Abstract
Tuberculosis affects pulmonary and extra‐pulmonary sites with a multitude of differing presentations. The involvement of thoracic wall is a rare entity. We report the case of a patient who had a tumefaction on the right chest wall 6 months after a right breast mastectomy. After an initial radiological suspicion of malignancy, we detected intraoperatively an abscess in which histologic examination revealed granulomas with multinucleated giant cells.
Keywords: Chest wall mass, metastasis, Mycobacterium tuberculosis
Introduction
Chest wall tuberculosis is a very rare condition with few cases reported in the literature. The aim of this article is to report a patient operated for chest wall tumefaction and to review the literature.
Case Report
A 45‐year‐old female patient from the Caribbean was diagnosed with an invasive mucinous breast cancer (pT1c pN0 (0/3) Mx, G2) in her right breast for which she underwent a nipple sparing mastectomy with axillary sentinel lymph node excision. Around 6 months later she presented with a painful swelling on her right chest wall following a mild thoracic trauma.
Physical examination showed a large solitary lesion over the eighth rib, 4 × 5 cm in dimension. The lesion was soft, tender, fluctuating with defined margins and not attached to underlying structures. She was afebrile with normal pulse and blood pressure. Examination of the respiratory system showed no pathological findings. Computed tomography (CT) scan of the chest showed a fracture of the eighth rib with an adjacent tumefaction. For further diagnostics, a positron emission tomography (PET)‐CT scan was ordered. The tumour adjacent to the fractured eighth rib was found PET‐positive, which was highly suspicious for a necrotizing metastasis (Fig. 1). Furthermore, several axillar and infraclavicular lymph nodes were fluorodeoxyglucose (FDG)‐positive but with a lower standardized uptake value (SUV). Several fine needle aspirations of the thoracic lesion and of the axillary lymph nodes showed a granulomatous inflammation without any sign of malignancy. Bacterial cultures remained all negative. The patient showed only mild normocytic normochromic anaemia (haemoglobin (Hb) 119 g/L) with normal leukocytes (8.6 G/L) and platelets (291 G/L). Electrolytes, creatinine, and liver enzymes were normal even if cholestasis parameters were elevated (alkaline phosphatase (ALP) 109 U/L, gamma‐glutamyltransferase (GGT) 203 U/L) without any clinical symptoms. However, the lesion showed a progressive growth. Considering also the high suspicion of malignancy, the patient was admitted for operative excision of the lesion.
Figure 1.
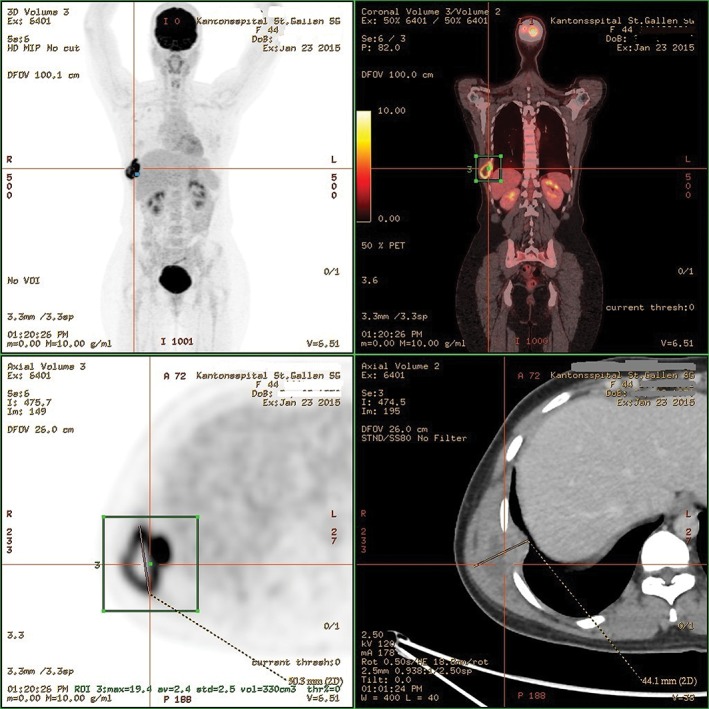
Positron emission tomography showing a fluorodeoxyglucose (FDG)‐positive lesion.
Intraoperatively we found an encapsulated abscess without any macroscopic suspicion of malignancy. Thus we performed an open biopsy and then we applied a vacuum sealing drainage associated with resection of the fractured eighth rib.
Real time polymerase chain reaction (Xpert MTB/RIF test) of the resected tissue specimen detected the presence of Mycobacterium tuberculosis complex with.
