2010) and no baseline covariates. DS at time 2 is regressed on falls and DS at time 1. Similarly, falls at time 2 are regressed on DS at time 1. Falls and DS at time 1 are allowed to correlate with one another, and the residuals from falls and DS at time 2 are allowed to correlate. The model evaluates the statistical significance of the structural coefficients for the path from falls at time 1 to DS at time 2 (pathway “2” in Figure 1), falls at time 2 to DS at time 3 (“4”), DS at time 1 to falls at time 2 (“1”), and DS at time 2 to falls at time 3 (“3”).
Figure 1. Illustration of Cross-lagged Panel Analysis with Structural Equation Modeling without Baseline Covariates to Estimate Associations between Depressive Symptoms and Falls over Three Time Periods, 2006–2010.
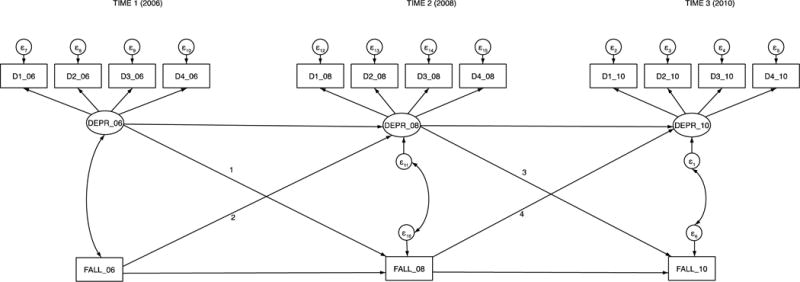
Note: For time 1, indicators D1_06, D2_06, D3_06, and D4_06 are four separate parcels that load onto the 2006 depressive symptoms variable, DEPR_06. For times 2 and 3, the indicators also represent parcels that load onto a depressive symptoms variable (DEPR_08 and DEPR_10). ε is the error associated with each of the indicators of the latent depressive symptoms variables. The numbers 1–4 are the cross-lags of interest.
Model estimation
The modeling approach involved several steps: development of a measurement model, the addition of structural elements, and re-estimation after removing several non-significant pathways (Anderson & Gerbing, 1988; Aneshensel et al., 1984). First, measurement models using data from each of (a) 2006, (b) 2006 and 2008, and (c) 2006, 2008, and 2010, were estimated. Incremental additions of survey wave data were used to ensure appropriate model fit at each stage. These models specified the relationships (i.e., factor loadings) between observed indicators and their underlying latent constructs (e.g., between feeling having restless sleep, feeling alone, or feeling sad and the DS construct) and allowed the underlying constructs to intercorrelate (Anderson & Gerbing, 1988). The constructs in the final measurement model included DS in years 2006, 2008, and 2010 and perceived social support, neighborhood social cohesion, and poor physical functioning at baseline in 2006. After estimating the full measurement model with 2006–2010 data, estimated was a structural model that included the elements of the measurement model as well as other observed variables (i.e., falls in each of 2006, falls in each of 2008, and 2010, and vision and chronic conditions at baseline). This model permitted an assessment of “causal” associations between falls and subsequent DS and DS and subsequent falls.
To assess the study hypotheses regarding relationships between DS and falls, we controlled for potential joint risk factors that might result in both DS and falls (and thus could bias estimates of the falls ➔DS or DS➔falls relationships). We controlled for potential joint risk factors for falls and DS—vision, chronic conditions, physical functioning, social support, and social cohesion at baseline. Correlated errors between observed indicators of latent variables (see below) and between latent variables were also estimated. We also allowed the physical functioning construct to covary with other baseline predictors, including 2006 falls and DS, and to predict outcomes (falls and DS) in each of 2008 and 2010. This was done to ensure that any associations between DS and falls in the 2006➔2008 and 2008➔2010 periods were not due to uncontrolled differences in respondent physical functioning. However, we did not include separate latent physical functioning constructs in 2008 and 2010 because those constructs were highly correlated (from 0.94 to ~1.00) with the baseline physical functioning construct. As with the physical functioning construct, vision and number of chronic conditions were also allowed to covary with other baseline variables and predict 2008 and 2010 outcomes.
The model was modified by removing non-significant parameter estimates, including direct effects of the time 1 measures on the time 2 measures and of the time 2 measures on the time 3 measures (Anderson & Gerbing, 1988). That is, pathways between 2006 falls, 2006 social support, 2006 falls and 2006 neighborhood social cohesion in 2006 were removed. We also removed pathways between 2006 vision and 2008 falls and DS, respectively, and 2006 vision and 2010 falls; between 2006 falls and 2008 DS, 2008 falls and 2010 DS, 2008 DS and 2010 falls, and 2006 chronic conditions and 2010 DS. Model goodness-of-fit was not notably altered after these modifications.
