Abstract
Background:
Household air pollution is a leading risk factor for respiratory morbidity and mortality in developing countries where biomass fuel is mainly used for cooking.
Materials and Method:
A household cross-sectional survey was conducted in a predominantly rural area of Ghana in 2007 to determine the prevalence of respiratory symptoms and their associated risk factors. Household cooking practices were also assessed as part of the survey.
Results:
Household heads of twelve thousand, three hundred and thirty-three households were interviewed. Fifty-seven percent (7006/12333) of these households had at least one child less than five years of age. The prevalence of symptoms of acute lower respiratory infections (ALRI) was 13.7% (n= 957, 95% CI 12.8 – 15.5%). A majority (77.8%, 95% CI, 77.7 - 78.5%) of households used wood as their primary fuel. Majority of respondents who used wood as their primary fuel obtained them by gathering wood from their neighborhood (95.6%, 9177/9595) and used a 3-stone local stove for cooking (94.9%, 9101/9595). In a randomly selected subset of respondents, females were the persons who mostly gathered firewood from the fields (90.8%, 296/326) and did the cooking (94.8%, 384/406) for the household.
Conclusion:
Symptoms of ALRI reported by caregivers is high in the Kintampo area of Ghana where biomass fuel use is also high. There is the need to initiate interventions that use improved cook stoves and to test the health benefits of such interventions.
Keywords: Acute Lower Respiratory infections, cooking practices, household air pollution, cook-stoves
Introduction
Household air pollution is a leading risk factor for morbidity and mortality in developing countries (Bruce et al., 2000; Lim et al., 2012; Rehfuess et al., 2009; Smith, 2000). Although outdoor air pollution is an important and growing concern in sub-Saharan Africa, it has been estimated that household air pollution (HAP) is actually a more significant environmental health threat (Lim et al., 2012). World-wide, exposure to high levels of HAP is a daily reality for approximately 3 billion users of solid cook-fuels (WHO, 2014). The World Health Organization (WHO) estimates that HAP leads to about 4 million deaths per year and is one of the major global environmental risk factors for reduced life expectancy (WHO, 2014). In Ghana, solid fuels are utilized by a large majority of the population (GSS/GHS/GNPHRL, 2015) and solid fuel use accounts for 2.2 percent of the national burden of disease according to WHO estimates (WHO, 2007). This health burden is largely borne by women and especially children. Among women and children, HAP is associated with the risk of poor birth outcomes (Amegah et al., 2013; Kim et al., 2011; Lakshmi et al., 2013), cardiovascular diseases (Brook, 2007; Miller et al., 2007) and acute lower respiratory infection (ALRI) (Perez-Padilla et al., 2010; Torres-Duque et al., 2008).
In sub-Saharan Africa, the burden of ALRI is high (Walker et al., 2013) and contributes significantly to household expenditure or the health system (Sinha et al., 2012). Since HAP is one of the leading causes of ALRI, there is the need to develop interventions to reduce HAP in sub-Saharan Africa where the use of biomass as the main domestic energy is high (WHO, 2014). Meeting domestic energy while reducing the burden of ALRI may be a challenge and requires relevant local data that quantifies the magnitude of the current health burden and point to optimal solutions.
In 2007, the Kintampo Health Research Centre (KHRC) and Columbia University started a collaboration to develop innovative approaches that will help reduce household air pollution, with the goal of preventing poor health outcomes among rural populations in Ghana. In this paper, we report the results of a large, population-based household survey carried out with the goal of characterizing household cooking practices and respiratory morbidity among infants.
Method
Study area
The study was carried out in the Kintampo North Municipality and Kintampo South District of Ghana in 2007, with a total area of 7162 km2 and a resident population of approximately 140,000 (Owusu-Agyei et al., 2012). The study area is located within the forest-savannah transitional zone in Ghana where community members are predominantly subsistent farmers, with literacy rate of about 40%. Malaria and respiratory infections are among the top ten diseases reported at health facilities(KNMA, 2013). There is significant poor ill-health among new-borns and infants; low birth weight prevalence is about 10% (Asante et al., 2013), neonatal mortality is 32/1000 live-birth, and infant mortality is 64/1000 child years (Kirkwood et al., 2010a). Health care is basic in the study area and the first point of call for an acute illness is a local chemical shop (Asante et al., 2010). This region has been under regular surveillance for births, deaths and migration patterns since 2003 by the Kintampo Health Research Centre (KHRC) under the Kintampo Health and Demographic Surveillance System (KHDSS) (Owusu-Agyei et al., 2012). The KHDSS platform provides the strength of contacting all households in the study area with a high response rate (Owusu-Agyei et al., 2012).
Data Collection
The survey consisted of a short set of questions addressing childhood respiratory infections and household cooking practices that were administered to 12,333 households in the study area using the KHDSS. A more extensive questionnaire was later administered to a randomly selected sub-sample of 421 out of the 12,333 households to determine more details of household cooking practices. A trained fieldworker using a pretested questionnaire interviewed household heads or their representatives. A household was eligible for the survey if the respondent gave consent.
Key variables included household cooking practices, including type of cook-stove used in cooking, type of fuel used for cooking, description of primary cooks and cooking area. We also assessed the presence of respiratory symptoms (cough, blocked nose, runny nose, fast breathing; or difficulty in breathing) among the youngest child in the household in the 2 weeks prior to the interview. Questions were also asked regarding family structure, decision-making and economic circumstances. The time for each interview was about 45 minutes.
