Abstract
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most frequent form of malformation at birth and represent the cause of 40–50% of pediatric and 7% of adult end-stage renal disease worldwide. The pathogenesis of CAKUT is based on the disturbance of normal nephrogenesis, secondary to environmental and genetic causes. Often CAKUT is the first clinical manifestation of a complex systemic disease, so an early molecular diagnosis can help the physician identify other subtle clinical manifestations, significantly affecting the management and prognosis of patients. The number of sporadic CAKUT cases explained by highly penetrant mutations in a single gene may have been overestimated over the years and a genetic diagnosis is missed in most cases, hence the importance of identifying new genetic approaches which can help unraveling the vast majority of unexplained CAKUT cases. The aim of our review is to clarify the current state of play and the future perspectives of the genetic bases of CAKUT.
Keywords: congenital abnormalities of the kidney and urinary tract (CAKUT), genetics, renal hypodysplasia, next-generation sequencing, copy number variants
1. Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) include a wide range of structural malformations resulting from defects in the morphogenesis of the kidney and of the urinary tract [1,2,3,4]. They are the most common form of malformations at birth, affecting 3–7 out of 1000 live births [5] and representing more than 20% of birth defects [6]. CAKUT effect 40–50% of pediatric and 7% of adult end-stage renal disease worldwide [7,8,9]. In a cohort of 312 children affected by renal malformations (excluding cases with isolated ureteric anomalies) who were followed up until the age of 30 years, an overall poor renal survival for CAKUT patients was described, with a lower outcome for patients carrying bilateral renal hypodysplasia, solitary kidney, and posterior urethral valves, compared with other categories [9]. Nevertheless, retrospective data from an Italian cohort of 146 children 0–18 years old with congenital solitary kidney show a decreased estimated glomerular filtration rate in 12% of the population at a median age of 2.2 years, an estimated survival of 82% at 10 years and proteinuria and/or systemic hypertension in less than 5% of the population; these data highlight the importance in renal outcome of an adequate size of the solitary kidney, which, if smaller than expected, can significantly increase the risk of chronic kidney disease (CKD) [10]. Anyhow, children with CAKUT are known to experience a slower progression of CKD compared to those with glomerular disease [11].
CAKUT are usually detected with prenatal sonography but many cases remain undiagnosed until adulthood [4] and represent a large spectrum of disease with different grade of severity and renal outcome. So far the most commonly used classification is based on anatomical characteristics (segment of the urinary tract involved), with ureteropelvic junction obstruction being the most frequent observed phenotype (20%) [4]. All the malformations can be either uni- or bilateral and, when more than one anomaly is present, it may be hard to understand if all the defects occur independently or if one of them is the primum movens of the whole phenotype [12,13,14]. Moreover, CAKUT can appear as an isolated feature or as part of a systemic condition with extra-renal manifestations [15,16,17] making diagnosis and clinical classification even more challenging.
The pathogenesis of CAKUT is based on the disturbance of normal nephrogenesis, secondary to environmental or genetic causes. Several environmental risk factors have been recognized so far, including maternal diabetes [18] and intrauterine exposure to ACE-inhibitors [19]. On the other hand, the observation of kidney and urinary tract malformations in different members of the same family or as a feature of complex genetic syndromes has enlightened the contribution of genetics in CAKUT and is driving research efforts towards its understanding. The increased recurrence risk of CAKUT among relatives has been confirmed in several studies and is estimated at 4–20% [20,21,22,23,24,25,26]. Multigenerational occurrence of disease has suggested multifactorial or dominant inheritance with reduced penetrance in most kindreds [23,24,25,27,28] but families with recessive inheritance have also been reported [26]. Moreover, the observation of CAKUT being relatively common and mostly sporadic suggests that de novo mutations in genes that potentially contribute to CAKUT, could explain the phenotype in most cases [29].
The aim of our review is to clarify the current state of play and the future perspectives of the genetic bases of CAKUT.
2. Pathogenesis
The development of the mammalian kidney during embryonic life is a multi-stage process that derives from reciprocally inductive events between two intermediate mesenchymal progenitors: the ureteric bud (UB) and the metanephric mesenchyme (MM). It begins at E10.5–E11 in the mouse and at 35–37 days of gestation in humans with the induction of the ureteric bud from the nephric duct, followed by mesenchymal to epithelial transition (MET) and branching morphogenesis, and terminates with nephron patterning and elongation (which include proximal and distal tubule morphogenesis and glomerulogenesis) [1,12,30,31,32,33,34,35]. These embryologic events require a tight regulation at the DNA level (mediated by transcriptional factors) and the post-transcriptional level [36]. As mentioned above, perturbation in each of these steps, due to exposure to environmental risk factors or to the dysfunction of genes that direct this process, can lead to CAKUT [1]. Moreover, the interdependence between distinct developmental pathways explains why defects in different genes result in similar phenotypes [14,34,37,38,39,40,41,42,43,44], why a mutation in a single gene can have pleiotropic effects and, therefore, why a morphologic classification alone can’t predict the primary genetic defect [4].
3. Research Strategies Overview
To better understand the genetic bases of CAKUT, it is useful to review the most commonly used genetic study approaches, which depend on the characteristics of the population study (sample size, number and size of pedigrees) and of the trait of interest (mono or polygenic) [4].
3.1. Candidate Gene Approach
It uses large cohorts of sporadic cases or small pedigrees in case-control association studies to find common disease-associated alleles [4].
3.2. Linkage Analysis
It uses a single large pedigree that co-segregate genes with large effect or a large number of small pedigrees. It has been successful for mapping rare Mendelian diseases and susceptibility loci of diseases such as Alzheimer disease, insulin dependent diabetes mellitus and breast cancer, but is not adequate in CAKUT, because it is not sufficiently powerful to detect susceptibility loci with a small effect size [29].
3.3. Genetic Isolates
These are populations originated from a limited group of founders, with little immigration into the population, which likely inherited few disease-contributing alleles from common ancestors. These mutations can be detected by searching for shared haplotype in affected individuals, through a genetic strategy called linkage disequilibrium mapping [45,46,47]. For instance, Izzi et al. identified a genetic isolate in an Italian Valley in which different glomerular disease occurred at a much higher prevalence compared to the general population and, using linkage disequilibrium mapping, they reconnected most of the patients to a few common founders [48].
3.4. Next-Generation Sequencing (NGS) (Whole Genome Sequencing, Whole Exome Sequencing and Targeted Resequencing)
The term NGS (also known as high-throughput sequencing) refers to a group of modern sequencing technologies developed to allow DNA and RNA sequencing in a more time-efficient and cost-effective manner compared to previous methods like Sanger sequencing. NGS can be applied to the whole genome, the whole exome (which is the protein-coding portion of the genome) or to specific genes or loci of interest [49]. For instance, exome sequencing of patient-parent trios can be used to detect de novo mutations, whose paradigm has been recently supported by an increasing rate of de novo mutations in some heterogeneous disorders (intellectual disability, schizophrenia, autisms spectrum) [50,51,52].
3.5. Genome-Wide Association Studies
It covers the whole genome to search for causative gene variants [53]. Association studies using a large number of patients and matched controls can be used in sporadic cases of CAKUT with complex genetic aetiology like vesicoureteral reflux (VUR), but, so far, they have not been successful in this field because they need larger sample size to increase the statistical power to reach genome-wide significance [29].
3.6. Structural Variants
Copy number variations (CNVs), defined as gain or loss of germ line DNA of a size ranging from 1 kilobase (Kb) to several megabases (Mb) [54] (identified by array-based Comparative Genomic Hybridization (aCGH) and high-density SNP arrays), are a common feature of the human genome [55,56] and have been associated with multiple human phenotypes, including neurodevelopmental diseases [57,58], schizophrenia [59,60], autism [61], epilepsy, cardiac defects [62,63], lung disease, craniofacial malformations, and others [58,61,64,65,66]. In one of the largest studies to date, pathogenic CNVs accounted for 14.2% of cases among 15,767 children with intellectual disability and variable congenital defects [58]. Given that CNVs usually affect the dosage of multiple genes at the same time, the identification of the major genetic drivers underlying such events is usually very challenging [67].
