Abstract
Introduction
This study's aims are to identify whether a relationship between statin use and rate of cognitive decline exists. The relationship between statins and mild cognitive impairment (MCI) has been investigated in the past with the evidence showing mixed results.
Methods
Seven hundred sixty-eight subjects were identified with MCI. Subjects were stratified into six possible groups according to apolipoprotein E (APOE) ε4 allele status and statin use and assessed for decline in cognitive function.
Results
All cognitive assessments trended toward less decline with statin use. Alzheimer’s Disease Assessment Scale 11 (ADAS 11) showed the biggest difference in mean change between statin users and nonusers (−0.82 vs. −1.22, respectively). Change reached marginal significance on the ADAS 11 when stratified by APOE ε4–negative subjects.
Discussion
All cognitive assessments trended toward less decline when subjects were concurrently treated with a statin, supporting the position that statins do not have a net negative effect on cognitive assessment and suggesting a potential treatment benefit.
Keywords: Statin, Alzheimer's disease, Mild cognitive impairment, ADAS, ADNI
1. Introduction
Alzheimer's disease (AD) is increasingly prevalent in the United States. As of 2015, there are an estimated 5.3 million individuals in the United States suffering from AD. It also affects approximately 10% of the population over the age of 65 years [1]. The rate of mild cognitive impairment (MCI) progressing to dementia when thought to be of neurodegenerative origin is approximately 10% per year. The rate of decline on the Mini-Mental State Examination (MMSE) in AD is approximated at 3 to 3.5 points per year. In rapidly progressive cases, decline can reach 5–6 points annually [2]. Mean survival after diagnosis of AD ranges from 3–8 years [2].
The direct effects of plasma cholesterol and related lipoproteins on the incidence of dementia and cognitive decline have long been controversial. Senile neuritic plaques and neurofibrillary tangles are the pathogenic hallmarks of AD, and increasing evidence links brain cholesterol with both plaques and tangles [3]. Recent studies have shown a positive correlation between high-density lipoprotein (HDL) levels and MMSE performance and a negative correlation between low-density lipoprotein (LDL) levels and immediate and delayed recall [4]. Several epidemiological studies also showed that elevated total serum cholesterol was a significant risk factor for AD, independent of apolipoprotein E (APOE) allele status [2]. Lowering cholesterol levels via statins is associated with decreased β-amyloid [5].
Past studies noted that subjects with incident dementia had higher total cholesterol at their first visit [6]. Cholesterol levels and atherosclerosis have also been found to correlate with AD [7]. Increased glucose levels and decreased HDL levels increase risk of incident MCI [6]. High midlife total cholesterol has been associated with decreased memory and fluency later in life [8]. For this reason, statins have long been purported to play a role in cognitive decline; however, the general consensus on this role is mixed. Recent studies have shown that statin use is associated with a reduced risk of dementia. Specifically, lipophilic statins were found to have the greatest reduction in risk [9].
Evidence that statins decrease the risk of incident dementia is convincing from an epidemiological standpoint. Some studies show that statin users had a 5-fold lower risk of incident AD and a 3-fold lower risk of MCI [6]. Statins have also been shown to decrease the risk of AD in subjects younger than 80 years old, after controlling for sex, education level, and self-rated health [10]. There have been three major clinical trials investigating the role of statins in cognitive decline. The Collaborative Low-dose Aspirin Study in Pregnancy (CLASP) study in 2011 assessed the use of simvastatin in probable AD. It showed no significant difference in cognitive decline between statin therapy and a placebo when measured by the Alzheimer's Disease Assessment Scale—Cognitive Subscale (ADAS-Cog) [11]. The Lipitor's Effect in Alzheimer's Dementia (LEADe) trial in 2010 studied atorvastatin therapy in mild-to-moderate AD and showed no net benefit of statin therapy to placebo over 72 weeks [12]. This study focused on ADAS-Cog and ADAS-Clinical Global Impression of Change as benchmarks. These two clinical trials contradict the initial findings by Sparks in 2005 that displayed a significantly decreased rate of cognitive decline by atorvastatin on ADAS-Cog and MMSE scores over 6 months [13]. These values were also near significant at the 12-month mark [13]. All three of these trials focused on subjects with AD. The Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) trial also showed that pravastatin had no significant effect on cognitive function in the elderly [14]. Clinical trial data on subjects with MCI do not exist. The severity of disease progression among the selected subject population may play a role. By focusing on individuals categorized as MCI, any relationship between progression of cognitive impairment and statin use should be teased out more easily.