Data Management and Analysis
Answered questionnaires were checked for completeness and consistency and sent to the KHRC computer laboratory for double entry into a password-protected database in Microsoft FoxPro version 9.0. Clean dataset was analyzed using Stata version 11.0 (Stata Corp, TX). Simple proportions and means were used to describe categorical and continuous data respectively. Socioeconomic status was defined using household assets such as household architecture or social amenities. Principal component analysis was applied to these variables and the first component was used as described others (Houweling et al., 2003; Howe et al., 2012; Vyas and Kumaranayake, 2006) The scores for the first component of wealth index were further classified into terciles as most poor, less poor and least poor.
Ethical Consideration
Scientific and ethical approvals for the study were obtained from the Kintampo Health Research Centre Scientific Review Committee, the Kintampo Health Research Centre Institution’s Ethics Committee (FWA00011103) and the Institutional Review Board of Columbia University. All participants were individually consented for voluntary participation in the study. The consenting process involved explaining the purpose of the study, confidentiality procedures, risks, benefits and freedom to opt out of the study at any time. Consent was indicated by a signature or thumbprint and a witness was used where respondent was illiterate. Completed survey forms have been kept safely under lock and key in KHRC and could be accessed only by named study investigators.
Results
Twelve thousand, three hundred and thirty-three households were approached and interviewed with 100% response rate. As shown in Table 1, majority of household heads/respondents were males (61.5%) and with no education (54.1%). Most (67%) of households were located in rural areas.
Table 1.
Characteristics of all households contacted (N= 12,333).
| n | % | |
|---|---|---|
| Gender of household head | ||
| Male | 7585 | 61.5 |
| Female | 4339 | 35.2 |
| Missing | 409 | 3.3 |
| Age of Household head in 2007 | ||
| 20-39 | 4605 | 37.3 |
| 40-59 | 4782 | 38.8 |
| 60+ | 2449 | 19.9 |
| Missing | 497 | 4.0 |
| Educational attainment of house head | ||
| No education | 6676 | 54.1 |
| Primary | 1003 | 8.1 |
| Middle/JSS | 2527 | 20.5 |
| Secondary+ | 999 | 8.1 |
| Missing | 1128 | 9.2 |
| Household size | ||
| 1 | 1314 | 10.6 |
| 2-5 | 2597 | 21.1 |
| 6-9 | 1988 | 16.1 |
| 10+ | 6025 | 48.9 |
| Missing | 409 | 3.3 |
| Area of stay | ||
| Rural | 8265 | 67.0 |
| Urban | 4068 | 33.0 |
| Household wealth terciles | ||
| Most poor | 3980 | 32.3 |
| Less poor | 3942 | 32.0 |
| Least poor | 4002 | 32.4 |
| Missing | 409 | 3.3 |
| Cigarettes smoking in the last month | ||
| Yes | 1687 | 13.7 |
| No | 10646 | 86.3 |
| Commercial cooking | ||
| Yes | 1765 | 14.3 |
| No | 10568 | 85.7 |
The prevalence of smoking among household members was 13.7% within the one month period prior to the survey. Approximately fifty-seven percent (7006/12333) of households had at least one child less than five years of age. Fifty-two percent of children were males [Table 2].
Table 2.
Characteristics of households and characteristics of children assessed for respiratory morbidity
| Total | At least one respiratory sign. n (%) | Symptoms of acute lower respiratory infection. n (%) | |||
|---|---|---|---|---|---|
| N=7006 | N=2413 | N=4593 | N=957 | N=6049 | |
| n (%) | Yes n(%) | No n(%) | Yes n(%) | No n(%) | |
| Gender of household head | |||||
| Male | 4624 (66.0) | 1589 (65.8) | 3035 (66.1) | 609 (63.6) | 4015 (66.4) |
| Female | 2176 (31.1) | 748 (31.0) | 1428 (31.1) | 311 (32.5) | 1865 (30.8) |
| Missing | 206 (2.9) | 76 (3.2) | 130 (2.8) | 37 (2.9) | 169 (2.8) |
| Age of Household head at time of survey | |||||
| 20-39 | 3050 (43.5) | 1077 (44.6) | 1973 (43.0) | 439 (45.9) | 2611 (43.2) |
| 40-59 | 2592 (37.0) | 884 (36.6) | 1708 (37.2) | 331 (34.6) | 2261 (37.4) |
| 60+ | 1118 (16.0) | 361 (15.0) | 757 (16.5) | 143 (14.9) | 975 (16.1) |
| Missing | 246 (3.5) | 91 (3.8) | 155 (3.6) | 44 (4.6) | 201 (3.3) |
| Educational attainment of house head | |||||
| No education | 3810 (54.4) | 1301 (53.9) | 2509 (54.6) | 497 (51.9) | 3313 (54.8) |
| Primary | 587 (8.4) | 185 (7.7) | 402 (8.7) | 66 (6.9) | 521 (8.6) |
| Middle/JSSa | 1400 (20.0) | 475 (19.7) | 925 (20.1) | 204 (21.3) | 1196 (19.7) |
| Secondary+ | 523 (7.4) | 197 (8.2) | 326 (7.1) | 90 (9.4) | 433 (7.2) |