4. Genetic Results
Our current knowledge in the genetics of CAKUT is mostly derived from mouse models and syndromic human developmental disease, which are easier to study and have led to the identification of numerous candidate genes of CAKUT in humans [3,29,68]. The hypothesis that CAKUT can be caused by single-gene mutations derives from the observation that some monogenic mouse models can show CAKUT phenotypes and that monogenic human syndromes can comprise CAKUT phenotypes [1,20]. So far, the most important genes identified to be involved in human and murine kidney development are RET and WNT11 (UB specific), GDNF, WT1, EYA1 (MM specific) and PAX2 (expressed in both UB and MM), being the GDNF/RET the most frequently studied pathway [34,69,70].
4.1. Syndromic Forms
As already mentioned above, syndromic forms were the first group of disease of interest in CAKUT research. Renal-Coloboma Syndrome (renal hypoplasia and coloboma, caused by PAX2 mutations), Orofaciodigital Syndrome (associated with renal cysts, caused by OFD1 gene mutations), Branchio-Oto-Renal Syndrome (caused by mutations in EYA1, SIX1 and SIX5 genes), Renal cysts and Diabetes Syndrome (associated with mutations in HNF1β gene), Fraser Syndrome (characterized by eye abnormalities, syndactyly and various CAKUT forms, caused with mutations in FRAS1, FREM2 or GRIP1 genes), Alagille Syndrome (bile ducts abnormalities, facial features, heart and kidney malformations, for JAG1 and NOTCH1 mutations), and Townes–Brocks Syndrome (imperforate anus, hands and ears malformations and kidney abnormalities, caused by SALL1 mutations) (Table 1) are all known to be caused by point mutations in single genes and show complex phenotypes with various renal and extra-renal involvement [17,71,72,73,74,75]. A better insight in the genetic background of these syndromes allowed to broad the spectrum of genes involved in their pathogenesis, identify genetic pathways of kidney development dysregulation and, in some cases, help to explain the phenotype also in patients with isolated CAKUT without extra-renal syndromic manifestations [44].
Table 1.
Genes involved in syndromic and non-syndromic CAKUT.
| Gene | Disease |
|---|---|
| ACE | Renal tubular dysgenesis |
| AGT | Renal tubular dysgenesis |
| AGTR1 | Renal tubular dysgenesis |
| BMP4 | CAKUT |
| DSTYK | CAKUT |
| EYA1 | Branchio-Oto-Renal Syndrome and renal hypoplasia |
| FRAS1 | Fraser Syndrome |
| FREM1 | Bifid nose, renal agenesis, anorectal malformations |
| FREM1 | Fraser Syndrome |
| GRIP1 | Fraser Syndrome |
| HNF1β | Multicystic dysplastic kidney, renal hypoplasia, renal cysts and diabetes Syndrome |
| NOTCH2 | Alagille syndrome, renal anomalies |
| PAX2 | Renal coloboma Syndrome and CAKUT |
| REN | Renal tubular dysgenesis |
| RET | Renal agenesis and Hirschsprung disease |
| SALL1 | Townes–Brocks Syndrome |
| SIX1 | Branchio-Oto-Renal Syndrome |
| SIX2 | Renal hypodysplasia |
| SIX5 | Branchio-Oto-Renal Syndrome |
| SOX17 | CAKUT |
| UPK3A | Renal dysplasia |
| WNT4 | Mullerian aplasia and hyperandrogenism |
| UMOD | Familial juvenile hyperuricemic nephropathy (FJHN), glomerulocystic kidney disease (GCKD), Autosomal dominant medullary cystic kidney disease 2 (MCKD2) |
4.2. Non-Syndromic Forms
Genetic research for non-syndromic CAKUT has been more challenging, but some candidate genes derived from both studies in syndromic disease and from knock-out mouse models have been successfully validated by the identification of mutations in affected individuals (Table 1) [29].
In 1995, the first gene defect described as being causative of CAKUT was a frameshift deletion in PAX2 in a family with optic nerve coloboma, renal hypoplasia and vesicoureteral reflux [15]. PAX2 plays a critical role in kidney development and its mutations (more than 55 have been reported so far) can lead to different isolated CAKUT phenotypes [76].
HNF1β (hepatocyte nuclear factor 1β), a transcription factor involved in the embryogenesis of the pancreas and liver and expressed in the Wolffian duct from a very early stage of kidney development [77], was the second gene to be identified following the discovery of a heterozygous mutation in two siblings with renal cysts and diabetes [16,78] and then reported in individuals with isolated CAKUT [44,79]. Interestingly, several publications show that gene deletion in the 17q12 region (which includes HNF1β) results in the clinical combination of autism/schizophrenia and CAKUT [80,81]. Moreover, mutations in HNF1β can inhibit PKHD1 gene expression and may contribute to the formation of renal cysts in humans with MODY5 (maturity-onset diabetes of the young type 5) and congenital cystic abnormalities of the kidney [82].
Many studies confirmed that PAX2 and HNF1β mutations can explain up to 15% cases of CAKUT [44,83,84], making them the most important genes to screen for diagnostic purpose. Mutations of PAX2 seem to be more frequently associated with renal hypodyplasia, while mutations in HNF1β are more frequently associated with cystic kidneys [44,83,84].
The ESCAPE STUDY [44] provided the first broad analysis of renal developmental genes contribution (HNF1β, PAX2, EYA1, SIX1, and SALL1) in a large cohort of children with renal hypodysplasia. This study showed a high prevalence of PAX2 and HNF1β mutations (15% of the population) and demonstrated that patients with identical mutations or large gene deletions could show variable renal phenotypes. In accordance with similar results from Ulinski et al. [85], the ESCAPE Study indicated that 22% of all children with cystic renal hypodysplasia carried a mutation of HNF1β, suggesting to screen HNF1β mutations in all the individuals with cystic renal dysplasia.
PAX2, EYA1, and SALL1 all belong to the GDNF-RET signaling pathway, which is required for the normal growth and morphogenesis of the ureteric bud during kidney development [70]. Conversely, BMP4 inhibits GDNF-RET-signaling and is expressed in the mesenchymal cells that surround the Wolffian duct [31]; missense mutations in BMP4, demonstrated to affect BMP4 protein function, were identified in five CAKUT patients [86,87]. RET mutations, which cause multiple endocrine neoplasia (MEN) syndrome [88] and Hirschsprung disease [89], were also described in bilateral renal hypodysplasia/agenesis cases [90,91] and, in addition, patients with Hirschprung disease are described to carry urinary tract defects [92]. Nevertheless, data regarding the frequency of RET as a CAKUT-causing gene are conflicting [90,91].
In a recent study [93] of 7 affected family members with CAKUT, disease-causing mutations were detected in DSTYK gene and additional DSTYK mutations were identified in 7 out of 311 (2.3%) unrelated patients with CAKUT. DSTYK was then proposed as a new CAKUT gene, as it is a dual serine/threonine and tyrosine protein kinase that acts as a positive regulator of ERK phosphorylation downstream of FGF-receptor activation during kidney development and colocalizes with FGF receptors in the ureteric bud and metanephric mesenchyme.
WNT proteins, like WNT9b and WNT4, play a crucial role in mesenchimal-to-epithelial transition (MET) [31,32]. WNT-pathway seems to be partially regulated by SIX2 [94] and mutations in WNT4 and SIX2 have been identified in patients with CAKUT [86,95].
Mutations in the genes encoding several components of the renin–angiotensin system such as AGT (angiotensinogen), REN (renin), ACE (angiotensin-converting enzyme), and AGTR1 (angiotensin II receptor type 1) have been linked to renal tubular dysgenesis [96]. Inactivation of different components of the RAS has been performed in mice with discordant results: Agtr2 [97] and Agt [98] null mice have CAKUT, while Ace and Ren null mice show normal renal development.
The Uromodulin (UMOD) gene encodes the Tamm-Horsfall protein (which is the most abundant physiological urinary protein in humans [99,100] produced by renal tubular cells of the distal loop of Henle) and its mutations have been linked to the pathogenesis of familial juvenile hyperuricemic nephropathy (FJHN), glomerulocystic kidney disease (GCKD) and autosomal dominant medullary cystic kidney disease 2 (MCKD2) [33,101]. Nevertheless, UMOD mutations were not identified in 96 patients with isolated CAKUT, implying that it may represent a very rare etiology for this condition [102].
