Highlights
-
•
We are reporting a very rare complication of bariatric surgeries.
-
•
Most of reported cases of GPF were post sleeve gastrectomy.
-
•
We could not find cases of GPF post minigastric bypass like our case.
-
•
The presentation was very late in this case (2 years post surgery).
-
•
The findings can be subtle and might be missed on some diagnostic tools.
Abbreviation: GPF, Gastropleural fistula; GBF, Gastrobronchial fistula; SAGB, Single Anastomosis Gastric Bypass (Minigastric Bypass)
Keywords: Gastropleural fistula, Single anastomosis gastric bypass, Minigastric bypass, Bariatric surgery, Empyema
Abstract
Introduction
Pulmonary complications after bariatric surgeries are rare but usually serious. They often occur early after surgery but the presentation might be delayed for several months. Gastropleural fistula after bariatric surgery is extremely rare and has been reported in a very small number of patients post sleeve gastrectomy and gastric bypass.
Case presentation
A 37-year-old lady presented with left sided pleural effusion and empyema 2 years post single anastomosis gastric bypass surgery. She was found to have a large gastropleural fistula and was managed by surgical repair of the fistula with conversion to gastric bypass and decortication of the affected pleura. That resulted in significant clinical improvement and resolution of the empyema.
Conclusion
Gastropleural fistula is a very rare complication of bariatric surgeries and should be considered in patients who present with chronic or recurrent pulmonary infections.
1. Introduction
Bariatric surgeries are very popular procedures for weight reduction in obese population and increasingly done in different parts of the world [1], [2]. Their efficacy in weight reduction and improvement of obesity associated metabolic diseases is well established [3], [4]. Early surgical complications and late dietary disturbances are not uncommon among bariatric surgery patients [5]. Pulmonary complications, however, are rare but they are often serious and occasionally life threatening [6]. These surgeries share the early postoperative pulmonary complications such as pulmonary embolism and atelectasis with other types of abdominal surgeries. Several late complications are related to gastroesophageal reflux due to gastric restrictive nature of some of these surgeries [7]. More specific complications related to bariatric surgeries include gastrobronchial (GBF) and gastropleural fistulae (GPF). Gastrobronchial fistula is an acquired tract between stomach (or gastric pouch) and tracheobronchial tree that can result in recurrent lung infections and abscesses formation [8]. This complication has been reported with all bariatric surgeries but more frequently after sleeve gastrectomy [9]. In a recent systematic review of case reports and case series, 36 patients with GBFs were identified and the mean period until diagnosis was 7.2 months. Half of the patients were treated endoscopically while others required surgical treatment [10]. Similarly, GPF is an acquired communication between stomach and the pleural cavity. This complication is much less frequently reported than GBF and was never reported post single anastomosis gastric bypass (SAGB) or Minigastric bypass (MGB) surgeries.
This report describes the presentation and the management of GPF in a young lady who presented with respiratory symptoms two years after SAGB and the review of literature on GPF particularly in the setting of bariatric surgeries. The case has been reported in line with SCARE criteria [11].
2. Case presentation
A 37-year-old lady presented with dry cough, left sided chest pain and shortness of breath for 2 days. She had no hemoptysis, fever or night sweating and the review of other systems was unrevealing. She had undergone laparoscopic Vertical Band Gastroplasty (VBG) at age of 24 years with body mass index (BMI) of 35 kg/m2, then she had laparoscopic conversion of VBG to Single Anastomosis Gastric Bypass (SAGB) with excision of the gastric Fundus 9 years after VBG due to weight regain with BMI of 38.7 kg/m2. At time of SAGB, there was no evidence of fistulation between stomach and adjacent structure neither on pre-operative imaging nor intra-operatively. Six months prior to this presentation she developed left upper quadrant pain and was found to have left sub-phrenic collection that required ultrasound guided catheter drainage. Upper GI gastrografin study, Upper GI endoscopy and abdominal CT Scan did not show leakage or fistula at that time.
