Abstract
Objective
The Joint Commission recommends all patients be screened for suicide. However, differences in suicide attempt and death rates may affect how well tools predict risk across age groups. Our objective was to determine whether item 9 of the Patient Health Questionnaire (PHQ9) predicts risk for suicide attempts and deaths across age groups.
Methods
PHQ9s completed by adult outpatients treated for mental health conditions in 2010–2012 at four Mental Health Research Network-affiliated healthcare systems were used to measure depression severity and suicidal ideation. Suicide attempts were identified via ICD-9 codes and suicide deaths via ICD-10 codes and state death certificates.
Results
In all, 939,268PHQ9s were completed by 297,290 outpatients. Compared to those without, those with nearly daily suicidal ideation were 5-to-8times more likely to attempt suicide and 3-to-11times more likely to die by suicide within 30 days, and 2-to-4times more likely to attempt suicide and 2-to-6 times more likely to die by suicide within 365 days. The increased risk of suicide death for those with any level of suicidal ideation persisted over two years. The relationships between suicide thoughts and attempts and deaths were similar across age groups.
Limitations
Our sample was limited to outpatients completing a PHQ9 and relied on pre-existing clinical and administrative data.
Conclusions
Suicidal ideation reported on the PHQ9 was a robust predictor of suicide attempts and deaths regardless of age, and this increased risk persisted for two years. Healthcare systems should address both the immediate and sustained risk for suicide for patients of all ages.
Keywords: depression, suicide attempts, suicide deaths
INTRODUCTION
Suicide is a major public health concern, with rates of suicide in the United States now surging to levels not seen in nearly 30 years.1 An estimated 3.9% of adults in the U.S. (9.3 million people) have had suicidal thoughts in the past year.2 Rates of suicidal ideation are highest among young adults (aged 18–25) at 7.4%, and lowest in older adults (aged 50 or older) at 2.7%. Approximately 1.1% of U.S. adults (2.7 million people) made a plan for attempting suicide in the past year, highest in young adults at 2.5% and lowest among older adults at 0.6%. About 0.6% of U.S. adults (1.3 million people) attempted suicide in the past year, with the majority of these adults (85%, or 1.1 million people) having made a plan for attempting suicide. A total of 41,149 adults died by suicide in the U.S. in 2013, making suicide the tenth leading cause of death.2
Results for lifetime prevalence of suicidal ideation and attempts globally have been similar. In a study of 84,850 adults interviewed across 17 countries, 9.2% reported lifetime suicidal ideation, while 3.1% reported lifetime suicide plans and 2.7% reported at least one suicide attempt.3 Of note, 60% of people who developed suicidal ideation developed a plan for suicide in the first year after the onset of suicidal ideation. For those with suicidal ideation, 33.6% made a plan for suicide, while 29.0% made a suicide attempt. Over half (56.0%) of patients who had both suicidal ideation and a plan for suicide attempted suicide, compared to 15.4% of patients who had suicidal ideation without a plan.
Clearly, suicidal ideation increases risk for suicide, and having a plan for suicide greatly further increases this risk. However, to date, the U.S. Preventative Services Task Force has found insufficient evidence to adequately assess the risks or benefits of screening for suicide risk in primary care.4 Since that 2014 recommendation, we reported that the Patient Health Questionnaire (PHQ9) can accurately identify primary care and mental health outpatients at increased risk of suicide attempts and deaths.5 Patients who reported frequent thoughts of death or self-harm on the ninth question of the PHQ9 were 6 times more likely to attempt suicide and five times more likely to die by suicide in the following year than those who did not report such thoughts. Many healthcare systems essentially routinely screen for suicidal ideation as part of the widely administered PHQ9, and last year, the Joint Commission issued a Sentinel Event Alert recommending that healthcare systems screen all patients in all healthcare settings for suicide risk using a brief, standardized, evidence-based screening tool, such as the PHQ9.6
The risk for suicide attempts and deaths is known to vary by age, with suicide death rates highest in people ages 45–64 (19.5 suicide deaths per 100,000) and 85 and older (19.3 per 100,000), relatively lower in those 30–44 (16.1 per 100,000) and 65–84 (16.2 per 100,000), and lowest in those 18–29 (13.9 per 100,000).7 Suicide attempts also vary by age, with an estimated 25 suicide attempts for every death in younger adults but only 4 attempts per death in elderly adults.8 Overall, middle-aged adults account for the largest proportion of suicides (56%),9 and this group saw the largest increase – nearly 30% – in suicide deaths between 1999 and 2010.10
It is unclear whether these differences in rates of suicide attempts and deaths by age7–10 might lead to differential risk prediction across age groups. Given this knowledge gap, along with the increasing use of the PHQ911 and the Joint Commission’s recommendation to screen all patients for suicide,6 we conducted this study to determine if PHQ9 item 9 responses consistently predicted risk for suicide attempts and deaths across age groups in a large, diverse populations of outpatients across the U.S.
