Abstract
Nurturing environments within the context of families, schools, and communities all play an important role in enhancing youth’s behavioral choices and health outcomes. The increasing prevalence rates of obesity among youth, especially among low income and ethnic minorities, highlight the need to develop effective and innovative intervention approaches that promote positive supportive environments across different contexts for at risk youth. We propose that the integration of Social Cognitive Theory, Family Systems Theory, and Self-Determination Theory offers a useful framework for understanding how individual, family and social-environmental level factors contribute to the development of nurturing environments. In this paper, we summarize evidence-based randomized controlled trials that integrate positive parenting, motivational, and behavioral skills strategies in different contexts, including primary care, home, community, and school-based settings. Taken together, these studies suggest that youth and parents are most likely to benefit when youth receive individual-level behavioral skills, family-level support and communication, and autonomous motivational support from the broader social environment. Future investigators and health care providers should consider integrating these evidence-based approaches that support the effects of positive social climate-based interventions on promoting healthy eating, physical activity, and weight management in youth.
Significance of Obesity and Chronic Disease in Youth
The United States has the highest costs associated with health care expenditures per capita and is one of the poorest in terms of health-related outcomes compared to other industrialized countries (Woolf & Aron, 2013). More than three-fourths of healthcare expenditures in the United States are spent on chronic disease management, with medical costs linked to obesity being estimated at $147 billion (CDC, 2016). Evidence increasingly suggests that behavioral interventions that target key health behaviors such as physical activity and a healthy diet may be effective at improving health outcomes including obesity and related chronic diseases (Kindig & Stoddart, 2003; Kindig, 2007). In this article we make a case for positive social climate-based interventions that target nurturance and support at multiple levels, including individual-level behavioral skills, family-level support and communication, and autonomous motivational support from the broader social environment.
In recent decades, as chronic conditions such as obesity and other diseases that cluster with obesity (e.g., diabetes, cardiovascular disease) have replaced acute medical conditions as the leading causes of mortality, a focus on prevention and intervening during adolescence has become increasingly important (Plumb, Weinstein, Brawer, & Scott, 2012). Health disparities continue to persist, with healthy lifestyle changes documented in higher income and Caucasian populations, but far less so in lower income and ethnic minority populations (Rehm, Penalvo, Afshin, & Mozaffarian, 2016). These trends are evident in the higher rates of chronic disease shown among ethnic minority as compared to Caucasian youth. For example, approximately 20% of African American and 22% Hispanic youth age 219 years of age are considered obese (≥95th BMI %) as compared to 15% in Caucasian youth (Ogden, Carroll, Kit, & Flegal, 2014). Increases in obesity over the past few decades have contributed also to a higher incidence of youth cardiovascular risk (Expert Panel on Integrated Guidelines for Cardiovascular, Risk Reduction in, Adolescents, National Heart, & Blood, 2011). For example, a 2003–2005 study of 6,000 multi-ethnic high school students found that 3.2% had hypertension, and 15% had prehypertension, with obesity increasing the odds of hypertension fourfold (OR=4.26, 3.12–5.83) (McNiece et al., 2007). These national estimates document the increasing rate of chronic disease risk in lower income and ethnic minority youth who have higher rates of obesity.
The relationship between socio-economic status, racial/ethnic background, and health trajectories is complex. Poverty rates are more than double among African Americans (25.8%) as compared to Caucasian communities (11.6%) (Macartney, Bishaw, & Fontenot, 2013). Both ethnic minorities and those of lower income status have been shown to have fewer improvements in diet over the past 30 years, and in some cases, a worsening of key dietary variables for prevention of obesity and related chronic diseases (Rehm et al., 2016). Impoverished communities have also been shown to lack physical activity resources (Jones et al., 2015), and access to healthy and affordable foods. Lack of access for healthy diet and for physical activity opportunities have also been associated with a greater risk for obesity (Larson, Story, & Nelson, 2009; Sallis & Glanz, 2006). In addition, living in low SES and impoverished communities is related to a higher risk of mortality from chronic disease including obesity (Di Cesare et al., 2013). These findings indicate a strong need for health promotion programs to address lifestyle behaviors, particularly in lower-income and ethnic minority communities, and to move towards integrating multiple sectors and supportive systems to reduce and prevent chronic disease (Baur, Briss, Goodman, & Bowman, 2014; Lushniak, Alley, Ulin, & Graffunder, 2015).
Models of Social Nurturance and Positive Social Environments
The broad impact of negative social conditions on obesity and chronic disease among youth is well documented (Braveman, Egerter, & Williams, 2011; Singh, Siahpush, & Kogan, 2010; Viner et al., 2012). However, causal effects of distinct social-environmental factors on specific health outcomes remains unclear as past research has tended to use cross-sectional designs, and has yielded mixed findings about certain social-environmental factors (An & Sturm, 2012; Lee, 2012). Rates of youth obesity remain high indicating a need for more effective intervention approaches that target specific aspects of the social environment. Biglan and colleagues (Biglan, Flay, Embry, & Sandler, 2012) have proposed that nurturance is a significant factor in affecting the prevalence of health problems in youth. Specifically, Biglan and colleagues emphasize that increasing nurturing environments, such as in schools, families and communities, will improve existing prevention programs and ultimately lead to an increase in overall well-being, as well as chronic diseases and related health problems in youth. In addition, Biglan and Embry (Biglan & Embry, 2013) have argued that evolving cultural practices are needed at a population level to make a more positive impact on the reduction and prevention of health problems in youth. These authors take a look at specific influences on individual behavior to determine ways to improve cultural practices. Namely, they suggest that an increase in nurturing environments and “prosociality” contribute to increased human well-being. In particular Biglan and Embry discuss these concepts in reducing toxic events, implementing positive parenting, and practicing psychological flexibility – all of which relate to promotion of nurturing environments in youth.