On examination, she looked unwell and was in mild pain. She had reduced breath sound on left side of the chest with stony-dull percussion note. Abdomen was soft with no tenderness and no palpable masses. Laboratory tests were as following: WBC: 13 109/L, Hb 11 g/dl, Plt: 315 109/L, Alb 33 g/L, INR: 1.5, C-reactive protein (CRP): 399 mg/L, erythrocyte sedimentation rate (ESR): 40 mm/hr while electrolytes were normal. Chest x-ray showed obliterated left costophrenic angle and that was interpreted as possible left side small effusion. CT scan of the chest showed a loculated left pleural effusion with air foci causing passive atelectasis and minimal mediastinal shift to the right side. Patient underwent drainage of pleural collection via chest tube and fluid analysis was highly suggestive of left side empyema since it was very turbid with high WBC count, very high fluid LDH (2466 U/L) compared to serum LDH (249 U/L), low glucose (0.2 mmol/L), high protein content (39 gm/dl) and low pH while fluid amylase level was low (30 U/L). Cultures were negative as well as the stain for acid-fast bacilli (AFB) and cytology did not show any malignant cells. Bronchoscopy with bronchoalveolar lavage was done and it showed collapsed left lung with mucus plug. Follow up CT scan for chest and abdomen showed air-filled tract extending from gastric pouch to left pleural cavity in keeping with GPF and interval development of mild right side pleural effusion (Fig. 1). Patient was started on total parentral nutrition (TPN) and was kept null per mouth. Gastrografin study confirmed the leak of orally administered contrast media from the upper part of stomach to the adjacent part of the left sub-phrenic collection but the communication between stomach and pleural cavity that was reported on CT scan could not be clearly seen (Fig. 2). Upper GI Endoscopy showed a normal esophagus however there was a fistula opening below gastroesophageal junction near to the anastomosis site (Fig. 3).
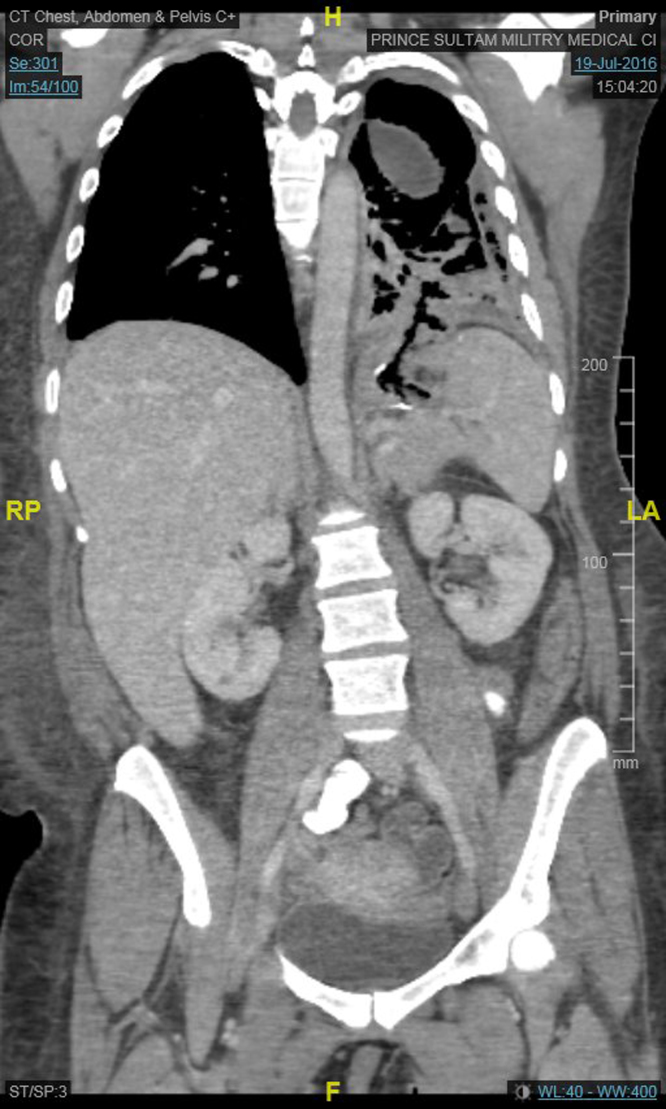
Fig. 1.
CT scan for chest and abdomen showing air filled tract extending from gastric pouch to left pleural cavity.
Fig. 2.

Gastrografin study showing the leakage of orally administered contrast media from the upper part of stomach to the adjacent part of the left sub-phrenic collection.