METHODS
Data Sources
The Mental Health Research Network (MHRN) is a consortium of public-domain research centers affiliated with 13 large not-for-profit integrated healthcare systems. Data included in this study were from four partner sites in the MHRN that were routinely administering PHQ9s to outpatients in 2010 through 2012: Group Health Cooperative, HealthPartners, Kaiser Permanente Colorado, and Kaiser Permanente Southern California. These healthcare systems provide comprehensive medical care, including mental health and primary care, to approximately 4.4 million members and/or patients in California, Colorado, Idaho, Minnesota, Washington and Wisconsin. Members are enrolled through employer-sponsored insurance plans, individual insurance plans, and capitated Medicaid and Medicare programs, and are largely representative of the regional populations of each healthcare system. Group Health and HealthPartners are mixed-model systems where both internal and external clinicians provide patient care; for these two sites, samples were limited to members who were also patients to ensure availability of electronic health records and claims data.
Data from electronic health records, insurance claims and other administrative systems from all MHRN sites were organized into a Virtual Data Warehouse (VDW), a federated data system using common data definitions and formats to facilitate sharing of de-identified data, such as gender, age, race/ethnicity, ICD-9 codes to assess comorbidities and suicide attempts, ICD-10 codes and state death data to assess suicide deaths, and visit codes, allowing for protected health information to remain at each site.12 PHQ9 data were organized into a separate research database, as these data were not yet available in the VDW. Each site’s Institutional Review Board and privacy board approved all study procedures and granted waivers of consent to use these de-identified data for research.
Study Population
All adult outpatients, aged 18 and older, who completed a PHQ9 11,13 between 1/1/2010 and 12/31/2012 and were receiving specialty mental healthcare or had a mental health diagnosis documented in primary or specialty care at a participating healthcare system in the two years prior to PHQ9 administration were included in analyses. The total number of people who made a specialty mental health visit or had a mental health diagnosis was about 1.9 million. Across the four healthcare systems, the proportion of these visits for which a PHQ9 was recorded ranged from 5% to 42%. In earlier work, we demonstrated that patients for whom a PHQ9 was recorded were not meaningfully different from those without a completed PHQ9.5 Patients could contribute multiple PHQ9s to the sample if these were administered during separate encounters. All four healthcare systems used the PHQ9 for assessment of depression severity, and the PHQ9 was documented in abstractable fields in the electronic medical record. Only PHQ9s completed at outpatient encounters were abstracted.
Depression Severity and Suicidal Ideation
The first 8 items of the PHQ9 ask about frequency of depression symptoms, such as anhedonia or feeling down or hopeless. Item 9 of the PHQ9 asks, “Over the last two weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” Response options for each item of the PHQ9 are “not at all” (0 points), “several days” (1 point), “more than half the days” (2 points) or “nearly every day” (3 points). PHQ9 total scores range from 0 to 27, and scores of 1–4 indicate minimal symptoms of depression, 5–9 mild, 10–14 moderate, 15–19 moderately severe, and 20+ severe.11 A PHQ9 score >10 has been shown to have a sensitivity of 88% and a specificity of 88% for major depression.11 PHQ8 scores, calculated using all of the PHQ9 items except for item 9, are categorized identically to PHQ9 scores.14
Suicide Attempts and Deaths
Suicide attempts were identified via electronic medical records and insurance claims data. Both fatal and non-fatal suicide attempts were included in all analyses of suicide attempts. A patient was considered to have experienced a non-fatal suicide attempt if he/she had an inpatient or outpatient encounter associated with one of the following categories of ICD-9 codes: (1) definite self-inflicted injury (E950–E958); (2) possible self-inflicted acute injury (E980–E988); or (3) poisoning (960–989) or open wound (870–897) combined with documented suicidal ideation (V62.84). A previous study using a gold standard of clinician-reviewed medical records found the positive predictive value to be 100% for category 1, 80% for category 2, and 86% for category 3. The combined weighted average positive predictive value was 92%.15 A patient experienced a suicide death if he/she had an ICD-10 code for suicide death (X60–X84) or an ICD-9 code for definite or possible self-inflicted injury (as defined above) and death confirmed by linking health insurance membership records to state death certificates.
Analyses
Descriptive analyses examined the risk of suicide attempts and deaths following completion of a PHQ9, stratified by response to item 9. Each new PHQ9 defined a new period at risk, and a patient could therefore contribute multiple overlapping risk periods by completing multiple PHQ9s, and each suicide attempt or death could be linked to multiple prior PHQ9s from a single patient. This approach examined risk based on data available when the PHQ was completed, regardless of subsequent PHQ9s, and avoided the censoring that would occur if the likelihood of completing a later PHQ was related to the risk of a subsequent suicide attempt. For analyses of suicide attempts and suicide deaths, each risk period was censored using the following events: disenrollment from the healthcare system, death from causes other than suicide, at 730 days past the PHQ9, or last availability of suicide attempt or death data. Because predictors of repeat suicide attempts may be different than those of first attempts, PHQ9s subsequent to a suicide attempt were excluded from analyses of suicide attempts.