Models were estimated using MPlus version 6.1 using full information maximum likelihood (FIML) (Muthen, 2004). With MPlus, SEMs with dichotomous dependent variables utilize a probit estimation (called a weighted least squares estimation), which produces probit coefficients; continuous outcomes are estimated using OLS regression (Muthén & Muthén, 2011). For the categorical outcomes, estimated coefficients indicate the relationship between the predictor of interest and the assumed underlying latent continuous variable. In addition to the main model, an additional model was estimated that included baseline use of psychiatric medication given that antidepressants and other psychiatric medications have been associated positively with falls and fractures (Iaboni & Flint, 2012).
Assessing goodness-of-fit of models
The fit of the SEM was evaluated using χ2, comparative fit index (CFI), normed fit index (NFI), non-normed fit index or Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA). These different indices account for the fact that χ2 does not adequately assess the model fit with a large or even moderate sample size. Fit is assessed using CFI (>0.93 is acceptable) (Reeve et al., 2007), NFI (>0.90 is acceptable) (Schumacker & Lomax, 2004), TLI (>0.95 is good fit) (Reeve et al., 2007), and RMSEA (<0.06 is good fit) (Reeve et al., 2007).
Assessing the measurement components of the model
Factor loadings in SEM indicate the extent to which the indicator represents the underlying latent variable or factor (Hox & Bechger, 1998). A loading of 0.45–0.54 is fair, 0.55–0.62 is good, 0.63–0.70 is very good, and >0.71 is excellent (Pett et al., 2003).
Estimated correlated errors
Covariances were estimated to account for associations between observed indicators that are not accounted for otherwise in the model. These correlated errors were suggested by SEM modification indices, but also were estimated because such covariances appeared plausible.
Assessing the structural components of the model
The structural components of the SEM were estimated next, following the measurement model estimation. To more easily interpret the probit coefficients for the dichotomous dependent variable, predicted probabilities were computed. To do so, the predicted probabilities of a fall at the mean estimated DS level (zero on the latent variable scale) were computed for DS in 2006 (Muthén, 2008). See Appendix C. Next, the predicted probabilities of a fall at 1 SD above or below the mean DS level were computed. A change of 1 SD is large (Cohen, 1992), so we also computed the change in probabilities associated with a change of 0.5 SD (medium).
The study was conducted at the UCLA Fielding School of Public Health and IRB approval was provided by the UCLA Office of Human Protection Research.
Results
Unadjusted Results
At baseline, approximately one in three respondents experienced a fall within the past two years. The average CES-D summed score was 1.3 (SD = 1.8) on a scale of 0–8. Average scores of neighborhood social cohesion were 5.6 (SD = 1.3) on a scale of 1–7. Average scores of positive social support were 3.2 (SD = 0.5) on a scale of 1–4 (where higher scores indicated more positive support) and average scores of negative social support were 3.4 (SD = 0.4) on a scale of 1–4 (where higher scores indicated less negative support). Respondents reported having a mean of 0.2 ADLs (SD = 0.6), 0.1 IADLs (SD = 0.1), and 3.9 functional limitations (SD = 2.9), a score of 2.8 (SD=1.0) on a vision scale of 1–6, and 2.0 (SD = 1.2) chronic conditions on a scale of 0–6 (Table A2).
Goodness-of-Fit Indices
Figure 1 displays the model, which had acceptable fit, with a CFI of 0.93, NFI of 0.92, TLI of 0.92, and RMSEA of 0.03.
Measurement Component Output
All loadings of the indicator variables on the latent variables were statistically significant (See Appendix B, Table B1). Standardized loadings for most observed indicators for latent variables were ≥0.55, which indicates ≥30% of the shared variance with the factor. Each of the four neighborhood social cohesion indicators had loadings of ≥0.71 (≥50% of the shared variance with the factor). For the social support latent factor, two of the four indicators had loadings that were ≥0.63 (≥40% of the shared variance with the factor).
Structural Component Output
Table 1 provides the shows the correlations between the variables and Table 2 provides the standardized regression coefficients and standard errors.
Table 1.