Hwang et al. [103] investigated the frequency of mutations in 17 known dominant CAKUT-causing genes in a cohort of 749 CAKUT patients and demonstrated that mutations of known CAKUT-causing genes are present in 6% of these families, with SALL1, HNF1β and PAX2 being the most prevalent disease causing genes. Their findings also revealed that some variants previously reported as disease-causing could not be accepted because of their lack of segregation within families. HNF1β and PAX2 were seen at lower frequency in this study, which could be explained by the fact that previous studies used CAKUT cohorts preselected for CKD and with severe renal anomalies [44,83,84,85,104]. They did not identify mutations in SOX17, UMOD, BMP4, SIX1, and UPK3A and, on the other hand, identified SALL1 mutations in >1% of patients, suggesting that this gene may be implicated in CAKUT etiology more commonly than usually believed [44].
Similarly, Nicolaou et al. [105] recently analyzed, through targeted NGS, 208 candidate genes (selected from studies on familial CAKUT, CAKUT-related multi-organ syndromes, and in vitro and in vivo models) in a phenotypically heterogeneous cohort of 453 CAKUT patients, which comprises the largest set of genes analyzed in a numerous cohort of CAKUT patients. They identified 148 candidate variants in 82 genes in 151 patients but only 5 disease-causing mutations (in HNF1β, PAX2, SIX5 and UMOD genes) were defined as causal mutations. In this study the contribution of previously implicated genes to CAKUT risk was significantly smaller than expected and as previously described because most variants were excluded or reported as of uncertain significance for the lack of segregation or of pathogenicity evidence. All together their results indicate that the genetic architecture of CAKUT can be more complex than previously suggested.
So far, analysis of multiple genes in parallel using next generation sequencing in patients with CAKUT has demonstrated that <10% patients with isolated CAKUT carry variants in about 20 genes [103,106,107] with insufficient data regarding their causative role [1,4,15,16,17,21,22,74,75,78,86,90,93,95,100,108,109,110,111,112,113,114,115,116,117,118,119]. Approximately 50% of mutations in PAX2 and microdeletion in HNF1β are estimated to occur de novo but evidence for de novo mutations in other genes is currently lacking [76].
All these findings imply that the majority of causes of CAKUT are still unknown, while the list of novel variants requiring functional characterization is extending [29], including variants in FRAS1, FREM2, GRIP1, ITGA8 and TRAP1 in which recessive mutations have been previously characterized [120,121] providing evidence that CAKUT might in some cases be an autosomal recessive disease.
4.3. Genomic Imbalance
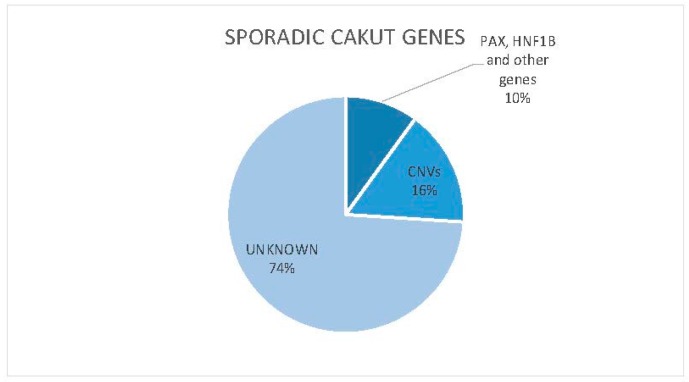
A new and promising approach in the genetics of CAKUT is copy number variants (CNVs) analysis. Human kidney and urinary tract development is particularly sensitive to gene dosage [122,123,124] and structural genomic defects are increasingly recognized as an important cause of congenital malformations, probably explaining over 16% cases of CAKUT (Figure 1) [125]. For instance, microdeletions of Chromosome 17q12 (which contains HNF1β gene), have been described to occur de novo in patients with CAKUT with or without diabetes mellitus [126].
Figure 1.
Sporadic CAKUT genes.
In two different studies the impact of CNVs in CAKUT has been particularly highlighted. In the first one, Sanna-Cherchi et al. [123] compared the frequency of gene-desrupting rare CNVs in two cohorts of patients affected by renal hypodysplasia (522 patients in total) to 4733 controls, demonstrating that rare CNVs account for up to 17% of patients with renal hypodysplasia, then representing a major molecular determinant of kidney malformations. In 2.3% of cases the identified CNV was a rearrangement in chromosomal region 17q12 which contains HNF1β gene. The Di George/Velocardiofacial syndrome (also known as 22.q11.2 deletion syndrome) was the next most frequent identified disorder, consistent with the observation that urologic defects occur in about 40% of individuals with this syndrome [127,128], mainly characterized by heart malformations, facial features, hypocalcemia and immune system dysregulation. Interestingly, Sanna-Cherchi identified in 3 cases with isolated renal hypodysplasia a deletion in the distal region of the DiGeorge locus, suggesting that the gene responsible for the urinary-tract defect is likely located in this particular segment. Moreover, 90% of the disorders detected in this study are also known to predispose to developmental delay or neuropsychiatric disease, suggesting shared pathways between renal and neurodevelopmental programs [58].
Westland et al. [129] similarly investigated the role of rare CNVs in 80 patients with solitary functioning kidney from the KIMONO (KIdney of MONofunctional Origin) study population, compared to over 23,000 controls. They identified rare known or new genomic imbalances in 14% of patients and identified five high-priority genetic drivers, proposing DLG1 and KIF12 as novel candidate genes for human CAKUT, because of their specific expression in maturing kidney and the development of CAKUT phenotype when mutated in animal models.
5. Future Perspectives
Recently, it has been shown that a depletion of miRNAs in different nephrogenic cell lineages in mouse models resembles human CAKUT [36]. MiRNAs are small non-coding RNA molecules of about 22 nucleotides, encoded by >1000 miRNA genes. They function in post-transcriptional regulation of gene expression either by promoting the degradation of mRNA or by inhibiting the translation. Jovanovic [130] recently identified 7 miRs with a potential role in CAKUT, with particular interest for hsa-miR-144. Further functional analysis must be performed to reveal the impact of hsa-miR-144 on CAKUT and to define the precise role of miRs as biomarkers for diagnosis and prognosis of the disease.
6. Conclusions
The importance of unraveling the genetics of CAKUT is well-established, since very often CAKUT is only the first manifestation of a complex systemic disease and can manifest in different members of the same family. A precise genetic definition can help the physician identify other subtle clinical features and give the patient and his family an appropriate genetic counseling.
Currently, HNF1β and PAX2 are the primary genes screened for mutations in CAKUT patients. Nevertheless, the number of cases of sporadic CAKUT explained by highly penetrant mutations in a single gene, as previously proposed from earlier studies on patients and animal models, may have been overestimated over the years (Figure 1).
Hence, it is important to identify new and more comprehensive genetic approaches which can help to explain the vast majority of CAKUT cases.
In recent years, along with an increasing interest in gene dosage imbalance as cause of developmental disease, CNVs analysis has become more and more promising in CAKUT genetic research and has allowed to explain another fraction of CAKUT cases (Figure 1).
In the near future, it will be of primary interest to reach a more exhaustive understanding of the genetics of CAKUT. This process will be more feasible as the cost of sequencing declines and as the investigators establish international collaborations to collect larger patient cohorts and share results. The ultimate goal of genetic research in this field will be to reclassify the wide spectrum of CAKUT phenotypes and to stratify renal prognosis (in terms of risk of developing renal failure) accordingly to genotype. Moreover, a better understanding of the biological pathways involved in kidney development dysregulation could lead to the development of innovative targeted therapeutic approaches.