Partially conditional Cox proportional hazards regression 16 was used to estimate the association between PHQ9 item 9 response and subsequent suicide attempt or death by age category (18–29, 30–44, 45–64, 65+ years old). A modification of the Cox proportional hazards model was used to accommodate multiple observations clustered within individuals. The models controlled for gender, healthcare system, patient mental health treatment status (defined as any antidepressant use or outpatient mental health visit or inpatient mental health admission in the prior 5 years), visit specialty type associated with the PHQ9 encounter, comorbidity burden (measured by Charlson score of 0, 1 or >1) and race/ethnicity (nonHispanic white, nonHispanic black, Hispanic, Asian, Hawaiian/Pacific Islander, Native American/Alaskan Native, other or mixed race or unknown, and missing). The estimated hazard associated with responding “nearly every day,” “more than half the days,” and “several days” on item 9 of the PHQ9 was compared to the estimated hazard associated with responding “not at all” (the reference group). An interaction term was also generated between the PHQ9 item 9 response and age at the time of the response. Results are reported within each age group referent to that group’s “risk” of responding “not at all.” Because each individual patient could contribute multiple PHQ9s, a robust sandwich estimator 17 was used to calculate confidence limits for hazard ratio estimates. As we previously found evidence of a log-linear decay of increased risk by PHQ9 item 9 response, we included time-dependent predictors of PHQ9 item 9 response to the model. This allowed the model to estimate a decay specific to each PHQ9 item 9 response, while constraining the decay to be constant within the interaction with age. All analyses were performed using Stata version 13.1.
RESULTS
Across four health systems, 297,290 outpatients completed 939,268 PHQ9s between January 1, 2010 and December 31, 2012 (Table 1). Of those PHQ9s, 70% were completed by women and 18–29, 30–44, 45–64, and 65+ year olds completed 17%, 27%, 40%, and 16% of PHQ9s, respectively. PHQ9s were most frequently completed by patients who self-identified as non-Hispanic white (74%;n=694,378) or Hispanic (10%; n=89,361), followed by patients who self-identified as Other or Mixed Race (6%; n=59,141), non-Hispanic black (6%; n=52,372), Asian (3%; n=27,090), Native American/Alaskan Native (1%; n=13,272), or Hawaiian/Pacific Islander (0.3%; n=3,654).
Table 1. Patient characteristics and suicidal ideation as assessed by the PHQ9.
939,268 PHQ9s were completed by 297,290 patients. Question 9 of the PHQ9 asks about thoughts of being better off dead or of hurting oneself in some way over the last two weeks. Response options include “not at all” (Q9=0), “several days” (Q9=1), “more than half the days” (Q9=2), or “nearly every day” (Q9=3).
| Total Sample | PHQ9s | Q9=0 | Q9=1 | Q9=2 | Q9=3 |
|---|---|---|---|---|---|
| 939,268 | 748,040 | 122,716 | 41,055 | 27,457 | |
| (80%) | (13%) | (4%) | (3%) | ||
| Gender | |||||
| Male | 283,515 | 217,225 (77%) | 42,725 (15%) | 14,396 (5%) | 9,169 (3%) |
| Female | 655,753 | 530,815 (81%) | 79,991 (12%) | 26,659 (4%) | 18,288 (3%) |
| Age | |||||
| 18–29 | 156,977 | 122,423 (78%) | 22,554 (14%) | 7,422 (5%) | 4,578 (3%) |
| 30–44 | 252,863 | 203,294 (80%) | 32,047 (13%) | 10,656 (4%) | 6,866 (3%) |
| 45–64 | 378,649 | 297,273 (79%) | 51,650 (14%) | 17,765 (5%) | 11,961 (3%) |
| 65+ | 150,779 | 125,050 (83%) | 16,465 (11%) | 5,212 (3%) | 4,052 (3%) |
| Race/Ethnicity | |||||
| Non-Hispanic white | 694,378 | 556,681 (80%) | 89,881 (13%) | 28,829 (4%) | 18,987 (3%) |
| Asian | 27,090 | 20,455 (76%) | 4,242 (16%) | 1,526 (6%) | 867 (3%) |
| Non-Hispanic black | 52,372 | 40,361 (77%) | 6,901 (13%) | 3,018 (6%) | 2,092 (4%) |
| Hawaiian/Pacific Islander | 3,654 | 2,723 (75%) | 522 (14%) | 208 (6%) | 201 (6%) |
| Native American/ Alaskan Native | 13,272 | 10,307 (78%) | 1,763 (13 %) | 679 (5%) | 523 (4%) |
| Other, Mixed or Unknown | 59,141 | 44,746 (76%) | 9,107 (15%) | 3,178 (5%) | 2,110 (4%) |
| Hispanic | 89,361 | 72,767 (81%) | 10,300 (12%) | 3,617 (4%) | 2,677 (3%) |
| PHQ8 score | |||||
| 0–4 (minimal depression) | 265,547 | 255,108 (96%) | 8153 (3%) | 1350 (1%) | 936 (<1%) |
| 5–9 (mild depression) | 241,655 | 215,551 (89%) | 23,234 (10%) | 2220 (1%) | 650 (<1%) |
| 10–14 (moderate depression) | 203,482 | 155,630 (76%) | 36,758 (18%) | 8352 (4%) | 2742 (1%) |
| 15+ (moderately- severe to severe depression) | 228,584 | 121,751 (53%) | 54,571 (24%) | 29,133 (13%) | 23,129 (10%) |
| Visit Type | |||||
| Mental Health | 499,157 | 379,204 (76%) | 75,453 (15%) | 26,229 (5%) | 18,271 (4%) |
| Primary Care | 262,294 | 218,528 (83%) | 28,954 (11%) | 9,202 (4%) | 5,610 (2%) |
| Other | 177,817 | 150,308 (85%) | 18,309 (10%) | 5,624 (3%) | 3,576 (2%) |
| Charlson Score | |||||
| 0 | 583,688 | 469,153 (80%) | 74,874 (13%) | 23,865 (4%) | 15,796 (3%) |
| 1 | 154,940 | 122,410 (79%) | 20,531 (13%) | 7,339 (5%) | 4,660 (3%) |
| >1 | 148,423 | 116,718 (79%) | 19,436 (13%) | 7,132 (5%) | 5,137 (3%) |
Depression Severity and Suicidal Ideation
Patients experiencing the full spectrum of depression severity were represented, with 28% of encounters with patients self-reporting no or minimal symptoms of depression (PHQ8 score of 0–4), 26% with mild symptoms (5 – 9), 22% with moderate symptoms (10 – 14), and 24% with moderately-severe or severe symptoms (> 15) of depression. In the majority of encounters (80%), patients did not report suicidal thoughts over the previous two weeks. Those who did report suicidal thoughts over the past two weeks reported having these thoughts several days in 13% of visits, more than half the days in 4% of visits, and nearly every day in 3% of visits.