The ADNI database has the unique attribute of possessing prospectively collected data, which have not been analyzed in past studies. Past epidemiological studies have focused on utilizing retrospectively gathered data. The focus of this study will be to assess whether or not cognitive decline is affected by a statin regimen. Randomized controlled trials suggest that the dementia stage of AD may be too late for significant benefits of statin therapy [15]. To assess cognitive decline at an earlier time point in disease progression, it is necessary to study subjects that have not progressed to AD. MCI is an ideal population to assess whether or not early intervention with a statin will be beneficial.
2. Methods
Data used in the preparation of this article were obtained from the Alzheimer's Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). The ADNI was launched in 2003 as a public-private partnership, led by principal investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging, positron emission tomography, other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of MCI and early AD.
ADNI's data requisition website was the source of all data. The analysis focused on information contained within a summary file that ADNI had compiled and a medication file containing home medications for each subject. These files were the ADNIMERGE and RECCMEDS data files, respectively. This list was used to isolate any subject that had been prescribed a statin. Each subject was included in the database regardless of statin type or dose. No other lipid-lowering medications were considered when data were being collected; however, patients concurrently on other lipid-lowering agents were not excluded from analysis. Of the 1737 subjects contained within the ADNIMERGE file, 939 were identified as statin users after cross-referencing with the RECCMEDS file. Statins queried include atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin.
ADNI's summary file was then used to isolate any subject within the database who was labeled as having a diagnosis of MCI. ADNI has classified each subject into various levels of cognition based on the Petersen criteria for MCI [16]. The two levels of progression that we decided to include in our definition of MCI were the early and late MCI. Within these categories, 872 subjects were identified with a diagnosis of MCI. These two parameters (statin status and MCI status) formed the major categorical parameters for isolating data. MCI status formed our inclusion criteria, and statin status formed the dividing line between control and test groups.
All enrolled subjects or their legal representatives sign a written informed consent approved by an Institutional Review Board (Western Institutional Review Board, Puyallup, WA). Annual visits and examinations for cognition and criteria for clinical diagnoses are as previously described. All assessments were conducted in accordance with the Declaration of Helsinki.
All subjects who had two cognitive assessments at least 1 year apart were then identified. This would make a valuation of cognitive change over a 1-year period possible and assess whether or not statins played a role in rate of change. Among the 872 subjects with a past diagnosis of MCI, 768 subjects also had greater than 1 year of cognitive assessment.
Finally, to formulate the parameters for each test group, we evaluated subjects' APOE ε4 allele status. Within the ADNI database, each subject was labeled as a 0, 1, or 2 depending on how many APOE ε4 alleles he or she carried. A status of 0 correlates to homozygous negative for APOE ε4(−/−), 1 correlates to heterozygous for APOE ε4(+/−), and 2 correlates to homozygous positive for APOE ε4(+/+).
This final parameter was cross-referenced with each subject's statin status to yield six total groups:
-
1.
MCI, APOE ε4(−/−), statin negative (n = 179),
-
2.
MCI, APOE ε4(−/−), statin positive (n = 198),
-
3.
MCI, APOE ε4(+/+), statin negative (n = 26),
-
4.
MCI, APOE ε4(+/+), statin positive (n = 60),
-
5.
MCI, APOE ε4(+/−), statin negative (n = 120), and
-
6.
MCI, APOE ε4(+/−), statin positive (n = 185).
These six groups were then analyzed in three separate iterations. First, the data were analyzed as two large groups: MCI statin positive and MCI statin negative. These groups had 443 and 325 subjects, respectively. The analysis of these two groups would yield information on the effect statins have on MCI independent of APOE ε4 status. We then performed a second analysis comparing MCI, APOE ε4 (+/+), statin positive versus MCI, APOE ε4 (+/+), statin negative (245 and 146 subjects, respectively), and a second group comparing MCI APOE ε4 (−/−) statin positive versus MCI, APOE ε4 (−/−), statin negative (198 and 179 subjects, respectively). In this iteration, APOE ε4 (+/−) and APOE ε4 (+/+) were lumped together in the APOE ε4 (+/+) category. The final analysis compared the six groups shown previously. ApoE4 trait, carriers, and negatives were used as controls comparing the effects statins had on each group.
Each subject was analyzed by multiple forms of cognitive assessment yielding up to four possible cognitive assessments: The Alzheimer's Disease Assessment Scale 11 (ADAS 11), ADAS 13 (ADAS 13), MMSE, and Montreal Cognitive Assessment (MoCA). Each subject is given baseline scores for each cognitive assessment at the time of being entered into the ADNI database. These scores were compared with future cognitive assessment as close as possible to 1 year in the future. This cognitive change was the value used to assess significance.
The data were then reassessed in a mixed-effects model while controlling for age, sex, ethnicity, and marital status. This analysis consisted of the same six iterations as stated previously; however, it used all data points based on how many years past baseline they occurred.