Expanding on the work of Biglan and colleagues, we argue that to effectively reduce obesity and related chronic disease conditions in youth it is important to understand the theoretical mechanisms that may reinforce social nurturance and the promotion of positive social environments across differing contexts. Growing evidence suggests that interventions that integrate parenting, motivational, and behavioral constructs are likely to have greater success in producing weight loss outcomes for underserved ethnic minority youth (Barr-Anderson, Adams-Wynn, DiSantis, & Kumanyika, 2013; Kitzman-Ulrich et al., 2010; Kitzman-Ulrich et al., 2011; Kitzmann et al., 2010; Whitlock, Williams, Gold, Smith, & Shipman, 2005; Wilson, 2009; Wilson et al., 2015). In this paper we argue for an ecological perspective that integrates essential elements from Family Systems Theory (FST) (Broderick, 1993), Self-Determination Theory (SDT) (Ryan & Deci, 2000), and Social Cognitive Theory (SCT) (Bandura, 1986, 2004) to better understand how individual-level behavioral skills, family-level support and communication, and autonomous motivational support from the broader social environment facilitate health and well-being among youth. As illustrated in Figure 1, each of these three theories emphasizes the importance of a positive social environment, while simultaneously making distinct predictions about the key constructs and mechanisms that drive behavior change.
Figure 1.
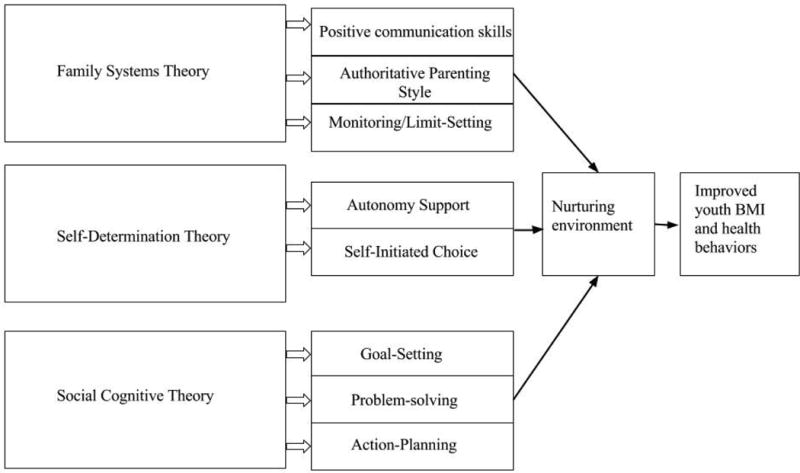
Overview of the constructs targeted by Family Systems Theory, Self-Determination Theory, and Social Cognitive Theory that promote a nurturing environment.
FST proposes that positive parenting skills, including providing social support, practicing positive communication styles, and engaging in monitoring and limit-setting, are critical for promoting shared decision-making, improved parent-child communication, and positive support for youth. According to FST, functional families are able to manage daily life in the context of warm and supportive family interactions (Beavers & Hampson, 2000; Broderick, 1993). Distinct parenting styles have been defined as authoritative (moderate control and monitoring, shared-decision making), authoritarian (high control and monitoring, rigid and inflexible) or as permissive (low control and monitoring) (Baumrind, 1966). Authoritative parenting styles that incorporate skills such as setting appropriate boundaries, providing moderate levels of monitoring, and effective conflict resolution have been associated with more positive health behaviors in youth such as weight management skills, healthy eating and physical activity (Kremers, Brug, de Vries, & Engels, 2003; Radziszewska, Richardson, Dent, & Flay, 1996; Rhee, 2008; Ryan & Deci, 2000; van der Horst et al., 2007; Kitzman-Ulrich et al, 2010b).
In a meta-analytic review by our group (Kitzman-Ulrich et al., 2010a) it was concluded that family-based interventions that target authoritative parenting styles and positive parenting strategies (e.g., monitoring) had the greatest success in both the prevention and treatment of obesity in youth. In another review of general parenting programs, Sleddens and colleagues (2011) found that children who grew up in more authoritative households (e.g., nurturing, autonomy supportive, moderate control) had healthier diets, engaged in more physical activity, and had lower BMIs, than youth growing up in authoritarian, permissive or neglectful households. Taken together, these reviews indicate that parenting strategies that create positive and nurturing environments are related to improvements in weight-related outcomes in youth. Importantly, the majority of past programs that target parenting skills (monitoring and limit setting) have been implemented with middle to upper class children (Epstein, Paluch, Roemmich, & Beecher, 2007; Epstein, Wing, Koeske, & Valoski, 1987; Niemeier, Hektner, & Enger, 2012), with few studies testing whether such programs have comparable effects among underserved and ethnic minority youth (Barr-Anderson et al., 2013). Thus, although a family systems approach provides evidence for the importance of positive parenting skills for improving health outcomes in middle class and non-minority youth, more evidence is needed to demonstrate the effects of positive parenting interventions in high-risk youth.
Consistent with FST, SDT argues for a social contextual approach to promote positive interactions for increasing youth motivation by encouraging youth to have input and choice (autonomy-support) in making healthy lifestyle choices (Ryan & Deci, 2000). SDT postulates that behavior change that is motivated by intrinsic factors, such as viewing a behavior as novel, enjoyable, self-driven, and satisfying, promotes and sustains behavior change. Importantly, past studies have shown that members of one’s broader social environment play a critical role in providing autonomous motivational support, including parents, teachers, health-care providers, and peers (Hagger er al., 2009; Ng et al., 2012; Ntoumanis & Standage, 2009; Standage, Gillison, Ntoumanis & Treasure, 2011). In a recent metaanalysis of 184 interventions, it was shown that an SDT approach was effective for improving a broad range of both physical and mental health outcomes including exercise, weight loss, diet, depression and quality of life (Ng et al., 2012). Providing youth with choices and opportunities to engage in self-initiated behavior change has been shown to increase intrinsic motivation for physical activity, including underserved ethnic minorities in the context of school-based interventions (Ferrer-Caja & Weiss, 2000; Thompson & Wankel, 1980; Wilson et al., 2005; Wilson et al., 2011). Taken together, these studies indicate that positive autonomy-supportive interactions with members of one’s broader social environment play a critical role in facilitating sustained health behavior change.