Standardized Latent Variable Correlations for Trimmed Falls and Depressive Symptoms (DS), 2006–10 (n=7,233)
| Dependent Variable | Predictor Variable
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Social Support |
Social Cohesion |
Vision | Chronic Conditions |
Poor Functioning |
2006 Fall |
2006 DS |
2008 Fall |
2008 DS |
2010 Fall |
2010 DS |
|
| Social Support | 1.00 | ||||||||||
| Social Cohesion | 0.38 | 1.00 | |||||||||
| Vision | −0.12 | −0.10 | 1.00 | ||||||||
| Chronic Conditions | −0.10 | −0.11 | 0.16 | 1.00 | |||||||
| Poor Health | −0.22 | −0.18 | 0.33 | 0.37 | 1.00 | ||||||
| 2006 Fall | −0.05 | −0.06 | 0.07 | 0.13 | 0.28 | 1.00 | |||||
| 2006 DS | −0.41 | −0.28 | 0.27 | 0.21 | 0.56 | 0.17 | 1.00 | ||||
| 2008 Fall | −0.07 | −0.07 | 0.09 | 0.17 | 0.28 | 0.41 | 0.20 | 1.00 | |||
| 2008 DS | −0.32 | −0.23 | 0.24 | 0.20 | 0.53 | 0.16 | 0.65 | 0.24 | 1.00 | ||
| 2010 Fall | −0.07 | −0.06 | 0.10 | 0.10 | 0.30 | 0.25 | 0.23 | 0.53 | 0.23 | 1.00 | |
| 2010 DS | −0.26 | −0.19 | 0.25 | 0.19 | 0.50 | 0.15 | 0.65 | 0.21 | 0.79 | 0.24 | 1.00 |
Note: All associations reach significance at p<0.05.
Table 2.
Standardized Regression Coefficients (and Standard Errors) for Trimmed Falls and Depressive Symptoms (DS), 2006–2010 (n=7,233)
| Dependent Variable | Predictor Variable
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Social Support |
Social Cohesion |
Vision | Chronic Conditions |
Poor Functioning |
2006 Fall |
2006 DS |
2008 Fall |
2008 DS |
2010 Fall |
2010 DS |
|
| Social Support | |||||||||||
| Social Cohesion | 0.38 (0.02) |
||||||||||
| Vision | −0.12 (0.02) |
−0.10 (0.02) |
|||||||||
| Chronic Conditions | −0.11 (0.02) |
−0.11 (0.02) |
0.16 (0.01) |
||||||||
| Poor Functioning | −0.23 (0.03) |
−0.23 (0.02) |
0.33 (0.01) |
0.37 (0.01) |
|||||||
| 2006 Fall | −0.05 (0.02) |
−0.06 (0.02) |
0.07 (0.01) |
0.13 (0.01) |
0.28 (0.01) |
||||||
| 2006 DS | −0.40 (0.02) |
−0.28 (0.02) |
0.27 (0.01) |
0.21 (0.01) |
0.56 (0.01) |
0.17 (0.01) |
|||||
| 2008 Fall | 0.06 (0.02) |
0.12 (0.02) |
0.36 (0.01) |
0.06 (0.02) |
|||||||
| 2008 DS | 0.12 (0.02) |
0.74 (0.02) |
0.11 (0.03) |
||||||||
| 2010 Fall | 0.05 (0.02) |
0.15 (0.02) |
0.48 (0.02) |
||||||||
| 2010 DS | 0.05 (0.01) |
0.10 (0.02) |
0.72 (0.02) |
0.12 (0.03) |
|||||||
Note: All associations reach significance at p<0.05.
Associations between Control Variables at Baseline and with Subsequent Outcome Variables
As shown in Table 2, at baseline (in 2006), social support was positively associated with neighborhood social cohesion and both of these variables were associated negatively with poor physical functioning (as noted earlier, higher scores indicated poorer functioning). Poorer physical functioning at baseline was positively associated with baseline falls and DS. Other baseline health variables (vision and number of chronic conditions) were also positively associated with falls and DS at baseline. Better social support and neighborhood social cohesion at baseline were associated with fewer baseline DS, and poor physical functioning was associated with greater baseline DS. 2006 falls were significantly positively associated with 2008 falls (β = 0.36, SE = 0.01) and 2008 falls were significantly positively associated with 2010 falls (β = 0.48, SE = 0.02). Similarly, 2006 DS were strongly associated with 2008 DS (β = 0.74, SE = 0.02) and 2008 DS were associated with 2010 DS (β = 0.72, SE = 0.02).
The Association of DS with Subsequent Falls
In terms of the “cross-lags,” DS were associated significantly with subsequent fall risk in one of the cross-wave time periods assessed. The probit coefficient for the 2006–2008 cross-wave time period was significant (β = 0.06, SE = 0.02); the coefficient for the 2008–2010 time period was not significant. In terms of predicted probabilities, the risk of a 2008 fall at the mean 2006 DS level was 30% (Appendix C). At 0.5 SD below the mean, the risk was 21% while at 0.5 SD above the mean, the risk was 39% (Figure 2). Thus, a 0.5 SD increase in DS above the mean was associated with about a [(39 − 30)/30] 30% increase in fall risk.
Figure 2.