2.1. Statistical methods
Demographic characteristics of statin users and nonusers were evaluated using descriptive statistics, including means, standard deviations, frequencies, and proportions. Two-sample t-tests were implemented to determine differences in means between statin users and nonusers. Furthermore, chi-squared analysis was employed to test differences in proportions. Means and standard deviations of outcome differences from baseline were assessed in statin users and nonusers. Two-sample t-tests were used to determine differences in outcome change from baseline. To investigate whether the APOE ε4 status confounded the results, we assessed means and standard deviations of outcome differences from baseline between statin users and nonusers in strata defined by APOE ε4 status (APOE ε4 negative or APOE ε4 positive). Further analyses were performed within the APOE ε4–positive stratum by further stratifying by ApoE4 trait status (APOE ε4[+/−] or APOE ε4[+/+]). Finally, the generalized mixed-effects model was implemented to estimate the mean differences of the primary outcomes between the six APOE ε4/statin groups with “MCI, APOE ε4(−/−), statin negative” as our reference group. The final model adjusted for age, sex, ethnicity, marital status, and time from baseline. Furthermore, the interaction group, APOE ε4/statin group × time, was added to the model to ascertain whether the time from baseline modifies the association between APOE ε4/statin status and the primary outcomes. Unless stated otherwise, P values <.05 were deemed statistically significant. All analyses were conducted using Stata Statistical Software (Version 14, StataCorp, College Station, TX).
3. Results
3.1. Overall demographics
Subjects' demographic characteristics are shown in Table 1. The mean age of the statin user and nonuser population was 73 years of age. However, 62% of the statin population was male compared with 55% in the nonuser population. The statin user population consisted mostly of non-Hispanic subjects (98.2%) and Caucasian subjects (93.5%). Similarly, the non-Hispanic and Caucasian subjects were the highest percentage within the statin nonuser population (94.8% and 94.5%, respectively). Sex and ethnicity showed statistically significant differences in proportions between the statin user and nonuser categories (P = .046 and P = .008, respectively) (Table 1).
Table 1.
Demographics
| Variables | Statin use (n = 443) | No statin use (n = 325) | P values∗ |
|---|---|---|---|
| Demographics | |||
| Age (y), mean (SD) | 73.0 (7.4) | 72.9 (7.7) | .81 |
| Sex (male, %) | 273 (61.6) | 177 (54.5) | .046 |
| Ethnicity | .008 | ||
| Hispanic/Latino | 8 (1.8) | 17 (5.2) | |
| Not Hispanic/Latino | 435 (98.2) | 308 (94.8) | |
| Race | .43 | ||
| Caucasian | 414 (93.5) | 307 (94.5) | |
| African-American | 11 (2.5) | 10 (3.1) | |
| Asian | 11 (2.5) | 3 (0.9) | |
| Other/unknown | 7 (1.6) | 5 (1.5) | |
| Marital status | .059 | ||
| Married | 357 (80.6) | 237 (72.9) | |
| Divorced | 33 (7.5) | 37 (11.4) | |
| Never married | 11 (2.5) | 7 (2.2) | |
| Widowed | 38 (8.6) | 43 (13.2) | |
| Unknown | 4 (0.9) | 1 (0.3) | |
| Education | .82 | ||
| High school | 73 (14.5) | 51 (15.7) | |
| Some college | 80 (18.1) | 63 (19.4) | |
| College graduate | 108 (24.3) | 71 (21.9) | |
| Graduate/professional | 182 (41.1) | 140 (43.1) | |
Abbreviation: SD, standard deviation.
P values are calculated using independent t test for continuous variables and chi-squared analysis for categorical variables.
3.2. MCI outcomes between statin users and nonusers
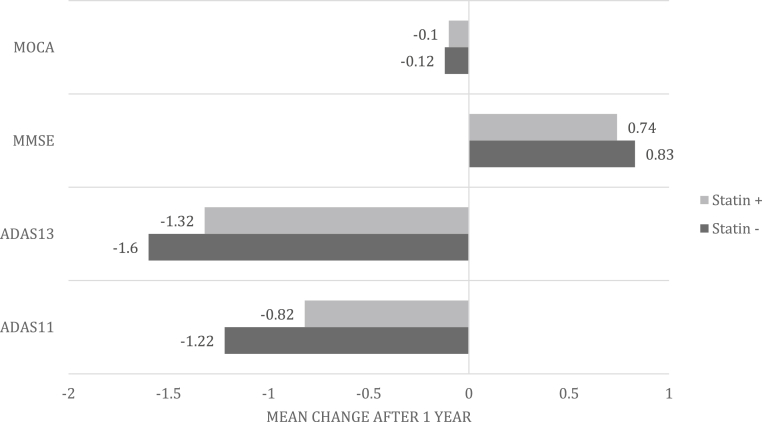
Differences in the mean change of MCI outcomes between statin users and nonusers are shown in Table 2 and Fig. 1. ADAS 11 showed the biggest difference in mean change between statin users and nonusers (−0.82 vs. −1.22, respectively), followed by ADAS 13 (−1.32 vs. −1.6, respectively). MMSE (statin positive = 0.74 vs. statin negative = 0.83) and MoCA (statin positive = −0.10 vs. statin negative = −0.12) showed the least differences in mean change from baseline. There were no statistically significant differences in mean change from baseline between statin users and statin nonusers.