| Missing | 686 (9.8) | 255 (10.5) | 431 (9.4) | 100 (10.5) | 586 (9.7) |
| Household size | |||||
| 1 | 620 (8.8) | 255 (10.6) | 365 (7.9) | 113 (11.8) | 507 (8.4) |
| 2-5 | 1395 (19.9) | 490 (20.3) | 905 (19.7) | 216 (22.6) | 1179 (19.5) |
| 6-9 | 1074 (15.3) | 381 (15.8) | 693 (15.1) | 124 (13.0) | 950 (15.7) |
| 10+ | 3711 (53.0) | 1211 (50.2) | 2500 (54.4) | 467 (48.8) | 3244 (53.6) |
| Missing | 206 (2.9) | 76 (3.1) | 130 (2.8) | 37 (3.8) | 169 (2.8) |
| Area of residence | |||||
| Rural | 4855 (69.3) | 1577 (65.3) | 3278 (71.4) | 558 (58.3) | 4289 (71.0) |
| Urban | 2151 (30.7) | 836 (34.7) | 1315 (28.6) | 399 (41.7) | 1752 (29.0) |
| Cigarettes smoking in the last month | |||||
| Yes | 1042 (14.9) | 376 (15.6) | 666 (14.5) | 139 (14.5) | 903 (14.9) |
| No | 5964 (85.1) | 2037 (84.4) | 3927 (85.5) | 818 (85.5) | 5146 (85.1) |
| Household wealth terciles | |||||
| Most poor | 2137 (30.5) | 755 (31.3) | 1382 (30.1) | 283 (29.6) | 1854 (30.7) |
| Less poor | 2381 (34.0) | 824 (34.1) | 1557 (33.9) | 322 (33.6) | 2059 (34.0) |
| Least poor | 2282 (32.6) | 758 (31.4) | 1524 (33.2) | 315 (32.9) | 1967 (32.5) |
| Missing | 206 (2.9) | 76 (3.2) | 130 (2.8) | 37 (3.9) | 169 (2.8) |
| Commercial cooking in household | |||||
| Yes | 1082 (15.4) | 420 (17.4) | 662 (14.4) | 775 (81.0) | 5149 (85.1) |
| No | 5924 (84.6) | 1993 (82.6) | 3931 (85.6) | 182 (19.0) | 900 (14.9) |
| Sex of youngest child | |||||
| Male | 3627 (51.8) | 1300 (53.9) | 2327 (50.7) | 3100 (51.3) | 527 (55.1) |
| Female | 3345 (47.7) | 1102 (45.7) | 2243 (48.8) | 2917 (48.2) | 428 (44.7) |
| Missing | 34 (0.5) | 11 (0.4) | 23 (0.5) | 32 (0.53) | 2 (0.21) |
| Age of child | |||||
| 0 | 1626 (23.2) | 594 (24.6) | 1032 (22.5) | 251 (26.2) | 1375 (22.7) |
| 1 | 1851 (26.4) | 696 (28.8) | 1155 (25.1) | 287 (30.0) | 1564 (25.9) |
| 2 | 1857 (26.5) | 588 (24.4) | 1269 (27.6) | 214 (22.4) | 1643 (27.2) |
| 3 | 841 (12.0) | 281 (11.6) | 560 (12.2) | 98 (10.2) | 743 (12.2) |
| 4 | 831 (11.9) | 254 (10.6) | 577 (12.6) | 107 (11.2) | 724 (12.0) |
| Primary cooking fuel | |||||
| LPG/ Electricity | 16 (0.2) | 8 (0.3) | 8 (0.2) | 4 (0.4) | 12 (0.2) |
| Biomass fuel (Wood/ Charcoal) | 6957 (99.3) | 2390 (99.1) | 4567 (99.4) | 945 (98.8) | 6012 (99.4) |
| Other | 33 (0.5) | 15 (0.6) | 18 (0.4) | 8 (0.8) | 25 (0.4) |
| Primary cooking area | |||||
| Open with no roof and walls | 4071 (58.1) | 1360 (56.3) | 2711 (59.0) | 556 (58.1) | 3515 (58.1) |
| Open with roof only | 433 (6.2) | 154 (6.4) | 279 (6.1) | 62 (6.5) | 371 (6.1) |
| Partially enclosed with walls and roof | 1260 (18.0) | 484 (20.1) | 776 (16.9) | 187 (19.5) | 1073 (17.8) |
| Fully enclosed | 1227 (17.5) | 413 (17.1) | 814 (17.7) | 151 (15.8) | 1076 (17.8) |
| No primary cooking area | 15 (0.2) | 2 (0.1) | 13 (0.3) | 1 (0.1) | 14 (0.2) |
| Stove for burning wood | |||||
| Open mokyiab | 5764 (82.3) | 1975 (81.9) | 3789 (82.5) | 748 (78.2) | 5016 (82.9) |
| Clay mokyiab | 197 (2.8) | 69 (2.9) | 128 (2.8) | 35 (3.7) | 162 (2.7) |
| Metal mokyiab | 131 (1.9) | 23 (0.9) | 108 (2.3) | 10 (1.0) | 121 (2.0) |
| Other | 29 (0.4) | 12 (0.5) | 17 (0.4) | 7 (0.7) | 22 (0.4) |
| Do not use wood | 885 (12.6) | 334 (13.8) | 551 (12.0) | 157 (16.4) | 728 (12.0) |
| Way in obtaining wood | |||||
| Gather from the field only | 1287 (18.4) | 449 (18.6) | 838 (18.3) | 721 (75.3) | 5059 (83.6) |
| Gather from the field and purchase from market | 120 (1.7) | 54 (2.2) | 66 (1.4) | 15 (1.6) | 75 (1.3) |
| Purchase from the market only | 2455 (35.0) | 950 (39.4) | 1505 (32.8) | 63 (6.6) | 190 (3.1) |
| Do not gather wood | 3144 (44.9) | 960 (39.8) | 2184 (47.5) | 158 (16.5) | 725 (12.0) |
JSS - Junior Secondary School
Mokyia - A local stove
Prevalence of at Least One Respiratory Symptom and Potential Risk Factors
At least one respiratory symptom (cough, blocked nose, fast breathing, or chest in drawing) was reported in 34.4% (n=2413, 95% CI 33.3 - 35.5) of children <5 years of age (N=7006). A majority (51.9%) of children with at least one respiratory symptom lived in households with a male head, with those in the rural areas going up to 65.3%. Also 99.3% of male-headed households used biomass fuel (wood or charcoal) as the main primary fuel (Table 2). Blocked nose was the commonest symptom reported (29.6%, 95% CI: 28.4 – 30.6) (Figure 1). Seventeen percent (413/2413) of children who were reported to have had at least one respiratory symptom sought medical treatment.