SCT theory assumes that individual-cognitive factors, environmental events, and behavior are interacting and reciprocal determinants of each other (Bandura, 2004). SCT theory expands on FST and SDT in that it proposes that behavioral strategies, including goal-setting, self-monitoring, and actionplanning, are important elements for building self-efficacy (self-confidence, competence, and selfregulation) for promoting long-term lifestyle changes. According to SCT individuals who adopt challenging goals and are confident (have high self-efficacy) about performing a desired behavior, attain their goals more effectively as compared with individuals with little confidence in their ability to perform the desired behavior. Several large community-based trials have evaluated the effects of SCT interventions on promoting healthy diet and physical activity changes in children in schools and community settings. The Child and Adolescent Trial on Cardiovascular Health trial (Luepker et al., 1996) demonstrated significant effects for a school-based SCT intervention on improved self-efficacy, dietary behaviors, and perceived reinforcement for healthy food choices after 3 years. Similarly, in the Planet Health trial (Gortmaker et al., 1999), a SCT-based health program was implemented in middle school PE classes, which led to a significant reduction in the prevalence of obesity among female students in the intervention group compared to the control group. These community and school-based trials provide evidence that an SCT approach is effective for building individual-level behavioral skills, which, in turn, facilitate long-term health behavior changes in children and adolescents.
By targeting distinct communication, motivational and behavioral factors at the individual, family, and social-environmental levels, integration of these three theories offers an ecological perspective of the different systems and mechanisms that promote sustained health behavior change. Recent studies from our research group have shown that the integration of these three theories is important in promoting healthy lifestyle changes in underserved minority adolescents and their families (Kitzman-Ulrich et al., 2011; St George, Wilson, Schneider, & Alia, 2013; Wilson et al., 2005; Wilson et al., 2011; Wilson et al., 2015). For example, preliminary evidence for the importance of the integration of these three theories comes from a randomized study in which African American adolescents and their caregivers were randomized to a 6-week general health education program or a positive parenting-based and motivational intervention (St George et al., 2013). The intervention integrated essential elements form FST, SDT, and SCT, and targeted positive parenting skills (including monitoring and limit-setting), autonomous support for healthy dietary choices and physical activity, and individual-level behavior skills (including problem-solving and goal-setting). Families who reported more positive communication showed lower adolescent self-reported sedentary behaviors from baseline to post-treatment than those who reported less positive communication or who were in the general health education comparison program. These findings provide initial support for the need to develop health promotion interventions that provide youth with the behavioral skills needed to build self-efficacy, as well as a nurturing environment that supports behavior change.
In summary, we propose that in order to effectively reduce obesity in youth and overall health, especially in underserved ethnic minorities, it is important to understand the theoretical constructs that reinforce social nurturance and the promotion of positive social environments across differing contexts. Below we provide a selective summary of youth-focused randomized controlled trials that integrate elements from FST, SDT, and SCT and target weight loss through lifestyle changes in diet and physical activity. We highlight trials that target at risk youth (defined in terms of BMI, health behaviors, or socioeconomic status) and have been implemented across a variety of contexts, including: schools, primary care, home, and community-based settings. Table 1 provides a summary of key characteristics from these studies. We adapted a scale developed by Miller and colleagues (1995) (see also Sung-Chan, Sung, Zhao & Brownson, 2012) for evaluating the methodological quality of these studies based on study design, treatment integrity, measures, length of follow-up, dose, attrition rate, statistical analyses, and sample size. The methodological quality rating scores are on a 12-point scale. We selected studies with a score of 8 or higher (M = 9.43) (see Table 1 for ratings).
Table 1.
Study characteristics of randomized controlled trials integrating elements from SDT, SCT, and FST
| First Author & Year | MQRS | Location | Design | Participants | Sample Size | Treatment Intensity/Dose | Length of Follow-Up | Attrition Ratio | Theories | Intervention Features | Obesity-Related Results | Motivational and Behavioral Results | Parenting-Related Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resnicow 2015 | 10 | Primary Care | 3 groups: 1) Usual Care; 2) Motivational Interviewing with a primary-care provider; 3) Motivational Interviewing with a primary-care provider plus RD | Parents of overweight youth, ages 2 to 8 | 645 | 4–10 in-person sessions delivered to the parent over 2 years | 2 years | 29% | SDT, SCT | 1) Motivational interviewing with the parent; 2) Behavioral skills training | Youth whose parent received motivational interviewing and behavioral skills training from both a primary care provider and a RD had a significantly lower BMI than the usual care group. | ||
| Davoli 2013 | 8 | Primary Care | 2 groups: 1) Usual Care; 2) Motivational Interviewing | Parents and overweight youth, ages 4–7 | 372 | Five in-person sessions with parent & child over 1 year | 1 year | 5% | SDT, SCT | 1) Motivational interviewing with the parent; 2) Behavioral skills training | Children in the intervention group gained significantly less weight over one year than those in the usual care group. Female children and children whose caregiver had a higher educational level were more responsive to the intervention. | ||
| Taveras 2011 | 9 | Primary Care | 2 groups: 1) Motivational Interviewing intervention; 2) Wait-List Control | Parents of overweight/obese youth, ages 4 to 6 and parents | 475 | Four in-person 25-min visits and three 15 min phone calls delivered over 1 year | 1 year | 6% | SDT, SCT | 1) Motivational interviewing with the parent; 2) Behavioral skills training (specific to TV-watching, fast food consumption, and sweetened beverages intake) | At the conclusion of the first year, there was no significant difference in BMI. In a post hoc analysis, the researchers found a significant change in BMI among girls, but not boys | The intervention group showed a significant decrease in screen time | |
| West 2010 | 9 | Community | 2 groups: 1) Positive parenting lifestyle intervention; 2) Wait-list control group | Parents of overweight/obese youth, ages 4–11 | 101 | 12 week program with nine 90-minute group sessions and three 20-minute telephone sessions | 1 year | 34.60% | FST, SCT | 1) Motivational interviewing; 2) Behavioral skills training for improving nutrition and PA strategies ; 3) Positive parenting strategies; 4) Feedback & problem-solving w/ a counselor | At the conclusion of the intervention, there was a significant reduction in children’s BMI, with additional reductions in BMI after a one year follow-up | At the conclusion of the intervention and at a one-year follow-up, parents reported greater confidence in managing their children’s weight- related problem behavior and less frequent use of inconsistent or coercive parenting strategies. | |
| Østbye 2012 | 10 | Home | 2 groups: 1) home-based weight-loss intervention; 2) Usual care control group | Mothers with children ages 2–5 who were overweight or obese prior to pregnancy | 200 | 8 month program with monthly mailed interactive kits and monthly motivational interviewing sessions delivered by telephone | 1 year | 23% | FST, SDT, SC T | 1) Intervention kits that targeted positive parenting practices; 2) monthly motivational interviewing phone calls with behavioral skills training | At the conclusion of the intervention, there was no significant difference in BMI. | Mothers in the intervention group were less likely to use food as a reward, to feed children in front of the TV., and displayed greater role-modeling, including drinking less sugar-sweetened beverages and greater fruit and vegetable consumption. | |
| Wilson 2011 | 10 | School | 2 groups: 1) afterschool motivational intervention; 2) health education control group | Middle-school students, ages 10–12 | 1422 | 17 weeks | 6 months | 8% | SDT, SCT | 1) Self-initiated choice of physical activity; 2) Motivational and behavioral skills training | At the conclusion of the intervention, there was no significant difference in BMI. | Students in the intervention group showed greater increases in physical activity during the intervention than those who were in the general health education comparison group. | Post-intervention focus groups revealed that competing demands at home and lack of parental involvement were two of the key barriers that prevented students from making sustainable changes in physical activity |
| Lubans 2016 | 10 | School | 2 groups: 1) school-based intervention; 2) Usual care control | Middle-school students, ages 12–14 | 361 | 20 weeks | 18 months | 26.30% | SDT, SCT | 1) In-person physical activity sessions delivered by a teacher trained in Supportive Active, Autonomous, Fair, and Enjoyable teaching principles; 2) lunch-time physical activity leadership sessions run by students; 3) pedometers for physical activity self-monitoring; 4) a web-based smart phone application, 5) newsletters for parents that highlighted strategies for reducing their family’s screen-time | At an 18-month follow-up, there was no significant difference in BMI between the control and intervention groups | The intervention group did display greater autonomous motivation for physical activity and reduced screen-time relative to the control group. |
Note. MQRS = Methodological Quality Rating Scale, range 0–12.