Table 2.
Assessing the mean MCI change between statin users and nonusers stratified by APOE allele status
| Mean (SD) |
||||
|---|---|---|---|---|
| Variables | ADAS 11 (n = 762) | ADAS 13 (n = 761) | MMSE (n = 768) | MoCA (N = 414) |
| Regardless of APOE ε4 | ||||
| Statin+ | −0.82 (4.1) | −1.32 (5.3) | 0.74 (2.4) | −0.10 (3.8) |
| Statin− | −1.22 (4.5) | −1.6 (6.1) | 0.83 (2.4) | −0.12 (3.1) |
| P value∗ | .20 | .50 | .62 | .96 |
| Required sample size† | 3142 | 12,116 | N/A | N/A |
| APOE ε4+ | ||||
| Statin+ | −1.3 (4.3) | −1.9 (5.8) | 0.99 (2.5) | 0.22 (3.5) |
| Statin− | −1.6 (4.8) | −2.4 (6.7) | 1.4 (2.5) | 0.22 (2.8) |
| P value∗ | .59 | .46 | .12 | .99 |
| Required sample size† | N/A | 4524 | 1170 | N/A |
| APOE ε4− | ||||
| Statin+ | −0.18 (3.8) | −0.57 (4.5) | 0.43 (2.2) | −0.46 (4.1) |
| Statin− | −0.93 (4.3) | −0.95 (5.4) | 0.36 (2.3) | −0.36 (3.2) |
| P value∗ | .07 | .47 | .74 | .84 |
| Required sample size† | 896 | 3782 | N/A | N/A |
| APOE ε4(+/+) | ||||
| Statin+ | −1.6 (4.4) | −2.5 (5.3) | 1.2 (2.6) | 0.88 (2.5) |
| Statin− | −2.9 (5.5) | −3.8 (6.1) | 2.1 (2.3) | 1.2 (3.5) |
| P value∗ | .23 | .32 | .15 | .74 |
| Required sample size† | 468 | 564 | 246 | N/A |
| APOE ε4(+/−) | ||||
| Statin+ | −1.3 (4.3) | −1.7 (5.9) | 0.92 (2.5) | 0.04 (3.7) |
| Statin− | −1.3 (4.6) | −2.1 (6.8) | 1.3 (2.5) | −0.03 (2.6) |
| P value∗ | .93 | .63 | .25 | .89 |
| Required sample size† | N/A | N/A | 1362 | N/A |
Abbreviations: ADAS 11, Alzheimer's Disease Assessment Scale 11; ADAS 13, Alzheimer's Disease Assessment Scale 13; MCI, mild cognitive impairment; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; N/A, not available; SD, standard deviation.
P value and crude mean differences are calculated using the independent t test.
Total sample size required to achieve 80% power with α 0.05 and 1:1 ratio between statin+ and statin−.
Fig. 1.
Mean outcome changes between statin users and statin nonusers.