Figure 1.
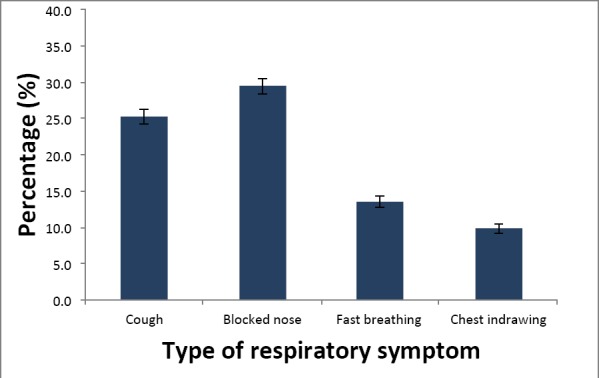
Bar chart of Prevalence of respiratory morbidity among children in the last two weeks prior to the survey (with confidence intervals).
Prevalence of ALRI Symptoms and Potential Risk Factors
The prevalence of ALRI symptoms (cough with fast breathing and/or difficulty in breathing) was 13.7% (n= 957, 95% CI: 12.8–15.5%). A majority of children with ALRI symptoms lived in households with household heads who had no education (51.9%) and also in households that used biomass fuel (98.8%) as the main primary fuel (Table 2).
Cooking Practices
In all households contacted, a majority (77.8%, 95% CI 77.7 - 78.5%) of households used wood as their primary fuel (Table 3). Majority of respondents who used wood as their primary fuel obtained them by gathering wood from their neighborhood (95.6%, 9177/9595) and used a 3-stone local stove for cooking (94.9%, 9101/9595). Charcoal use was less common (Table 3). LPG or electricity use was rare (Table 3). A majority of respondents primarily cooked in open areas with no roofs and walls (56.7%). Partially enclosed areas were the commonest (38.0%) secondary cooking area (Figure 2). None of the cooking practice variables was significantly associated with respiratory symptoms.
Table 3.
Cooking practices among all households N=12,333
| N | % | |
|---|---|---|
| Primary cooking fuel | ||
| LPG/ Electricity | 63 | 0.5 |
| Charcoal | 2364 | 19.2 |
| Wood | 9595 | 77.8 |
| Other | 311 | 2.5 |
| Primary cooking area | ||
| Open with no roof and walls | 6996 | 56.7 |
| Open with roof only | 748 | 6.1 |
| Partially enclosed with walls and roof | 2208 | 17.9 |
| Fully enclosed | 2101 | 17.0 |
| No primary cooking area | 280 | 2.3 |
| Stove for burning wood | ||
| Open mokyia | 9691 | 78.6 |
| Clay mokyia | 319 | 2.6 |
| Metal mokyia | 214 | 1.7 |
| Other | 41 | 0.3 |
| Do not use wood | 2068 | 16.8 |
| Way in obtaining wood* | ||
| Gather | 9660 | 78.3 |
| Gather and purchase | 150 | 1.2 |
| Purchase | 455 | 3.7 |
| Do not use wood | 2068 | 16.8 |
Includes respondents who use wood as their primary or secondary source of fuel.
Figure 2.
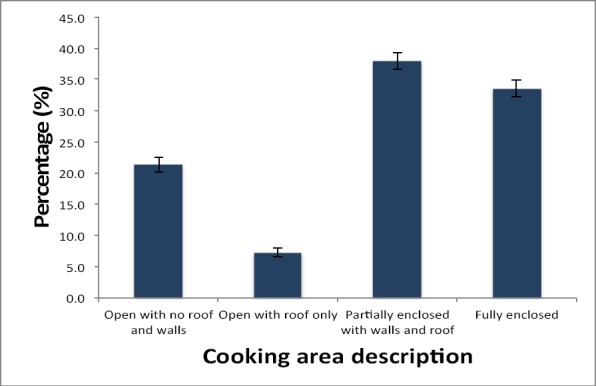
Proportion of secondary cooking areas among all households that had a secondary cooking area (N= 4825). Numerator (n) for each secondary cooking area is as follows: Open with no roof and walls =1027, Open with roof only =348, partially enclosed with walls and roof= 1833, fully enclosed=1617
Legend: Bar chart of the prevalence of respiratory symptoms among children less than five years old (N=7006) in the Kintampo area, 2007. Numerator (n) for each symptom is as follows: cough =1775, blocked nose/runny nose=2070, fast breathing =944, chest in-drawing =692
In a randomly selected subset of respondents, females were the persons who mostly gathered firewood from the fields (90.8%, 296/326) and did the cooking (94.8%, 384/406) for the household; 58.7% (247/421) of households cooked on their farms outside their homes. In the same subset of households, 74% (313/421), 47.7% (201/421), and 93.6% (394/421) of households cooked breakfast, lunch, or supper respectively. The median time for cooking was 2 hours and 20 minutes (range 0 – 5 hours, 30 minutes).