SDT = Self-Determination Theory; SCT = Social-Cognitive Theory; FST = Family-Systems Theory
Summary of Evidence-Based Randomized Controlled Trials
Health-Care Setting Interventions
One example of an intervention that integrated elements from SDT and SCT in a primary care setting is a trial by Resnicow and colleagues (Resnicow et al., 2015), which targeted the parents of children ages 2 to 8 who were overweight or obese. Pediatric offices were randomized to deliver 1 of 3 interventions: usual care; four motivational interviewing sessions delivered by a primary-care provider; or four motivational interviewing sessions delivered by a primary-care provider plus 6 additional sessions delivered by a registered dietician. Integrating elements from SDT, motivational interviewing is a counseling style that promotes autonomous motivation and self-initiated behavioral change through techniques such as shared decision-making and reflective listening. Additionally, integrating elements from SCT, the motivational interviewing sessions included behavioral skills training to facilitate positive changes in diet and physical activity among families, included goal-setting, self-monitoring, and problemsolving. At the a two-year follow-up, youth whose parent received motivational interviewing and behavioral skills training from both a primary-care provider and a RD had a significantly lower BMI than the usual care group. Youth whose parents received motivational interviewing from only a primary-care provider did not differ significantly in BMI from those in the usual care group. These results suggest that families may benefit most from nurturing environments that integrate autonomy support and behavioral skills training from multiple sources.
Another example of a randomized controlled trial that integrated elements from SDT and SCT in a primary-care setting is a trial by Davoli and colleagues (2013). Overweight youth, ages 4 to 7, and their primary caregivers were randomized to receive 5 motivational interviewing sessions delivered by a primary-care provider or to complete a usual care program. The motivational interviewing sessions were delivered over 1 year to both the child and parent, and at each session the child and parent engaged in shared decision-making to develop an achievable dietary and a physical activity goal. At the following session, those goals were assessed for adherence and adjusted as needed through problem solving and the development of new goals and action-plans. Children in the intervention group gained significantly less weight over one year than those in the usual care group. Additionally, the researchers found that female children and children whose caregiver had a higher educational level were more responsive to the intervention. The results of this study are consistent with Resnicow et al.’s (2015) findings above showing that the integration of SDT and SCT in a primary-care setting is an effective approach to weight management for improving parenting interaction to prevent weight gain young children.
In another primary care setting trial, the “High Five for Kids” Study (Taveras et al., 2011), children (ages of 2–6 years old) and their primary caregivers were randomized to a SDT and SCT weight loss program or a usual care program. Ten pediatric facilities participated to test whether an intervention delivered in a primary care setting would be successful in reducing BMI and obesity-related behaviors, such as television watching and fast food consumption among overweight or obese children. Healthcare providers at the pediatric offices providing the intervention were trained in using the Chronic Care Model, which integrates involvement from multiple medical care providers (nurse practitioners, physicians, medical assistants). The intervention specifically integrated motivational interviewing and targeted behavioral skills for promoting weight loss, including decreasing television viewing, and intake of fast food and sugar-sweetened beverages. Parents completed four in-person sessions and three telephone sessions over one year. At the conclusion of the first year, there was no significant difference in BMI; however, the researchers found there was a significant reduction in the amount of time children viewed television in the intervention group relative to the usual care group. Importantly, only half of the families completed 2 of the 6 sessions. In a post-hoc analysis, the researchers found a significant change in BMI among girls, but not boys. This study indicates that although interventions that integrate SDT and SCT have a positive impact on obesity-related health behaviors, future studies may consider further strategies for maximizing participant engagement and intervention dose.
Home- or Community-Based Interventions
Another approach to promoting nurturing environments involves developing interventions that can be implemented in organizations and centers throughout communities. A randomized controlled trial by West and colleagues (2010), for example, incorporated a range of cites for implementing a weight-loss intervention program, including a university psychology clinic, a teaching hospital, and elementary schools. Overweight or obese children, ages 4–11, and their primary caregivers were randomized to a positive parenting lifestyle intervention or a wait-list control group. Parents completed a 12-week intervention that consisted of nine 90-minute group sessions and three 20-min telephone sessions. The sessions integrated a SDT-based, motivational interviewing approach to promote autonomy support and self-initiated behavior change among parents. Additionally, the intervention targeted FST-and SCT-based constructs, including developing behavioral skills for improving nutrition and physical activity, as well as developing positive parenting strategies, such as monitoring and limitsetting. During the phone sessions, parents received feedback on their progress, and engaged in problem solving to develop strategies for overcoming potential barriers. At the end of the 12-week program, there was a significant intervention effect demonstrating decreases in adolescents’ BMI in the treatment but not control condition. Additionally, parents reported greater confidence in managing their children’s weight-related problem behavior and less frequent use of inconsistent or coercive parenting strategies. At a one-year follow-up, all of the post-intervention positive parenting effects were maintained and there were additional positive changes in children’s BMI.