3.3. MCI outcomes stratified by APOE ε4 positive versus negative
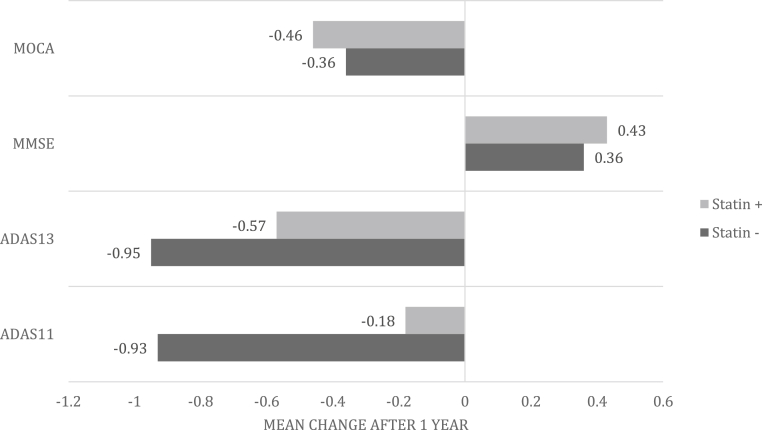
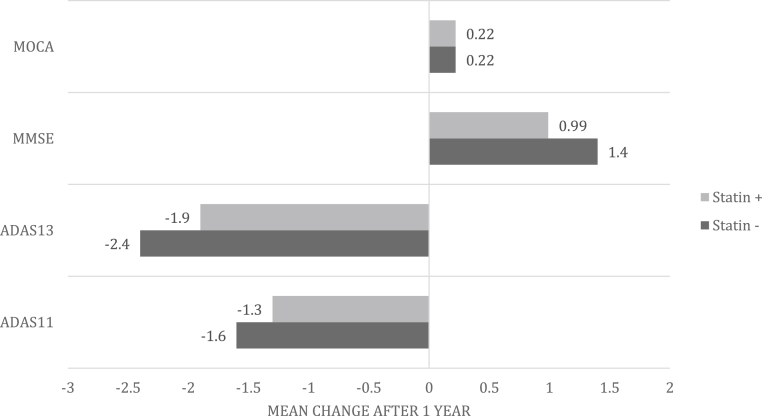
Among the subjects who were APOE ε4 positive, ADAS 13 showed the biggest difference in mean change from baseline between statin users and nonusers (statin positive = −1.9 vs. statin negative = −2.4), followed by MMSE (statin positive = 0.99 vs. statin negative = 1.4) and ADAS 11 (statin positive = −1.3 vs. statin negative = −1.6). MoCA did not show any differences in mean change between statin users and nonusers (statin positive = 0.22 vs. statin negative = 0.22). The differences in mean change from baseline for the outcomes were not statistically significant (Table 2 and Fig. 2, Fig. 3). Among the APOE ε4–negative subjects, ADAS 11 presented a marginally significant difference in mean change from baseline between statin users and nonusers (statin positive = −0.18 vs. statin negative = −0.93, P = .07). However, the differences in the mean changes of ADAS 13 (statin positive = −0.57 vs. statin negative = −0.95), MMSE (statin positive = 0.43 vs. statin negative = 0.36), and MoCA (statin positive = −0.46 vs. statin negative = −0.36) between statin users and nonusers were not statistically significant (Table 2 and Fig. 2, Fig. 3).
Fig. 2.
Mean outcome changes between statin users and statin nonusers among APOE ε4–negative subjects.
Fig. 3.
Mean outcome changes between statin users and statin nonusers among APOE ε4–positive subjects.
3.4. MCI outcomes stratified by APOE ε4(+/−) versus APOE ε4(+/+)
After further stratification of the APOE ε4-positive group into APOE ε4(+/−) (allele carrier) and APOE ε4(+/+) (allele trait), ADAS 11 and ADAS 13 presented the biggest differences in mean cognitive outcome changes from baseline among the APOE ε4(+/+) subject population (statin positive = −1.6 vs. statin negative = −2.9 and statin positive = −2.5 vs. statin negative = −3.8, respectively), followed by MMSE (statin positive = 1.2 vs. statin negative = 2.1) and MoCA (statin positive = 0.88 vs. statin negative = 1.2). Although the differences in the mean change are clinically relevant, the differences were not statistically significant (Table 2). Subjects who are APOE ε4 carriers yielded differences in mean change from baseline in ADAS 13 (statin positive = −1.7 vs. statin negative = −2.1), MMSE (statin positive = 0.92 vs. statin negative = 1.3), and MoCA (statin positive = 0.04 vs. statin negative = −0.03). ADAS 11 showed changes of −1.3 in statin users and nonusers.
3.5. Mixed-effects model estimating mean difference in outcomes
The mixed-effects model showing the mean differences between APOE ε4/statin status and ADAS 11, ADAS 13, MMSE, and MoCA, respectively, are reported in Table 3. After adjustment for selected covariates, the mean differences of ADAS 11 scores relative to the reference group were greater within the statin-negative groups (APOE ε4 [+/+], statin-negative β [95% confidence interval {CI}] = 1.53 [0.28, 2.78], APOE ε4 [+/−], statin-negative β = 2.13 [−0.17, 4.45]) compared with the statin-positive groups (APOE ε4 [−/−], statin-positive β [95% CI] = −0.85 [−1.95, 0.25], APOE ε4 [+/+], statin-positive β [95% CI] = 0.72 [−0.42, 1.86], APOE ε4 [+/−], statin-positive β [95% CI] = 1.48 [−0.16, 2.14]). Similar trends are reported with ADAS 13, MMSE, and the MoCA as our primary outcome that indicates statins are positively affecting cognitive impairment relative to the scores. Finally, our analysis shows that the covariate of time significantly modifies the association between APOE ε4/statin and ADAS 11 (β [95% CI] = 0.45 [0.39, 0.51]), ADAS 13 (β [95% CI] = 0.52 [0.46, 0.59]), MMSE (β [95% CI] = −0.25 [−0.27, −0.21]), and MoCA (β [95% CI] = −0.22 [−0.27, 0.18]), respectively (P < .001).