Suicidal ideation varied by gender and race/ethnicity. Male patients who completed a PHQ9 were somewhat more likely to report suicidal ideation (PHQ9 item 9>0) than were female patients (23% of encounters vs. 19%). Rates of reported suicidal ideation were similar across age groups (ranging from 11% to 22%). Suicidal ideation varied slightly by race/ethnicity, with encounters with Hispanic (19%) and non-Hispanic white (20%) patients less likely to be associated with suicidal ideation than encounters with patients of other self-identified racial and ethnic groups (22–25%).
As expected, suicidal ideation varied by severity of depression symptoms. For example, suicidal ideation was uncommon (4%) in encounters where patients reported minimal symptoms of depression, and increasingly common as depression severity increased; suicidal ideation was reported in 11% of encounters with patients with mild depression, 24% of encounters with patients with moderate depression, and 47% of encounters with patients with moderately-severe to severe depression. Suicidal ideation was more likely to be reported in encounters in mental health clinics (24%) than those in primary care clinics (17%).
Suicide Attempts
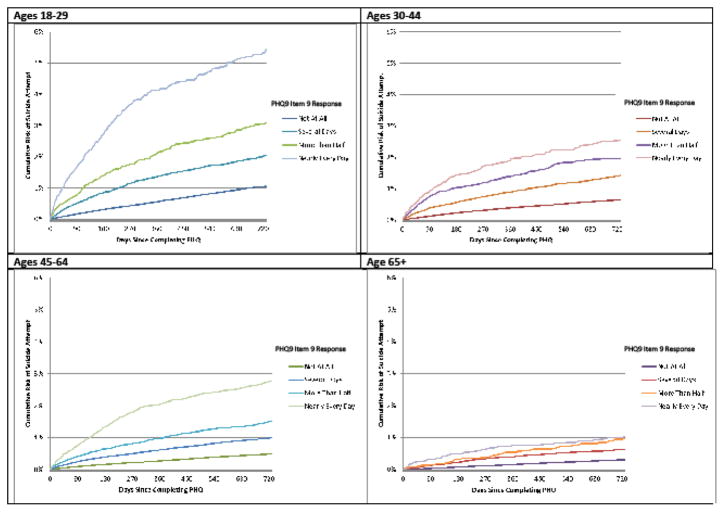
The cumulative hazard of suicide attempts by age group is illustrated in Figure 1. The absolute risk of suicide attempts generally declined with age. However, the relationship between suicide attempts and reported suicidal ideation was similar across age groups. Patients who reported more frequent thoughts of self-harm were at increased risk of acting on those thoughts regardless of age. The risk of suicide attempts in those with nearly daily thoughts of self-harm persisted over two years of follow-up. At two years, the cumulative hazard of suicide attempt ranged from approximately 5% in young adults who reported nearly daily suicidal ideation to 1% in those over age 65 who reported nearly daily suicidal ideation.
FIGURE 1. Cumulative risk of suicide attempts in the days following PHQ9 completion, grouped by age.
Question 9 of the PHQ9 asks about thoughts of being better off dead or of hurting oneself in some way over the last two weeks. Response options include “not at all,” “several days,” “more than half the days,” or “nearly every day”. Models adjusted for gender, healthcare system, patient mental health treatment status, visit type, Charlson score and race/ethnicity.