Fig. 3.
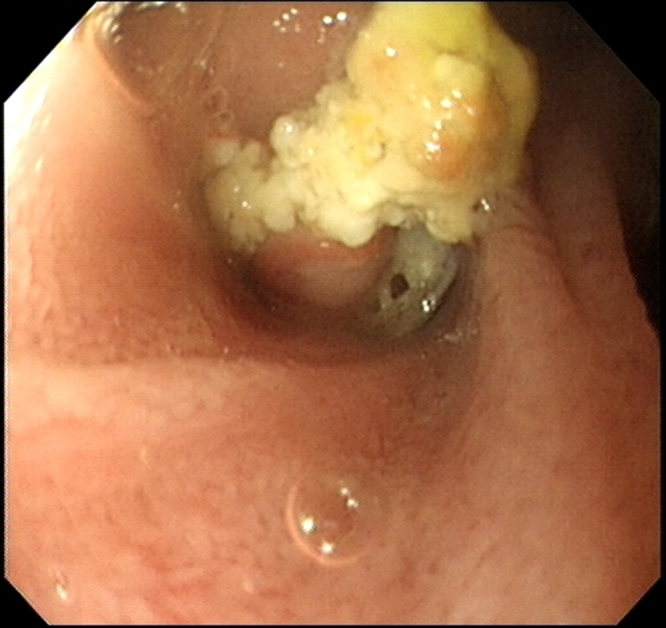
Endoscopic view of the fistula opening below gastroesophageal junction and near to the anastomosis site.
Laparoscopic exploration showed extensive adhesions and complex fistulation between the gastric pouch, left sub-phrenic collection and left diaphragm (Fig. 4). The adhesions were released, the collection was drained and the GPF together with the gastric pouch were excised and gastro-jejunal anastomosis was performed. Additionally, excision of esophago-gastric junction and creation of esophago-jejunal and jejuno-jejunal anastomosis were carried out. Drainage of the left pleural collection was attempted with pigtail catheter but the left lung was entrapped and failed to expand and the patient continued to experience dyspnea on exertion and left side chest pain. Therefore, she underwent video assisted thoracoscopy (VATS) where pleural collection was evacuated and decortication of left lung was performed however the left lower lobe was tightly stuck to the left hemidiaphragm and thus required left anterolateral mini-thoracotomy. Upon release of left lobe, the fistula was seen underneath (Fig. 5) with a surgical clip inside it. Excision of the fistula followed by repair of the diaphragmatic defect was carried out without using mesh. The patient had smooth recovery with gradual resumption of oral intake 48 h post-operatively and after confirming absence of leak by upper GI gastrografin study. Follow up CT of chest and abdomen showed good expansion of the left lung and no leakage of contrast. Patient was discharged home in a very good condition.
Fig. 4.
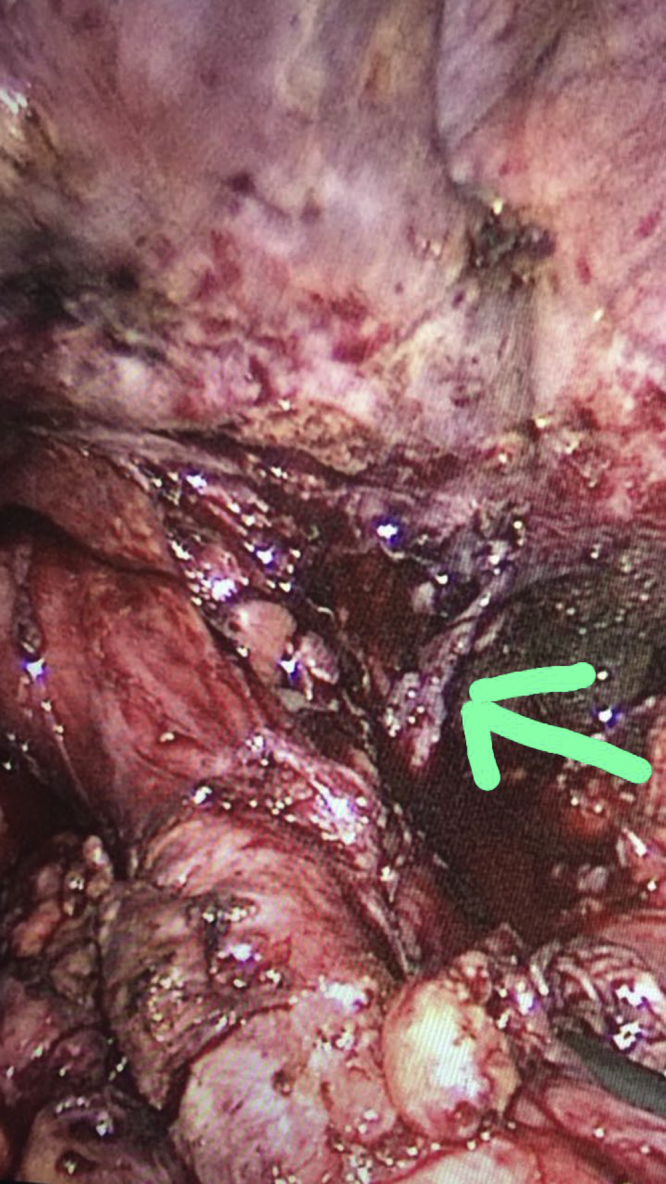
Gastropleural fistula from the peritoneal side as appeared during laparoscopic exploration.