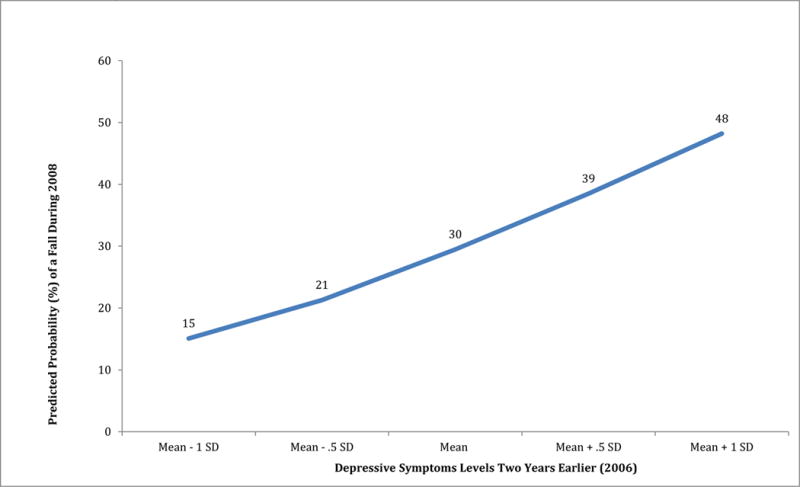
Predicted Probabilities of Falls (Assessed in Survey Wave 2008) at Different Depressive Symptoms Levels (Assessed in Nearest Prior Survey Wave, 2006).
The Association of Falls with Subsequent DS
However, falls were not associated with subsequent DS in either cross-wave time period. Adjusting for baseline characteristics, regression coefficients for 2006➔2008 and 2008➔2010 associations of falls with DS were non-significant and were not included in the final model.
Model results were changed when psychiatric medication use at baseline was included. In that model, 2006 medication use was positively associated with each of 2008 (β = 0.04, SE = 0.02) and 2010 (β = 0.08, SE = 0.01) falls and the 2006 DS➔2008 fall structural relationship became non-significant (β = 0.04, SE = 0.02, p=0.07), suggesting that the impact of 2006 DS on 2008 falls may be mediated, at least in part, through psychotropic medication use.
Discussion
This study of falls and depressive symptomatology (DS) among community-dwelling older adults had several notable findings. First, contrary to the first study hypothesis, falls were not associated with later increases in DS. The present study’s results conflict with findings from a study examining older adults experiencing falls, in which depression did not increase in the five months following the fall but gradually increased between five months and one year (Scaf-Klomp et al., 2003). There are several potential explanations for this finding. Continuity theory suggests that, because individuals can maintain their feelings of self-worth after a major life event, falls may not lead to lasting distress (Kim & Moen, 2002). Individuals may have personal resources (such as self-mastery, or the ability to resolve stress) or economic resources that enable them to recover from difficult life events (Ong et al., 2006). This suggests that future work might examine the falls➔DS relationship using models stratified by socioeconomic status. A second, related explanation is that older individuals can recover from falls through rehabilitation. An older faller may experience several months of social isolation or a reduction in interactions with others as well as less physical activity; yet, the individual may return to full activity later. A temporary, measurable reduction in DS or an increase in DS may follow a fall, but these DS may be reversed over time. By measuring outcomes in two-year increments, the study is incapable of observing such temporary increases in DS. Another potential explanation for this finding has to do with differential dropout of participants. Comparatively higher dropout among depressed compared to non-depressed individuals (which was observed in the study sample, as 32% of depressed compared to 22% of non-depressed individuals in 2006 dropped out of the survey by 2010) could attenuate the association between falls and subsequent DS. However, in a sensitivity analysis we controlled for variables that were associated with dropout (age, gender, and educational level) and obtained nearly identical results. Assuming the estimates are unbiased, this non-association is perhaps an encouraging finding, suggesting that older adults are resilient and able to cope with a fall occurrence.
Further, in support of our hypothesis, greater DS was associated with short-term fall risks in one of the cross-wave time periods examined. For a 0.5 SD increase in DS, future fall risk increased by 30%. Additionally, we observed contemporaneous, cross-sectional associations (significant covariances) between falls and DS in each wave, even after accounting for the DS-fall association. These associations represent a bi-directional relationship between the two outcomes outside of any direct effect indicated by the significant cross-lagged association and other covariates that were controlled for in the model. Given earlier findings, it is unsurprising that there is a significant relationship between DS and falls over time. Fall risk is associated with physical health decline and problems with cognitive functioning, which may reflect executive functioning difficulty (Marks, 2011). This is, in turn, associated with depressive symptoms (Burt et al., 1995). Executive functioning can impact the ability to dual task and adequately process information while walking and talking at the same time, resulting in gait and balance problems that cause falls or affect the ability to quickly recover from a slip or trip incident. Depressed individuals may also have less energy and focus when performing tasks and so are likelier to fall compared to other individuals (Anstey et al., 2008). Moreover, individuals who fear falling may also be depressed (Murphy et al., 2002; Painter et al., 2012)—nearly four in ten hospitalized fallers afraid of falling also had depressive disorder compared to four percent of those not afraid of falling (Iaboni & Flint, 2012)—with fear of falling also putting them at greater risk for falls (Boyd & Stevens, 2009).