The estimated hazard ratios for suicide attempts for different age groups and frequency of suicidal ideation, if any, are summarized in Table 2. Across all age groups, the risk of suicide attempt increased with a higher frequency of reported suicidal ideation. Compared to those who did not report any thoughts of self-harm, those who reported such thoughts nearly every day were 4.9 to 8.2 times more likely to attempt suicide within 30 days, and 2.2 to 3.6times more likely to attempt suicide within 365 days. Patients with any level of suicidal ideation (PHQ9 item 9 >0) were approximately three times more likely to attempt suicide in the next 30 days, and nearly twice as likely to attempt suicide in the following year. There was no significant interaction between suicidal ideation and age for suicide attempts (p=0.116).
Table 2. Hazard ratios for suicide attempts at 30 days and 365 days after completion of the PHQ9 by age group.
Question 9 of the PHQ9 asks about thoughts of being better off dead or of hurting oneself in some way over the last two weeks. Response options include “not at all” (Q9=0), “several days” (Q9=1), “more than half the days” (Q9=2), or “nearly every day” (Q9=3).*
| Age Group | PHQ9 item 9 score | 30 Days | 365 Days | ||
|---|---|---|---|---|---|
|
| |||||
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | ||
| Ages 18–29 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.49 | 2.08–2.98 | 1.53 | 1.29–1.82 | |
| Q9=2 | 3.95 | 3.08–5.07 | 1.91 | 1.48–2.47 | |
| Q9=3 | 7.61 | 5.52–10.49 | 3.37 | 2.42–4.70 | |
| Q9>0 | 3.42 | 2.83–4.14 | 1.79 | 1.48–2.17 | |
| Ages 30–44 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.63 | 2.19–3.16 | 1.62 | 1.36–1.93 | |
| Q9=2 | 4.22 | 3.31–5.39 | 2.04 | 1.61–2.59 | |
| Q9=3 | 5.61 | 4.26–7.39 | 2.49 | 1.90–3.25 | |
| Q9>0 | 3.34 | 2.83–4.14 | 1.75 | 1.47–2.08 | |
| Ages 45–64 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.49 | 2.10–2.94 | 1.53 | 1.30–1.81 | |
| Q9=2 | 4.12 | 3.32–5.13 | 1.99 | 1.59–2.49 | |
| Q9=3 | 8.19 | 6.25–10.72 | 3.63 | 2.71–4.85 | |
| Q9>0 | 3.59 | 3.03–4.26 | 1.88 | 1.59–2.23 | |
| Ages 65+ | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.71 | 2.08–3.55 | 1.67 | 1.28–2.19 | |
| Q9=2 | 4.28 | 2.98–6.14 | 2.07 | 1.42–3.01 | |
| Q9=3 | 4.86 | 3.25–7.29 | 2.16 | 1.43–3.25 | |
| Q9>0 | 3.35 | 2.59–4.34 | 1.75 | 1.35–2.29 | |
p=0.116
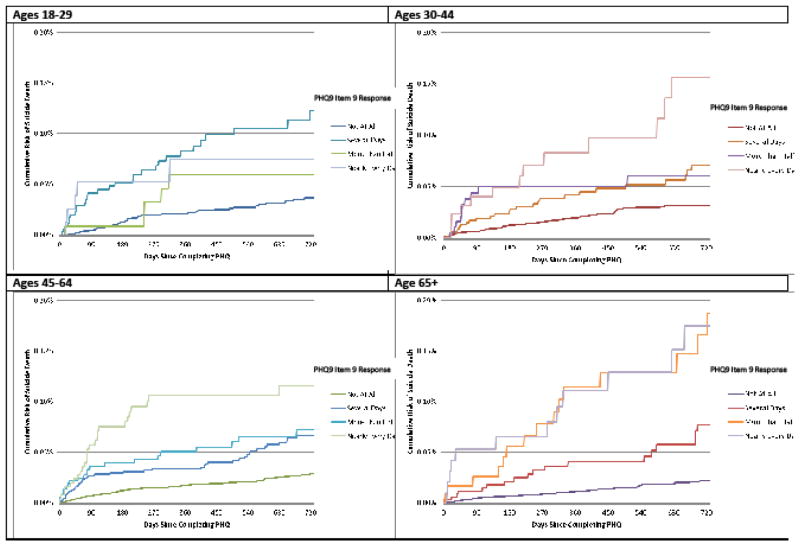
Suicide Deaths
The cumulative hazard of suicide deaths by age group is shown in Figure 2. In contrast to suicide attempts, the absolute risk of suicide death generally increased with age. Similar to attempts, the relationship of suicide deaths to the frequency of reported suicidal ideation remained similar across age groups, with those reporting more frequent thoughts of self-harm at increased risk of death from suicide regardless of age. The risk of suicide death persisted over two years following PHQ9 completion; at two years, the cumulative hazard of suicide death ranged from 0.12% in young adults to 0.18% in older adults.
FIGURE 2. Cumulative risk of suicide deaths in the days following PHQ9 completion, grouped by age.
Question 9 of the PHQ9 asks about thoughts of being better off dead or of hurting oneself in some way over the last two weeks. Response options include “not at all,” “several days,” “more than half the days,” or “nearly every day”. Models adjusted for gender, healthcare system, patient mental health treatment status, visit type, Charlson score and race/ethnicity.