Fig. 5.
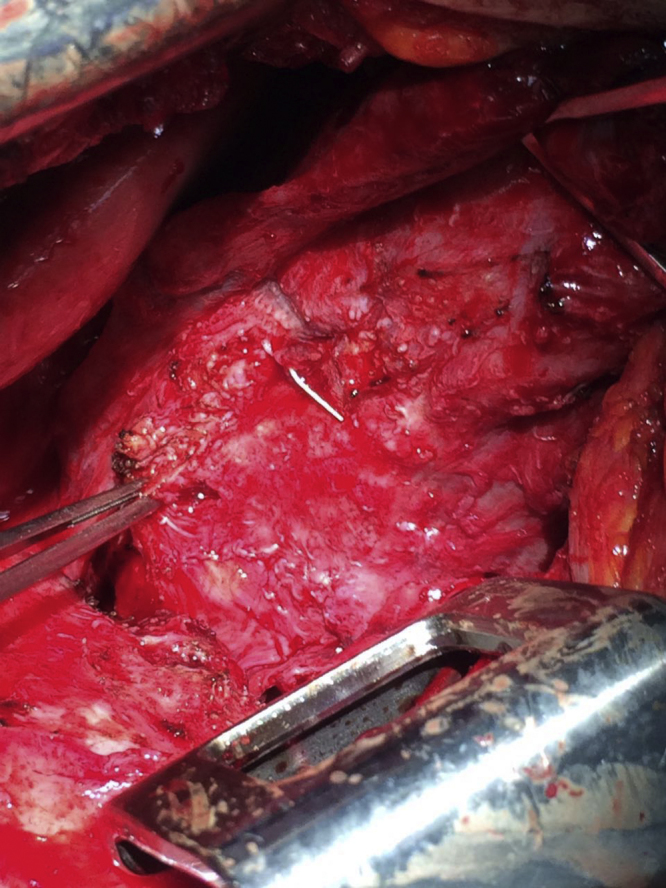
Gastropleural Fistula from the thoracic side as appeared during minithoracotomy.
3. Discussion
Gastropleural Fistula is a very rare condition where there is a pathological communication between stomach and pleural cavity. The reported cases of GPF were mostly related to trauma [12], [13], chronic gastrointestinal herniation in the thoracic cavity as in diaphragmatic and hiatus hernia [14], [15] and malignancy (ovarian carcinoma [16], ewing’s sarcoma [17] and renal cell carcinoma [18]).
Both GBF and GPF represent very rare, yet, serious form of late respiratory complications of bariatric surgeries. The mechanism of formation of these types of fistulae is not clear but it is likely to be secondary to postoperative leak that leads to abscess formation and subsequently creation of a tract between stomach and the pleural cavity in GPF and a bronchus in GBF [19].
The presentation of GPF is usually insidious since patients present with chronic non-specific respiratory symptoms including cough and shortness of breath. They are usually treated conservatively for recurrent lung infections until more diagnostic tests are requested and hence the diagnosis can be delayed for several months [19].