Although community-based studies offer critical opportunities for reaching a wider range of individuals, home-based interventions may offer a more practical solution for hard-to-reach groups. In the “Kids and Adults Now – Defeat Obesity” (KAN-DO) study mother-child dyads (ages 2–5) were randomized to a home-based weight-loss intervention that incorporated monthly mailed interactive kits and monthly telephone motivational interviewing sessions or a usual care program (Østbye et al., 2012). At baseline, 60% of enrolled mothers were obese and 25% of children were overweight or obese. This study targeted postpartum women who were overweight or obese prior to pregnancy and had at least two children; as such women may be more vulnerable to practicing convenience strategies (e.g., feeding their children fast food) and less capable of attending in-person intervention sessions. The intervention integrated FST and SCT by targeting positive parenting skills and practices, including implementing an authoritative parenting style, developing a supportive home environment, and modeling healthy behavior. The monthly telephone sessions integrated motivational interviewing strategies and behavioral skills training, and targeted autonomous motivation, self-efficacy, and problem solving. At a 12-month follow-up, there was no significant difference in BMI between the intervention and control groups. However, there were several differences in parenting practices, including a reduced tendency to use food as a reward and to feed children in front of the television. Mothers in the intervention group displayed greater role modeling, including drinking less sugar-sweetened beverages and increasing consumption of fruits and vegetables. These findings may have been impacted by participant engagement, as participants completed on average about half of the telephone sessions (mean of 4.1 out of 8 sessions). Taken together, the KAN-DO study highlights the challenges of implementing a home-based intervention among hard-to-reach groups, but also provides evidence that parenting practices and changes in the home environment can be improved through home-based interventions.
School-Based Studies
There are an increasing number of school-based trials that have targeted health behaviors related to weight management among youth, including underserved ethnic minority youth. For example, in a randomized controlled trial by our group an afterschool program (involving 24 middle schools) for middle school students was implemented to increase moderate-to-vigorous physical activity (Wilson et al., 2008; Wilson et al., 2009; Wilson et a., 2011). This program targeted middle schools with a large percentage of low income (free or reduced lunch) and ethnic minorities. Schools were randomized to the intervention that integrated elements from SDT and SCT, or a health education after school program. Drawing upon SDT, the content of the intervention program was delivered by staff and teachers, who were trained to allow the students to experience autonomy, belongingness, and social support, related to the after-school program social interactions and physical activities. Additionally, the intervention targeted behavioral strategies from SCT, including group-based goal-setting and strategies for providing and seeking social support, which were intended to increase self-efficacy, behavioral competency, and social-support (from peers and family) for making sustainable changes in physical activity.
Students in the intervention group showed greater increases in physical activity than those who were in the general health education comparison group during the intervention but not beyond the school environment (after the intervention ended; Wilson et al., 2011). A nurturing after-school environment was shown to impact these results. Process evaluation results showed that students in the intervention reported feeling greater respect from the staff and teachers and having more motivation to engage in physical activities as compared to students in the control schools (Wilson et al., 2011). A qualitative follow-up study also showed that the youth, staff, teachers and school leaders felt that the climate at the schools was more positive after implementing the intervention program (Zarrett, Skiles, Wilson, & McClintock, 2012). Furthermore, post-intervention focus groups revealed that competing demands at home and lack of parental involvement were two of the key barriers that prevented students from making sustainable long-term changes in physical activity beyond the school intervention setting (Wilson et al., 2011). These findings highlight the importance of afterschool settings that promote nurturance and provide children with opportunities to play. Furthermore, these findings underscore the need to go beyond individually focused interventions and to integrate support from both teachers and parents.
In another example of a school-based randomized controlled trial targeting obesity prevention, Lubans and colleagues (2016) integrated elements from SDT and SCT and targeted autonomy, competence, and self-efficacy for school-based leisure physical activity. Inactive adolescent boys (ages 12–14) who were at high-risk for becoming overweight were recruited. At baseline, approximately one third of participants were overweight or obese. Adolescents from 14 middle schools were randomized to a 20-week school based intervention or a control group. Teachers were trained to use SAAFE (Supportive Active, Autonomous, Fair, and Enjoyable) teaching principles. Specifically, the intervention included face-to-face physical activity sessions delivered by a teacher (20 × 90 minutes), lunch-time physical activity leadership sessions run by students (6 × 20 minutes), pedometers for physical activity self-monitoring, a web-based smart phone application, and newsletters for parents that highlighted strategies for reducing their family’s screen-time. At an 18-month follow-up, there was no significant difference in BMI between the control and intervention groups. However, the intervention group did display greater autonomous motivation for physical activity and reduced screen-time relative to the control group.
Recommendations for Future Research
In summary, these randomized controlled trials offer some perspective on the different motivational, parenting, and behavioral strategies that can be implemented at the individual, family, and social-environmental levels. Primary care settings, especially those that involve multiple medical health care personnel (Resnicow et al., 2015) appear to be a critical environment for promoting positive behavioral and parenting skills. Relatedly, training teachers and staff to use autonomy supportive strategies offer rich opportunities for developing positive supportive environments for youth (Lubans et al., 2016); however, sustainable behavioral change may require positive support from both parents and teachers (Wilson et al., 2011). Taken together, these studies suggest that youth and parents are likely to benefit when they receive positive support from multiple sources and across different contexts. Whereas previous studies have focused primarily on intervening in one domain, future research is needed to test the feasibility and efficacy of promoting nurturing environments across multiple contexts, including communities, schools, and primary care settings.