Notably, however, inclusion of baseline use of psychiatric medications resulted in a non-significant relationship between DS and subsequent fall risk. Thus, it may be that part of the explanation for the observed DS-falls relationship is that those using psychiatric medications have greater DS, which explains why failure to account for such medication use results in a significant finding. Antidepressants may have effects on blood pressure, movement disorders, cardiac changes, sedation, and drug interactions—all of which can increase fall risk (Iaboni & Flint, 2012). To further explore this, we reexamined the data and observed that in 2006 the average CES-D score (higher score representing more DS) for those using such medications in our sample was 3 compared to 1 for those not using medications. Thus, while prior studies found a significant relationship (Iaboni & Flint, 2012; Kerse et al., 2008; Kvelde et al., 2013), these findings suggest that psychotropic medication use mediates the DS➔falls relationship. Further study of this potentially mediated relationship is warranted using this study’s SEM approach.
Limitations
Though this study’s models controlled to an extent for reverse causality between DS and falls, it may still have overstated DS➔falls risk in the main model. The model did not include social support, neighborhood social cohesion, and physical and emotional health in years 2008 and 2010. However, sensitivity analyses with imputed scores for the psychosocial variables showed no changes to our results. For the three physical functioning latent factors, the correlations across years were nearly 1, suggesting on average little change in functioning. Other research using cross-lagged associations has previously observed strong correlations in physical health over time within individuals (Hays et al., 1994). Because of this, we used 2006 physical functioning as a predictor of 2008 and 2010 falls and DS. When we did not use baseline physical functioning as a predictor of 2008 and 2010 outcomes, the magnitude of the DS-falls relationship was much greater.
All in all, we were able to control for a number of known and/or potential predictors for falls and DS (physical functioning, chronic conditions, social support). Also, unlike prior examinations, this study was able to assess multiple associations simultaneously and thus provides perhaps less biased evidence for a DS-falls relationship. It is possible that unmeasured variables could jointly affect falls and DS and thus bias our estimates. However, associations between unmeasured joint factors at baseline and DS and falls in subsequent survey waves are captured in the covariances (pathways between DS and falls in 2008 and 2010 with the double-headed arrows in Figure 1) in the model.
Another limitation is that we were unable to control for certain shared risks of falls and DS. This includes executive functioning, which allows individuals to cognitively process information while performing other tasks simultaneously and declines as adults age (Wright et al., 2011). This decline could potentially result in greater fall risk. Depression and cognitive status are both associated with poor executive function (Wright et al., 2011). To an extent, these factors might be controlled for with our study design given that we controlled for baseline physical functioning (which would be affected by executive function) as well as baseline DS and falls (which would reflect executive functioning and bone mineral density). Future work may further examine whether these factors are specifically pertinent for the DS➔falls relationship. Finally, self-reporting of sensitive topics is subject to bias, which could result in potential bias in model estimates—which could be a source for future inquiry for researchers examining this topic.
Although our results were similar to those of some of the earlier studies in terms of sign and significance, by using more sophisticated methods and a large U.S. sample, we were able to find larger magnitudes of effect. A significant relationship also appeared in a systematic review of 17 studies examining the relationship between depression and subsequent falls (pooled OR = 1.63) (Deandrea et al., 2010). A more recent systematic review and meta-analysis of 14 studies examining the relationship between DS and falls found that DS were a significant predictor of falls (pooled OR = 1.46). Those studies used several different scales to measure DS (Kvelde et al., 2013). One study observed that a 1-point increase in the 20-item CES-D was associated with a 3% increase in fall risk (Anstey et al., 2008). The SD for that study was ~6 points. Thus, a 0.5-SD (3-point) change would be associated with an approximate 9% increase in risk, whereas the present study observed a much larger risk increase (30%). This study estimated associations of large magnitude for the DS-falls relationships over time. While it did not estimate separate models for injurious and non-injurious falls—which potentially have different etiologies and thus distinct relationships with DS—the odds of a fall and for a fracture were similar for those with compared to those without depression across earlier studies (Kvelde et al., 2013; Spangler et al., 2008).