Awareness of Cook-Stoves and Health Risk of Smoke
In the randomly selected subset of households, a majority (92.4%, n=389/421) of respondents were not aware of improved cookstoves. However, most respondents were aware of health hazards associated with smoke. About 97.4% (410/421) were aware that tobacco could lead to health hazard and cook smoke could lead to childhood pneumonia (96.7%, n=407/421) or lung disease in adults (96.4%, n=406/421). Other sources of smoke identified by household members were those from mosquito coils (39.7%, 167/421) as well as from paraffin or kerosene lantern (92.6%, 390/421).
Household Decision-Making and Sources of Information
In all households, fathers/husbands were the primary decision makers for households in health seeking (64.3%, 7924/12,333) or for major item purchases (67.2%, 8286/12,333). Mothers/wives made primary decisions in 25.4% (3135/12,333) of health-seeking in households and 23.1% (2850/12,333) for major items purchases. The local radio was the commonest primary source of agricultural (55.2%) or health (51.4%) information (Table 4). Other sources included agricultural officers or health officers.
Table 4.
Source of information among households (N=12,333)
| Agricultural information | Health information | |||
|---|---|---|---|---|
| Source | N | % | N | % |
| Radio | 6,813 | 55.2 | 6,338 | 51.4 |
| Nearby neighbors | 1,275 | 10.3 | 302 | 2.5 |
| Agricultural officer | 877 | 7.1 | 26 | 0.2 |
| Community elders | 810 | 6.6 | 313 | 2.5 |
| Other | 384 | 3.1 | 80 | 0.7 |
| Other community members | 330 | 2.7 | 210 | 1.7 |
| Health officer | 47 | 0.4 | 4,285 | 34.7 |
| Extended family | 26 | 0.2 | 12 | 0.1 |
| Friend elsewhere | 24.0 | 0.2 | 8 | 0.1 |
| NK | 1,747 | 14.2 | 759 | 6.2 |
Discussion
A survey was conducted in a predominantly rural area of Ghana to determine household respiratory morbidity and cooking practices among young children. The prevalence of at least one respiratory symptom (cough, blocked nose, fast breathing, or chest in drawing) was very high among children who were less than five years of age at the time of the survey. Cough was one of the commonest symptoms reported. The reported cough could be pathological or non-pathological (Bonney et al., 2012). Though it is likely that a proportion of the symptoms reported may not be pathological, the prevalence of runny nose suggests a high probability of an upper respiratory tract infection (URTI). URTI may result from common viruses such as Influenza Sp that sometimes occur as outbreaks but are usually eliminated within a short period (i.e. within periods less than 6 months) (Iskander et al., 2013). It could have been possible an URTI outbreak occurred at the time of this survey, but this was unlikely as there was no report of such an outbreak by health authorities in our surveyed area in the six-month period of our survey. The prevalence of respiratory symptoms determined in this survey is similar to that obtained in other surveys in rural areas of Kenya (Feikin et al., 2011), and in industrialized countries where air pollution is high (Kumar et al., 2007; Ranzi et al., 2014).
The prevalence of ALRI symptoms (13.7%), though lower than that of URTI represents a significant health burden if they truly reflect underlying ALRI prevalence. In studies conducted in southern Ghana, the prevalence of ALRI symptoms assessed by trained community health personnel was <10% (Chinbuah et al., 2013). In our study, ALRI symptoms were reported by mothers or caregivers and not by health professionals or trained community volunteers. It is therefore likely that the prevalence determined in this survey could have been under-estimated since mild to moderate breathlessness or chest in-drawing may go unnoticed by the mother as was found in surveys in other parts of Ghana (Denno et al., 1994) and in Ethiopia (Muhe, 1996).
The use of firewood for cooking was very high in the study area and similar to other rural areas of Ghana and developing countries (Bonjour et al., 2013; GSS/GHS/GNPHRL, 2015). Uncontrolled, unventilated firewood combustion leads to air pollution, which is associated with high disease burden including respiratory diseases (Thacher et al., 2013; Wong et al., 2013). In this survey, no associations were sought between use of firewood and respiratory symptoms. This is due to the fact that few households (0.5%) used clean cook stoves or fuels (electricity or LPG) as their primary cooking fuel and we lacked exposure monitoring at the time of the survey to test for exposure-response among those families using wood for cooking. Respiratory symptoms were higher among children living in urban areas. It is likely that the children living in urban areas are exposed to other risk factors of respiratory signs such as smoke from vehicles.
A majority of households primary cooks were women of childbearing age. We assume that, if pregnant, the foetus of these primary cooks were likely to be exposed to environmental pollutants such as carbon monoxide that may lead to poor health outcomes (Naeher et al., 2000). The GRAPHS study (Jack et al., 2015) currently under way in Ghana is seeking to evaluate the potential impact of use of improved cook-stoves on low birth weight and infant respiratory morbidity and will be able to provide additional data to help explain this assumption being made in the manuscript. Other cohort studies will be required to investigate the potential impact of using improved cook-stoves on other infant health outcomes such as motor and neurodevelopment and infant anthropometry growth.