Table 3.
Mixed-effects model assessing the estimated mean difference of cognitive outcomes among APOE ε4/statin status
| Coefficient (95% CI) |
||||
|---|---|---|---|---|
| Variables | ADAS 11 | ADAS 13 | MMSE | MoCA |
| APOE ε4/statin groups | ||||
| APOE ε4 (−/−), statin negative | Ref | Ref | Ref | Ref |
| APOE ε4 (−/−), statin positive | −0.85 (−1.95, 0.25) | −0.93 (−2.50, 0.64) | 0.40 (−0.08, 0.88) | 0.76 (−0.10, 1.62)∗ |
| APOE ε4 (+/+), statin negative | 1.53 (0.28, 2.78)† | 2.95 (1.18, 4.73)† | −0.45 (−1.01, 0.09) | −1.12 (−2.13, −0.12)† |
| APOE ε4 (+/+), statin positive | 0.72 (−0.42, 1.86) | 1.85 (0.23, 3.47)† | −0.29 (−0.79, 0.21) | −0.43 (−1.36, 0.51) |
| APOE ε4 (+/−), statin negative | 2.13 (−0.17, 4.45)∗ | 4.35 (1.08, 7.63)† | −0.84 (−1.85, 0.17) | −1.91 (−3.71, −0.11)† |
| APOE ε4 (+/−), statin positive | 1.48 (−0.16, 2.14)∗ | 3.46 (1.13, 5.80)† | −0.27 (−1.00, 0.45) | −1.33 (−2.76, 0.09)∗ |
| Time (y) | 0.48 (0.35, 0.61)‡ | 0.71 (0.56, 0.86)‡ | −0.26 (−0.33, −0.20)‡ | −0.10 (−0.20, 0.006)∗ |
| APOE ε4/statin group × time interaction | 0.45 (0.39, 0.51)‡ | 0.52 (0.46, 0.59)‡ | −0.25 (−0.27, −0.21)‡ | −0.22 (−0.27, 0.18)‡ |
Abbreviations: ADAS 11, Alzheimer's Disease Assessment Scale 11; CI, confidence interval; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; Ref, reference.
NOTE. Mixed-effects linear model adjusting for all other variables in the model and age, ethnicity, sex, and marital status.
P values: .05 < P < .10.
Statistical significance at P < .05.
Statistical significance at P < .001.
4. Discussion
Using the ADNI dataset and analyzing cognitive assessment in amnestic MCI for statin use with APOE ε4 allele status as a covariate, we identify many important findings. First, all cognitive assessments trended toward less decline when the subject was concurrently treated with a statin. This supports the position that statins do not have a net negative effect on any form of cognitive assessment. When APOE ε4 allele status was examined as a covariate by holding statin status constant, statistical significance was found in two of four cognitive assessments in statin-negative subjects and in three of four cognitive assessments in statin-positive subjects. ADAS 13 and MMSE in statin-negative subjects and ADAS 11, ADAS 13, and MMSE in statin-positive patients were found to have APOE ε4 positivity. These data suggest the effect of statins is not primarily an APOE ε4 effect. Finally, although no significant numerical trends were apparent, the trending of the data does suggest a potential treatment benefit. When it comes to the mixed-effects model, all iterations that were statin positive had less cognitive decline compared with their statin-negative counterparts. This trend held firm across all four cognitive assessments.
Past studies have shown that APOE ε4 carriers have significantly greater mean LDL compared with APOE ε4–negative individuals [17]. However, no significant differences were noted in total cholesterol, HDL, total cholesterol to HDL ratio, or triglyceride levels [17]. APOE ε4 heterozygotes were also noted to have higher HDL levels and lower total cholesterol to HDL ratios compared with APOE ε4 homozygotes. Because of the significant effect that statins have on LDL, it would seem appropriate for APOE ε4 carriers to have a greater reduction in rate of cognitive decline than their APOE ε4–negative counterparts. Consistent with these past studies, APOE ε4(+/+) subjects had higher rates of cognitive decline.
Aside from the obvious effects statins have on cholesterol and lipoprotein levels, statins have been found to have other effects that may prove effective against dementia progression. Statins have anti-inflammatory and antithrombotic effects that block the synthesis of isopretinoid intermediates, which serve as lipid attachments for intercellular signaling [2]. Not all effects of statins have proved beneficial. Statins have been shown to decrease levels of vitamin E and ubiquinone (coenzyme Q10). Research speculates that decreased levels of lipoproteins in the blood lead to subtle impairments in mental processing via vitamin E, vitamin A, and other fat-soluble substances [2]. Confounding this issue is the fact that cognitive impairments and decrements over time are associated with cardiovascular disease, hypertension, diabetes, etc. Cerebrovascular changes (white matter hyperintensities) increase stroke risk, and these individuals are very likely to receive statin therapy [18]. For these reasons, the general consensus on statins is that the current evidence is insufficient.