Those who reported nearly daily thoughts of self-harm were 3.3- to 10.8-times more likely to die by suicide within 30 days of the completed PHQ9 (Table 3), and 1.7- to 5.7-times more likely to die by suicide within a year, compared to those without suicidal ideation. Patients with any level of suicidal ideation (PHQ9 item 9 >0) were 3-to-7 times more likely to die by suicide in the next 30 days, and 2-to-4 times as likely to die by suicide in the following year. There was no significant interaction between suicidal ideation and age for the risk of death from suicide (p=0.346).
Table 3. Hazard ratios for suicide deaths at 30 days and 365 days after completion of the PHQ9 by age group.
Question 9 of the PHQ9 asks about thoughts of being better off dead or of hurting oneself in some way over the last two weeks. Response options include “not at all” (Q9=0), “several days” (Q9=1), “more than half the days” (Q9=2), or “nearly every day” (Q9=3).*
| Age Group | PHQ9 item 9 score | 30 Days | 365 Days | ||
|---|---|---|---|---|---|
|
| |||||
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | ||
| Ages 18–29 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 3.94 | 1.81–8.56 | 2.58 | 1.35–4.91 | |
| Q9=2 | 2.27 | 1.10–4.69 | 1.04 | 0.44–2.46 | |
| Q9=3 | 3.29 | 1.62–6.68 | 1.74 | 0.85–3.57 | |
| Q9>0 | 3.46 | 2.05–5.87 | 1.98 | 1.22–3.22 | |
| Ages 30–44 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.30 | 1.27–4.15 | 1.50 | 0.76–2.98 | |
| Q9=2 | 3.14 | 1.25–7.89 | 1.45 | 0.58–3.62 | |
| Q9=3 | 5.69 | 2.62–12.34 | 3.00 | 1.29–7.01 | |
| Q9>0 | 2.93 | 1.71–5.00 | 1.67 | 0.93–2.99 | |
| Ages 45–64 | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 2.87 | 1.66–4.98 | 1.88 | 1.17–3.01 | |
| Q9=2 | 3.43 | 1.50–7.85 | 1.58 | 0.79–3.15 | |
| Q9=3 | 5.63 | 2.69–11.81 | 2.97 | 1.39–6.36 | |
| Q9>0 | 3.36 | 1.95–5.77 | 1.92 | 1.22–3.02 | |
| Ages 65+ | Q9=0 | [reference] | [reference] | ||
| Q9=1 | 4.22 | 2.05–8.65 | 2.76 | 1.36–5.60 | |
| Q9=2 | 12.95 | 4.57–36.68 | 5.96 | 1.54–23.04 | |
| Q9=3 | 10.81 | 3.63–32.17 | 5.70 | 1.65–19.70 | |
| Q9>0 | 6.97 | 3.04–15.96 | 3.98 | 1.56–10.12 | |
p=0.346
Models adjusted for gender, healthcare system, patient mental health treatment status, visit type, Charlson score and race/ethnicity.
DISCUSSION
Suicidal ideation, as assessed by item 9 of the PHQ9, was a robust predictor of suicide attempts and deaths regardless of age in this very large and diverse sample of adult outpatients. The absolute risk of suicide attempt generally declined with age, while the absolute risk of suicide death generally increased with age. However, the relationships between suicidal ideation and suicide attempts and deaths were similar across all age groups. The risk of suicide attempts and deaths was highest in the first 30 days following patients’ reports of suicidal ideation but remained elevated for at least two years.
We are not aware of other studies that have examined the relationship between suicidal ideation as measured by item 9 of the PHQ9 and suicide attempts or deaths by age groups. Two studies18,19 have examined the general association between item 9 of the PHQ9 and subsequent suicide attempts and deaths, but did not examine this association by age. One study18 was done at Group Health by Simon and colleagues and included outpatients cared for at Group Health, one of the four sites in our study, between 2007 and 2011 (our study included data from 2010 to 2012). The other study19 by Louzon and colleagues used national data for patients cared for by the Veterans Health Administration. Both studies found that response to item 9 of the PHQ9 identified patients at increased risk for suicide attempts and deaths, similar to our study. Additionally, these two studies found that the risk for suicide attempts and deaths was still elevated at least one year after PHQ9 completion, while our data show that this risk is sustained for at least two years. These findings together support understanding suicide to be a persistent susceptibility, rather than a short-term crisis, and healthcare systems should take this into account as they formulate their suicide prevention strategies.
Studies that have used measures other than the PHQ9 to assess suicidal ideation have found associations between suicidal ideation and subsequent suicide attempts that were similar to our findings. One study identified suicidal ideation using the Scale for Suicide Ideation,20 a 19-item scale with each item scored by patients from 0 to 2, so total scores range from 0 to 38. Items ask about such things as wish to die, desire to make a suicide attempt, and duration and frequency of suicidal ideation. Participants were 6,891 psychiatric outpatients consecutively evaluated at University of Pennsylvania. Patients who scored a 3 or higher were found to have a hazard ratio of 2.80 (95% CI: 1.44–5.45) for suicide attempt in the 20 years following administration of the scale.21 In another study of 3481 participants in the 13-year follow-up of the Baltimore sample of the NIMH Epidemiologic Catchment Area survey, people who reported suicidal ideation at baseline (assessed via a single item question asking “Have you ever felt so low you thought of committing suicide?”) were much more likely to report a suicide attempt at follow-up (RR=6.09, 95% CI: 2.58–14.36).22 Our findings are consistent with both of these studies and confirm the association between suicidal ideation and suicide attempts on a much larger scale in a geographically and ethnically diverse population of outpatients.