This study also highlights the risk of falls for older adults with DS. Greater DS were associated with higher fall risk and there was additional contemporaneous covariance unexplained by this direct DS-falls pathway. Additionally, a novel and interesting finding is that this relationship may be attributable to the use of psychotropic medications by older individuals with relatively high DS. No prior work has explored these relationships using SEM. Thus, these findings confirm the importance of psychotropic medications to the risk of falls (Iaboni & Flint, 2012; Kerse et al., 2008). However, they also imply that DS (or depression) alone may not be a primary factor for falls, as suggested in earlier studies (Cesari et al., 2002; Whooley et al., 1999). Still, given that such medications are typically taken by individuals who experience DS, a focus on individuals with DS remains important.
These findings have implications for falls assessments for older adults. The American Geriatrics Society’s (AGS) recommendations for falls assessments include questions about whether an older individual has fallen in the past year or whether the individual had problems with walking or balance (American Geriatrics Society, 2014), but no clinical depression assessment. Similarly, quality indicators for falls and mobility problems were developed as part of the Assessing Care of Vulnerable Elders (ACOVE) project, but those fall/mobility indicators do not address depression.
Accordingly, there may be untreated risks for individuals with DS. First, older adults with psychological distress are less likely to see providers compared to younger adults (Pratt et al., 2007). Without a medical visit, older individuals may not be screened for falls risk. Second, older individuals may not admit to having fallen or having unsteady walking and thus may not receive a falls assessment per professional guidelines. Qualitative studies of older individuals indicate that characteristics associated with fall risk may be considered shameful or embarrassing (Ballinger & Clemson, 2006). This may be particularly true of depressed individuals. Third, individuals with DS may be apathetic about engaging in activities that improve their health. Even older individuals who do receive referrals to exercise programs or other falls interventions may not participate, due to lack of social support or lack of education or lack of involvement in decision-making about the interventions (Stevens et al., 2010). Individuals may not participate in exercise programs, for instance, due to concerns about medical problems, pain, fear of injury, or lack of interest; this may be particularly true of depressed older individuals (Devereux-Fitzgerald et al., 2016; Taylor & Pescatello, 2016).
Given these concerns, medical providers might assess individuals for DS as part of a broader falls prevention approach (Anstey et al., 2008) and providers might also assess patients’ use of psychotropic medications that can result in heightened fall risk (Iaboni & Flint, 2012). If older adults present evidence of DS, the provider could initiate a falls risk evaluation. This would require a shift in the current professional society recommendations. Older individuals, in consultation with family, friends, and their providers, might also consider treatment for DS as part of a broader falls prevention strategy. Also, given that psychotropic medication use mediates the DS-fall pathway, further study of the pharmacology of antidepressants in older adults—to identify those medications with the fewest side effects—may also be warranted. These steps could contribute to a public health approach to address costly and debilitating falls among the growing, community-dwelling older adult population.
Supplementary Material
Research Highlights.
We evaluated bi-directional associations between falls and depressive symptoms
Depressive symptoms were associated with increased fall risk
Fall risk was not associated with increased depressive symptoms
Psychiatric medications mediated the depressive symptoms—falls association
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Geoffrey J. Hoffman, Post-doctoral Research Fellow, Department of Systems, Populations and Leadership, University of Michigan School of Nursing, 400 N. Ingalls Street, Room 4352, Ann Arbor, MI 48109
Ron D. Hays, Professor, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine Professor, Department of Health Policy and Management UCLA Fielding School of Public Health.
Steven P. Wallace, Professor and Chair, Department of Community Health Sciences, UCLA Fielding School of Public Health
Martin Shapiro, Chief, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine Professor, Department of Health Policy and Management UCLA Fielding School of Public Health.