Author Contributions
Valentina P. Capone conceptualized the paper, selected the studies, drafted the initial manuscript and approved the final manuscript as submitted; William Morello conceptualized the paper, revised the initial draft and approved the final manuscript as submitted; Francesca Taroni revised the initial draft and approved the final manuscript as submitted; Giovanni Montini conceptualized the paper, revised the initial manuscript and approved the final manuscript as submitted.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Vivante A., Kohl S., Hwang D., Dworschak G., Hildebrandt F. Single-gene causes of congential anomalies of the kidney and urinary tract (CAKUT) in humans. Pediatr. Nephrol. 2014;29:695–704. doi: 10.1007/s00467-013-2684-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dressler G. The cellular basis of kidney development. Annu. Rev. Cell Dev. Biol. 2006;22:509–529. doi: 10.1146/annurev.cellbio.22.010305.104340. [DOI] [PubMed] [Google Scholar]
- 3.Ichikawa I., Kuwayama F., Pope J., Stephens F., Miyazaki Y. Paradigm shift from classic anatomic theories to contemporary cell biological views of CAKUT. Kidney Int. 2002;61:889–898. doi: 10.1046/j.1523-1755.2002.00188.x. [DOI] [PubMed] [Google Scholar]
- 4.Sanna-Cherchi S., Caridi G., Weng P., Scolari F., Perfumo F., Gharavi A., Ghiggeri G. Genetic approaches to human renal agenesis/hypoplasia and dysplasia. Pediatr. Nephrol. 2007;22:1675–1684. doi: 10.1007/s00467-007-0479-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anonymous. Birth Defects Monitoring Program (BDMP)/Commission on Professional and Hospital Activities (CPHA) surveillance data 1988–1991. Teratology. 1993;48:658–675. doi: 10.1002/tera.1420480608. [DOI] [PubMed] [Google Scholar]
- 6.Loane M., Dolk H., Kelly A., Teljeur C., Greenlees R., Densem J. EUROCAT working group paper 4: EUROCAT statistical monitoring: Identification and investigation of ten year trends of congenital anomalies in Europe. Birth Defects Res. A Clin. Mol. Teratol. 2011;91:31–43. doi: 10.1002/bdra.20778. [DOI] [PubMed] [Google Scholar]
- 7.North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) 2008 Annual Report. [(accessed on 10 April 2017)]; Available online: https://web.emmes.com/study/ped/annlrept/Annual%20Report%20-2008.pdf.
- 8.Ardissino G., Daccò V., Testa S., Bonaudo R., Claris-Appiani A., Taioli E., Marra G., Edefonti A., Sereni F. Epidemiology of chronic renal failure in children: Data from the ItalKid project. Pediatrics. 2003;111:382–387. doi: 10.1542/peds.111.4.e382. [DOI] [PubMed] [Google Scholar]
- 9.Sanna-Cherchi S., Ravani P., Corbani V., Parodi S., Haupt R., Piaggio G., Innocenti M., Somenzi D., Trivelli A., Caridi G., et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 2009;76:528–533. doi: 10.1038/ki.2009.220. [DOI] [PubMed] [Google Scholar]
- 10.La Scola C., Ammenti A., Puccio G., Lega M., de Mutiis C., Guiducci C., de Petris L., Perretta R., Venturoli V., Vergine G., et al. Congenital solitary kidney in children: Size matters. J. Urol. 2016;196:1250–1256. doi: 10.1016/j.juro.2016.03.173. [DOI] [PubMed] [Google Scholar]
- 11.Harambat J., van Stralen K., Kim J., Tizard E. Epidemiology of chronic kidney disease in children. Pediatr. Nephrol. 2012;27:363–373. doi: 10.1007/s00467-011-1939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pope J., Brock J., Adams M., Stephens F., Ichikawa I. How they begin and how they end: Classic and new theories for the development and deterioration of congenital anomalies of the kidney and urinary tract, CAKUT. J. Am. Soc. Nephrol. 1999;10:2018–2028. doi: 10.1681/ASN.V1092018. [DOI] [PubMed] [Google Scholar]
- 13.Hiraoka M., Tsukahara H., Ohshima Y., Kasuga K., Ishihara Y., Mayumi M. Renal aplasia is the predominant cause of congenital solitary kidneys. Kidney Int. 2002;61:1840–1844. doi: 10.1046/j.1523-1755.2002.00322.x. [DOI] [PubMed] [Google Scholar]
- 14.Woolf A., Price K., Scambler P., Winyard P. Evolving concepts in human renal dysplasia. J. Am. Soc. Nephrol. 2004;15:998–1007. doi: 10.1097/01.ASN.0000113778.06598.6F. [DOI] [PubMed] [Google Scholar]
- 15.Sanyanusin P., Schimmenti L., McNoe L., Ward T., Pierpont M., Sullivan M., Dobyns W., Eccles M. Mutation of the PAX2 gene in a family with optic nerve colobomas, renal anomalies and vesicoureteral reflux. Nat. Genet. 1995;9:358–364. doi: 10.1038/ng0495-358. [DOI] [PubMed] [Google Scholar]
- 16.Lindner T., Njolstad P., Horikawa Y., Bostad L., Bell G., Sovik O. A novel syndrome of diabetes mellitus, renal dysfunction and genital malformation associated with a partial deletion of the pseudo-POU domain of hepatocyte nuclear factor-1β. Hum. Mol. Genet. 1999;8:2001–2008. doi: 10.1093/hmg/8.11.2001. [DOI] [PubMed] [Google Scholar]
- 17.Abdelhak S., Kalatzis V., Heilig R., Compain S., Samson D., Vincent C., Weil D., Cruaud C., Sahly I., Leibovici M., et al. A human homologue of the Drosophila eyes absent gene underlies branchio-oto-renal (BOR) syndrome and identifies a novel gene family. Nat. Genet. 1997;15:157–164. doi: 10.1038/ng0297-157. [DOI] [PubMed] [Google Scholar]
- 18.Parikh C., McCall D., Engelman C., Schrier R. Congenital renal agenesis: Case-control analysis of birth characteristics. Am. J. Kidney Dis. 2002;39:689–694. doi: 10.1053/ajkd.2002.31982. [DOI] [PubMed] [Google Scholar]
- 19.Cooper W., Hernandez-Diaz S., Arbogast P., Dudley J., Dyer S., Gideon P., Hall K., Ray W. Major congenital malformations after first-trimester exposure to ACE inhibitors. N. Engl. J. Med. 2006;354:2443–2451. doi: 10.1056/NEJMoa055202. [DOI] [PubMed] [Google Scholar]
- 20.Bulum B., Ozçakar Z., Ustüner E., Düşünceli E., Kavaz A., Duman D., Walz K., Fitoz S., Tekin M., Yalçınkaya F. High frequency of kidney and urinary tract anomalies in asymptomatic first-degree relatives of patients with CAKUT. Pediatr. Nephrol. 2013;28:2143–2147. doi: 10.1007/s00467-013-2530-8. [DOI] [PubMed] [Google Scholar]
- 21.Renkema K., Winyard P., Skovorodkin I., Levtchenko E., Hindryckx A., Jeanpierre C., Weber S., Salomon R., Antignac C., Vainio S., et al. Novel perspectives for investigating congenital anomalies of the kidney and urinary tract (CAKUT) Nephrol. Dial. Transplant. 2011;26:3843–3851. doi: 10.1093/ndt/gfr655. [DOI] [PubMed] [Google Scholar]
- 22.Weber S. Novel genetic aspects of congenital anomalies of kidney and urinary tract. Curr. Opin. Pediatr. 2012;24:212–218. doi: 10.1097/MOP.0b013e32834fdbd4. [DOI] [PubMed] [Google Scholar]
- 23.Roodhooft A., Birnholz J., Holmes L. Familial nature of congenital absence and severe dysgenesis of both kidneys. N. Engl. J. Med. 1984;310:1341–1345. doi: 10.1056/NEJM198405243102101. [DOI] [PubMed] [Google Scholar]
- 24.McPherson E., Carey J., Kramer A., Hall J., Pauli R., Schimke R., Tasin M. Dominantly inherited renal adysplasia. Am. J. Med. Genet. 1987;26:863–872. doi: 10.1002/ajmg.1320260413. [DOI] [PubMed] [Google Scholar]
- 25.Carter C., Evans K., Pescia G. A family study of renal agenesis. J. Med. Genet. 1979;16:176–188. doi: 10.1136/jmg.16.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pasch A., Hoefele J., Grimminger H., Hacker H., Hildebrandt F. Multiple urinary tract malformations with likely recessive inheritance in a large Somalian kindred. Nephrol. Dial. Transplant. 2004;19:3172–3175. doi: 10.1093/ndt/gfh514. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan B., Milner L., Jequier S., Kaplan P., de Chadarevian J. Autosomal dominant inheritance of small kidneys. Am. J. Med. Genet. 1989;32:120–126. doi: 10.1002/ajmg.1320320126. [DOI] [PubMed] [Google Scholar]