The studies summarized in this article provide converging evidence that positive parenting skills, autonomy support, and behavioral skills training play an important role in weight-management among youth. However, such studies tend to be multi-faceted, and, as a result, are not designed to allow for strong tests of the critical components or underlying mechanisms that drive weight loss (for further discussion of this issue see Sheeran, Klein, & Rothman, 2017). Thus, while the selected trials provide general support for the importance of constructs derived from FST, SCT, and SDT (i.e., positive parenting skills, autonomy support, and behavioral skills training), it is difficult to draw empirically-supported conclusions about best practices given the lack of mediational analyses supporting these linkages in intervention trials. However, taken together, these studies suggest that youth and parents are most likely to benefit when youth receive individual-level behavioral skills, family-level support and communication, and autonomous motivational support from the broader social environment. Thus, future investigators and health care providers should consider integrating positive parenting, motivational, and behavioral skills strategies into their treatment approaches for obesity prevention in youth. However, we argue that future research is needed to better understand the mechanisms of change (e.g. see Miller et al., 2011a e.g. see Miller et al., 2011b for examples of potential biological mechanisms) and that more experimental evidence is needed to explain why interventions that promote nurturing environments relate to changes in obesity-related outcomes in youth.
Developing an Evidence-Base to Inform Health Policy
In recent years, numerous expert panels and systematic reviews have sought to provide guidance and research recommendations for obesity prevention (Doak et al. 2006; Flodmark et al 2006; Flynn et al., 2006; Koplan, Liverman, Kraak, & Wisham, 2006), with many researchers advocating for an ecological framework that encompasses social and environmental changes at multiple-levels, including government, industry, communities, schools, and homes (for a review, see Kumanyika et al., 2008). Expanding on this framework, the evidence-based approaches summarized in this paper support the effects of positive social climate-based interventions for promoting healthy eating, physical activity, and weight management in youth, and especially among those at high-risk for obesity. According to the Institute of Medicine, of the 717 bills proposed to prevent childhood obesity between 2003 to 2005, those that had a higher rate of passage pertained to farmer’s markets, walking and biking paths, and safe routes to schools (Koplan et al., 2006). These types of policies provide rich opportunities for considering how changes in the physical environment can be enhanced by positive support from parents, teachers, and healthcare providers. In order to provide programs throughout communities, schools, and healthcare settings that improve positive support, nurturance, and pro-social behaviors, well-designed and rigorous studies need to be conducted that will influence policy makers and stakeholders. Policy makers are dependent upon consistent and available evidence to inform decisions, often weighing costs, and return on investment in their decisions.
Based on the present state of the literature, we propose three key recommendations for developing a stronger evidence-base to inform health policy development. First, cost-effectiveness and cost-benefit analyses need to be increasingly incorporated into intervention evaluation plans to provide clear evidence for policy makers (Brownson, Fielding, & Maylahn, 2009). Second, more research is needed to evaluate the translation of evidence-based programs into delivery settings, including metrics such as costs, return on investment, and health outcomes tied to federal and state funding. To date, much scientific research has focused on internal validity, often not evaluating programs in the context in which they will be delivered. An increasing number of models from the field of implementation science are being used to facilitate understanding of translation and complex behavioral interventions (Colquhoun et al., 2011; Wandersman, Chien, & Katz, 2012). Third, political decision makers will need to be educated on the importance of allocation of resources to support more positive social environments for youth who are at risk for poverty and the development of obesity and associated chronic diseases. It has been estimated that health inequities cost the economy approximately $300 billion dollars per year (LaVeist, Gaskin, & Richard, 2011), and the studies discussed in this review provide approaches to improving nurturing and supportive environments across contexts that could greatly reduce these inequities.
Summary and Conclusions
The increasing prevalence rates of obesity among youth, especially among low income and ethnic minorities, underscore the need to develop effective and innovative intervention approaches and best practices. Consistent with Biglan and colleagues’ (Biglan et al., 2012) emphasis on nurturing environments, we proposed that positive environments within the context of families, schools, communities and health-care settings are critical for enhancing positive changes in youth’s health-related behaviors. In this paper we argued for an ecological perspective that integrates essential elements from FST (Broderick, 1993), SDT (Ryan & Deci, 2000), and SCT (Bandura, 1986, 2004) to better understand how individual-level behavioral skills, family-level support and communication, and autonomous motivational support from the broader social environment facilitate health and well-being among youth. These theories provide guiding frameworks for understanding how a positive social environment is facilitated by positive parenting skills, behavioral skills, and autonomy support. The summary provided here shows evidence-based approaches that support the effects of positive social climate-based interventions for promoting healthy eating, physical activity, and weight management in the youth and provides a foundation to guide policy recommendations to promote nurturing environments in youth.
Acknowledgments
This research was supported in part by the National Institute of Child Health and Human Development (R01HD072153) to Dawn K. Wilson, Ph.D..
Footnotes
Conflicts of Interest The authors declare they have no conflicts of interest.
References
- An R, Sturm R. School and residential neighborhood food environment and diet among California youth. American Journal of Preventive Medicine. 2012;42:129–135. doi: 10.1016/j.amepre.2011.10.012. doi: 1016/j.amepre.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baciu A, Sharfstein JM. Population Health Case Reports: From Clinic to Community. JAMA. 2016;315:2663–2664. doi: 10.1001/jama.2016.4932. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall, Inc; 1986. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Barr-Anderson DJ, Adams-Wynn AW, DiSantis KI, Kumanyika S. Family-focused physical activity, diet and obesity interventions in African-American girls: a systematic review. Obesity Review. 2013;14:29–51. doi: 10.1111/j.1467-789X.2012.01043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014;38:45–52. doi: 10.1016/s0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- Baumrind D. Effects of authoritative control on child behavior. Child Dev. 1966;37:887–907. [Google Scholar]