In many developing sub-Saharan countries, government policies recognize the need to provide improved cook-stoves as means of maintaining trees and plantations to halt climate change (Kgathi and Zhou, 1995). In Ghana, pilot programmes are being implemented by providing free LPG stoves to some rural communities. There is the need to take advantage of such programmes to assess the health benefits of improved cook-stoves on non-communicable diseases such as cardiovascular diseases. In planning such intervention studies, there is the need to consider the social context within which the study will be carried out. In the current study, knowledge of improved cook-stoves is documented to be limited. Community members will therefore need to be educated on the use of the chosen improved cook-stove to ensure compliance through an appropriate medium. Community durbars and community worker discussion of topical issues in the study were found to be the best ways of deploying information. Even though, interventions of this nature may be targeted at women and their children, household decision makers will need to be consulted to ensure acceptance and compliance to the improved cook-stove as majority of households decisions are made by male household heads.
Study Limitation
A cross-sectional survey was conducted and therefore temporal relationship between use of cook-stoves and respiratory symptoms cannot be assessed. Secondly the symptoms such as breathlessness was not counted but was dependent on the subjective observations of the mother or caregiver of the child. Studies will however require counting and observations by a trained health professional or community worker as was used in other studies in Ghana (Kirkwood et al., 2010b) and the RESPIRE study (Smith et al., 2011).
Conclusion
Symptoms of ALRI reported by caregivers are high in the Kintampo area of Ghana where use of biomass fuel use is also high. There is the need to plan interventions to use improved cook-stoves and to test the health benefits of such interventions.
Acknowledgement
The authors are grateful to the staff of Kintampo Health Research Centre and to Columbia University for supporting this study; the community leadership and community members, local political leaders and local government agencies and Ghana Health Service.
The Kintampo Health Research Centre is a member-centre of the INDEPTH Network.
Footnotes
Authors’ contribution KP, DJ, SOA and PK conceived the idea. All authors contributed to the study implementation. KP and EN analyzed the data. KP wrote the first draft of the paper and the final version was reviewed and approved by all authors. SOA, the Director of the Kintampo Health Research Centre and PK, the Director of Columbia Climate and Health Program, Department of Environmental Health Sciences, Mailman School of Public Health reviewed and approved the paper on behalf of the participating institutions.
Competing Interest: All authors declared that they have no competing interest.
References
- 1.Amegah A.K, Damptey O.K, Sarpong G.A, Duah E, Vervoorn D.J, Jaakkola J.J. Malaria infection, poor nutrition and indoor air pollution mediate socioeconomic differences in adverse pregnancy outcomes in Cape Coast Ghana. PLoS One. 2013;8:e69181. doi: 10.1371/journal.pone.0069181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asante K.P, Abokyi L, Zandoh C, Owusu R, Awini E, Sulemana A, Amenga-Etego S, Adda R, Boahen O, Segbaya S, Mahama E, Bart-Plange C, Chandramohan D, Owusu-Agyei S. Community perceptions of malaria and malaria treatment behaviour in a rural district of Ghana: implications for artemisinin combination therapy. BMC Public Health. 2010;10:409. doi: 10.1186/1471-2458-10-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asante K.P, Owusu-Agyei S, Cairns M, Dodoo D, Boamah E.A, Gyasi R, Adjei G, Gyan B, Agyeman-Budu A, Dodoo T, Mahama E, Amoako N, Dosoo D.K, Koram K, Greenwood B, Chandramohan D. Placental malaria and the risk of malaria in infants in a high malaria transmission area in ghana: a prospective cohort study. J Infect Dis. 2013;208:1504–1513. doi: 10.1093/infdis/jit366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonjour S, Adair-Rohani H, Wolf J, Bruce N.G, Mehta S, Pruss-Ustun A, Lahiff M, Rehfuess E.A, Mishra V, Smith K.R. Solid fuel use for household cooking: country and regional estimates for 1980-2010. Environmental health perspectives. 2013;121:784–790. doi: 10.1289/ehp.1205987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonney J.H, Kronmann K.C, Lindan C.P, Asante I.A, Parbie P, Aboagye J, Amankwah J, Odoom J.K, Adjabeng M, Nzussouo N.T, Ahadzie L, Barthel R.V, Cornelius C, Amofah G, Oyofo B, Ampofo W.K. Virological surveillance of influenza-like illness among children in Ghana, 2008-2010. J Infect Dis. 2012;206;(Suppl 1):S108–113. doi: 10.1093/infdis/jis577. [DOI] [PubMed] [Google Scholar]
- 6.Brook R.D. Is air pollution a cause of cardiovascular disease? Updated review and controversies. Reviews on environmental health. 2007;22:115–137. doi: 10.1515/reveh.2007.22.2.115. [DOI] [PubMed] [Google Scholar]
- 7.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull World Health Organ. 2000;78:1078–1092. [PMC free article] [PubMed] [Google Scholar]