- 28.Doray B., Gasser B., Reinartz I., Stoll C. Hereditary renal adysplasia in a three generations family. Genet. Couns. 1999;10:251–257. [PubMed] [Google Scholar]
- 29.Nicolaou N., Renkema K., Bongers E., Giles R., Knoers N. Genetic, environmental, and epigenetic factors involved in CAKUT. Nat. Rev. Nephrol. 2015;11:720–731. doi: 10.1038/nrneph.2015.140. [DOI] [PubMed] [Google Scholar]
- 30.Schedl A. Renal abnormalities and their developmental origin. Nat. Rev. Genet. 2007;8:791–802. doi: 10.1038/nrg2205. [DOI] [PubMed] [Google Scholar]
- 31.Dressler G. Advances in early kidney specification, development and patterning. Development. 2009;136:3863–3874. doi: 10.1242/dev.034876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reidy K., Rosenblum N. Cell and molecular biology of kidney development. Semin. Nephrol. 2009;29:321–337. doi: 10.1016/j.semnephrol.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Faa G., Gerosa C., Fanni D., Monga G., Zaffanello M., van Eyken P., Fanos V. Morphogenesis and molecular mechanisms involved in human kidney development. J. Cell Physiol. 2012;227:1257–1268. doi: 10.1002/jcp.22985. [DOI] [PubMed] [Google Scholar]
- 34.Vainio S., Lin Y. Coordinating early kidney development: Lessons from gene targeting. Nat. Rev. Genet. 2002;3:533–543. doi: 10.1038/nrg842. [DOI] [PubMed] [Google Scholar]
- 35.Woolf A. Embriology in Pediatric Nephrology. 5th ed. Springer; Berlin/Heidelberg, Germany: 2004. [Google Scholar]
- 36.Kohl S., Chen J., Vivante A., Hwang D., Shril S., Dworschak G., van der Ven A., Sanna-Cherchi S., Bauer S., Lee R., et al. Targeted sequencing of 96 renal developmental microRNAs in 1213 individuals from 980 families with congenital anomalies of the kidney and urinary tract. Nephrol. Dial. Transplant. 2016;31:1280–1283. doi: 10.1093/ndt/gfv447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mackie G., Stephens F. Duplex kidneys: A correlation of renal dysplasia with position of the ureteral orifice. J. Urol. 1975;114:274–280. doi: 10.1016/s0022-5347(17)67007-1. [DOI] [PubMed] [Google Scholar]
- 38.Grieshammer U., le Ma P.A., Wang F., Tessier-Lavigne M., Martin G. SLIT2-mediated ROBO2 signaling restricts kidney induction to a single site. Dev. Cell. 2004;6:709–717. doi: 10.1016/S1534-5807(04)00108-X. [DOI] [PubMed] [Google Scholar]
- 39.Yu J., McMahon A., Valerius M. Recent genetic studies of mouse kidney development. Curr. Opin. Genet. Dev. 2004;14:550–557. doi: 10.1016/j.gde.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Miyazaki Y., Oshima K., Fogo A., Ichikawa I. Evidence that bone morphogenetic protein 4 has multiple biological functions during kidney and urinary tract development. Kidney Int. 2003;63:835–844. doi: 10.1046/j.1523-1755.2003.00834.x. [DOI] [PubMed] [Google Scholar]
- 41.Durbec P., Marcos-Gutierrez C., Kilkenny C., Grigoriou M., Wartiowaara K., Suvanto P., Smith D., Ponder B., Costantini F., Saarma M., et al. GDNF signalling through the RET receptor tyrosine kinase. Nature. 1996;381:789–793. doi: 10.1038/381789a0. [DOI] [PubMed] [Google Scholar]
- 42.Torres M., Gómez-Pardo E., Dressler G., Gruss P. Pax-2 controls multiple steps of urogenital development. Development. 1995;121:4057–4065. doi: 10.1242/dev.121.12.4057. [DOI] [PubMed] [Google Scholar]
- 43.Schmidt-Ott K., Lan D., Hirsh B., Barasch J. Dissecting stages of mesenchymal-to-epithelial conversion during kidney development. Nephron Physiol. 2006;104:56–60. doi: 10.1159/000093287. [DOI] [PubMed] [Google Scholar]
- 44.Weber S., Moriniere V., Knüppel T., Charbit M., Dusek J., Ghiggeri G., Jankauskiené A., Mir S., Montini G., Peco-Antic A., et al. Prevalence of mutations in renal developmental genes in children with renal hypodisplasia: Results of the ESCAPE Study. J. Am. Soc. Nephrol. 2006;17:2864–2870. doi: 10.1681/ASN.2006030277. [DOI] [PubMed] [Google Scholar]
- 45.Nikali K., Suomalainen A., Terwilliger J., Koskinen T., Weissenbach J., Peltonen L. Random search for shared chromosomal regions in four affected individuals: The assignment of a new hereditary ataxia locus. Am. J. Hum. Genet. 1995;56:1088–1095. [PMC free article] [PubMed] [Google Scholar]
- 46.Houwen R., Baharloo S., Blankenship K., Raeymaekers P., Juyn J., Sandkuijl L., Freimer N. Genome screening by searching for shared segments: Mapping a gene for benign recurrent intrahepatic cholestasis. Nat. Genet. 1994;8:380–386. doi: 10.1038/ng1294-380. [DOI] [PubMed] [Google Scholar]
- 47.Gianfrancesco F., Esposito T., Ombra M., Forabosco P., Maninchedda G., Fattorini M., Casula S., Vaccargiu S., Casu G., Cardia F., et al. Identification of a novel gene and a common variant associated with uric acid nephrolithiasis in a Sardinian genetic isolate. Am. J. Hum. Genet. 2003;72:1479–1491. doi: 10.1086/375628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Izzi C., Sanna-Cherchi S., Prati E., Belleri R., Remedio A., Tardanico R., Foramitti M., Guerini S., Viola B., Movilli E., et al. Familial aggregation of primary glomerulonephritis in an Italian population isolate: Valtrompia study. KIdney Int. 2006;69:1033–1040. doi: 10.1038/sj.ki.5000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morinière V., Dahan K., Hilbert P., Lison M., Lebbah S., Topa A., Bole-Feysot C., Pruvost S., Nitschke P., Plaisier E., et al. Improving mutation screening in familial hematuric nephropathies through next generation sequencing. J. Am. Soc. Nephrol. 2014;25:2740–2751. doi: 10.1681/ASN.2013080912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vissers L., de Ligt J., Gilissen C., Janssen I., Steehouwer M., de Vries P., van Lier B., Arts P., Wieskamp N., del Rosario M., et al. A de novo paradigm for mental retardation. Nat. Genet. 2010;42:1109–1112. doi: 10.1038/ng.712. [DOI] [PubMed] [Google Scholar]
- 51.Girard S., Gauthier J., Noreau A., Xiong L., Zhou S., Jouan L., Dionne-Laporte A., Spiegelman D., Henrion E., Diallo O., et al. Increased exonic de novo mutation rate in individuals with schizophrenia. Nat. Genet. 2011;43:860–863. doi: 10.1038/ng.886. [DOI] [PubMed] [Google Scholar]
- 52.O’Roak B., Deriziotis P., Lee C., Vives L., Schwartz J., Girirajan S., Karakoc E., Mackenzie A., Ng S., Baker C., et al. Exome sequencing in sporadic autism spectrum disorders identifies severe de novo mutations. Nat. Genet. 2011;43:585–589. doi: 10.1038/ng.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.The International HapMap Consortium The International HapMap Project. Nature. 2003;426:789–796. doi: 10.1038/nature02168. [DOI] [PubMed] [Google Scholar]