The limitation with the largest potential impact on this study is the possibility of confounders. APOE ε4 has already been identified as a potential confounder. MCI can arise from different etiologies, and the effect of statins on these various causes cannot be extrapolated from our data. Other potential confounders could arise from the patient population. Drug interaction and other comorbidities associated with people on a statin regimen may also confound our data. Our sampling did not consist of subjects whose sole medication was a statin. Our analysis also lacks information regarding dose and duration of statin use. The ability to separate groups into high-dose and low-dose users was not possible. Our analysis consisted of cognitive assessment over a time period greater than 1 year. Although each subject's time points were narrowed to as close to one year as possible, potential outliers may have arisen from subjects whose cognitive assessments were prolonged over an extended timeframe. Finally, one potentially beneficial analysis not performed is a multivariate analysis controlling for age, diabetes, cholesterol levels, heart disease, or other health conditions.
Future research needs to reconcile the disparate points of view. Because we show here that statins have no adverse effect on cognition in MCI and may have a slight positive benefit, a clinical trial should be considered with sample sizes large enough to detect significant differences with statin treatment.
Research in Context.
-
1.
Systematic review: Mild cognitive impairment (MCI) amnestic form is widely considered the prodrome of AD dementia. Statins have been interpreted as having pro- and anticognitive benefits with mixed data showing signals in either direction.
-
2.
Interpretation: With the ADNI dataset, longitudinal data of prospectively characterized amnestic MCI subjects shows that statin use does not adversely affect cognition, that statin use might slow rate of progression, and that the observed effect of statins is not principally from APOE ε4 carrier status.
-
3.
Future directions: Statin use might continue to be beneficial. This approach from ADNI needs to be recapitulated in AD dementia. Other studies need to view whether subjects with AD dementia have a lower pathological burden for AD pathology. Finally, this might make an argument for a primary prevention trial with statins.
Acknowledgments
Data collection and sharing for this project were funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Inc.; Alzheimer's Association; Alzheimer's Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen, Inc.; Bristol-Myers Squibb Co.; CereSpir, Inc.; Eisai, Inc.; Elan Pharmaceuticals, plc; Eli Lilly and Co.; EuroImmun AG; F. Hoffmann-La Roche, Ltd.; Genentech, Inc.; Fujirebio Diagnostics, Inc.; GE Healthcare; IXICO, plc.; Janssen Alzheimer Immunotherapy Research & Development, LLC; Johnson & Johnson Pharmaceutical Research & Development, LLC; Lumos Labs, Inc.; H. Lundbeck A/S; Merck & Co., Inc.; Meso Scale Diagnostics, LLC; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corp.; Pfizer, Inc.; Piramal Imaging, SA; Servier; Takeda Pharmaceutical Co.; and Transition Therapeutics, Inc. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Disease Cooperative Study at the University of California, San Diego. ADNI data are disseminated by the Laboratory for Neuroimaging at the University of Southern California.
Footnotes
Sources of support and funding disclosures: Supported by NIAP30 AG019610 and Barrow Neurological Institute and University of Arizona College of Medicine – Phoenix.
Funding disclosures: Dr Sabbagh. Stock/ownership: Muses Labs, Inc.; Versanum, Inc.; Brain Health, Inc. Advisory: Biogen, Inc.; Eli Lilly and Co.; VTV Therapeutics. CME: Med Learning Group; Miller Meded; Medscape. Research investigator: AC Immune; Eli Lilly and Co; Biogen, Inc.; Merck and Co., Inc.; VTV Therapeutics; F. Hoffmann-La Roche, Ltd.; H. Lundbeck A/S; Avid Radiopharmaceuticals; Axovant Sciences, Ltd. Kyle B. Smith has nothing to disclose. Paul Kang has nothing to disclose.
Authorship contributions: Kyle B. Smith oversaw the design of the study, performed collection and organization of data, aided in the statistical analyses, wrote the first draft of the manuscript, and revised the manuscript. Paul Kang aided in statistical analysis, drafting, and revision of statistical analysis and figures. Marwan N. Sabbagh oversaw the design of the study, collection of data, and drafting and critical revision of the manuscript.