- 8.Chinbuah M.A, Abbey M, Kager P.A, Gyapong M, Nonvignon J, Ashitey P, Akpakli J, Appiatse S.A, Kubi D, Gyapong J.O. Assessment of the adherence of community health workers to dosing and referral guidelines for the management of fever in children under 5 years: a study in Dangme West District, Ghana. International health. 2013;5:148–156. doi: 10.1093/inthealth/ihs008. [DOI] [PubMed] [Google Scholar]
- 9.Denno D.M, Bentsi-Enchill A, Mock C.N, Adelson J.W. Maternal knowledge, attitude and practices regarding childhood acute respiratory infections in Kumasi, Ghana. Ann Trop Paediatr. 1994;14:293–301. doi: 10.1080/02724936.1994.11747732. [DOI] [PubMed] [Google Scholar]
- 10.Feikin D.R, Olack B, Bigogo G.M, Audi A, Cosmas L, Aura B, Burke H, Njenga M.K, Williamson J, Breiman R.F. The burden of common infectious disease syndromes at the clinic and household level from population-based surveillance in rural and urban Kenya. PLoS One. 2011;6:e16085. doi: 10.1371/journal.pone.0016085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GSS/GHS/GNPHRL. 2014 Ghana Demographic and Health Survey. Ghana Statistical Service, Ghana Health Service, Ghana National Public Health and Reference Laboratory. 2015 [Google Scholar]
- 12.Houweling T.A, Kunst A.E, Mackenbach J.P. Measuring health inequality among children in developing countries: does the choice of the indicator of economic status matter? International journal for equity in health. 2003;2:8. doi: 10.1186/1475-9276-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howe L.D, Galobardes B, Matijasevich A, Gordon D, Johnston D, Onwujekwe O, Patel R, Webb E.A, Lawlor D.A, Hargreaves J.R. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol. 2012;41:871–886. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iskander J, Strikas R.A, Gensheimer K.F, Cox N.J, Redd S.C. Pandemic influenza planning, United States, 1978-2008. Emerg Infect Dis. 2013;19:879–885. doi: 10.3201/eid1906.121478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jack D.W, Asante K.P, Wylie B.J, Chillrud S.N, Whyatt R.M, Ae-Ngibise K.A, Quinn A.K, Yawson A.K, Boamah E.A, Agyei O, Mujtaba M, Kaali S, Kinney P, Owusu-Agyei S. Ghana randomized air pollution and health study (GRAPHS): study protocol for a randomized controlled trial. Trials. 2015;16:420. doi: 10.1186/s13063-015-0930-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kgathi D.L, Zhou P. Biofuel use assessments in Africa: Implications for greenhouse gas emissions and mitigation strategies. Environmental monitoring and assessment. 1995;38:253–269. doi: 10.1007/BF00546767. [DOI] [PubMed] [Google Scholar]
- 17.Kim K.H, Jahan S.A, Kabir E. A review of diseases associated with household air pollution due to the use of biomass fuels. Journal of hazardous materials. 2011;192:425–431. doi: 10.1016/j.jhazmat.2011.05.087. [DOI] [PubMed] [Google Scholar]
- 18.Kirkwood B.R, Hurt L, Amenga-Etego S, Tawiah C, Zandoh C, Danso S, Hurt C, Edmond K, Hill Z, Ten Asbroek G, Fenty J, Owusu-Agyei S, Campbell O, Arthur P. Effect of vitamin A supplementation in women of reproductive age on maternal survival in Ghana (ObaapaVitA): a cluster-randomised, placebo-controlled trial. Lancet. 2010a;375:1640–1649. doi: 10.1016/S0140-6736(10)60311-X. [DOI] [PubMed] [Google Scholar]
- 19.Kirkwood B.R, Manu A, Tawiah-Agyemang C, ten Asbroek G, Gyan T, Weobong B, Lewandowski R.E, Soremekun S, Danso S, Pitt C, Hanson K, Owusu-Agyei S, Hill Z. NEWHINTS cluster randomised trial to evaluate the impact on neonatal mortality in rural Ghana of routine home visits to provide a package of essential newborn care interventions in the third trimester of pregnancy and the first week of life: trial protocol. Trials. 2010b;11:58. doi: 10.1186/1745-6215-11-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.KNMA. Kintampo North Municipal Health Administration (KNMA) Annual Report. 2013 [Google Scholar]
- 21.Kumar R, Nagar J.K, Kumar H, Kushwah A.S, Meena M, Kumar P, Raj N, Singhal M.K, Gaur S.N. Association of indoor and outdoor air pollutant level with respiratory problems among children in an industrial area of Delhi, India. Archives of environmental & occupational health. 2007;62:75–80. doi: 10.3200/AEOH.62.2.75-80. [DOI] [PubMed] [Google Scholar]
- 22.Lakshmi P.V, Virdi N.K, Sharma A, Tripathy J.P, Smith K.R, Bates M.N, Kumar R. Household air pollution and stillbirths in India: analysis of the DLHS-II National Survey. Environmental research. 2013;121:17–22. doi: 10.1016/j.envres.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Lim S.S, Vos T, Flaxman A.D, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson H.R, Andrews K.G, Aryee M, Atkinson C, Bacchus L.J, Bahalim A.N, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell M.L, Blore J.D, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce N.G, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett R.T, Byers T.E, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen J.S, Cheng A.T, Child J.C, Cohen A, Colson K.E, Cowie B.C, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais D.C, Devries K, Dherani M, Ding E.L, Dorsey E.R, Driscoll T, Edmond K, Ali S.E, Engell R.E, Erwin P.J, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane M.M, Flaxman S, Fowkes F.G, Freedman G, Freeman M.K, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez H.R, Hall W, Hoek