- 54.Alkan C., Coe B., Eichler E. Genome structural variation discovery and genotyping. Nat. Rev. Genet. 2011;12:363–376. doi: 10.1038/nrg2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khaja R., Zhang J., MacDonald J., He Y., Joseph-George A., Wei J., Rafiq M., Qian C., Shago M., Pantano L., et al. Genome assembly comparison identifies structural variants in the human genome. Nat. Genet. 2006;38:1413–1418. doi: 10.1038/ng1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Redon R., Ishikawa S., Fitch K., Feuk L., Perry G., Andrews T., Fiegler H., Shapero M., Carson A., Chen W., et al. Global variation in copy number in the human genome. Nature. 2006;444:444–454. doi: 10.1038/nature05329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Girirajan S., Rosenfeld J., Coe B., Parikh S., Friedman N., Goldstein A., Filipink R., McConnell J., Angle B., Meschino W., et al. Phenotypic heterogeneity of genomic disorders and rare copy-number variants. N. Engl. J. Med. 2012;367:1321–1331. doi: 10.1056/NEJMoa1200395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cooper G., Coe B., Girirajan S., Rosenfeld J., Vu T., Baker C., Williams C., Stalker H., Hamid R., Hannig V., et al. A copy number variation morbidity map of developmental delay. Nat. Genet. 2011;43:838–846. doi: 10.1038/ng.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walsh T., McClellan J., McCarthy S., Addington A., Pierce S., Cooper G., Nord A., Kusenda M., Malhotra D., Bhandari A., et al. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science. 2008;320:539–543. doi: 10.1126/science.1155174. [DOI] [PubMed] [Google Scholar]
- 60.Stefansson H., Rujescu D., Cichon S., Pietiläinen O., Ingason A., Steinberg S., Fossdal R., Sigurdsson E., Sigmundsson T., Buizer-Voskamp J., et al. Large recurrent microdeletions associated with schizophrenia. Nature. 2008;455:232–236. doi: 10.1038/nature07229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sebat J., Lakshmi B., Malhotra D., Troge J., Lese-Martin C., Walsh T., Yamrom B., Yoon S., Krasnitz A., Kendall J., et al. Strong association of de novo copy number mutations with autism. Science. 2007;316:445–449. doi: 10.1126/science.1138659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Soemedi R., Wilson I., Bentham J., Darlay R., Töpf A., Zelenika D., Cosgrove C., Setchfield K., Thornborough C., Granados-Riveron J., et al. Contribution of global rare copy-number variants to the risk of sporadic congenital heart disease. Am. J. Hum. Genet. 2012;91:489–501. doi: 10.1016/j.ajhg.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hitz M., Lemieux-Perreault L., Marshall C., Feroz-Zada Y., Davies R., Yang S., Lionel A., D’Amours G., Lemyre E., Cullum R., et al. Rare copy number variants contribute to congenital left-sided heart disease. PLoS Genet. 2012;8:9. doi: 10.1371/journal.pgen.1002903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brunetti-Pierri N., Berg J., Scaglia F., Belmont J., Bacino C., Sahoo T., Lalani S., Graham B., Lee B., Shinawi M., et al. Recurrent reciprocal 1q21.1 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat. Genet. 2008;40:1466–1471. doi: 10.1038/ng.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Osoegawa K., Vessere G., Utami K., Mansilla M., Johnson M., Riley B., L’Heureux J., Pfundt R., Staaf J., van der Vliet W., et al. Identification of novel candidate genes associated with cleft lip and palate using array comparative genomic hybridisation. J. Med. Genet. 2008;45:81–86. doi: 10.1136/jmg.2007.052191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Greenway S., Pereira A., Lin J., DePalma S., Israel S., Mesquita S., Ergul E., Conta J., Korn J., McCarroll S., et al. De novo copy number variants identify new genes and loci in isolated sporadic tetralogy of Fallot. Nat. Genet. 2009;41:931–935. doi: 10.1038/ng.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Golzio C., Katsanis N. Genetic architecture of reciprocal CNVs. Curr. Opin. Genet. Dev. 2013;23:240–248. doi: 10.1016/j.gde.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Uetani N., Bouchard M. Plumbing in the embryo: Developmental defects of the urinary tracts. Clin. Genet. 2009;75:307–317. doi: 10.1111/j.1399-0004.2009.01175.x. [DOI] [PubMed] [Google Scholar]
- 69.Majumdar A., Vainio S., Kispert A., McMahon J., McMahon A. Wnt11 and RET/GDNF pathways cooperate in regulating ureteric branching during metanephric kidney development. Development. 2003;130:3175–3185. doi: 10.1242/dev.00520. [DOI] [PubMed] [Google Scholar]
- 70.Costantini F., Shakya R. GDNF/RET signaling and the development of the kidney. Bioessays. 2006;28:117–127. doi: 10.1002/bies.20357. [DOI] [PubMed] [Google Scholar]
- 71.Limwongse C. Syndromes and malformations of the urinary tract. Pediatr. Nephrol. 2004:121–156. doi: 10.1007/978-3-540-76341-3_6. [DOI] [Google Scholar]
- 72.Turnpenny P., Ellard S. Alagille syndrome: Pathogenesis, diagnosis and management. Eur. J. Hum. Genet. 2012;20:251–257. doi: 10.1038/ejhg.2011.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ruf R., Xu P., Silvius D., Otto E., Beekmann F., Muerb U., Kumar S., Neuhaus T., Kemper M., Raymond R.J., et al. SIX1 mutations cause branchio-oto-renal syndrome by disruption of EYA1-SIX1-DNA complexes. Proc. Natl. Acad. Sci. USA. 2004;101:8090–8095. doi: 10.1073/pnas.0308475101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoskins B., Cramer C., Silvius D., Zou D., Raymond R., Orten D., Kimberling W., Smith R., Weil D., Petit C., et al. Transcription factor SIX5 is mutated in patients with branchio-oto-renal syndrome. Am. J. Hum. Genet. 2007;80:800–804. doi: 10.1086/513322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kohlhase J., Wischermann A., Reichenbach H., Froster U., Engel W. Mutations in the SALL1 putative transcription factor gene cause Townes-Brocks syndrome. Nat. Genet. 1998;18:81–83. doi: 10.1038/ng0198-81. [DOI] [PubMed] [Google Scholar]
- 76.Bower M., Salomon R., Allanson J., Antignac C., Benedicenti F., Benetti E., Binenbaum G., Jensen U., Cochat P., DeCramer S., et al. Update of PAX2 mutations in renal coloboma syndrome and establishment of a locus-specific database. Hum. Mutat. 2012;33:457–466. doi: 10.1002/humu.22020. [DOI] [PubMed] [Google Scholar]
- 77.Coffinier C., Thépot D., Babinet C., Yaniv M., Barra J. Essential role for the homeoprotein vHNF1/HNF1β in visceral endoderm differentiation. Development. 1999;21:4785–4794. doi: 10.1242/dev.126.21.4785. [DOI] [PubMed] [Google Scholar]
- 78.Horikawa Y., Iwasaki N., Hara M., Furuta H., Hinokio Y., Cockburn B., Lindner T., Yamagata K., Ogata M., Tomonaga O., et al. Mutation in hepatocyte nuclear factor-1β gene (TCF2) associated with MODY. Nat. Genet. 1997;17:384–385. doi: 10.1038/ng1297-384. [DOI] [PubMed] [Google Scholar]
- 79.Edghill E., Bingham C., Ellard S., Hattersley A. Mutations in hepatocyte nuclear factor-1β and their related phenotypes. J. Med. Genet. 2006;43:84–90. doi: 10.1136/jmg.2005.032854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moreno-De-Luca D., Mulle J.G., Kaminsky E.B., Sanders S.J., Myers S.M., Adam M.P., Pakula A.T., Eisenhauer N.J., Uhas K., Weik L. Deletion 17q12 is a recurrent copy number variant that confers high risk of autism and schizophrenia. Am. J. Hum. Genet. 2010;87:618–630. doi: 10.1016/j.ajhg.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Loirat C., Bellanné-Chantelot C., Husson I., Deschênes G., Guigonis V., Chabane N. Autism in three patients with cystic or hyperechogenic kidneys and chromosome 17q12 deletion. Nephrol. Dial. Transplant. 2010;25:3430–3433. doi: 10.1093/ndt/gfq380. [DOI] [PubMed] [Google Scholar]