Susan L. Ettner, Professor, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine
References
- Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. Journal of the American Osteopathic Association. 2006;106:S9–S14. [PubMed] [Google Scholar]
- American Geriatrics Society. Prevention of falls in older persons summary of recommendations. American Geriatrics Society; 2014. [Google Scholar]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103:411–423. [Google Scholar]
- Aneshensel CS, Frerichs RR, Huba GJ. Depression and physical illness: A multiwave, nonrecursive causal model. Journal of Health and Social Behavior. 1984;25:350–371. [PubMed] [Google Scholar]
- Anstey KJ, Burns R, von Sanden C, Luszcz MA. Psychological well-being is an independent predictor of falling in an 8-year follow-up of older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2008;63:P249–P257. doi: 10.1093/geronb/63.4.p249. [DOI] [PubMed] [Google Scholar]
- Ballinger C, Clemson L. Older people’s views about community falls prevention: An Australian perspective. British Journal of Occupational Therapy. 2006;69:263–270. [Google Scholar]
- Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. American Journal of Epidemiology. 2009;170:1290–1299. doi: 10.1093/aje/kwp266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Berkman CS, Kasl S, Freeman DH, Jr, Leo L, Ostfeld AM, et al. Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Epidemiology. 1986;124:372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- Biderman A, Cwikel J, Fried AV, Galinsky D. Depression and falls among community dwelling elderly people: A search for common risk factors. Journal of Epidemiology and Community Health. 2002;56:631–636. doi: 10.1136/jech.56.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd R, Stevens JA. Falls and fear of falling: Burden, beliefs and behaviours. Age and Ageing. 2009;38:423–428. doi: 10.1093/ageing/afp053. [DOI] [PubMed] [Google Scholar]
- Burt DB, Zembar MJ, Niederehe G. Depression and memory impairment: A metaanalysis of the association, its pattern, and specificity. Psychological Bulletin. 1995;117:285–305. doi: 10.1037/0033-2909.117.2.285. [DOI] [PubMed] [Google Scholar]
- Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R. Prevalence and risk factors for falls in an older community-dwelling population. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2002;57:M722–726. doi: 10.1093/gerona/57.11.m722. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: A systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- Devereux-Fitzgerald A, Powell R, Dewhurst A, French DP. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Social Science and Medicine. 2016;158:14–23. doi: 10.1016/j.socscimed.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Eggermont LH, Penninx BW, Jones RN, Leveille SG. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: The MOBILIZE Boston Study. Journal of the American Geriatrics Society. 2012;60:230–237. doi: 10.1111/j.1532-5415.2011.03829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Interagency Forum. Older Americans 2008: Key indicators of well-being. Hyattsville, MD: Federal Interagency Forum on Aging-Related Statistics; 2008. [Google Scholar]
- Hays RD, Marshall GN, Wang EY, Sherbourne CD. Four-year cross-lagged associations between physical and mental health in the Medical Outcomes Study. Journal of Consulting and Clinical Psychology. 1994;62:441–449. doi: 10.1037//0022-006x.62.3.441. [DOI] [PubMed] [Google Scholar]
- Hoffman GJ, Hays RD, Wallace SP, Shapiro MF, Yakusheva O, Ettner SL. Receipt of caregiving and fall risk in U.S. community-dwelling older adults. Medical Care. 2016 doi: 10.1097/MLR.0000000000000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox JJ, Bechger TM. An introduction to structural equation modeling. Family Science Review. 1998;11:354–373. [Google Scholar]
- HRS. Sample sizes and response rates. Health and Retirement Study 2011 [Google Scholar]
- HRS. Psychosocial and lifestyle questionnaire, 2006–2010: Documentation report Core Section LB. Health and Retirement Study 2013 [Google Scholar]
- Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: A clinical review. The American Journal of Geriatric Psychiatry. 2012 doi: 10.1016/j.jagp.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Harackiewicz JM. Cross-lagged panel correlation: Practice and promise. Journal of Applied Psychology. 1979;64:372–379. [Google Scholar]
- Kerse N, Flicker L, Pfaff JJ, Draper B, Lautenschlager NT, Sim M, et al. Falls, depression and antidepressants in later life: A large primary care appraisal. PloS One. 2008;3:e2423. doi: 10.1371/journal.pone.0002423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JE, Moen P. Retirement transitions, gender, and psychological well-being: A life-course, ecological model. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2002;57:P212–222. doi: 10.1093/geronb/57.3.p212. [DOI] [PubMed] [Google Scholar]
- Kvelde T, McVeigh C, Toson B, Greenaway M, Lord SR, Delbaere K, et al. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. Journal of the American Geriatrics Society. 2013;61:694–706. doi: 10.1111/jgs.12209. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, DeLongis A. Psychological stress and coping in aging. The American Psychologist. 1983;38:245–254. doi: 10.1037//0003-066x.38.3.245. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Munin MC, Skidmore ER, Dew MA, Rogers JC, Whyte EM, et al. Onset of depression in elderly persons after hip fracture: Implications for prevention and early intervention of late-life depression. Journal of the American Geriatrics Society. 2007;55:81–86. doi: 10.1111/j.1532-5415.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- Marks R. Physical activity and hip fracture disability: A review. Journal of Aging Research. 2011;2011:741918. doi: 10.4061/2011/741918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossey JM, Knott K, Craik R. The effects of persistent depressive symptoms on hip fracture recovery. Journal of Gerontology. 1990;45:M163–168. doi: 10.1093/geronj/45.5.m163. [DOI] [PubMed] [Google Scholar]