H.W, Hogan A, Hosgood H.D, 3rd, Hoy D, Hu H, Hubbell B.J, Hutchings S.J, Ibeanusi S.E, Jacklyn G.L, Jasrasaria R, Jonas J.B, Kan H, Kanis J.A, Kassebaum N, Kawakami N, Khang Y.H, Khatibzadeh S, Khoo J.P, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher J.L, Leigh J, Li Y, Lin J.K, Lipshultz S.E, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah G.A, Merriman T.R, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad A.A, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson P.K, Nolla J.M, Norman R, Olives C, Omer S.B, Orchard J, Osborne R, Ostro B, Page A, Pandey K.D, Parry C.D, Passmore E, Patra J, Pearce N, Pelizzari P.M, Petzold M, Phillips M.R, Pope D, Pope C.A, 3rd, Powles J, Rao M, Razavi H, Rehfuess E.A, Rehm J.T, Ritz B, Rivara F.P, Roberts T, Robinson C, Rodriguez-Portales J.A, Romieu I, Room R, Rosenfeld L.C, Roy A, Rushton L, Salomon J.A, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh G.M, Sleet D.A, Smith E, Smith K.R, Stapelberg N.J, Steenland K, Stockl H, Stovner L.J, Straif K, Straney L, Thurston G.D, Tran J.H, Van Dingenen R, van Donkelaar A, Veerman J.L, Vijayakumar L, Weintraub R, Weissman M.M, White R.A, Whiteford H, Wiersma S.T, Wilkinson J.D, Williams H.C, Williams W, Wilson N, Woolf A.D, Yip P, Zielinski J.M, Lopez A.D, Murray C.J, Ezzati M, AlMazroa M.A, Memish Z.A. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller K.A, Siscovick D.S, Sheppard L, Shepherd K, Sullivan J.H, Anderson G.L, Kaufman J.D. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- 25.Muhe L. Mothers’ perceptions of signs and symptoms of acute respiratory infections in their children and their assessment of severity in an urban community of Ethiopia. Ann Trop Paediatr. 1996;16:129–135. doi: 10.1080/02724936.1996.11747815. [DOI] [PubMed] [Google Scholar]
- 26.Naeher L.P, Leaderer B.P, Smith K.R. Particulate matter and carbon monoxide in highland Guatemala: indoor and outdoor levels from traditional and improved wood stoves and gas stoves. Indoor air. 2000;10:200–205. doi: 10.1034/j.1600-0668.2000.010003200.x. [DOI] [PubMed] [Google Scholar]
- 27.Owusu-Agyei S, Nettey O.E, Zandoh C, Sulemana A, Adda R, Amenga-Etego S, Mbacke C. Demographic patterns and trends in Central Ghana: baseline indicators from the Kintampo Health and Demographic Surveillance System. Glob Health Action. 2012;5:1–11. doi: 10.3402/gha.v5i0.19033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perez-Padilla R, Schilmann A, Riojas-Rodriguez H. Respiratory health effects of indoor air pollution. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2010;14:1079–1086. [PubMed] [Google Scholar]
- 29.Ranzi A, Porta D, Badaloni C, Cesaroni G, Lauriola P, Davoli M, Forastiere F. Exposure to air pollution and respiratory symptoms during the first 7 years of life in an Italian birth cohort. Occupational and environmental medicine. 2014 doi: 10.1136/oemed-2013-101867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rehfuess E.A, Tzala L, Best N, Briggs D.J, Joffe M. Solid fuel use and cooking practices as a major risk factor for ALRI mortality among African children. Journal of epidemiology and community health. 2009;63:887–892. doi: 10.1136/jech.2008.082685. [DOI] [PubMed] [Google Scholar]
- 31.Sinha A, Kim S, Ginsberg G, Franklin H, Kohberger R, Strutton D, Madhi S.A, Griffiths U.K, Klugman K.P. Economic burden of acute lower respiratory tract infection in South African children. Paediatrics and international child health. 2012;32:65–73. doi: 10.1179/2046905512Y.0000000010. [DOI] [PubMed] [Google Scholar]
- 32.Smith K.R. National burden of disease in India from indoor air pollution. Proc Natl Acad Sci U S A. 2000;97:132–293. doi: 10.1073/pnas.97.24.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith K.R, McCracken J.P, Weber M.W, Hubbard A, Jenny A, Thompson L.M, Balmes J, Diaz A, Arana B, Bruce N. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet. 2011;378:1717–1726. doi: 10.1016/S0140-6736(11)60921-5. [DOI] [PubMed] [Google Scholar]
- 34.Thacher J.D, Emmelin A, Madaki A.J, Thacher T.D. Biomass fuel use and the risk of asthma in Nigerian children. Respiratory medicine. 2013;107:1845–1851. doi: 10.1016/j.rmed.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 35.Torres-Duque C, Maldonado D, Perez-Padilla R, Ezzati M, Viegi G. Biomass fuels and respiratory diseases: a review of the evidence. Proceedings of the American Thoracic Society. 2008;5:577–590. doi: 10.1513/pats.200707-100RP. [DOI] [PubMed] [Google Scholar]
- 36.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 37.Walker C.L, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta Z.A, O’Brien K.L, Campbell H, Black R.E. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381:1405–1416. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WHO. Indoor Air Pollution: National Burden of Disease Estimates. World Health Organisation. 2007 [Google Scholar]
- 39.WHO. Household Air Pollution, World Health Organisation. 2014 [Google Scholar]
- 40.Wong G.W, Brunekreef B, Ellwood P, Anderson H.R, Asher M.I, Crane J, Lai C.K. Cooking fuels and prevalence of asthma: a global analysis of phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). The lancet. Respiratory medicine. 2013;1:386–394. doi: 10.1016/S2213-2600(13)70073-0. [DOI] [PubMed] [Google Scholar]