- 82.Hiesberger T., Bai Y., Shao X., McNally B., Sinclair A., Tian X., Somlo S., Igarashi P. Mutation of hepatocyte nuclear factor-1β inhibits PKHD1 gene expression and produces renal cysts in mice. J. Clin. Investig. 2004;113:814–825. doi: 10.1172/JCI200420083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thomas R., Sanna-Cherchi S., Warady B., Furth S., Kaskel F., Gharavi A. HNF1B and PAX2 mutations are a common cause of renal hypodysplasia in the CKiD cohort. Pediatr. Nephrol. 2011;26:897–903. doi: 10.1007/s00467-011-1826-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Madariaga L., Morinière V., Jeanpierre C., Bouvier R., Loget P., Martinovic J., Dechelotte P., Leporrier N., Thauvin-Robinet C., Jensen U., et al. Severe prenatal renal anomalies associated with mutations in HNF1B or PAX2 genes. Clin. J. Am. Soc. Nephrol. 2013;8:1179–1187. doi: 10.2215/CJN.10221012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ulinski T., Lescure S., Beaufils S., Guigonis V., Decramer S., Morin D., Clauin S., Deschênes G., Bouissou F., Bensman A., et al. Renal phenotypes related to hepatocyte nuclear factor-1β (TCF2) mutations in a pediatric cohort. J. Am. Soc. Nephrol. 2006;17:497–503. doi: 10.1681/ASN.2005101040. [DOI] [PubMed] [Google Scholar]
- 86.Weber S., Taylor J., Winyard P., Baker K., Sullivan-Brown J., Schild R., Knüppel T., Zurowska A., Caldas-Alfonso A., Litwin M., et al. SIX2 and BMP4 mutations associate with anomalous kidney development. J. Am. Soc. Nephrol. 2008;19:891–903. doi: 10.1681/ASN.2006111282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tabatabaeifar M., Schlingmann K., Litwin M., Emre S., Bakkaloglu A., Mehls O., Antignac C., Schaefer F., Weber S., ESCAPE Trial Group Functional analysis of BMP4 mutations identified in pediatric CAKUT patients. Pediatr. Nephrol. 2009;24:2361–2368. doi: 10.1007/s00467-009-1287-6. [DOI] [PubMed] [Google Scholar]
- 88.Santoro M., Carlomagno F., Romano A., Bottaro D., Dathan N., Grieco M., Fusco A., Vecchio G., Matoskova B., Kraus M. Activation of RET as a dominant transforming gene by germline mutations of MEN2A and MEN2B. Science. 1995;267:381–383. doi: 10.1126/science.7824936. [DOI] [PubMed] [Google Scholar]
- 89.Romeo G., Ronchetto P., Luo Y., Barone V., Seri M., Ceccherini I., Pasini B., Bocciardi R., Lerone M., Kääriäinen H. Point mutations affecting the tyrosine kinase domain of the RET proto-oncogene in Hirschsprung’s disease. Nature. 1994;367:377–378. doi: 10.1038/367377a0. [DOI] [PubMed] [Google Scholar]
- 90.Skinner M., Safford S., Reeves J., Jackson M., Freemerman A. Renal aplasia in humans is associated with RET mutations. Am. J. Hum. Genet. 2008;82:344–351. doi: 10.1016/j.ajhg.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jeanpierre C., Macé G., Parisot M., Morinière V., Pawtowsky A., Benabou M., Martinovic J., Amiel J., Attié-Bitach T., Delezoide A., et al. RET and GDNF mutations are rare in fetuses with renal agenesis or other severe kidney development defect. J. Med. Genet. 2011;48:497–504. doi: 10.1136/jmg.2010.088526. [DOI] [PubMed] [Google Scholar]
- 92.Prato A.P., Musso M., Ceccherini I., Mattioli G., Giunta C., Ghiggeri G., Jasonni V. Hirschsprung disease and congenital anomalies of the kidney and urinary tract (CAKUT): A novel syndromic association. Medicine. 2009;88:83–90. doi: 10.1097/MD.0b013e31819cf5da. [DOI] [PubMed] [Google Scholar]
- 93.Sanna-Cherchi S., Sampogna R., Papeta N., Burgess K., Nees S., Perry B., Choi M., Bodria M., Liu Y., Weng P., et al. Mutations in DSTYK and dominant urinary tract malformations. N. Engl. J. Med. 2013;369:621–629. doi: 10.1056/NEJMoa1214479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Park J., Ma W., O’Brien L., Chung E., Guo J., Cheng J., Valerius M., McMahon J., Wong W., McMahon A. Six2 and Wnt regulate self-renewal and commitment of nephron progenitors through shared gene regulatory networks. Dev. Cell. 2012;23:637–651. doi: 10.1016/j.devcel.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vivante A., Mark-Danieli M., Davidovits M., Harari-Steinberg O., Omer D., Gnatek Y., Cleper R., Landau D., Kovalski Y., Weissman I., et al. Renal hypodysplasia associates with a WNT4 variant that causes aberrant canonical WNT signaling. J. Am. Soc. Nephrol. 2013;24:550–558. doi: 10.1681/ASN.2012010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gribouval O., Gonzales M., Neuhaus T., Aziza J., Bieth E., Laurent N., Bouton J., Feuillet F., Makni S., Amar H.B., et al. Mutations in genes in the renin-angiotensin system are associated with autosomal recessive tubular dysgenesis. Nat. Genet. 2005;37:964–968. doi: 10.1038/ng1623. [DOI] [PubMed] [Google Scholar]
- 97.Nishimura H., Yerkes E., Hohenfellner K., Miyazaki Y., Ma J., Hunley T., Yoshida H., Ichiki T., Threadgill D., Phillips J., et al. Role of the angiotensin type 2 receptor gene in congenital anomalies of the kidney and urinary tract, CAKUT, of mice and men. Mol. Cell. 1999;3:1–10. doi: 10.1016/S1097-2765(00)80169-0. [DOI] [PubMed] [Google Scholar]
- 98.Okubo S., Niimura F., Matsusaka T., Fogo A., Hogan B., Ichikawa I. Angiotensinogen gene null-mutant mice lack homeostatic regulation of glomerular filtration and tubular reabsorption. Kidney Int. 1998;53:617–625. doi: 10.1046/j.1523-1755.1998.00788.x. [DOI] [PubMed] [Google Scholar]
- 99.Tamm I., Horsfall F.J. Characterization and separation of an inhibitor of viral hemagglutination present in urine. Proc. Soc. Exp. Biol. Med. 1959;74:106–108. doi: 10.3181/00379727-74-17825. [DOI] [PubMed] [Google Scholar]
- 100.Hart T., Gorry M., Hart P., Woodard A., Shihabi Z., Sandhu J., Shirts B., Xu L., Zhu H., Barmada M., et al. Mutations of the UMOD gene are responsible for medullary cystic kidney disease 2 and familial juvenile hyperuricaemic nephropathy. J. Med. Genet. 2002;39:882–892. doi: 10.1136/jmg.39.12.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Weichhart T., Zlabinger G., Säemann M. The multiple functions of Tamm-Horsfall protein in human health and disease: A mystery clears up. Wien. Klin. Wochenschr. 2005;117:316–322. doi: 10.1007/s00508-005-0353-8. [DOI] [PubMed] [Google Scholar]
- 102.Wolf M., Hoskins B., Beck B., Hoppe B., Tasic V., Otto E., Hildebrandt F. Mutation analysis of the Uromodulin gene in 96 individuals with urinary tract anomalies (CAKUT) Pediatr. Nephrol. 2009;24:55–60. doi: 10.1007/s00467-008-1016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hwang D., Dworschak G., Kohl S., Saisawat P., Vivante A., Hilger A., Reutter H., Soliman N., Bogdanovic R., Kehinde E., et al. Mutations in 12 known dominant disease-causing genes clarify many congenital anomalies of the kidney and urinary tract. Kidney Int. 2014;85:1429–1433. doi: 10.1038/ki.2013.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Heidet L., Decramer S., Pawtowski A., Morinière V., Bandin F., Knebelmann B., Lebre A., Faguer S., Guigonis V., Antignac C., et al. Spectrum of HNF1B mutations in a large cohort of patients who harbor renal diseases. Clin. J. Am. Soc. Nephrol. 2010;5:1079–1090. doi: 10.2215/CJN.06810909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nicolaou N., Pulit S., Nijman I., Monroe G., Feitz W., Schreuder M., van Eerde A., de Jong T., Giltay J., van der Zwaag B., et al. Prioritization and burden analysis of rare variants in 208 candidate genes suggest they do not play a major role in CAKUT. Kidney Int. 2016;89:476–486. doi: 10.1038/ki.2015.319. [DOI] [PubMed] [Google Scholar]