Histologic examination of the excised tissue confirmed the presence of typical tubercular lesions revealing granulomas with caseous necrosis. Sputum smear microscopy and cultures ruled out any primary focus in the body. Risk factors for tuberculosis (except the country of origin of the patient) were all negative and there was no history of diabetes or alcohol abuse. The patient was treated with a combination of rifampin, isoniazid, pyrazinamide, and ethambutol and discharged 9 days after admission. On the day of discharge, the wound was healing without any swelling or tenderness of the affected area. Although the World Health Organisation (WHO) recommends a standard 6‐month regimen, according to clinical presentation, bacillary load, and response to therapy, the treatment can be extended up to 9–12 months 1.
Therefore, the plan was to treat the patient as an outpatient and to re‐evaluate her to decide on the total duration of therapy. After 6 months follow‐up, we found no evidence of abnormal wound healing.
Discussion
Tuberculosis is the second leading cause of death from infectious diseases worldwide with 1.5 million deaths in 2013 (WHO report 2014). The Dominican Republic, where our patient originally came from, shows an incidence of 91 cases per 100,000 people in 2005 (eight cases/100,000 people in Switzerland) (WHO report) and 4–9.9/100,000 mortality rate.
Chest wall tuberculosis is a very rare location. Pathogenesis of chest wall tuberculosis includes different causes: either direct spread from pleural or pulmonary disease 2, haematogenous dissemination, extension from lymphadenitis or penetration of the skin to form chronic ulcers. Clinically, it can appear as an abscess or soft tumour most frequently on the sternum or on the ribs 3. Initial diagnosis can be difficult, as patients do not show other specific symptoms. Fine needle aspiration is the favourite diagnostic tool, even though it is not always reliable. Faure et al. showed that only 36% of cases were successfully diagnosed through fine needle aspiration 4.
CT and PET‐CT scan are further diagnostic tools, but differentiating between tuberculosis, abscess or metastasis may be very difficult. The optimal treatment of chest wall tuberculosis is controversial. Some small series showed good results with drug therapy alone 5, 6. However, in other studies, abscesses were not cured and even recurred or progressed despite adequate medical treatment. Good results were obtained with surgery and removal of the tumour including the adjacent rib combined with medical management 7. A recent review of patients who have undergone surgery showed that whole excision of the abscess and primary closure of the wound prevents recurrence 8. Anti‐tuberculosis drug therapy is essential to avoid recurrence, regardless of surgical management.
This case highlights the necessity to include tuberculosis in the differential diagnosis for patients with a persistent chest wall mass, especially the ones whose origin includes endemic regions. In our case, the suspicion of malignancy was prevalent due to the oncological history of the patient.
After surgical removal of all pathological tissues and beginning of anti‐tuberculosis medical treatment, on follow‐up after 7 months, the patient was responding well to treatment.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Minervini, F. , Greuter, L. , Kestenholz, P. , Schneider, T. , Gutmann, C. and Dutly, A.E. (2017) A chest wall mass after breast carcinoma surgery: a simple diagnosis?. Respirology Case Reports, 5 (4), e00240. doi: 10.1002/rcr2.240.
Associate Editor: Coenraad Koegelenberg
References
- 1. Kuzucu A, Soysal O, and Gunen H. 2004. The role of surgery in chest wall tuberculosis. Interact. Cardiovasc. Thorac. Surg. 3:99–103. [DOI] [PubMed] [Google Scholar]
- 2. Hsu HS, Wang LS, Wu YC, et al. 1995. Management of primary chest wall tuberculosis. Scand. J. Thorac. Cardiovasc. Surg. 29(3):119–123. [DOI] [PubMed] [Google Scholar]
- 3. Wiebe ER, and Elwood RK. 1991. Tuberculosis of the ribs – a report of three cases. Respir. Med. 85(3):251–253. [DOI] [PubMed] [Google Scholar]
- 4. Faure E, Souilamas R, Riquet M, et al. 1998. Cold abscess of the chest wall: a surgical entity? Ann. Thorac. Surg. 66(4):1174–1178. [DOI] [PubMed] [Google Scholar]
- 5. Chen CH, Shih JF, Wang LS, et al. 1996. Tuberculous subcutaneous abscess: an analysis of seven cases. Tuber. Lung Dis. 77(2):184–187. [DOI] [PubMed] [Google Scholar]
- 6. Blunt SB, and Harries MG. 1989. Discrete pleural masses without effusion in a young man: an unusual presentation of tuberculosis. Thorax 44(5):436–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paik HC, Chung KY, Kang JH, et al. 2002. Surgical treatment of tuberculous cold abscess of the chest wall. Yonsei Med. J. 43(3):309–314. [DOI] [PubMed] [Google Scholar]
- 8. Lim SY, Pyon JK, Mun GH, et al. 2010. Reconstructive surgical treatment of tuberculosis abscess in the chest wall. Ann. Plast. Surg. 64(3):302–306. https://doi.org/10.1097/SAP.0b013e3181b0bb03. [DOI] [PubMed] [Google Scholar]