- Mossey JM, Mutran E, Knott K, Craik R. Determinants of recovery 12 months after hip fracture: the importance of psychosocial factors. American Journal of Public Health. 1989;79:279–286. doi: 10.2105/ajph.79.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of the American Geriatrics Society. 2002;50:516–520. doi: 10.1046/j.1532-5415.2002.50119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK. Interpretation of coefficient. MPlus 2004 [Google Scholar]
- Muthén LK. Calculating probit probabilities. MPlus 2008 [Google Scholar]
- Muthén LK, Muthén B. Regression analysis, exploratory factor analysis, confirmatory factor analysis. MPlus 2011 [Google Scholar]
- Ni Mhaolain AM, Fan CW, Romero-Ortuno R, Cogan L, Cunningham C, Lawlor B, et al. Depression: A modifiable factor in fearful older fallers transitioning to frailty? International Journal of Geriatric Psychiatry. 2012;27:727–733. doi: 10.1002/gps.2780. [DOI] [PubMed] [Google Scholar]
- Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- Ortman JM, Velkoof VA, Hogan H. Current Population Reports. Washington, DC: United States Census Bureau; 2014. An aging nation: The older population in the United States. [Google Scholar]
- Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. American Journal of Occupational Therapy. 2012;66:169–176. doi: 10.5014/ajot.2012.002535. [DOI] [PubMed] [Google Scholar]
- Peel NM, McClure RJ, Hendrikz JK. Psychosocial factors associated with fall-related hip fractures. Age and Ageing. 2007;36:145–151. doi: 10.1093/ageing/afl167. [DOI] [PubMed] [Google Scholar]
- Peirce RS, Frone MR, Russell M, Cooper ML, Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychology. 2000;19:28–38. doi: 10.1037//0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Pett MA, Lackey NR, Sullivan JJ. Making sense of factor analysis: The use of factor analysis for instrument development in health care research. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Pratt LA, Dey AN, Cohen AJ. Advance Data No. 382. Characteristics of adults with serious psychological distress as measured by the K6 scale: United States, 2001-04. In: Centers for Disease Control and Prevention, editor. Advance Data Reports from the National Health Interview Survey. 2007. pp. 1–18. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, et al. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Medical Care. 2007;45:S22–31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- Scaf-Klomp W, Sanderman R, Ormel J, Kempen GI. Depression in older people after fall-related injuries: A prospective study. Age and Ageing. 2003;32:88–94. doi: 10.1093/ageing/32.1.88. [DOI] [PubMed] [Google Scholar]
- Schoenmakers EC, van Tilburg TG, Fokkema T. Coping with loneliness: What do older adults suggest? Aging & Mental Health. 2011 doi: 10.1080/13607863.2011.630373. [DOI] [PubMed] [Google Scholar]
- Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. New Jersey: Lawrence Erlbaum Associates, Inc., Publishers; 2004. [Google Scholar]
- Spangler L, Scholes D, Brunner RL, Robbins J, Reed SD, Newton KM, et al. Depressive symptoms, bone loss, and fractures in postmenopausal women. Journal of General Internal Medicine. 2008;23:567–574. doi: 10.1007/s11606-008-0525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford M, McMunn A, De Vogli R. Neighborhood social environment and depressive symptoms in mid-life and beyond. Ageing and Society. 2011;31:893–910. [Google Scholar]
- Stevens JA, Noonan RK, Rubenstein LZ. Older adult fall prevention: Perceptions, beliefs, and behaviors. American Journal of Lifestyle Medicine. 2010;4:17. doi: 10.1177/1559827616687263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor BA, Pescatello LS. For the love of it: Affective experiences that may increase physical activity participation among older adults. Social Science and Medicine. 2016;161:61–63. doi: 10.1016/j.socscimed.2016.05.034. [DOI] [PubMed] [Google Scholar]
- Tinetti ME. Prevention of falls among the elderly. New England Journal of Medicine. 1989;348:1055–1059. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- van den Berg M, Verdijk NA, Leusink GL, Wijnands-van Gent CJ, Romeijnders AC, Pop VJ, et al. Depression after low-energy fracture in older women predicts future falls: A prospective observational study. BMC Geriatrics. 2011;11:73. doi: 10.1186/1471-2318-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haastregt JC, Zijlstra GA, van Rossum E, van Eijk JT, Kempen GI. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. The American Journal of Geriatric Psychiatry. 2008;16:186–193. doi: 10.1097/JGP.0b013e3181591c1e. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Kip KE, Cauley JA, Ensrud KE, Nevitt MC, Browner WS. Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Archives of Internal Medicine. 1999;159:484–490. doi: 10.1001/archinte.159.5.484. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Physical illness and symptoms of depression among elderly outpatients. Psychology and Aging. 1992;7:343–351. doi: 10.1037//0882-7974.7.3.343. [DOI] [PubMed] [Google Scholar]
- Wright SL, Kay RE, Avery ET, Giordani B, Alexander NB. The impact of depression on dual tasking among patients with high fall risk. Journal of Geriatric Psychiatry and Neurology. 2011;24:142–150. doi: 10.1177/0891988711409408. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