Our patient presented with pleural effusion that required doing CT scan of the chest, which although confirmed the presence of left side empyema, it failed initially to demonstrate the presence of gastropleural communication. The tract however was shown on repeated CT scan and gastrografin study indicating that high index of suspicion is required since finding might be subtle initially and diagnosis can be missed.
Few cases of GPF complicating bariatric surgeries were reported. Garcia et al. reported 2 cases of GPF, first was post sleeve gastrectomy while the second after gastric bypass. Both patients required surgical treatment after failure of conservative approach [20]. Nguyen also reported one patient in his small series with GPF post sleeve gastrectomy and that was corrected surgically as well [19]. Endoscopic closure was successful in a post sleeve gastrectomy GPF with the use of human fibrin and endoscopic clip [21]. Our patient might be the first reported case of GPF post SAGB. The conservative management was not sufficient for closure of the fistula and therefore patient underwent gastrectomy with the conversion of SAGB to Roux-en-Y gastric bypass as well as pleural decortication and drainage.
In conclusion, GPF is a very rare serious complication of bariatric surgeries. It can occur after any type of these surgeries and the diagnosis can be delayed due to non-specificity of symptoms at presentation and false negative results of the diagnostic imaging. High index of suspicion therefore is required to identify patients with GPF post bariatric surgery and the diagnosis should be considered in patients presenting with recurrent respiratory infections. Surgical repair is usually required for treatment however endoscopic approach might be considered.
Conflict of interest
None.
Sources of funding
No Funding required.
Ethical approval
Ethical approval not required since it is a retrospective case report.
Consent
A copy of written consent by the patient is available for review by editor in chief of the journal on request.
Author contributions
Dr Haider Alshurafa: Treating Physician, wrote the introduction and case presentation.
Dr Saleh Alghamdi: Consultant thoracic surgeon, wrote the section of thoracotomy, and did the final revision of the report.
Dr Ali Albenmousa: wrote discussion and submitted the article.
Dr Haifa Alolayani: Did literature review.
Dr Zahraa Alshurafa: Collection of images, language review, and Obtained consent.
Registration of research studies
This is not a clinical trial, Registration is not applicable.
Guarantor
Dr Haider Alshurafa.
References
- 1.Nguyen N.T., Varela J.E. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat. Rev. Gastroenterol. Hepatol. 2016;(November) doi: 10.1038/nrgastro.2016.170. [DOI] [PubMed] [Google Scholar]
- 2.Al-Shurafa H., Elzaafarany A.H., Albenmousa A., Balata M.G. Primary experience of bariatric surgery in a newly established private obesity center. Saudi Med. J. 2016;37(October (10)):1089–1095. doi: 10.15537/smj.2016.10.14043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schauer P.R., Bhatt D.L., Kirwan J.P. Bariatric surgery versus intensive medical therapy for diabetes–3-year outcomes. N. Engl. J. Med. 2014;370(May (21)):2002–2013. doi: 10.1056/NEJMoa1401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caiazzo R., Lassailly G., Leteurtre E. Roux-en-Y gastric bypass versus adjustable gastric banding to reduce nonalcoholic fatty liverdisease: a 5-year controlled longitudinal study. Ann. Surg. 2014;260(November (5)):893–898. doi: 10.1097/SLA.0000000000000945. [DOI] [PubMed] [Google Scholar]
- 5.Van der Beek E.S., Monpellier V.M., Eland I., Tromp E., van Ramshorst B. Nutritional deficiencies in gastric bypass patients; incidence, time of occurrence and implications for post-operative surveillance. Obes. Surg. 2015;25(May (5)):818–823. doi: 10.1007/s11695-014-1456-y. [DOI] [PubMed] [Google Scholar]