References
- 1.Jick H., Zornberg G.L., Jick S.S., Seshadri S., Drachman D.A. Statins and the risk of dementia. Lancet. 2000;356:1627–1631. doi: 10.1016/s0140-6736(00)03155-x. [DOI] [PubMed] [Google Scholar]
- 2.McGuinness B., Craig D., Bullock R., Malouf R., Passmore P. Statins for the treatment of dementia. Cochrane Database Syst Rev. 2014;July 8;(8):CD007514. doi: 10.1002/14651858.CD007514.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kandiah N., Feldman H.H. Therapeutic potential of statins in Alzheimer's disease. J Neurol Sci. 2009;283:230–234. doi: 10.1016/j.jns.2009.02.352. [DOI] [PubMed] [Google Scholar]
- 4.Sparks D.L., Kryscio R.J., Connor D.J., Sabbagh M.N., Sparks L.M., Lin Y. Cholesterol and cognitive performance in normal controls and the influence of elective statin use after conversion to mild cognitive impairment: results in a clinical trial cohort. Neurodegener Dis. 2010;7:183–186. doi: 10.1159/000295660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chuang C.-, Lin C.-, Lin M.-, Sung F.-, Kao C.- Decreased prevalence of dementia associated with statins: a national population-based study. Eur J Neurol. 2015;22:912–918. doi: 10.1111/ene.12402. [DOI] [PubMed] [Google Scholar]
- 6.Beydoun M.A., Beason-Held L.L., Kitner-Triolo M.H., Beydoun H.A., Ferrucci L., Resnick S.M. Statins and serum cholesterol's associations with incident dementia and mild cognitive impairment. J Epidemiol Community Health. 2011;65:949–957. doi: 10.1136/jech.2009.100826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malfitano A.M., Marasco G., Proto M.C., Laezza C., Gazzerro P., Bifulco M. Statins in neurological disorders: an overview and update. Pharmacol Res. 2014;88:74–83. doi: 10.1016/j.phrs.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Solomon A., Kareholt I., Ngandu T., Wolozin B., Macdonald S.W., Winblad B. Serum total cholesterol, statins and cognition in non-demented elderly. Neurobiol Aging. 2009;30:1006–1009. doi: 10.1016/j.neurobiolaging.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Bettermann K., Arnold A.M., Williamson J., Rapp S., Sink K., Toole J.F. Statins, risk of dementia, and cognitive function: secondary analysis of the Ginkgo Evaluation of Memory Study. J Stroke Cerebrovasc Dis. 2012;21:436–444. doi: 10.1016/j.jstrokecerebrovasdis.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rockwood K., Kirkland S., Hogan D.B., MacKnight C., Merry H., Verreault R. Use of lipid-lowering agents, indication bias, and the risk of dementia in community-dwelling elderly people. Arch Neurol. 2002;59:223–227. doi: 10.1001/archneur.59.2.223. [DOI] [PubMed] [Google Scholar]
- 11.Sano M., Bell K., Galasko D., Galvin J.E., Thomas R.G., van Dyck C.H. A randomized, double-blind, placebo-controlled trial of simvastatin to treat Alzheimer disease. Neurology. 2011;77:556–563. doi: 10.1212/WNL.0b013e318228bf11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldman H.H., Doody R.S., Kivipelto M., Sparks D.L., Waters D.D., Jones R.W. Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease: LEADe. Neurology. 2010;74:956–964. doi: 10.1212/WNL.0b013e3181d6476a. [DOI] [PubMed] [Google Scholar]
- 13.Sparks D.L., Sabbagh M.N., Connor D.J., Lopez J., Launer L.J., Petanceska S. Atorvastatin therapy lowers circulating cholesterol but not free radical activity in advance of identifiable clinical benefit in the treatment of mild-to-moderate AD. Curr Alzheimer Res. 2005;2:343–353. doi: 10.2174/1567205054367900. [DOI] [PubMed] [Google Scholar]
- 14.Trompet S., van Vliet P., de Craen A.J., Jolles J., Buckley B.M., Murphy M.B. Pravastatin and cognitive function in the elderly: results of the PROSPER study. J Neurol. 2010;257:85–90. doi: 10.1007/s00415-009-5271-7. [DOI] [PubMed] [Google Scholar]
- 15.Solomon A., Kivipelto M. Cholesterol-modifying strategies for Alzheimer's disease. Expert Rev Neurother. 2009;9:695–709. doi: 10.1586/ern.09.25. [DOI] [PubMed] [Google Scholar]
- 16.Petersen R.C., Caracciolo B., Brayne C., Gauthier S., Jelic V., Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. 2014;275:214–228. doi: 10.1111/joim.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabbagh M.N., Sandhu S., Kolody H., Lahti T., Silverberg N.B., Sparks D.L. Studies on the effect of the apolipoprotein E genotype on the lipid profile in Alzheimer's disease. Curr Alzheimer Res. 2006;3:157–160. doi: 10.2174/156720506776383013. [DOI] [PubMed] [Google Scholar]
- 18.Kelley B.J., Glasser S. Cognitive effects of statin medications. CNS Drugs. 2014;28:411–419. doi: 10.1007/s40263-014-0147-5. [DOI] [PubMed] [Google Scholar]