Similar to other studies and national databases 7,8,10,23–25, we found that suicide attempts and deaths differed by age. Younger (ages 18–29) and middle-aged (ages 45–64) patients made suicide attempts more frequently, while suicide death rates were lowest in the youngest (ages 18–29) and highest in the oldest (ages 65 and older) patients. Suicide attempts and deaths were highest for patients in all age groups who reported nearly daily thoughts of suicide. However, there was still elevated risk for both attempts and deaths in those who reported experiencing suicidal ideation several days or more than half the days in the past two weeks, and the risk for those who denied suicidal thoughts was not zero. The 2-year cumulative hazard of suicide attempts for those who denied thoughts of suicide in the previous 2 weeks was 1% in 18–29 year-olds and less than 1% in other age groups. These findings support the idea of targeting those who report thoughts of suicide on the PHQ9 for both short-term and sustained suicide prevention outreach, but also suggest a need to better understand why patients who deny suicidal ideation go on to attempt or die by suicide. It may be that these patients are intentionally misleading clinicians to prevent intervention or they may be answering this question truthfully but go on to experience suicidal ideation at a later date or make an impulsive suicide attempt.
There is an emerging body of work examining what may increase the risk of translating suicidal thoughts into suicidal behaviors in at-risk populations. In our study, we found that frequency of suicidal ideation as reported on the PHQ9 to be a strong predictor of suicide attempts and deaths, with patients who reported suicidal thoughts nearly every day at 5-to-8 times the risk for suicide attempts and 3-to-11 times the risk for suicide deaths within 30 days compared to those who did not report thoughts of suicide. Several studies have found depression severity, substance use disorders, and comorbid anxiety to be significant predictors of suicide attempts in people with suicidal ideation.26,27 Results are a bit more mixed with personality disorders, with one study finding cluster B personality disorders (antisocial, borderline, histrionic or narcissistic personality disorders) to be significant predictors of suicide attempts in people with depression or dysthymia and suicidal ideation (RR=3.14, 95% CI: 1.36–7.25, p=0.007),28 while another study found no association between suicide attempts and borderline personality disorder in people with suicidal ideation.27 Certainly, discerning risk for an individual patient versus populations of people who share certain characteristics can be difficult at best, and much more work is needed in this area to help providers better assess individual risk in clinical settings.
There are several potential limitations to our study. First, it should be noted that the PHQ9 was designed to screen for depression and assess its severity, not to assess risk for suicide. We do not have measures of additional ways, beyond the PHQ9, that people may have communicated thoughts of suicide to their care teams, which a recent meta-analysis estimated is done in some form by approximately 45% people who go on to die by suicide.29. However, even with this somewhat limited measure of suicidal ideation, we have found item 9 of the PHQ9 to be a robust predictor of suicide attempts that can guide clinical care. Second, our study sample included only those adult outpatients were receiving care for mental health conditions and completed a PHQ9, possibly limiting the generalizability of our sample to the general population. However, with increasing use of the PHQ9 in clinical settings, we think our sample is largely representative of populations that will be monitored with the PHQ9 in outpatient settings. Third, as our study relied on ICD-9 codes to identify suicide attempts, we likely included some false positive (and missed some false negative) events in our sample. However, as noted in our methods section, our process of identifying suicide attempts has a weighted average positive predictive value of 92%,15 which should lead to relatively few misclassifications. Additionally, we only have access to data available for medically-treated suicide attempts, meaning that we almost certainly underestimated suicide attempts. Fourth, despite our large sample size, suicide deaths were fairly rare events, limiting our ability to assess any dose-dependent relationship between degree of suicidal ideation as measured by the PHQ9 and suicide death. Finally, these data may be helpful in predicting risk of suicide attempts and deaths in a population of medical outpatients, but may not be helpful in predicting any individual patient’s risk. Overall, we think any potential limitations of these data are outweighed by the unique opportunity to better understand the predictive value of item 9 of the PHQ9 in a very large and diverse population.
Regardless of age, people with suicidal ideation are at much greater risk of suicide attempts and deaths, particularly if they report nearly daily thoughts of self-harm, and this risk continues over the subsequent two years. Healthcare systems should have programs in place to address both the immediate and sustained risk for suicide for patients of all ages. Such programs will need to be effective yet low-cost to be sustainable on the large scale needed to prevent suicide attempts and deaths at the population level. To this end, we are currently conducting a pragmatic trial that compares the effectiveness of a coach-facilitated online dialectical behavioral therapy program to a care management intervention that uses primarily emailed communication, with both compared to usual care.30 This study will ultimately randomize approximately 18,000 patients who score a 2 or 3 on item 9 of the PHQ9 at three of our healthcare systems (Group Health in Seattle, HealthPartners in Minneapolis, and Kaiser Colorado in Denver). Our findings from this trial may help us determine how to better address both the immediate and sustained risk for suicide for patients of all ages following a positive report of suicidal ideation.