- 6.Morino M., Toppino M., Forestieri P., Angrisani L., Allaix M.E., Scopinaro N. Mortality after bariatric surgery: analysis of 13,871 morbidly obese patients from a national registry. Ann. Surg. 2007;246(December (6)):1002–1009. doi: 10.1097/SLA.0b013e31815c404e. [DOI] [PubMed] [Google Scholar]
- 7.Shitrit A.B., Magen A., Swartzs E. Long-term reflux-related symptoms after bariatric surgery: comparison of sleeve gastrectomy versus laparoscopic adjustable gastric banding. Lung. 2013;191(June (3)):289–293. doi: 10.1007/s00408-013-9454-8. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg S., Kanth N., Kanth A. A woman with cough: gastrobronchial fistula as a delayed complication of bariatric surgery. Case report and literature review. Am. J. Emerg. Med. 2015;33(April (4)) doi: 10.1016/j.ajem.2013.11.022. 597. e1-2. [DOI] [PubMed] [Google Scholar]
- 9.Guillaud A., Moszkowicz D., Nedelcu M. Gastrobronchial fistula: a serious complication of sleeve gastrectomy. Results of a French multicentric study. Obes. Surg. 2015;25(December (12)):2352–2359. doi: 10.1007/s11695-015-1702-y. [DOI] [PubMed] [Google Scholar]
- 10.Silva L.B., Moon R.C., Teixeira A.F. Gastrobronchial fistula in sleeve gastrectomy and roux-en-Y gastric bypass – a systematic review. Obes. Surg. 2015;25(October (10)):1959–1965. doi: 10.1007/s11695-015-1822-4. [DOI] [PubMed] [Google Scholar]
- 11.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Muzaffar M.S., Umair B., Asghar A., Ali M.Z., Hanif M.S., Kamal D. Gastropleural fistula: an unusual sequel of blunt chest trauma. J. Coll. Phys. Surg. Pak. 2009;19(July (7)):447–449. 07.2009/JCPSP.447449. [PubMed] [Google Scholar]
- 13.Chowdary P.B., Sadashivaiah S.B., Gangappa R.B., Shivashankar S.C. Gastro pleural fistula: a rare entity presenting as a complication of empyema thoracis following stab injury to the chest. J. Clin. Diagn. Res. 2015;9(April (4)):PD05–PD06. doi: 10.7860/JCDR/2015/12257.5764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tzeng J.J., Lai K.H., Lo G.H., Hsu J.H., Mok K.T. Gastropleural fistula caused by incarcerated diaphragmatic herniation of the stomach. Gastrointest. Endosc. 2001;53(March (3)):382–384. doi: 10.1016/s0016-5107(01)70426-9. [DOI] [PubMed] [Google Scholar]
- 15.Markowits A.M., Herter F.P. Gastro-pleural fistula as a complication of esophageal hiatal hernia. Ann. Surg. 1960;152(July):129–134. doi: 10.1097/00000658-196007000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dohrmann T., Kutup A., Mahner S. Gastropleural fistula in a patient with recurrent ovarian cancer receiving combination therapy with carboplatin, gemcitabine, and bevacizumab. J. Clin. Oncol. 2013;31(April (12)):e208–e210. doi: 10.1200/JCO.2012.45.1708. [DOI] [PubMed] [Google Scholar]
- 17.Bozkurt M.A., Köneş O., Başoğlu I., Alış H. Gastropleural fistula: a rare complication of ewing sarcoma. Korean J. Thorac. Cardiovasc. Surg. 2013;46(August (4)):293–294. doi: 10.5090/kjtcs.2013.46.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neri A., Lambert Y., Marrelli D. Gastro-pleuro-pericardial fistula following combined radiation and chemotherapy for lung metastases from renal cell carcinoma: report of a case. Surg. Today. 2013;43(December (12)):1457–1460. doi: 10.1007/s00595-012-0475-3. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen D., Dip F., Hendricks L., Lo Menzo E., Szomstein S., Rosenthal R. The surgical management of complex fistulas after sleeve gastrectomy. Obes. Surg. 2016;26(February (2)):245–250. doi: 10.1007/s11695-015-1788-2. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Quintero P., Hernandez-Murcia C., Romero R., Derosimo J., Gonzalez A. Gastropleural fistula after bariatric surgery: a report of two cases. J Robot Surg. 2015;9(June (2)):163–166. doi: 10.1007/s11701-015-0505-4. [DOI] [PubMed] [Google Scholar]
- 21.Mendoza Ladd A., Al-Bayati I., Shah P., Haber G. Endoscopic closure of a gastropleural fistula. Endoscopy. 2015;47(Suppl. 1) doi: 10.1055/s-0034-1391357. UCTN:E131-2. [DOI] [PubMed] [Google Scholar]