- Beavers WR, Hampson RB. Succesful families: Assessment and Intervention. New York, NY; W.W. Norton & Co; 2000. [Google Scholar]
- Biglan A, Embry DD. A Framework for Intentional Cultural Change. Joirnal of Contextual Behavioral Science. 2013;2:95–104. doi: 10.1016/j.jcbs.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A, Flay BR, Embry DD, Sandler IN. The critical role of nurturing environments for promoting human well-being. American Psychologist. 2012;67:257–271. doi: 10.1037/a0026796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual Review of Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Broderick C. Understanding family process: Basics of family systems theory. Thousand Oaks, CA: Sage Publications; 1993. [Google Scholar]
- Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annual Review of Public Health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.10013410.1146/annurev.pu.30.031709.100001. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control. Chronic Disease Prevention and Health Promotion. 2016 Retrieved from http://www.cdc.gov/chronicdisease/overview/
- Colquhoun H, Leeman J, Michie S, Lokker C, Bragge P, Hempel S, Grimshaw J. Towards a common terminology: a simplified framework of interventions to promote and integrate evidence into health practices, systems, and policies. Implementation Science. 2014;9:781. doi: 10.1186/1748-5908-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davoli AM, Broccoli S, Bonvicini L, Fabbri A, Ferrari E, D’Angelo S, Giorgi Rossi P. Pediatrician-led motivational interviewing to treat overweight children: an RCT. Pediatrics. 2013;132:e1236–1246. doi: 10.1542/peds.2013-1738. [DOI] [PubMed] [Google Scholar]
- Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, Ezzati M. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–597. doi: 10.1016/s0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- Doak CM, Visscher TLS, Renders CM, Seidell JC. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obesity Reviews. 2006;7:111–136. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychology. 2007;26:381–391. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Valoski A. Long-term effects of family-based treatment of childhood obesity. Journal of Consulting and Clinical Psychology. 1987;55:91–95. doi: 10.1037/0022-006X.55.1.91. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Integrated Guidelines for Cardiovascular, H., Risk Reduction in, C., Adolescents, National Heart, L., & Blood, I. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer-Caja E, Weiss MR. Predictors of intrinsic motivation among adolescent students in physical education. Research Quarterly for Exercise and Sport. 2000;71:267–279. doi: 10.1080/02701367.2000.10608907. [DOI] [PubMed] [Google Scholar]
- Flodmark CE, Marcus C, Britton M. Interventions to prevent obesity in children and adolescents: a systematic literature review. International Journal of Obesity. 2006;30:579–589. doi: 10.1038/sj.ijo.0803290. [DOI] [PubMed] [Google Scholar]
- Flynn MAT, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, Tough SC. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’recommendations. Obesity Reviews. 2006;7:7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Archives of Pediatrics & Adolescent Medicine. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- Hagger M, Chatzisarantis NL, Hein V, Soos I, Karsai I, Lintunen T, Leemans S. Teacher, peer and parent autonomy support in physical education and leisure-time physical activity: A trans-contextual model of motivation in four nations. Psychology and Health. 2009;24:689–711. doi: 10.1080/08870440801956192. [DOI] [PubMed] [Google Scholar]
- Jones SA, Moore LV, Moore K, Zagorski M, Brines SJ, Diez Roux AV, Evenson KR. Disparities in physical activity resource availability in six US regions. Prevative Medicine. 2015;78:17–22. doi: 10.1016/j.ypmed.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D, Stoddart G. What is population health? American Journal of Public Health. 2003;93:380–383. doi: 10.2105/AJPH.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig DA. Understanding population health terminology. Milbank Quarterly. 2007;85:139–161. doi: 10.1111/j.1468-0009.2007.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzman-Ulrich H, Wilson DK, St George SM, Lawman H, Segal M, Fairchild A. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clincal Child and Family Psychology Review. 2010a;13:231–253. doi: 10.1007/s10567-010-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzmann KM, Dalton WT, 3rd, Stanley CM, Beech BM, Reeves TP, Buscemi J, Midgett EL. Lifestyle interventions for youth who are overweight: a meta-analytic review. Health Psychology. 2010b;29:91–101. doi: 10.1037/a0017437. [DOI] [PubMed] [Google Scholar]
- Kitzman-Ulrich H, Wilson DK, St George SM, Segal M, Schneider E, Kugler K. A Preliminary Test of a Motivational and Parenting Weight Loss Program Targeting Low-Income and Minority Adolescents. Child Obesity. 2011;7:379–384. doi: 10.1089/chi.2011.0030. [DOI] [Google Scholar]
- Koplan J, Liverman CT, Kraak VI, Wisham SL. Progress in Preventing Childhood Obesity, How Do We Measure Up? The National Academies Press; Washington, DC: 2006. [Google Scholar]
- Kremers SP, Brug J, de Vries H, Engels RC. Parenting style and adolescent fruit consumption. Appetite. 2003;41:43–50. doi: 10.1016/S0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, Stevens J. Population-based prevention of obesity. Circulation. 2008;118:428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Prevative Medicine. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. International Journal of Health Services. 2011;41:231–238. doi: 10.2190/HS.41.2.c. [DOI] [PubMed] [Google Scholar]
- Lee H. The role of local food availability in explaining obesity risk among young school-aged children. Social Science & Medicine. 2012;74:1193–1203. doi: 10.1016/j.socscimed.2011.12.036. [DOI] [PubMed] [Google Scholar]
- Lubans DR, Smith JJ, Plotnikoff RC, Dally KA, Okely AD, Salmon J, Morgan PJ. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: the ATLAS cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2016;13:92. doi: 10.1186/s12966-016-0420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- Lushniak BD, Alley DE, Ulin B, Graffunder C. The National Prevention Strategy: leveraging multiple sectors to improve population health. American Journal of Public Health. 2015;105:229–231. doi: 10.2105/AJPH.201s4.302257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macartney S, Bishaw A, Fontenot K. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007–2011. American Community Survey Briefs. 2013 Retrieved from: http://www.census.gov/prod/2013pubs/acsbr11-17.pdf.
- McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. Journal of Pediatrics. 2007;150:640–644, 644 e641. doi: 10.1016/j.jpeds.2007.01.052. [DOI] [PubMed] [Google Scholar]
- Miller WR, Brown JM, Simpson TL, et al. What works? A methodological analysis of the alcohol treatment outcome literature. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 2nd. Allyn & Bacon; Needham Heights, MA: 1995. pp. 12–44. [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011a;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, Seeman TE. Pathways to resilience maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychological Science. 2011b;22:1591–1599. doi: 10.1177/0956797611419170.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng JY, Ntoumanis N, Thogersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, Williams GC. Self-Determination Theory Applied to Health Contexts: A Meta-Analysis. Perspectives in Psychological Science. 2012;7:325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- Niemeier BS, Hektner JM, Enger KB. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Prevative Medicine. 2012;55:3–13. doi: 10.1016/j.ypmed.2012.04.021. [DOI] [PubMed] [Google Scholar]
- Ntoumanis N, Standage M. Motivation in physical education classes: A self-determination theory perspective. School Field. 2009;7:194–202. doi: 10.1177/1477878509104324. [DOI] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østbye T, Krause KM, Stroo M, Lovelady CA, Evenson KR, Peterson BL, Zucker NL. Parent-focused change to prevent obesity in preschoolers: results from the KAN-DO study. Preventive Medicine. 2012;55:188–195. doi: 10.1016/j.ypmed.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plumb J, Weinstein LC, Brawer R, Scott K. Community-based partnerships for improving chronic disease management. Primary Care. 2012;39:433–447. doi: 10.1016/j.pop.2012.03.011. [DOI] [PubMed] [Google Scholar]
- Radziszewska B, Richardson JL, Dent CW, Flay BR. Parenting style and adolescent depressive symptoms, smoking, and academic achievement: ethnic, gender, and SES differences. Journal of Behavioral Medicine. 1996;19:289–305. doi: 10.1007/BF01857770. [DOI] [PubMed] [Google Scholar]
- Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999–2012. JAMA. 2016;315:2542–2553. doi: 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, McMaster F, Bocian A, Harris D, Zhou Y, Snetselaar L, Wasserman RC. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135:649–657. doi: 10.1542/peds.2014-1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. Annals of the American Academy of Political and Social Science. 2008;615:12–37. doi: 10.1177/0002716207308400. [DOI] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037/0003-066X.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sallis J, Glanz K. The role of built environments in physical activity, eating, adn obesity in childhood. Child Obesity. 2006;16:89–108. doi: 10.1353/foc.2006.0009. Retrieved from: http://www.jstor.org/stable/3556552. [DOI] [PubMed] [Google Scholar]
- Sheeran P, Klein WM, Rothman AJ. Health behavior change: Moving from observation to intervention. Annual Review of Psychology. 2017;68:573–600. doi: 10.1146/annurev-psych-010416-044007. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Affairs. 2010;29:503–512. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. International Journal of Pediatric Obesity. 2011;6:e12–27. doi: 10.3109/17477166.2011.566339. [DOI] [PubMed] [Google Scholar]
- Standage M, Gillison FB, Ntoumanis N, Treasure DC. Predicting students’ physical activity and health-related well-being: A prospective cross-domain investigation of motivation across school physical education and exercise settings. Journal of Sport and Exercise Psychology. 2012;34:37–60. doi: 10.1123/jsep.34.1.37. [DOI] [PubMed] [Google Scholar]
- St George SM, Wilson DK, Schneider EM, Alia KA. Project SHINE: effects of parent-adolescent communication on sedentary behavior in African American adolescents. Journal of Pediatric Psychology. 2013;38:997–1009. doi: 10.1093/jpepsy/jst027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung-Chan P, Sung YW, Zhao X, Brownson RC. Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obesity Reviews. 2013;14:265–278. doi: 10.1111/obr.12000. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, Gillman MW. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Archives of Pediatric and Adolescescent Medicine. 2011;165:714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson C, Wankel L. The effects of perceived activity choice upon frequency of exercise behavior. Journal of Applied Social Psychology. 1980;10:436–443. doi: 10.1111/j.1559-1816.1980.tb00722.x. [DOI] [Google Scholar]
- van der Horst K, Kremers S, Ferreira I, Singh A, Oenema A, Brug J. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Education Ressearch. 2007;22:295–304. doi: 10.1093/her/cyl080. [DOI] [PubMed] [Google Scholar]
- Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, Currie C. Adolescence and the social determinants of health. The Lancet. 2012;379:1641–1652. doi: 10.1016/S0140-6736(12)60531-5. [DOI] [PubMed] [Google Scholar]
- Wandersman A, Chien VH, Katz J. Toward an Evidence-Based System for Innovation Support for Implementing Innovations with Quality: Tools, Training, Technical Assistance, and Quality Assurance/Quality Improvement. American Journal of Community Psychology. 2012;50:445–459. doi: 10.1007/s10464-012-9509-7. [DOI] [PubMed] [Google Scholar]
- West F, Sanders MR, Cleghorn GJ, Davies PS. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behaviour Research and Therapy. 2010;48:1170–1179. doi: 10.1016/j.brat.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–144. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- Wilson DK. New perspectives on health disparities and obesity interventions in youth. Journal of Pediatric Psychology. 2009;34:231–244. doi: 10.1093/jpepsy/jsn137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Evans AE, Williams J, Mixon G, Sirard JR, Pate R. A preliminary test of a student-centered intervention on increasing physical activity in underserved adolescents. Annals of Behavioral Medicine. 2005;30:119–124. doi: 10.1207/s15324796abm3002_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Friend R, Teasley N, Green S, Reaves IL, Sica DA. Motivational versus social cognitive interventions for promoting fruit and vegetable intake and physical activity in African American adolescents. Annals of Behavioral Medicine. 2002;24:310–319. doi: 10.1207/S15324796ABM2404_07. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Griffin S, Saunders RP, Kitzman-Ulrich H, Meyers DC, Mansard L. Using process evaluation for program improvement in dose, fidelity and reach: the ACT trial experience. International Journal of Behavioral Nutrition and Physical Activity. 2009;6:79. doi: 10.1186/1479-5868-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Kitzman-Ulrich H, Resnicow K, Van Horn ML, George SM, Siceloff ER, Prinz R. An overview of the Families Improving Together (FIT) for weight loss randomized controlled trial in African American families. Contemporary Clinical Trials. 2015;42:145–157. doi: 10.1016/j.cct.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Kitzman-Ulrich H, Williams JE, Saunders R, Griffin S, Pate R, Mixon G. An overview of “The Active by Choice Today” (ACT) trial for increasing physical activity. Contemporary Clinical Trials. 2008;29:21–31. doi: 10.1016/j.cct.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Van Horn ML, Kitzman-Ulrich H, Saunders R, Pate R, Lawman HG, Brown PV. Results of the “Active by Choice Today” (ACT) randomized trial for increasing physical activity in low-income and minority adolescents. Health Psychology. 2011;30:463–471. doi: 10.1037/a0023390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Aron LY. The US health disadvantage relative to other high-income countries: findings from a National Research Council/Institute of Medicine report. JAMA. 2013;309:771–772. doi: 10.1001/jama.2013.91. [DOI] [PubMed] [Google Scholar]
- Zarrett N, Skiles B, Wilson DK, McClintock L. A qualitative study of staff’s perspectives on implementing an after school program promoting youth physical activity. Evaluation and Program Planning. 2012;35:417–426. doi: 10.1016/j.evalprogplan.2011.12.003. [DOI] [PubMed] [Google Scholar]