- 106.Saisawat P., Tasic V., Vega-Warner V., Kehinde E., Günther B., Airik R., Innis J., Hoskins B., Hoefele J., Otto E., et al. Identification of two novel CAKUT-causing genes by massively parallel exon resequencing of candidate genes in patients with unilateral renal agenesis. Kidney Int. 2012;81:196–200. doi: 10.1038/ki.2011.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chatterjee R., Ramos E., Hoffman M., VanWinkle J., Martin D., Davis T., Hoshi M., Hmiel S., Beck A., Hruska K., et al. Traditional and targeted exome sequencing reveals common, rare and novel functional deleterious variants in RET-signaling complex in a cohort of living US patients with urinary tract malformations. Hum. Genet. 2012;131:1725–1738. doi: 10.1007/s00439-012-1181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yosypiv I. Congenital anomalies of the kidney and urinary tract: A genetic disorder? Int. J. Nephrol. 2012;2012:909083. doi: 10.1155/2012/909083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chen F. Genetic and developmental basis for urinary tract obstruction. Pediatr. Nephrol. 2009;24:1621–1632. doi: 10.1007/s00467-008-1072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Barak H., Huh S., Chen S., Jeanpierre C., Martinovic J., Parisot M., Bole-Feysot C., Nitschké P., Salomon R., Antignac C., et al. FGF9 and FGF20 maintain the stemness of nephron progenitors in mice and man. Dev. Cell. 2012;22:1191–1207. doi: 10.1016/j.devcel.2012.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen T., Li Q., Xu J., Ding K., Wang Y., Wang W., Li S., Shen Y. Mutation screening of BMP4, BMP7, HOXA4 and HOXB6 genes in Chinese patients with hypospadias. Eur. J. Hum. Genet. 2007;15:23–28. doi: 10.1038/sj.ejhg.5201722. [DOI] [PubMed] [Google Scholar]
- 112.Groenen P.M., Vanderlinden G., Devriendt K., Fryns J.P., van de Ven W.J. Rearrangement of the human CDC5L gene by a t(6;19)(p21;q13. 1) in a patient with multicystic renal dysplasia. Genomics. 1998;49:218–229. doi: 10.1006/geno.1998.5254. [DOI] [PubMed] [Google Scholar]
- 113.Brockschmidt A., Chung B., Weber S., Fischer D., Kolatsi-Joannou M., Christ L., Heimbach A., Shtiza D., Klaus G., Simonetti G., et al. CHD1L: A new candidate gene for congenital anomalies of the kidneys and urinary tract (CAKUT) Nephrol. Dial. Transplant. 2012;27:2355–2364. doi: 10.1093/ndt/gfr649. [DOI] [PubMed] [Google Scholar]
- 114.Lu W., van Eerde A., Fan X., Quintero-Rivera F., Kulkarni S., Ferguson H., Kim H., Fan Y., Xi Q., Li Q., et al. Disruption of ROBO2 is associated with urinary tract anomalies and confers risk of vesicoureteral reflux. Am. J. Hum. Genet. 2007;80:616–632. doi: 10.1086/512735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ruf R., Berkman J., Wolf M., Nurnberg P., Gattas M., Ruf E., Hyland V., Kromberg J., Glass I., Macmillan J., et al. A gene locus for branchio-otic syndrome maps to chromosome 14q21.3-q24.3. J. Med. Genet. 2003;40:515–519. doi: 10.1136/jmg.40.7.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gimelli S., Caridi G., Beri S., McCracken K., Bocciardi R., Zordan P., Dagnino M., Fiorio P., Murer L., Benetti E., et al. Mutations in SOX17 are associated with congenital anomalies of the kidney and the urinary tract. Hum. Mutat. 2010;31:1352–1359. doi: 10.1002/humu.21378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jenkins D., Bitner-Glindzicz M., Malcolm S., Hu C., Allison J., Winyard P., Gullett A., Thomas D., Belk R., Feather S., et al. De novo Uroplakin IIIa heterozygous mutations cause human renal adysplasia leading to severe kidney failure. J. Am. Soc. Nephrol. 2005;16:2141–2149. doi: 10.1681/ASN.2004090776. [DOI] [PubMed] [Google Scholar]
- 118.Van Esch H., Groenen P., Nesbit M., Schuffenhauer S., Lichtner P., Vanderlinden G., Harding B., Beetz R., Bilous R., Holdaway I., et al. GATA3 haplo-insufficiency causes human HDR syndrome. Nature. 2000;406:419–422. doi: 10.1038/35019088. [DOI] [PubMed] [Google Scholar]
- 119.Gbadegesin R., Brophy P., Adeyemo A., Hall G., Gupta I., Hains D., Bartkowiak B., Rabinovich C., Chandrasekharappa S., Homstad A., et al. TNXB mutations can cause vesicoureteral reflux. J. Am. Soc. Nephrol. 2013;24:1313–1322. doi: 10.1681/ASN.2012121148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kohl S., Hwang D., Dworschak G., Hilger A., Saisawat P., Vivante A., Stajic N., Bogdanovic R., Reutter H., Kehinde E., et al. Mild recessive mutations in six Fraser syndrome-related genes cause isolated congenital anomalies of the kidney and urinary tract. J. Am. Soc. Nephrol. 2014;25:1917–1922. doi: 10.1681/ASN.2013101103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Saisawat P., Kohl S., Hilger A., Hwang D., Gee H.Y., Dworschak G., Tasic V., Pennimpede T., Natarajan S., Sperry E., et al. Whole-exome resequencing reveals recessive mutations in TRAP1 in individuals with CAKUT and VACTERL association. Kidney Int. 2014;85:1310–1317. doi: 10.1038/ki.2013.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Weber S., Landwehr C., Renkert M., Hoischen A., Wühl E., Denecke J., Radlwimmer B., Haffner D., Schaefer F., Weber R. Mapping candidate regions and genes for congenital anomalies of the kidneys and urinary tract (CAKUT) by array-based comparative genomic hybridization. Nephrol. Dial. Transplant. 2011;26:136–143. doi: 10.1093/ndt/gfq400. [DOI] [PubMed] [Google Scholar]
- 123.Sanna-Cherchi S., Kiryluk K., Burgess K., Bodria M., Sampson M., Hadley D., Nees S., Verbitsky M., Perry B., Sterken R., et al. Copy-number disorders are a common cause of congenital kidney malformations. Am. J. Hum. Genet. 2012;91:987–997. doi: 10.1016/j.ajhg.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Caruana G., Wong M., Walker A., Heloury Y., Webb N., Johnstone L., James P., Burgess T., Bertram J. Copy-number variation associated with congenital anomalies of the kidney and urinary tract. Pediatr. Nephrol. 2015;30:487–495. doi: 10.1007/s00467-014-2962-9. [DOI] [PubMed] [Google Scholar]
- 125.Materna-Kiryluk A., Kiryluk K., Burgess K., Bieleninik A., Sanna-Cherchi S., Gharavi A., Latos-Bielenska A. The emerging role of genomics in the diagnosis and workup of congenital urinary tract defects: A novel deletion syndrome on chromosome 3q13.31-22.1. Pediatr. Nephrol. 2014;29:257–267. doi: 10.1007/s00467-013-2625-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mefford H., Clauin S., Sharp A., Moller R., Ullmann R., Kapur R., Pinkel D., Cooper G., Ventura M., Ropers H., et al. Recurrent reciprocal genomic rearrangements of 17q12 are associated with renal disease, diabetes, and epilepsy. Am. J. Hum. Genet. 2007;81:1057–1069. doi: 10.1086/522591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Burtey S. 22q11.2 microdeletion syndrome is a common cause of renal tract malformations. Nat. Clin. Pract. Nephrol. 2008;4 doi: 10.1038/ncpneph0906. [DOI] [PubMed] [Google Scholar]
- 128.Shprintzen R. Velocardiofacial syndrome and DiGeorge sequence. J. Med. Genet. 1994;31:423–424. doi: 10.1136/jmg.31.5.423-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Westland R., Verbitsky M., Vukojevic K., Perry B., Fasel D., Zwijnenburg P., Bökenkamp A., Gille J., Saraga-Babic M., Ghiggeri G., et al. Copy number variation analysis identifies novel CAKUT candidate genes in children with a solitary functioning kidney. Kidney Int. 2015;88:1402–1410. doi: 10.1038/ki.2015.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jovanovic I., Zivkovic M., Kostic M., Krstic Z., Djuric T., Kolic I., Alavantic D., Stankovic A. Transcriptome-wide based identification of miRs in congenital anomalies of the kidney and urinary tract (CAKUT) in children: The significant upregulation of tissue miR-144 expression. J. Transl. Med. 2016;3:193. doi: 10.1186/s12967-016-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]