Highlights.
The Joint Commission recommends all patients be screened for suicide
Nearly daily suicidal ideation on PHQ9 predicted risk of suicide attempts and deaths
Suicidal ideation was a robust predictor of suicide attempts and deaths in all ages
Risk of suicide attempts and deaths persisted over two years
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1. [Accessed June 1, 2016];CDC Increase in Suicide in the United States, 1999–2014. http://www.cdc.gov/nchs/products/databriefs/db241.htm?version=meter+at+1&module=meter-Links&pgtype=article&contentId=&mediaId=&referrer=&priority=true&action=click&contentCollection=meter-links-click.
- 2. [Accessed January 10, 2017];Suicide: Facts at a glance. 2015 https://www.cdc.gov/violenceprevention/pdf/suicide-datasheet-a.pdf.
- 3.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LeFevre ML Force USPST. Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(10):719–726. doi: 10.7326/M14-0589. [DOI] [PubMed] [Google Scholar]
- 5.Simon GE, Coleman KJ, Rossom RC, et al. Risk of suicide attempt and suicide death following completion of the Patient Health Questionnaire depression module in community practice. J Clin Psychiatry. 2016;77(2):221–227. doi: 10.4088/JCP.15m09776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sentinel Event Alert 56: Detecting and treating suicide ideation in all settings. The Joint Commission; 2016. [PubMed] [Google Scholar]
- 7.Injury Prevention & Control: Data & Statistics. [Accessed November 13, 2015];Fatal Injury Reports. http://www.cdc.gov/injury/wisqars/fatal.html.
- 8.American Foundation for Suicide Prevention. [Accessed June 1, 2016];Suicide Statistics. https://afsp.org/about-suicide/suicide-statistics/
- 9. [Accessed May 13, 2016];Web-based Injury Statistics Query and Reporting System (WISQARS) http://www.cdc.gov/injury/wisqars/index.html.
- 10.Sullivan EMA, JL, Luo F, Simon TR, Dahlberg LL. Suicide Among Adults Aged 35–36 Years – United States, 1999–2010. MMWR. (2013) 2013;62:321–325. [PMC free article] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ross TRND, Brown JS, Pardee R, Hornbrook MC, Hart G, Steiner JF. The HMO Research Network Virtual Data Warehouse: A Public Data Model to Support Collaboration. eGEMs (Generating Evidence & Methods to Improve Patient Outcomes) 2014;2(1) doi: 10.13063/2327-9214.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21(6):547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 15.Simon GE, Savarino J. Suicide attempts among patients starting depression treatment with medications or psychotherapy. Am J Psychiatry. 2007;164(7):1029–1034. doi: 10.1176/ajp.2007.164.7.1029. [DOI] [PubMed] [Google Scholar]
- 16.Zheng Y, Heagerty PJ. Partly conditional survival models for longitudinal data. Biometrics. 2005;61(2):379–391. doi: 10.1111/j.1541-0420.2005.00323.x. [DOI] [PubMed] [Google Scholar]
- 17.Lin DY, Wei LJ. The robust inference for the proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 18.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Louzon SA, Bossarte R, McCarthy JF, Katz IR. Does Suicidal Ideation as Measured by the PHQ-9 Predict Suicide Among VA Patients? Psychiatr Serv. 2016;67(5):517–522. doi: 10.1176/appi.ps.201500149. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 21.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- 22.Kuo WH, Gallo JJ, Tien AY. Incidence of suicide ideation and attempts in adults: the 13-year follow-up of a community sample in Baltimore, Maryland. Psychol Med. 2001;31(7):1181–1191. doi: 10.1017/s0033291701004482. [DOI] [PubMed] [Google Scholar]
- 23.Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 25.Moscicki EK, O’Carroll P, Rae DS, Locke BZ, Roy A, Regier DA. Suicide attempts in the Epidemiologic Catchment Area Study. Yale J Biol Med. 1988;61(3):259–268. [PMC free article] [PubMed] [Google Scholar]
- 26.Bolton JM, Pagura J, Enns MW, Grant B, Sareen J. A population-based longitudinal study of risk factors for suicide attempts in major depressive disorder. J Psychiatr Res. 2010;44(13):817–826. doi: 10.1016/j.jpsychires.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sokero TP, Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Isometsa ET. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. 2003;64(9):1094–1100. doi: 10.4088/jcp.v64n0916. [DOI] [PubMed] [Google Scholar]
- 28.May AM, Klonsky ED, Klein DN. Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. J Psychiatr Res. 2012;46(7):946–952. doi: 10.1016/j.jpsychires.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pompili M, Belvederi Murri M, Patti S, et al. The communication of suicidal intentions: a meta-analysis. Psychol Med. 2016;46(11):2239–2253. doi: 10.1017/S0033291716000696. [DOI] [PubMed] [Google Scholar]
- 30.Simon GE, Beck A, Rossom R, et al. Population-based outreach versus care as usual to prevent suicide attempt: study protocol for a randomized controlled trial. Trials. 2016;17(1):452. doi: 10.1186/s13063-016-1566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]